ABSTRACT
BACKGROUND
Depression and adherence to antidepressant treatment are important clinical concerns in diabetes care. While patient–provider communication patterns have been associated with adherence for cardiometabolic medications, it is unknown whether interpersonal aspects of care impact antidepressant medication adherence.
OBJECTIVE
To determine whether shared decision-making, patient–provider trust, or communication are associated with early stage and ongoing antidepressant adherence.
DESIGN
Observational new prescription cohort study.
SETTING
Kaiser Permanente Northern California.
PATIENTS
One thousand five hundred twenty-three adults with type 2 diabetes who completed a survey in 2006 and received a new antidepressant prescription during 2006–2010.
MEASUREMENTS
Exposures included items based on the Trust in Physicians and Interpersonal Processes of Care instruments and the Consumer Assessment of Healthcare Providers and Systems (CAHPS) communication scale. Measures of adherence were estimated using validated methods with physician prescribing and pharmacy dispensing data: primary non-adherence (medication never dispensed), early non-persistence (dispensed once, never refilled), and new prescription medication gap (NPMG; proportion of time without medication during 12 months after initial prescription).
RESULTS
After adjusting for potential confounders, patients’ perceived lack of shared decision-making was significantly associated with primary non-adherence (RR = 2.42, p < 0.05), early non-persistence (RR = 1.34, p < 0.01) and NPMG (estimated 5 % greater gap in medication supply, p < 0.01). Less trust in provider was significantly associated with early non-persistence (RRs 1.22–1.25, ps < 0.05) and NPMG (estimated NPMG differences 5–8 %, ps < 0.01).
LIMITATIONS
All patients were insured and had consistent access to and quality of care.
CONCLUSIONS
Patients’ perceptions of their relationships with providers, including lack of shared decision-making or trust, demonstrated strong associations with antidepressant non-adherence. Further research should explore whether interventions for healthcare providers and systems that foster shared decision-making and trust might also improve medication adherence.
KEY WORDS: medication adherence, antidepressive agents, shared decision making, trust, physician–patient relations, diabetes mellitus
INTRODUCTION
Among adults with diabetes, patient–provider communication and interpersonal aspects of care, such as patients’ trust in their provider and perceptions of shared decision-making, are associated with medication non-adherence for cardiometabolic (blood pressure, lipid and glucose-lowering) therapies.1 It is not known whether these potentially modifiable characteristics of the patient–provider relationship are similarly associated with initiation of and persistence to other medication types, such as antidepressant medications, and whether they are also important for adherence in the early stages of treatment.2 The focus on early adherence is important, as one in five patients newly prescribed a cardiometabolic medication either never fills or never refills the prescription and fails to become an ongoing user.3
Depression, an important comorbidity among adults with diabetes, has been associated with poorer disease self-management and greater risk of diabetic complications, including microvascular and macrovascular disease, dementia, and early mortality.4–8 This association is substantial in magnitude; estimates suggest that smoking, poor diet, and inactivity may be increased by 30–100 % and the risk for adverse outcomes including dementia and mortality doubles when diabetes is complicated by depression.5–7 However, depression is often unrecognized among patients with diabetes in primary care settings, and adequate antidepressant treatment is received by less than one-third of such patients.2,9 Premature discontinuation of antidepressant treatment is common, representing one contributor to low rates of adequate depression care.10,11 We recently reported that 40 % of adults with diabetes prescribed an antidepressant medication did not refill it after the initial dispensing, and two-thirds had discontinued within 12 months of initiating treatment.12 Both limited health literacy and racial/ethnic minority status were independent risk factors for non-adherence. Less is known about whether potentially modifiable provider factors, such as communication patterns, are associated with antidepressant non-adherence and may serve as targets for interventions.2 In this study of adults with diabetes, we examined whether the patient–provider relationship is associated with adherence for newly prescribed antidepressants across the acute, continuation, and maintenance phases of depression treatment.13 This study was approved by the Kaiser Permanente Institutional Review Board.
METHODS
Participants
The Diabetes Study of Northern California (DISTANCE) Survey was conducted during 2005–2006 among members of Kaiser Permanente Northern California (KPNC), a large integrated healthcare delivery system that serves 30 % of the population of Northern California within the KPNC catchment area. We contacted an ethnically stratified random sample of adults with diabetes aged 30 to 75 years, with a final sample of 20,188 respondents (62 % response rate via Council on American Survey Research Organizations algorithm adjusting for eligibility). Participants completed a written (33.1 %) or web-based survey (15.2 %) in English, or a computer-assisted telephone interview (51.7 %) in English, Spanish, Cantonese, Mandarin, or Tagalog. Details of the design and methods have been described previously.14
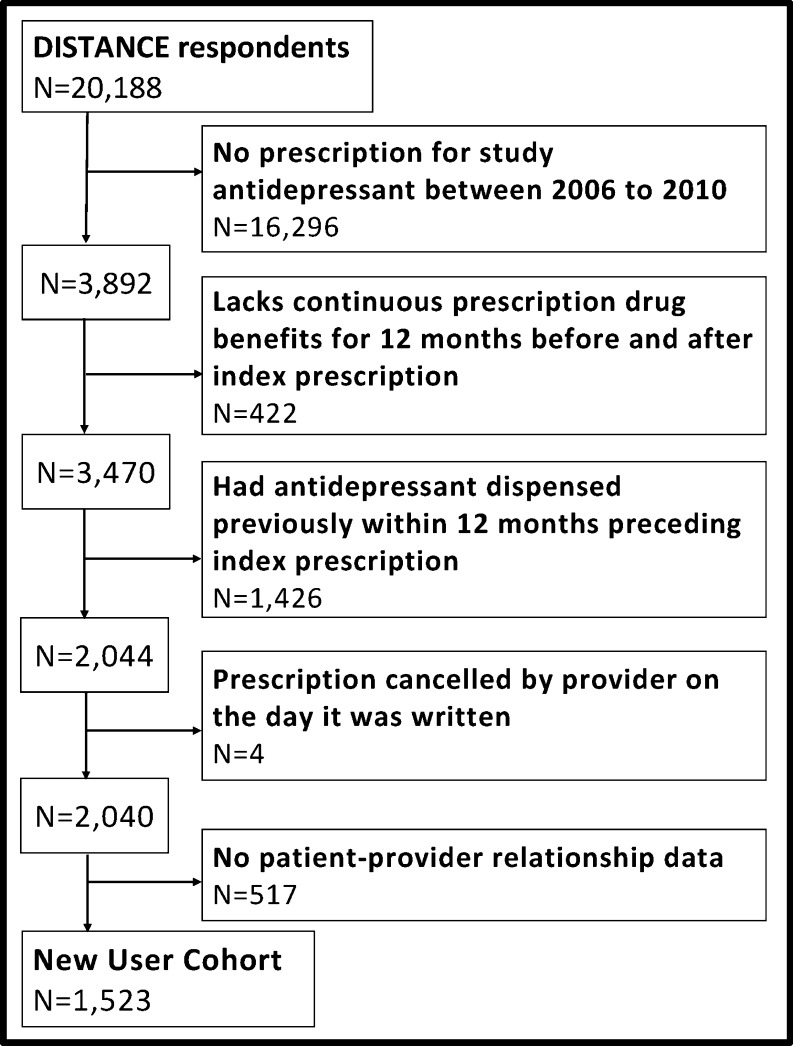
DISTANCE respondents were included in this study if they were newly prescribed a selective serotonin reuptake inhibitor, a serotonin-norepinephrine reuptake inhibitor, bupropion or mirtazapine during 2006–2010 (index prescription) based on physician orders in the KPNC electronic medical record; had not been dispensed any of these antidepressants in the 12 months preceding the index prescription; had continuous pharmacy benefits for at least 12 months before and after the index prescription; and responded to one or more survey items assessing patient–provider communication (Fig. 1).
Figure 1.
Flowchart of new antidepressant user cohort.
Measures
Each participant rated the quality of his/her provider relationship during the preceding 12 months. Overall patient–provider communication quality was assessed with the four-item Consumer Assessment of Healthcare Providers and Systems (CAHPS) communication composite.15 Trust was assessed with two items adapted from the Trust in Physicians Scale.16,17 Shared decision-making was assessed with two items modified from the Interpersonal Processes of Care Instrument,18,19 one of which is similar to a CAHPS supplementary item (see Table 2 for specific item wording).15,20 To simplify the survey and improve consistency across items, the time frame (last 12 months) and response choices (“never”, “sometimes”, “usually”, and “always”) from the CAHPS were employed for all items. Items assessing trust and shared decision-making were analyzed individually and coded dichotomously as better (“always”) versus worse (“never”/“sometimes”/“usually”) quality, based on the distribution of responses, as few participants reported worse quality (Table 2). The CAHPS communication items have high internal consistency15,21 and were combined to create a CAHPS summary variable for each participant who responded to as least two CAHPS items. A participant who answered “always” for all CAHPS items was classified as having better quality communication, whereas one who responded “never”, “sometimes”, or “usually” to any of the items was classified as having worse quality. Sensitivity models were conducted using a CAHPS summary score recoded to identify more serious communication deficits by averaging the responses for patients who answered two or more CAHPS questions. The summary score had a range of 0 to 3 and was dichotomized at > 1.5 (better quality) versus ≤ 1.5 (worse quality; n = 160, 12.7 %).
Table 2.
Proportion of Participants Reporting Lower Quality of Communication* with their Provider
| Lower quality N (%) | |
|---|---|
| Trust | |
| In the last 12 months, how often have you felt confidence and trust in your personal physician? (N = 1,468) | 498 (33.9) |
| In the last 12 months, how often did you feel that your personal physician was putting your medical needs above all other considerations when treating your medical problems? (N = 1,224) | 473 (38.6) |
| Shared decision-making | |
| In the last 12 months, how often did your personal physician involve you in making decisions about your care as much you wanted? (N = 1,219) | 594 (48.7) |
| In the last 12 months, how often did your personal physician seem to understand the kinds of problems you have in carrying out recommended treatments? (N = 1,067) | 490 (45.9) |
| Overall communication quality | |
| In the last 12 months, how often did doctors or health care providers listen carefully to you? (N = 1,256) | 476 (37.9) |
| In the last 12 months, how often did doctors or health care providers explain things (directly or through an interpreter) in a way you could understand? (N = 1,454) | 565 (38.9) |
| In the last 12 months, how often did doctors or health care providers show respect for what you had to say? (N = 1,248) | 403 (32.3) |
| In the last 12 months, how often did doctors or health care providers spend enough time with you? (N = 1,255) | 562 (44.8) |
| Overall communication quality summary score (N = 1,260) | 741 (58.8) |
*Participants responded “never”, “sometimes” or “usually” as opposed to “always”
Adherence
Medication adherence indicators were based on pharmacy utilization according to validated methods designed to assess adherence in newly prescribed medications.3,22 Primary non-adherence was defined as no dispensing of the index prescription. Early non-persistence was defined as the dispensing of the index prescription, without at least one medication refill within the period, defined by the number of days’ supply of medication dispensed plus a grace period equal to the original days’ supply. New prescription medication gap (NPMG) was calculated as the proportion of time that a person was without medication during 12 months after the initial prescription date based on the actual days’ supply dispensed.3 It is common for individuals to switch antidepressants early in the course of treatment because of side effects or lack of response, so if pharmacy data indicated a switch from the original medication to any other antidepressant medication under study, we counted dispensing of the new medication toward the adherence measure.
Data Analysis
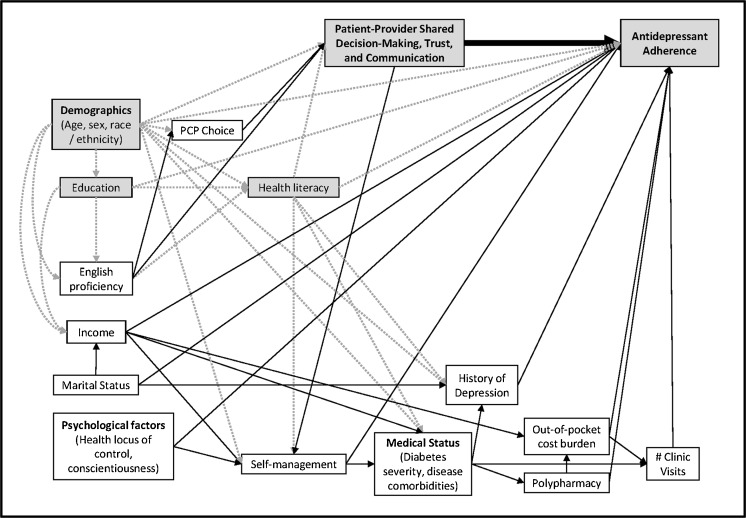
We constructed a directed acyclic graph (DAG) (Fig. 2) based on our team’s interpretation of a broad review of the literature, and applied established methods for analysis to identify potentially confounding variables and avoid errors from overadjustment of unnecessary variables in generating causal estimates of the impact of communication on adherence.23,24 Analysis of the DAG indicated that adjustments for age, gender, race/ethnicity, education, and health literacy were both necessary and sufficient, and those variables (described below) were included as covariates in multivariate models. Multivariate, modified log Poisson regression models were specified to provide a direct estimate of the relative risk of antidepressant non-adherence for those with better versus worse communication quality.25 Modified least squares regression was used to estimate the mean absolute prevalence (predicted probabilities) of non-adherence for each communication group.26 For the continuous outcome (NPMG), a generalized linear regression model was specified with the same covariates. Multivariate models were expansion weighted for the race-stratified sampling design (non-proportional sampling fractions) and weighted for survey non-response using the Horvitz-Thompson approach.27 Multiple imputation with 20 imputations was used for missing covariates, and an alpha level of 0.05 was set as the threshold for statistical significance. As sensitivity analyses, all models were repeated after excluding patients prescribed bupropion or duloxetine, both of which have Food and Drug Administration (FDA)-approved non-psychiatric indications, who lacked a chart diagnosis of a depressive or anxiety disorder within 1 year of the index prescription.
Figure 2.
Directed acyclic graph demonstrating covariate selection to estimate the effect of patient–provider relationship variables on antidepressant adherence. Shaded box: variable included in multivariate analyses. White box: variable excluded as potential confounder, and therefore not included in multivariate analyses. Solid arrow: causal pathways that do not confound the association between patient–provider relationship variables and antidepressant adherence. Dotted arrow: causal pathways that potentially confound the association between patient–provider relationship variables and antidepressant adherence in unadjusted analyses, but do not serve as confounders in multivariate models that include the variables identified in the shaded boxes. A directed acyclic graph was constructed based on published literature to illustrate the relationships between variables associated with patient–provider relationship quality and antidepressant adherence. All of the variables represented were available in the DISTANCE data set. An established process for analysis of a directed acyclic graph was applied to identify which of these variables were potential confounders of the association between patient–provider relationship variables and antidepressant adherence.23 This analysis revealed that adjustments for the variables in the shaded boxes (age, gender, race/ethnicity, education, and health literacy) were necessary and sufficient to include in the analysis as covariates, while variables in the white boxes were excluded as covariates. The causal relationships shown in the grey dotted arrows are accounted for by adjustment for the identified covariates (age, gender, race/ethnicity, education, and health literacy), and therefore, the relationships shown in dotted lines do not confound the association between patient–provider relationship and antidepressant adherence. The remaining causal pathways (solid arrows) do not require adjustment because they do not function as confounders. This is visualized in the graph because variables with causal links to the independent variable (English proficiency and PCP choice have solid arrows to patient–provider relationship variables) do not have direct causal pathways to the dependent variable (there are no solid arrows from these variables to antidepressant adherence). Likewise, variables with causal associations with the dependent variable (all other variables in white boxes have solid arrows to antidepressant adherence) do not have causal associations with the independent variable (these variables do not have solid arrows terminating at patient–provider relationship variables).
Covariates
The DISTANCE survey assessed demographic information (age, gender, race/ethnicity: white; African American; Latino; Asian American; Filipino; or other/multiracial/unknown, and education) and health literacy based on a validated instrument.28,29
RESULTS
Of 2,040 patients newly prescribed an antidepressant, those who responded to at least one communication item (75 %; n = 1,523) had a mean age of 58 years, included more females, were 70 % minorities, and included many with low educational attainment or limited health literacy (Table 1). Participants reported high ratings for the quality of their provider relationship, with only one-third to one-half of participants selecting the responses that were below the highest possible rating for individual survey items (Table 2).
Table 1.
Characteristics of Participants Who Were Prescribed an Antidepressant Medication (n = 1,523)
| Mean (SD) or n (%) | |
|---|---|
| Age | 58.0 (10.5) |
| Gender | |
| Male | 609 (40.0) |
| Female | 914 (60.0) |
| Race/ethnicity | |
| African American | 287 (18.8) |
| Asian American | 100 (6.6) |
| Caucasian | 457 (30.0) |
| Filipino | 112 (7.4) |
| Latino | 339 (22.3) |
| Multiracial | 158 (10.4) |
| Other/unknown | 70 (4.6) |
| Education (N = 1492) | |
| Less than high school | 265 (17.8) |
| High school graduate or greater | 1,227 (82.2) |
| Health literacy (N = 1282) | |
| No limitations | 361 (28.2) |
| Any limitations | 921 (71.8) |
| Length of patient’s relationship with primary care provider in years (N = 1522) | 6.1 (4.4) |
Primary Non-Adherence
Primary non-adherence for antidepressants, while not common (4.3 %; n = 66), was strongly associated with patients’ perceived lack of involvement in decision-making (RR = 2.42, 95 % CI 1.13–5.16), and had modest but nonsignificant associations with lack of trust on one item (patient’s needs first RR = 1.97, 95 % CI 0.97–4.00) and worse overall communication quality (RR = 1.88, 95 % CI 0.89–3.99; Table 3).
Table 3.
Adjusted Associations Between Patient–Provider Communication and Antidepressant Medication Non-Adherence at Different Phases of Treatment
| n | Primary non-adherence | Early non-persistence | NPMG | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RR (95 % CI) | Est. % non-adherent | p | RR (95 % CI) | Est. % non-adherent | p | β (95 % CI) | Est. % of year without medication (# days) | p | ||
| Trust items | ||||||||||
| Confidence and trust | 1468 | 1.14 (0.59, 2.18) | 0.70 | 1.22 (1.02, 1.45) | 0.03 | 0.05 (0.01, 0.09) | < 0.01 | |||
| Worse quality * | 5.1 % | 48.7 % | 43.2 % (158) | |||||||
| Better quality † | 4.6 % | 40.9 % | 38.1 % (139) | |||||||
| Difference | 0.5 % | 7.8 % | 5.1 % (19) | |||||||
| Patient’s needs first | 1224 | 1.97 (0.97, 4.00) | 0.06 | 1.25 (1.04, 1.51) | 0.02 | 0.08 (0.04, 0.12) | < 0.01 | |||
| Worse quality * | 5.5 % | 47.7 % | 44.1 % (161) | |||||||
| Better quality † | 3.0 % | 39.0 % | 35.9 % (131) | |||||||
| Difference | 2.5 % | 8.7 % | 8.2 % (30) | |||||||
| Shared decision-making items | ||||||||||
| Involvement in decisions | 1219 | 2.42 (1.13, 5.16) | 0.02 | 1.34 (1.11, 1.62) | < 0.01 | 0.05 (0.01, 0.09) | < 0.01 | |||
| Worse quality * | 6.1 % | 47.9 % | 42.0 % (153) | |||||||
| Better quality † | 2.7 % | 37.1 % | 36.6 % (134) | |||||||
| Difference | 3.4 % | 10.8 % | 5.4 % (20) | |||||||
| Understood problems | 1067 | 1.08 (0.52, 2.24) | 0.84 | 1.28 (1.04, 1.58) | 0.02 | 0.01 (−0.03, 0.05) | 0.69 | |||
| Worse quality * | 4.4 % | 45.5 % | 38.4 % (140) | |||||||
| Better quality † | 4.1 % | 36.6 % | 37.6 % (137) | |||||||
| Difference | 0.3 % | 8.9 % | 0.9 % (3) | |||||||
| Overall communication quality | ||||||||||
| CAHPS summary score | 1260 | 1.88 (0.89, 3.99) | 0.10 | 1.13 (0.94, 1.36) | 0.18 | 0.01 (−0.03, 0.05) | 0.53 | |||
| Worse quality * | 5.2 % | 45.9 % | 40.2 % (147) | |||||||
| Better quality † | 3.1 % | 41.1 % | 38.9 % (142) | |||||||
| Difference | 2.1 % | 4.8 % | 0.3 % (5) | |||||||
Models adjusted for age, gender, race/ethnicity, education, and health literacy
*Worse quality: For Trust and Shared Decision-Making items, participants responded “never”, “sometimes”, or “usually.” For CAHPS Summary Score, participants responded to at least two items and responded “never”, “sometimes”, or “usually” for at least one of these items
†Better quality: For Trust and Shared Decision-Making items, participants responded “always.” For CAHPS Summary Score, participants responded to at least two items and responded “always” to both items
Early Non-Persistence
Unlike primary non-adherence, antidepressant early non-persistence was quite common (44.8 %: n = 682), and was also significantly associated with all items indicating patients’ perceived lack of shared decision-making (RR 1.34, 95 % CI 1.11–1.62 and 1.28, 95 % CI 1.04–1.58) and lack of trust (RR 1.22, 95 % CI 1.02–1.45 and 1.25 95 % CI 1.04–1.15; Table 3), but not with worse overall communication quality (RR 1.13, 95 % CI 0.94, 1.36).
New Prescription Medication Gap (NPMG)
During the 12 months following the index prescription, adherence was poorer, as indicated by higher mean absolute proportion of time without a sufficient antidepressant medication supply (NPMG) among patients who perceived a lack of trust (43 % gap in medications versus 38 % for “confidence and trust”, and 44 % versus 36 % for “patient’s needs first”, p < 0.01) or a lack of shared decision-making on one survey item (42 % versus 37 % for “involvement in decisions”, p < 0.01). Patients who rated their physicians lower on these measures on average had between 19 and 30 excess days without antidepressant medications over the course of the year (Table 3). Overall communication quality was not significantly associated with NPMG.
Sensitivity Analyses
In the sensitivity analyses that employed the recoded CAHPS variable indicating more severe communication deficits, worse overall communication quality was not significantly associated with primary non-adherence (RR = 1.63, 95 % CI 0.82–3.23) or NPMG (45 % gap in medications versus 39 %, p = 0.07), but was significantly associated with early non-persistence (RR = 1.40, 95 % CI 1.10–1.77). After excluding patients prescribed bupropion or duloxetine without a chart diagnosis of a depressive or anxiety disorder, the point estimates for the effects of relationship variables on adherence were largely unchanged, with minor changes in the confidence intervals.
DISCUSSION
Among adults with diabetes, patients demonstrated poorer antidepressant adherence when they perceived the provider relationship to be of poorer quality, particularly lacking trust or shared decision-making. These associations, which were adjusted for potential confounders (age, gender, race/ethnicity, education and health literacy), varied across different stages of adherence during the first year, suggesting that different elements of the patient–provider relationship may have differing impact at each stage.
Primary non-adherence more than doubled among patients who perceived less involvement in decision-making as compared to those who perceived more involvement. Although this pattern is perhaps unsurprising, the magnitude of this association was much greater than for other stages of adherence examined, suggesting that patients’ perceptions of involvement may have particular significance for the initiation of new antidepressant treatment. Some associations between relationship quality and primary adherence were moderate in magnitude (overall communication quality RR = 1.88; patient’s needs first RR = 1.97) but not statistically significant in this sample. Because primary non-adherence was so infrequent (4.3 %), the models had limited statistical power to detect significant associations.
Early non-persistence was very common (45 % of this sample) and substantially more prevalent than we previously observed for cardiometabolic therapies (18 %),3 indicating that many patients never refilled their prescription and thus failed to become ongoing users. We found that patients’ perceptions of low trust and shared decision-making were significantly associated with never refilling antidepressants after the initial dispensing, with similar patterns for NPMG, the integrated measure that summarizes non-adherence over the first year of treatment. In contrast, overall communication quality was not significantly associated with either early non-persistence or NPMG in our primary analyses. This less robust association was confirmed by the sensitivity models, in which severely impaired overall communication was not significantly associated with primary non-adherence or NPMG, but was associated with early non-persistence. Our findings are consistent with a recent study that reported that antidepressant adherence was associated with specific types of patient–provider communication that displayed more empathy and elements of motivational interviewing, a technique consistent with shared decision-making.30 These findings suggest that measures of overall communication quality may be too general, and less sensitive than indicators of those specific aspects of patient–provider relationships when examining associations with outcomes such as medication adherence.
These findings are similar to previous work in the DISTANCE sample in which we found poor adherence to cardiometabolic medications was associated with poorer communication quality.1 However, the current study extends the literature on communication and medication adherence in demonstrating the strong association of shared decision-making and patient–provider trust among a new prescription cohort and during the earliest stages of treatment when treatment discontinuation is most likely to occur. The importance of understanding the correlates of early adherence, such as shared-decision making and trust, is underscored by a recent study that found that 22 % of patients prescribed an initial cholesterol lowering medication and 8 % prescribed a cardiovascular medication never filled their initial prescription.31
Although not directly comparable, we note that the adjusted effects of trust and shared decision-making on antidepressant early non-persistence (8–11 % greater prevalence of early non-persistence, Table 3) were almost twice as large as the effects for these same variables on secondary cardiovascular medication adherence (4–6 % greater prevalence of non-adherence based on continuous medication gap).1 Further research is warranted to identify reasons underlying the larger communication effect for antidepressant adherence relative to cardiovascular medication adherence. Potential explanations could include differences in the side effect profiles of these classes of medications (i.e., communication patterns might be more important for initial adherence among patients who are concerned about or experience side effects); differences in patient or provider perception of the benefit of the medication; differences among a new prescription cohort versus established users; or methodological differences between the studies.
Patient–provider relationships are potentially modifiable, and these findings suggest ways providers may further help patients with depression. Research has shown that adherence to antidepressant medications is improved when treatment is provided in the context of a team-based collaborative care model.32,33 Our findings are consistent with research demonstrating that models of care that are effective in improving antidepressant adherence provide opportunities for an enhanced relationship between a patient and his/her primary care team through frequent contacts, outreach, and support by care managers, as well as psychoeducation and care coordination. An extension of the chronic care model, the ‘health literate care model’, applies a ‘universal precautions’ framework in advocating for the institutionalization of practices at both the level of individual providers and the healthcare system, many of which are intended to promote trust and foster improved patient–provider relationships.34–36 Future research on adherence interventions may wish to emphasize methods that can help providers prioritize efforts to foster trust and a positive therapeutic alliance through shared decision-making with patients. It would also be important to evaluate whether tailored interventions that may emphasize different aspects of the relationship based on individual patient characteristics, such as health literacy or others, provide further benefit in addition to a ‘universal precautions’ framework.
The sample size in this study, although reasonably large, restricted our ability to detect associations between rare outcomes, such as primary non-adherence, and aspects of the patient–provider relationship. Lacking adherence at the early stages of antidepressant treatment is an important clinical problem, and our findings suggest that future research may wish to pay particular attention to interventions that impact primary non-adherence and early non-persistence. The scope of this problem may be greater in settings outside KPNC, where all patients were insured and had convenient access to on-site or mail order pharmacy services.
Some other study limitations and strengths should be noted. Although participants reported on the provider relationship quality in 2006, some patients did not receive an antidepressant prescription for several years after the survey, and we were unable to verify whether the provider who prescribed the antidepressant medication was the same as the one the patient reported about in the survey. This limitation introduces some measurement error that would decrease our ability to detect a true association between relationship quality and adherence; thus, our findings are likely conservative. However, patients in this study did have long-term relationships with their primary care providers, with the average duration being over 6 years. Thus, our findings of consistent associations between the patient’s perception of relationship quality and subsequent medication adherence support the durability of this association over longer intervals of time.
Antidepressant adherence was estimated based on pharmacy utilization data according to validated methods,3 thus extending the literature on associations between communication and antidepressant adherence to include objective measures. Dispensing records likely overestimate adherence (as dispensed medications may not have been consumed), although we assume such misclassification is likely similar across communication quality and thus not biasing the associations. Some patients may have been referred for psychotherapy for depression; however, this is also unlikely to have introduced a systematic bias to the observed associations. Psychotherapy is an uncommon treatment approach among depressed patients with diabetes, as illustrated by research in another setting demonstrating that 93 % failed to receive a minimal treatment course (four sessions).2
Our findings arise from a large and diverse patient sample (approximately 30 % of the population within the KPNC catchment area), and therefore should be applicable to a population with varying socioeconomic conditions who are cared for in settings with consistent access to and quality of care. Thus findings may not generalize to uninsured patients.
Specific aspects of the patient–provider relationship, shared decision-making and trust, may influence adherence to antidepressant medications at the initiation of treatment and over the course of 12 months. These effects are independent of patient characteristics, including health literacy and education. Inadequate medication adherence across stages of treatment and across medication classes is common and a pressing public health concern. Because the patient–provider relationship is potentially modifiable, this serves as a promising target for interventions to improve adherence. Relevant interventions to encourage providers to engage in shared decision-making and facilitate trust and communication can be developed at the level of the individual provider, clinic, provider network, or healthcare system. Further research is needed to examine whether such provider or structural interventions focusing on improving the patient–provider relationship will actually improve treatment adherence.
Acknowledgements
This research was supported by funding from the National Institutes of Health (R01-DK080726, R01-DK081796, P30-DK092924, and NCATS Grant KL2 TR000421). The research reported in this manuscript was presented at the annual meeting of the Academy of Psychosomatic Medicine in Tuscon, AZ, November 2013.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Ratanawongsa N, Karter AJ, Parker MM, et al. Communication and medication refill adherence: the Diabetes Study of Northern California. JAMA Intern Med. 2013;173(3):210–218. doi: 10.1001/jamainternmed.2013.1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katon WJ, Simon G, Russo J, et al. Quality of depression care in a population-based sample of patients with diabetes and major depression. Med Care. 2004;42(12):1222–1229. doi: 10.1097/00005650-200412000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Karter AJ, Parker MM, Moffet HH, Ahmed AT, Schmittdiel JA, Selby JV. New prescription medication gaps: a comprehensive measure of adherence to new prescriptions. Health Serv Res. 2009;44(5 Pt 1):1640–1661. doi: 10.1111/j.1475-6773.2009.00989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001;63(4):619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Lin EH, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–2160. doi: 10.2337/diacare.27.9.2154. [DOI] [PubMed] [Google Scholar]
- 6.Katon WJ, Rutter C, Simon G, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28(11):2668–2672. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 7.Katon W, Lyles CR, Parker MM, Karter AJ, Huang ES, Whitmer RA. Association of depression with increased risk of dementia in patients with type 2 diabetes: the diabetes and aging study. Arch Gen Psychiatry. 2012;69(4):410–417. doi: 10.1001/archgenpsychiatry.2011.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sullivan MD, O’Connor P, Feeney P, et al. Depression predicts all-cause mortality: epidemiological evaluation from the ACCORD HRQL sub study. Diabetes Care. 2012;35(8):1708–1715. doi: 10.2337/dc11-1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hudson DL, Karter AJ, Fernandez A, et al. Differences in the clinical recognition of depression in diabetes patients: the diabetes study of northern California (DISTANCE) Am J Manage Care. 2013;19(5):344–352. [PMC free article] [PubMed] [Google Scholar]
- 10.Lin EH, Von Korff M, Katon W, et al. The role of the primary care physician in patients’ adherence to antidepressant therapy. Med Care. 1995;33(1):67–74. doi: 10.1097/00005650-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Mojtabai R, Olfson M. National patterns in antidepressant treatment by psychiatrists and general medical providers: results from the national comorbidity survey replication. J Clin Psychiatry. 2008;69(7):1064–1074. doi: 10.4088/JCP.v69n0704. [DOI] [PubMed] [Google Scholar]
- 12.Bauer AM, Schillinger D, Parker MM, et al. Health literacy and antidepressant medication adherence among adults with diabetes: the Diabetes Study of Northern California (DISTANCE) J Gen Intern Med. 2013;28(9):1181–1187. doi: 10.1007/s11606-013-2402-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Practice guideline for the treatment of patients with major depressive disorder. 3. Washington DC: American Psychiatric Association; 2010. [PubMed] [Google Scholar]
- 14.Moffet HH, Adler N, Schillinger D, et al. Cohort Profile: The Diabetes Study of Northern California (DISTANCE)–objectives and design of a survey follow-up study of social health disparities in a managed care population. Int J Epidemiol. 2009;38(1):38–47. doi: 10.1093/ije/dyn040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hargraves JL, Hays RD, Cleary PD. Psychometric properties of the Consumer Assessment of Health Plans Study (CAHPS) 2.0 adult core survey. Health Serv Res. 2003;38(6 Pt 1):1509–1527. doi: 10.1111/j.1475-6773.2003.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anderson LA, Dedrick RF. Development of the trust in physician scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol Rep. 1990;67(3 Pt 2):1091–1100. doi: 10.2466/pr0.1990.67.3f.1091. [DOI] [PubMed] [Google Scholar]
- 17.Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the trust in physician scale. The Stanford Trust Study Physicians. Med Care. 1999;37(5):510–517. doi: 10.1097/00005650-199905000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Stewart AL, Napoles-Springer A, Perez-Stable EJ. Interpersonal processes of care in diverse populations. Milbank Q. 1999;77(3):305–339. doi: 10.1111/1468-0009.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stewart AL, Napoles-Springer AM, Gregorich SE, Santoyo-Olsson J. Interpersonal processes of care survey: patient-reported measures for diverse groups. Health Serv Res. 2007;42(3 Pt 1):1235–1256. doi: 10.1111/j.1475-6773.2006.00637.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agency for Health Care Policy and Research. CAHPS Health Plan Survey 4.0 Supplemental Items for the Adult Questionnaires https://cahps.ahrq.gov/surveys-guidance/item-sets/HP/1157a_engadultsupp_40.pdf. Accessed October 3, 2014.
- 21.Dyer N, Sorra JS, Smith SA, Cleary PD, Hays RD. Psychometric properties of the Consumer Assessment of Healthcare Providers and Systems (CAHPS(R)) clinician and group adult visit survey. Med Care. 2012;50(Suppl):S28–S34. doi: 10.1097/MLR.0b013e31826cbc0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raebel MA, Schmittdiel J, Karter AJ, Konieczny JL, Steiner JF. Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases. Med Care. 2013;51(8 Suppl 3):S11–S21. doi: 10.1097/MLR.0b013e31829b1d2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48. doi: 10.1097/00001648-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Hernan MA, Hernandez-Diaz S, Werler MM, Mitchell AA. Causal knowledge as a prerequisite for confounding evaluation: an application to birth defects epidemiology. Am J Epidemiol. 2002;155(2):176–184. doi: 10.1093/aje/155.2.176. [DOI] [PubMed] [Google Scholar]
- 25.Zou GY. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 26.Cheung YB. A modified least-squares regression approach to the estimation of risk difference. Am J Epidemiol. 2007;166(11):1337–1344. doi: 10.1093/aje/kwm223. [DOI] [PubMed] [Google Scholar]
- 27.Horvitz DG, Thompson DJ. A generalization of sampling without replacement from a finite universe. J Am Stat Assoc. 1952;47(260):663–685. doi: 10.1080/01621459.1952.10483446. [DOI] [Google Scholar]
- 28.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594. [PubMed] [Google Scholar]
- 29.Sarkar U, Schillinger D, Lopez A, Sudore R. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J Gen Intern Med. 2011;26(3):265–271. doi: 10.1007/s11606-010-1552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaplan JE, Keeley RD, Engel M, Emsermann C, Brody D. Aspects of patient and clinician language predict adherence to antidepressant medication. J Am Board Fam Med. 2013;26(4):409–420. doi: 10.3122/jabfm.2013.04.120201. [DOI] [PubMed] [Google Scholar]
- 31.Shin J, McCombs JS, Sanchez RJ, Udall M, Deminski MC, Cheetham TC. Primary nonadherence to medications in an integrated healthcare setting. Am J Manage Care. 2012;18(8):426–434. [PubMed] [Google Scholar]
- 32.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lin EH, Von Korff M, Ciechanowski P, et al. Treatment adjustment and medication adherence for complex patients with diabetes, heart disease, and depression: a randomized controlled trial. Ann Fam Med. 2012;10(1):6–14. doi: 10.1370/afm.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DeWalt D, Callahan L, Hawk V, et al. Health literacy universal precautions toolkit (Prepared by North Carolina Network Consortium, The Cecil G. Sheps Center for Health Services Research, The University of North Carolina at Chapel Hill, under Contract No. HHSA290200710014.) AHRQ Publication No. 10-0046-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2010.
- 35.Koh HK, Brach C, Harris LM, Parchman ML. A proposed ‘health literate care model’ would constitute a systems approach to improving patients’ engagement in care. Health Aff (Millwood) 2013;32(2):357–367. doi: 10.1377/hlthaff.2012.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brach C, Keller D, Hernandez L, et al. Ten Attributes of Health Literate Health Care Organizations: National Academy of Sciences; 2012: http://iom.edu/~/media/Files/Perspectives-Files/2012/Discussion-Papers/BPH_Ten_HLit_Attributes.pdf. Accessed October 3, 2014.