ABSTRACT
BACKGROUND
Leaders in medical education have called for redesign of internal medicine training to improve ambulatory care training. 4 + 1 block scheduling is one innovative approach to enhance ambulatory education.
AIM
To determine the impact of 4 + 1 scheduling on resident clinic continuity.
SETTING
Resident continuity clinic in traditional scheduling in which clinics are scheduled intermittently one-half day per week, compared to 4 + 1 in which residents alternate 1 week of clinic with 4 weeks of an inpatient rotation or elective.
PARTICIPANTS
First-year internal medicine residents.
PROGRAM DESCRIPTION
We measured patient–provider visit continuity, phone triage encounter continuity, and lab follow-up continuity.
PROGRAM EVALUATION
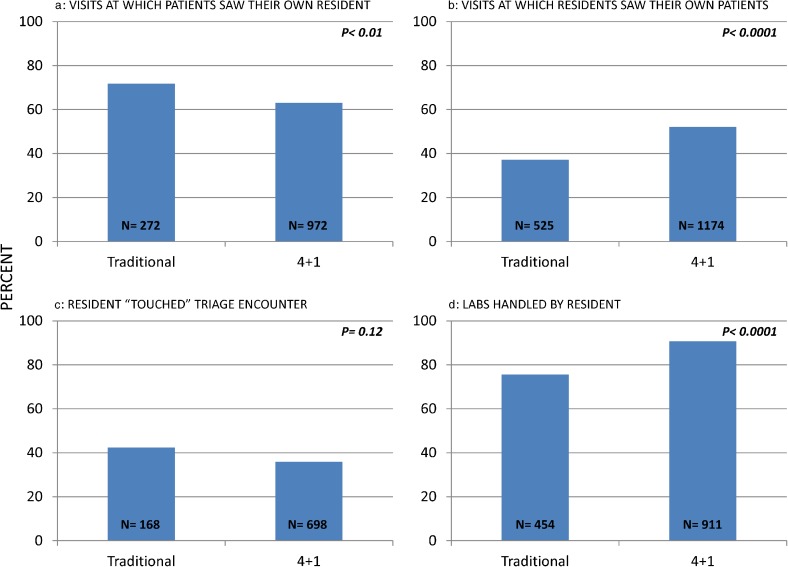
In traditional scheduling as opposed to 4 + 1 scheduling, patients saw their primary resident provider a greater percentage; 71.7 % vs. 63.0 % (p = 0.008). In the 4 + 1 model, residents saw their own patients a greater percentage; 52.1 % vs. 37.1 % (p = 0.0001). Residents addressed their own labs more often in 4 + 1 model; 90.7 % vs. 75.6 % (p = 0.001). There was no significant difference in handling of triage encounters; 42.3 % vs. 35.8 % (p = 0.12).
DISCUSSION
4 + 1 schedule improves visit continuity from a resident perspective, and may compromise visit continuity from the patient perspective, but allows for improved laboratory follow-up, which we pose should be part of an emerging modern definition of continuity.
KEY WORDS: “4 + 1”, block, continuity, resident, clinic
INTRODUCTION
Leaders in graduate medical education have recognized the many challenges facing resident education, and have called for innovative approaches to resident education redesign.1–4 Task forces established by the Society of General Internal Medicine and the Alliance for Academic Internal Medicine Education Redesign have identified inherent problems with the traditional method in which ambulatory care training is incorporated into internal medicine training. One element identified as needing improvement is providing patient-centered longitudinal care.1 Challenges with the current model of teaching ambulatory care include lack of balance between inpatient and outpatient responsibilities. This traditional model often provides disjointed experiences that do not promote longitudinal continuity of care.5,6
In light of these challenges, several residency programs have created innovative methods for scheduling ambulatory clinic, such as block scheduling.7–9 In these models, residents alternate 3 to 6 weeks of inpatient or subspecialty rotations with 1 to 2 weeks of ambulatory time. Prior research has shown that this method of scheduling minimizes conflicts between inpatient and outpatient care, provides a more satisfying outpatient experience for residents and faculty,7,9–11 and increases learning opportunities.9 However, the impact on continuity of patient care remains unclear. This construct is important, because continuity of care between a patient and a provider is a strong component of the patient—provider relationship and is key to the educational value of clinic.6,12,13 Continuity can also lead to improved quality of care, including decreased costs and improved outcomes.14–16
Previously, a 1-year ambulatory care block demonstrated improved visit continuity.8 However, analysis of a 50/50 block scheduling model, in which residents alternated 1 month blocks of inpatient and outpatient experiences, demonstrated decreased visit continuity.17 While research to date has focused on visit continuity, newer definitions of continuity are needed18 that encompass the movement towards the Patient-Centered Medical Home and incorporate all aspects of the care relationship. Our study aims to define continuity with a more modern, encompassing definition including not only visit continuity, but also “in-between” visit continuity in the form of laboratory review and triage calls.
SETTING AND PARTICIPANTS
The University of Colorado Internal Medicine Residency Program consists of 166 residents, with 66 first-year residents. Residents are assigned to one of seven continuity clinic locations, two of which use EPIC as its electronic medical record. Only those interns assigned to clinics using EPIC were included in our study. In these two EPIC-based clinics, there were 15 first-year residents during the 2011–2012 academic year and 23 first-year residents during the 2012–2013 academic year. The change in number of residents between the two years was due to change in overall residency distribution, and was not associated with any change in clinic structure.
PROGRAM DESCRIPTION
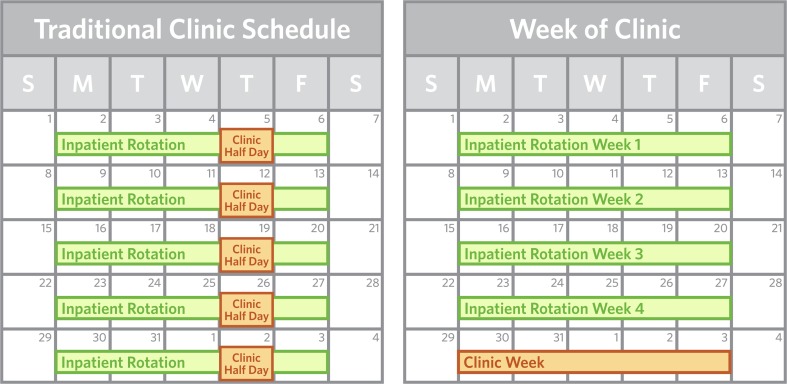
Prior to June of 2012, residents were scheduled using a traditional model in which they participated in continuity clinic 1 to 2 half days per week (Fig. 1). During inpatient rotations, residents attended clinic on their assigned clinic day unless they were on-call or post-call. On outpatient rotations, residents attended clinic twice per week.
Figure 1.
Clinic schedule in the traditional model versus clinic schedule in the 4 + 1 model.
During the 2012–2013 academic year, first-year residents were scheduled in a 4 + 1 block model, in which residents alternated 1 week of clinic with 4 weeks of an inpatient rotation or elective (Fig. 1). Second and third year residents continued with traditional scheduling, and thus were excluded from our study. During their clinic week, residents had seven to eight clinic sessions. The remaining 2 to 3 half days were spent working on Quality Improvement projects, addressing team tasks, and focused reading time. Residents did not go to clinic during inpatient rotations or electives. In both years, residents started with two patients per clinic session with a gradual increase to four patients per clinic session over the first 2 months. There were no other practiced-based interventions during the 2-year program that would have impacted continuity of care.
Residents are assigned their own panel of continuity patients, including transfers from graduating residents and new patients to clinic. During clinic, residents may see patients from their own panel as well as other resident or faculty patients. Visits may include new patient visits, chronic disease management, acute care, and preventative care.
When residents are in clinic, they are expected to see patients, follow-up on lab results, and respond to patient communication. Patient calls or questions are communicated to the resident via triage encounters. If a resident is not in clinic, a team of covering providers (including residents, faculty, nurses and medical assistants) address these labs and triage encounters.
PROGRAM EVALUATION
In this quality assurance project, we measured patient–provider visit continuity based on well-established metrics from previous work,19 phone triage encounter continuity, and lab follow-up continuity. All data was pulled from EPIC, using 2010 Clarity Tables. The project was approved by the local institutional review board (IRB) as Not Human Subject Research Quality Improvement.
METHODS
Patient visit encounters in which a patient had a first-year resident assigned as their primary care provider (PCP) and the visit was completed during the first 5 months of each academic year (2011 in the traditional model and 2012 in the 4 + 1 model) were included in our analysis.
Patient Visit Continuity
From the patient perspective, we evaluated the percentage of time a patient was able to see their primary resident provider versus the percentage of time the patient saw a different provider. From the provider perspective, we analyzed the percentage of time a resident provider saw their own patients versus the percentage of time they saw patients assigned to another provider.
Triage Encounter
We measured continuity of care in between visits by looking at all triage encounters created for patients assigned to a resident provider. Triage encounters are created when patients call the clinic or when providers initiate contact to relay clinical information. We evaluated the percentage of time the encounter was handled by the assigned primary resident provider versus a covering provider on their team.
Lab Follow-Up
Lab results are sent to the ordering provider’s in-basket via EPIC. Once a resident has communicated with the patient regarding the result, the result is then marked as completed. We analyzed the percentage of time a resident handled his or her own lab results versus the percentage of time a result was handled by a covering provider.
Data Analysis
Each of these proportions was calculated according to the pre and post periods, and associations were tested with the Chi-Square statistic. Statistical analyses were performed with SAS Version 9.3 (SAS Institute, Cary, NC).
RESULTS
The total number of clinic sessions per intern increased in 4 + 1 scheduling. The 15 traditional schedule residents had on average 17 sessions for the first 5 months and completed 525 visits. The 23 4 + 1 schedule residents had on average 22.5 clinic sessions for the first 5 months and completed 1,174 visits.
Patient Visit Continuity
From the patient perspective, the percentage of time a patient saw his/her primary resident provider was greater in traditional scheduling as opposed to 4 + 1 scheduling (71.7 % vs. 63.0 %, p = 0.008) (Fig. 2a). From the provider perspective, residents were significantly more likely to see their own patients in the 4 + 1 scheduling system versus the traditional model (52.1 % vs. 37.1 %, p < 0.0001) (Fig. 2b).
Figure 2.
a Continuity from the patient perspective b. Continuity from the resident provider perspective c. Triage encounter continuity d. Lab continuity.
Triage Encounter
The percentage of triage encounters addressed by the primary resident was not statistically significant when comparing the traditional versus 4 + 1 scheduling (42.3 % vs. 35.8 %, p = 0.12) (Fig. 2c).
Lab Follow-Up
The percentage of time a resident addressed their own lab results was significantly greater in 4 + 1 compared to traditional scheduling (90.7 % vs. 75.6 %, p < 0.001) (Fig. 2d).
DISCUSSION
Our project is the first to our knowledge to use a more encompassing definition of continuity, including not only visit continuity, but also lab follow-up and phone triage encounters. The foundation of an outpatient doctor–patient relationship still rests firmly upon mutual visits, but in this era with increased focus on team-centered and patient-centered care, we feel it is appropriate to redefine continuity in this more global fashion.
We demonstrated that for visit continuity, there were advantages to each system. From the resident perspective, residents were more likely to see their own patients in the 4 + 1 system. From the patient perspective, in 4 + 1 scheduling, patients were less likely to see their primary provider. We did not analyze the type of visit scheduled, so it is unknown if visits were for routine follow-up versus urgent visits. We theorize that in 4 + 1 scheduling, residents were more likely to see their own patients for routine follow-up for chronic disease management, as these are visits that can be scheduled weeks in advance, but that patients were less likely to see their primary provider for acute visits.
Patient continuity in terms of communication in between visits using triage encounters did not differ between the two models. There are likely several reasons for this finding. We hypothesize that the majority of triage encounters are created shortly after a visit, and thus residents in the 4 + 1 model of scheduling would have more opportunity able to address these issues that arise during the same clinic week, whereas residents in the traditional model can address triage encounters throughout the month. The ability of our residents to address triage encounters remotely during both study periods likely also contributed to the non-significant outcome.
Residents were more likely to follow-up on their own lab results in the 4 + 1 system. Laboratory follow-up is a key aspect of clinic education, as this is an opportunity to understand disease progression and learn appropriate management skills. The opportunity to both see patients during the same clinic week, if clinically indicated, and to follow-up on labs and triage during the week, offers ‘diagnostic closure’ that was not previously available in continuity clinic. Diagnostic closure allows residents to revise their illness scripts and facilitates deliberate practice amongst our learners.5,20
A significant limitation to our study is that we analyzed the first 5 months of continuity clinic for a first-year resident. This is a very short period of time over which to develop a patient–provider care relationship. It is also during the time of year when a significant transfer of patients occurs. This time frame may affect the patient perspective on their ability to see their own PCP, but this phenomenon would have occurred with the same frequency for both study periods. We theorize that since patients were less likely to be very familiar with their primary provider, they may have been less likely to wait until their resident was in clinic again to address a semi-urgent concern. As the resident–patient relationship develops during residency, it would be interesting to see whether or not continuity measures would change as patients and providers develop a more established care relationship.
The 4 + 1 schedule did significantly increase overall clinic visit volume for the residents. This increased volume allowed for more educational opportunities and a greater exposure to the outpatient setting from early on in residency. We theorize that this increased volume and clinic time, in addition to previously demonstrated improved clinic satisfaction, 7,9 will create a greater comfort level for our residents in the outpatient setting, and potentially encourage greater interest in outpatient-based careers.
A significant limitation to our study is the lack of a control group. In addition, our results are from a single institution, and therefore may not be generalizable to other institutions.
In summary, this program provides a better understanding of the impact of two different scheduling models on an expanded definition of continuity of care in outpatient internal medicine resident clinic. Our program demonstrates that the 4 + 1 schedule for resident continuity clinic allows residents to maintain greater continuity of patient care and greater ability to manage patient care by addressing lab results, but may compromise visit continuity from the patient perspective. Several programs have now developed an “add back” clinic system in which clinic sessions are scheduled in-between extended periods away from clinic to facilitate chronic disease management and continuity. It will be interesting to see if acute care continuity is remedied by such models in future research, as well as how developing models of team-based care impact patient–provider continuity.
Acknowledgements
Contributors
None.
Funders
Colorado Health Foundation. There is no grant number; this funding has a Memorandum of Understanding between the Colorado Health Foundation and the University of Colorado Department of Medicine.
Prior Presentations
Poster Presentation on 4 October 2013 at the Fall Association of Program Directors in Internal Medicine (APDIM) Conference.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Fitzgibbons J, Bordley D, Berkowitz L, Miller B, Henderson M. Redesigning residency education in internal medicine: a position paper from the association of program directors in internal medicine. Ann Intern Med. 2006;144(12):920–926. doi: 10.7326/0003-4819-144-12-200606200-00010. [DOI] [PubMed] [Google Scholar]
- 2.Meyers F, Weinberger S, Fitzgibbons J, Glassroth J, Duffy D, Clayton C. Redesigning residency training in internal medicine: the consensus report of the Alliance for Academic Internal Medicine Education Redesign Task Force. Acad Med. 2007;82(12):1211–1219. doi: 10.1097/ACM.0b013e318159d010. [DOI] [PubMed] [Google Scholar]
- 3.Thomas KG, West CP, Popkave C, Bellini LM, Weinberger SE, Kolars JC, et al. Alternative approaches to ambulatory training: internal medicine residents’ and program directors’ perspectives. J Gen Intern Med. 2009;24:904–10. doi: 10.1007/s11606-009-1015-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holmboe E, Bowen J, Green M, et al. Reforming internal medicine residency training: a report from the Society of General Internal Medicine’s Task force for Residency Reform. J Gen Intern Med. 2005;20(12):1165–1172. doi: 10.1111/j.1525-1497.2005.0249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bowen J, Salerno S, Chamberlain J, Eckstrom E, Chen H, Brandenburg S. Changing habits of practice: transforming internal medicine residency education in ambulatory settings. J Gen Intern Med. 2005;20(12):1181–1187. doi: 10.1111/j.1525-1497.2005.0248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keirns CC, Bosk CL. The unintended consequences of training residents in dysfunctional outpatient settings. Acad Med. 2008;83(5):498–502. doi: 10.1097/ACM.0b013e31816be3ab. [DOI] [PubMed] [Google Scholar]
- 7.Mariotti JL, Shalaby M, Fitzgibbons JP. The 4:1 schedule: a novel template for internal medicine residencies. J Grad Med Educ. 2010;2:541–547. doi: 10.4300/JGME-D-10-00044.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Warm EJ, Schauer DP, Diers T, et al. The ambulatory long-block: an accreditation council for Graduate Medical Education (ACGME) Educational Innovations Project (EIP) J Gen Intern Med. 2008;23(7):921–926. doi: 10.1007/s11606-008-0588-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chaudhry SI, Balwan S, Friedman KA, et al. Moving forward in GME reform: a 4 + 1 model of resident ambulatory training. J Gen Intern Med. 2013;28(8):1100–4. doi: 10.1007/s11606-013-2387-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saultz J, Albedaiwi W. Interpersonal continuity of care and patient satisfaction: a critical review. Ann Fam Med. 2004;2(5):445–451. doi: 10.1370/afm.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blankfield RP, Kelly RB, Alemagno SA, King CM. Continuity of care in a family practice residency program. Impact on physician satisfaction. J Fam Pract. 1990;31(1):69–73. [PubMed] [Google Scholar]
- 12.Strange K. In this issue: continuity of care. Ann Fam Med. 2003;1(3):130–131. doi: 10.1370/afm.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saultz J. Defining and measuring interpersonal continuity of care. Ann Fam Med. 2003;1(3):134–143. doi: 10.1370/afm.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosenblatt R, Wright G, Baldwin L, et al. The effect of the doctor patient relationship on emergency department use among the elderly. Am J Public Health. 2000;90(1):97–102. doi: 10.2105/AJPH.90.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Fam Pract. 2004;53(12):974–980. [PubMed] [Google Scholar]
- 16.Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005;3(2):159–66. doi: 10.1370/afm.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wieland ML, Halvorsen AJ, Chaudhry R, et al. An evaluation of internal medicine residency continuity clinic redesign to a 50/50 outpatient-inpatient model. J Gen Intern Med. 2013;28(8):1014–9. doi: 10.1007/s11606-012-2312-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haggerty J, Reid R, Freeman G, Starfield B, Adair C, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(425):1219–1221. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Breslau N, Reeb KG. Continuity of care in a university-based practice. J Med Educ. 1975;50:965–969. doi: 10.1097/00001888-197510000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Bowen, J. Personal Communication.