Abstract
Introduction: Many of highly-alkaline dental materials have some adverse effects on physical properties of dentin. As basic substances, mineral trioxide aggregate (MTA), calcium hydroxide (CH) and the new endodontic material, calcium-enriched mixture (CEM) cement, may adversely affect dentin. The purpose of this in vitro study was to evaluate the effect of long-term application of CEM cement, MTA and CH on flexural strength of bovine dentin. Materials and Methods: Three hundred and twenty bovine dentin samples were divided into 4 groups, which were either exposed to CEM cement, CH, MTA or normal saline (control group). Samples of each group were divided into 4 subgroups which were tested by means of Instron Universal Testing Machine for periods of 7, 30, 180 and 365 days after exposure to the test materials. The required force for sample breakage was recorded. The data were analyzed by the two-way ANOVA and Tukey tests. Results: The mean value of forces to break the samples in CEM cement and CH groups was significantly lower than the control group after 1 month (P<0.05). After 180 days, the samples of CEM cement group retrieved their strength but in MTA and CH groups the time interval weakened the samples. After one year of exposure to CH and MTA, flexural strength of the dentin reduced to 72% and 38.7%, respectively (P<0.05). Yet the flexural strength of samples in CEM cement group did not change significantly compared to control group. Conclusion: Following 365 days of application of experimental materials to bovine dentin, the CEM cement showed an interesting result and the samples in this group reached their initial strength during the first week of the study but the other materials caused a reduction in dentin strength at the end of the study.
Key Words: Calcium-Enriched Mixture Cement, Calcium Hydroxide, CEM, Flexural Strength, Fracture Resistance, Mineral Trioxide Aggregate, MTA, Root Canal Filling Materials
Introduction
Root canal treatment (RCT) is a common dental procedure to retain teeth with necrotic or infected pulps. One of the most common clinical problems affecting the endodontically treated teeth is fracture, which can potentially lead to tooth extraction [1]. Loss of tooth structure due to reparation of the access cavity and caries removal, make these teeth more susceptible to fracture [2, 3].
Irrigants, medicaments or root canal filling materials may also affect the mechanical properties of dentin and make it more fragile [4]. Some materials can cause dentin erosion and softening during endodontic treatment. These changes make the dentin and root structure more vulnerable to fracture [5, 6].
Since its introduction to dentistry by Hermann in 1920, calcium hydroxide (CH) has been commonly used as an intra-canal inter-appointment medicament. Various biological properties have been attributed to this substance, such as antimicrobial activity, tissue-dissolving ability, inhibition of tooth resorption, and induction of hard tissue formation [7]. In aqueous solution, CH releases hydroxyl ions and produces a pH of 12.4, which is the antibacterial mechanism of this biomaterial [8]. Researchers found that using CH as an intra-canal medicament can weaken the dentin compared to non treated teeth. They suggested that CH may affect the dentin structure by reducing its organic component, which may influence the mechanical properties of dentin [9-11].
Mineral trioxide aggregate (MTA) was first introduced in 1993 and was approved for endodontic application in 1998 [12, 13]. Portland cement is the major component of MTA and bismuth oxide has been added for its radiopacity [14]. MTA produces an initial pH of 10.2, which rises to 12.5 during the next three hours [15]. MTA is used as a material for root-end filling, direct pulp capping, repair of root and furcation perforations, and also apexification [16]. MTA has also shown a weakening effect on dentin, probably due to breakdown of the protein structure, caused by its alkalinity [17].
A new endodontic cement, named calcium-enriched mixture (CEM) cement, has been recently developed with different chemical composition from MTA but with similar clinical applications. This material can produce hydroxyapatite crystals from endogenous and exogenous ions sources. This cement has the similar biocompatibility to that of MTA, with more efficient properties such as good handling characteristics, shorter setting time, and no tooth staining [18]. CEM cement has acceptable film thickness, flow and sealing ability compared to MTA [19, 20]. Also, it has lower cytotoxicity on different cell lines [21, 22]. The antibacterial effect of CEM cement is comparable to CH and greater than MTA [23]. CEM cement produces favorable results when used as a root-end filling material [24] and a pulp capping agent in primary and permanent teeth [25, 26]. It appears that CEM cement can be used as a pulpotomy material in permanent teeth with open apices [27] and also in mature and primary teeth [28, 29]. This cement can be used for management of internal root resorption and repair of furcal perforation [30, 31].
As this material is used for endodontic treatment, the effect of CEM cement on the mechanical properties of teeth substrates during its application could help clinicians improve their clinical procedure. The aim of this in vitro study was to evaluate the effect of CH, MTA and CEM cement on the flexural strength of standardized dentin bars during different time periods.
Methods and Materials
The dentin specimens were prepared as originally described by Haapasalo and Ørstavik [32]. Intact bovine incisors were used for this experiment. Less than one week prior to commencing the study, the teeth were kept in physiologic saline to prevent their dehydration. The apical 5-mm and two-thirds of the crowns were removed with a water-cooled, high-speed diamond bur (D&Z, Wiesbaden, Germany). Samples were embedded in a self-cure acrylic resin, and a 3.5-mm diameter twist drill was used parallel to the long axis of root canal to widen the canal. Symmetrical cylinders of dentin with outer and inner diameter of approximately 6- and 3.5-mm, respectively and with length of 15-mm was prepared with this method. These cylinders were cut lengthwise into four symmetrical pieces using a diamond disk (Leco, St. Joseph, MI, USA).
A cross-section cut was made in order to prepare four 10-mm-long pieces. All sections were then weighted on a Mettler balance (Mettler Instrument Company, Hightstown, NJ, U.S.A.) to verify similarity of slices for use in this study. Samples that were out of the normal range were discarded. The remaining samples (n=320) were randomly divided to 16 groups with 20 samples each. The samples were placed into the Petri dishes and on the surfaces of test materials with their dentinal side in contact with the material, as follows:
Four Petri dishes containing a 2-mm-thick bulk of CH [calcium hydroxide powder (Merck, Darmstadt, Germany)] which was mixed with distilled water to make a creamy paste.
Four Petri dishes containing 2-mm-thick bulk of CEM cement (BioniqueDent, Tehran, Iran) which was prepared according to the manufacturer instructions.
Four Petri dishes containing 2-mm-thick bulk of MTA (Angelus, Lodrina, Brazil) which was also prepared according to the instructions provided by the manufacturer.
Four Petri dishes containing physiologic saline with 2-mm depth. This group was considered as a negative control group.
The samples remained in the dishes for 7, and 30, 180 and 365 days. Distilled water was added to the Petri dishes every 3 to 4 days as needed to maintain their moisture. All Petri dishes were stored at 37° C and 100% humidity.
Upon completion of each time period, each sample was rinsed with tap water. The dentin bars were subjected to the three-point bend test, using an Instron Universal Testing Machine (Z010, Zwick GmbH, Ulm, Germany). Each bar was loaded at the mid-point through the loading head and shaft. The loaded testing machine was set at a speed of 1 mm/min. The required force for breaking each sample was recorded in MPa.
Statistical analysis
The raw data were tabulated and the means and standard deviation was calculated for each group. The results were analyzed using the two-way ANOVA with material type and time, as two factors, and flexural strength as a response variable. If a significant interaction was identified, the one-way ANOVA test was performed for each time-duration. Data were analyzed using the one-way ANOVA test for comparison of the groups as a whole, and the Tukey’s post-hoc test was used to compare the groups with each other. Statistical calculations were performed with the SPSS software (SPSS INC., Chicago, IL, USA, version 16). A P-value less than 0.05 was considered statistically significant.
Results
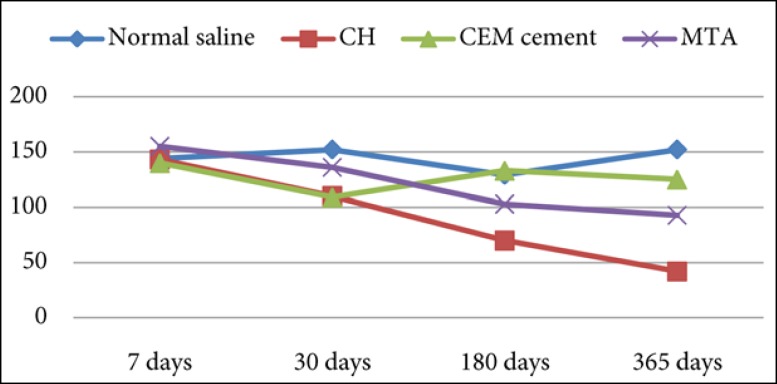
Table 1 and Figure 1 summarize the result of the fracture strength testing. The force required to fracture dentin samples in each group was different, depending on time interval.
Table 1.
Mean (SD) of flexural strength in 16 groups
| Time | Normal Saline | CH | MTA | CEM |
|---|---|---|---|---|
| 7 days | 144.6 (35.5) | 143.6 (36.5) | 155.7 (56) | 140.6 (48.9) |
| 30 days | 152.9 (52.4) | 110.7 (38.8) | 136.2 (34.2) | 109.07 (33.4) |
| 180 days | 129.2 (54.2) | 70.8 (24.5) | 103.8 (38.8) | 133.7 (49) |
| 365 days | 152.8 (60.1) | 42.2 (13.9) | 93.6 (37) | 125 (38.5) |
Figure 1.
Flexural strength means (MPa) for each group
The materials were compared with each other at four time periods: 7, 30, 180 and 365 days. The differences between the amounts of fracture load was not statistically significant for any of the 7-day specimens (P>0.05).
There was a significant reduction in flexural strength in CEM cement and CH groups after 30 days in comparison with normal saline group, which was 28% and 27.5%, respectively (P<0.05).
The decrease in mean value of flexural strength after 180 days in CH and MTA groups was more than 45% and 19%, respectively (P<0.05). Samples in CEM group retrieved their strength after 180 days and reached the strength amount slightly more than normal saline group.
After 365 days of exposure to CH and MTA, flexural strength of the dentin reduced to 72% and 38.7% ,respectively (P<0.05), but the flexural strength of samples in CEM cement group did not change significantly in comparison with the control group. The reduction of flexural strength in dentin bars in CEM group was less than MTA without any significant differences (P>0.05).
Discussion
This study revealed the alteration of dentin physical properties after 30-day exposure to CH, MTA and CEM cement. All the samples showed a decrease in their strength in comparison with normal saline group. This finding is in agreement with the other studies that applied these materials on dentin surfaces for ±30 days [11, 33-35].
The current study used bovine incisors since they were easy to obtain in a good condition and showed less variability in comparison with human teeth [36]. No significant differences were found in diffusion rates of CH paste in human and bovine teeth [37]. Although bovine and human teeth have some differences in their morphology, several studies have demonstrated similarities between their substrates. Sano et al. [38] showed the same ultimate tensile strength and modulus of elasticity (MOE) between human and bovine dentin. Moreover, other studies have also reported similar results in bonding tests and the number and distribution of dentinal tubules between bovine and human dentin [33, 36, 39]. Above all, bovine incisors show less variation in anatomical morphology than human teeth. Therefore, bovine teeth provide a standard and reproducible material that allows evaluation of different treatment modalities for management of this clinical situation.
Several studies have indicated that CH has a weakening effect on dentin [11, 17, 34, 35, 40], but such studies on the effect(s) of MTA on fracture resistance of teeth have reported contradictory results. The results of this study is not in agreement with those of Bortoluzzi et al. [41], Hatibovic-Kofman et al. [42] and Milani et al. [43], who found a significant increase in fracture strength of dentin when the teeth were filled with MTA. It seems that the main reason for this difference is in methodology of these studies. Those studies did not evaluate the pure effect of experimental materials on dentin strength, because the force was applied on root-canal filled teeth while in this study, the load was applied on dentin bars.
A finite element analysis showed that the materials with similar MOE to dentin could reinforce the weak roots [44], also Cauwels et al. [45] showed that the samples obturated with gutta-percha, MTA and calcium-phosphate bone cement (CPC) had a significantly higher fracture resistance compared to unfilled samples. In our study, the samples were rinsed before testing to remove the remnants of experimental materials from dentin bars and also the force was applied on the standard dentin samples instead of root canal filled roots. Furthermore, they applied parallel forces or forces with 135° angulation to the long axis of the tooth on the incisal edge but in the present study, 3-point bending load was applied on dentin bars. Methodology of this study was almost similar to the studies by White et al. [17] and Sahebi et al. [35]. Both of them showed that MTA decreased dentin strength.
The weakening effect of CH, CEM cement and MTA observed in this study maybe due to the break-down of protein structures caused by the alkalinity of the used materials. Previous studies have also reported that materials with high alkalinity can cause conformational changes in protein structure [17].
This study showed that after 365 days of exposure to CH and MTA, the samples become more fragile, but surprisingly the samples which were exposed to CEM cement almost retrieved their initial strength after six months of exposure and maintained their flexural strength till the end of the study.
This behavior of CEM cement, despite the fact that its initial pH is comparable to that of CH and MTA, is unclear but may be explained by the pH changes during the long-term contact of samples with CEM cement compared to CH and MTA. The pH changes of CEM cement during one month has been investigated in one study [46], but there is no available study regarding the alteration of pH caused by CEM cement in long-term studies. It seems that further studies are needed for better understanding of this phenomenon.
Conclusion
In conclusion, it is highly probable that alkaline endodontic materials reduce the mechanical properties of root dentin; however CEM cement may be the most favorable biomaterial in this regard as it does not negatively affect the dentinal strength.
Acknowledgment
The authors would like to thank the Vice-Chancellery of Shiraz University of Medical Sciences for supporting this research (Grant no. 3697). This manuscript is based on the thesis by Dr. Davoud Jamshidi. The authors also thank Dr. Bijan Noori from the Center of Research Improvement, school of the Dentistry, for statistical analysis.
Conflict of Interest: ‘None declared’.
References
- 1.Driscoll CO, Dowker SEP, Anderson P, Wilson RM, Gulabivala K. Effects of sodium hypochlorite solution on root dentine composition. J Mater Sci Mater Med. 2002;13(2):219–23. doi: 10.1023/a:1013894432622. [DOI] [PubMed] [Google Scholar]
- 2.Blaser PK, Lund MR, Cochran MA, Potter RH. Effect of designs of Class 2 preparations on resistance of teeth to fracture. Oper Dent. 1983;8(1):6–10. [PubMed] [Google Scholar]
- 3.Hood JA. Biomechanics of the intact, prepared and restored tooth: Some clinical implications. Int Dent J. 1991;41(1):25–32. [PubMed] [Google Scholar]
- 4.Soares CJ, Santana FR, Silva NR, Preira JC, Pereira CA. Influence of the endodontic treatment on mechanical properties of root dentin. J Endod. 2007;33(5):603–6. doi: 10.1016/j.joen.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 5.Hülsmann M, Heckendorff M, Lennon A. Chelating agents in root canal treatment: mode of action and indications for their use. Int Endod J. 2003;36(12):810–30. doi: 10.1111/j.1365-2591.2003.00754.x. [DOI] [PubMed] [Google Scholar]
- 6.Hargreaves KM, Cohen S. Pathways of the pulp. 10thEdition. St Louis: CV : Mosby; 2011. p. 253. [Google Scholar]
- 7.Siqueira JF, Lopes HP. Mechanisms of antimicrobial activity of calcium hydroxide: a critical review. Int Endod J. 1999;32(5):361–69. doi: 10.1046/j.1365-2591.1999.00275.x. [DOI] [PubMed] [Google Scholar]
- 8.Kawamoto R, Kurokawa H, Takubo C, Shimamura Y, Yoshida T, Miyazaki M. Change in elastic modulus of bovine dentine with exposure to a calcium hydroxide paste. J Dent. 2008;36(11):959–64. doi: 10.1016/j.jdent.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dental Traumatology. 2002;18(3):134–37. doi: 10.1034/j.1600-9657.2002.00097.x. [DOI] [PubMed] [Google Scholar]
- 10.Doyon GE, Dumsha T, von Fraunhofer JA. Fracture resistance of human root dentin exposed to intracanal calcium hydroxide. J Endod. 2005;31(12):895–7. doi: 10.1097/01.don.0000194542.02521.af. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg B, Murray PE, Namerow K. The effect of calcium hydroxide root filling on dentin fracture strength. Dent Traumatol. 2007;23(1):26–9. doi: 10.1111/j.1600-9657.2006.00453.x. [DOI] [PubMed] [Google Scholar]
- 12.Lee SJ, Monsef M, Torabinejad M. Sealing ability of a mineral trioxide aggregate for repair of lateral root perforations. J Endod. 1993;19(11):541–4. doi: 10.1016/S0099-2399(06)81282-3. [DOI] [PubMed] [Google Scholar]
- 13.Schmitt DD, Bogen G. Multifaceted use of ProRootTM MTA root canal repair material. Pediatr Dent. 2001;23(4):326–30. [PubMed] [Google Scholar]
- 14.Roberts HW, Toth JM, Berzins DW, Charlton DG. Mineral trioxide aggregate material use in endodontic treatment: a review of the literature. Dent Mater. 2008;24(2):149–64. doi: 10.1016/j.dental.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new root-end filling material. J Endod. 1995;21(7):349–53. doi: 10.1016/S0099-2399(06)80967-2. [DOI] [PubMed] [Google Scholar]
- 16.Sarkar NK, Caicedo R, Ritwik P, Moiseyeva R, Kawashima I. Physicochemical basis of the biologic properties of mineral trioxide aggregate. J Endod. 2005;31(2):97–100. doi: 10.1097/01.don.0000133155.04468.41. [DOI] [PubMed] [Google Scholar]
- 17.White JD, Lacefield WR, Chavers LS, Eleazer PD. The effect of three commonly used endodontic materials on the strength and hardness of root dentin. J Endod. 2002;28(12):828–30. doi: 10.1097/00004770-200212000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Asgary S, Shahabi S, Jafarzadeh T, Amini S, Kheirieh S. The properties of a new endodontic material. J Endod. 2008;34(8):990–3. doi: 10.1016/j.joen.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 19.Asgary S, Eghbal MJ, Parirokh M, Ghanavati F, Rahimi H. A comparative study of histologic response to different pulp capping materials and a novel endodontic cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(4):609–14. doi: 10.1016/j.tripleo.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 20.Asgary S, Eghbal MJ, Parirokh M. Sealing ability of a novel endodontic cement as a root-end filling material. J Biomed Mater Res A. 2008;87(3):706–9. doi: 10.1002/jbm.a.31678. [DOI] [PubMed] [Google Scholar]
- 21.Mozayeni MA, Milani AS, Marvasti LA, Asgary S. Cytotoxicity of calcium enriched mixture cement compared with mineral trioxide aggregate and intermediate restorative material. Aust Endod J. 2012;38(2):70–5. doi: 10.1111/j.1747-4477.2010.00269.x. [DOI] [PubMed] [Google Scholar]
- 22.Asgary S, Moosavi SH, Yadegari Z, Shahriari S. Cytotoxic effect of MTA and CEM cement in human gingival fibroblast cells. Scanning electronic microscope evaluation. N Y State Dent J. 2012;78(2):51–4. [PubMed] [Google Scholar]
- 23.Asgary S, Kamrani FA. Antibacterial effects of five different root canal sealing materials. J Oral Sci. 2008;50(4):469–74. doi: 10.2334/josnusd.50.469. [DOI] [PubMed] [Google Scholar]
- 24.Asgary S, Eghbal MJ, Ehsani S. Periradicular regeneration after endodontic surgery with calcium-enriched mixture cement in dogs. J Endod. 2010;36(5):837–41. doi: 10.1016/j.joen.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Fallahinejad Ghajari M, Asgharian Jeddi T, Iri S, Asgary S. Direct pulp-capping with calcium enriched mixture in primary molar teeth: a randomized clinical trial. Iran Endod J. 2010;5(1):27–30. [PMC free article] [PubMed] [Google Scholar]
- 26.Zarrabi MH, Javidi M, Jafarian AH, Joushan B. Histologic assessment of human pulp response to capping with mineral trioxide aggregate and a novel endodontic cement. J Endod. 2010;36(11):1778–81. doi: 10.1016/j.joen.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 27.Nosrat A, Seifi A, Asgary S. Pulpotomy in caries-exposed immature permanent molars using calcium-enriched mixture cement or mineral trioxide aggregate: a randomized clinical trial. Int J Paediatr Dent. 2013;23(1):56–63. doi: 10.1111/j.1365-263X.2012.01224.x. [DOI] [PubMed] [Google Scholar]
- 28.Asgary S, Eghbal MJ. Treatment outcomes of pulpotomy in permanent molars with irreversible pulpitis using biomaterials: A multi-center randomized controlled trial. Acta Odontol Scand. 2013;71(1):130–36. doi: 10.3109/00016357.2011.654251. [DOI] [PubMed] [Google Scholar]
- 29.Malekafzali B, Shekarchi F, Asgary S. Treatment outcomes of pulpotomy in primary molars using two endodontic biomaterials A 2-year randomised clinical trial. Eur J Paediatr Dent. 2011;12(3):189–93. [PubMed] [Google Scholar]
- 30.Asgary S, Ehsani S. Permanent molar pulpotomy with a new endodontic cement: A case series. J Conserv Dent. 2009;12(1):31–6. doi: 10.4103/0972-0707.53340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Samiee M, Eghbal MJ, Parirokh M, Abbas FM, Asgary S. Repair of furcal perforation using a new endodontic cement. Clin Oral Investig. 2010;14(6):653–58. doi: 10.1007/s00784-009-0351-8. [DOI] [PubMed] [Google Scholar]
- 32.Haapasalo M, Orstavik D. In vitro infection and disinfection of dentinal tubules. J Dent Res. 1987;66(8):1375–9. doi: 10.1177/00220345870660081801. [DOI] [PubMed] [Google Scholar]
- 33.Schilke R, Lisson JA, Bauß O, Geurtsen W. Comparison of the number and diameter of dentinal tubules in human and bovine dentine by scanning electron microscopic investigation. Arch Oral Biol. 2000;45(5):355–61. doi: 10.1016/s0003-9969(00)00006-6. [DOI] [PubMed] [Google Scholar]
- 34.Sahebi S, Moazami F, Abbott P. The effects of short-term calcium hydroxide application on the strength of dentine. Dent Traumatol. 2010;26(1):43–6. doi: 10.1111/j.1600-9657.2009.00834.x. [DOI] [PubMed] [Google Scholar]
- 35.Sahebi S, Nabavizadeh M, Dolatkhah V, Jamshidi D. Short term effect of calcium hydroxide, mineral trioxide aggregate and calcium-enriched mixture cement on the strength of bovine root dentin. Iran Endod J. 2012;7(2):68–73. [PMC free article] [PubMed] [Google Scholar]
- 36.Yassen GH, Platt JA, Hara AT. Bovine teeth as substitute for human teeth in dental research: a review of literature. J Oral Sci. 2011;53(3):273–82. doi: 10.2334/josnusd.53.273. [DOI] [PubMed] [Google Scholar]
- 37.Camargo CHR, Bernardineli N, Valera MC, De Carvalho CAT, De Oliveira LD, Menezes MM, Afonso SE, Mancini MNG. Vehicle influence on calcium hydroxide pastes diffusion in human and bovine teeth. Dent Traumatol. 2006;22(6):302–6. doi: 10.1111/j.1600-9657.2005.00326.x. [DOI] [PubMed] [Google Scholar]
- 38.Sano H, Ciucchi B, Matthews WG, Pashley DH. Tensile properties of mineralized and demineralized human and bovine dentin. J Dent Res. 1994;73(6):1205–11. doi: 10.1177/00220345940730061201. [DOI] [PubMed] [Google Scholar]
- 39.Ruse ND, Smith DC. Adhesion to bovine dentin--surface characterization. J Dent Res. 1991;70(6):1002–8. doi: 10.1177/00220345910700060101. [DOI] [PubMed] [Google Scholar]
- 40.Andreasen JO, Munksgaard EC, Bakland LK. Comparison of fracture resistance in root canals of immature sheep teeth after filling with calcium hydroxide or MTA. Dent Traumatol. 2006;22(3):154–6. doi: 10.1111/j.1600-9657.2006.00419.x. [DOI] [PubMed] [Google Scholar]
- 41.Bortoluzzi EA, Souza EM, Reis JMSN, Esberard RM, Tanomaru-Filho M. Fracture strength of bovine incisors after intra-radicular treatment with MTA in an experimental immature tooth model. Int Endod J. 2007;40(9):684–91. doi: 10.1111/j.1365-2591.2007.01266.x. [DOI] [PubMed] [Google Scholar]
- 42.Hatibović-Kofman S, Raimundo L, Zheng L, Chong L, Friedman M, Andreasen JO. Fracture resistance and histological findings of immature teeth treated with mineral trioxide aggregate. Dent Traumatol. 2008;24(3):272–76. doi: 10.1111/j.1600-9657.2007.00541.x. [DOI] [PubMed] [Google Scholar]
- 43.Milani AS, Rahimi S, Borna Z, Jafarabadi MA, Bahari M, Deljavan AS. Fracture resistance of immature teeth filled with mineral trioxide aggregate or calcium-enriched mixture cement: An ex vivo study. Dent Res J (Isfahan) 2012;9(3):299–304. [PMC free article] [PubMed] [Google Scholar]
- 44.Li LL, Wang ZY, Bai ZC, Mao Y, Gao B, Xin HT, Zhou B, Zhang Y, Liu B. Three-dimensional finite element analysis of weakened roots restored with different cements in combination with titanium alloy posts. Chin Med J (Engl) 2006;119(4):305–11. [PubMed] [Google Scholar]
- 45.Cauwels RGEC, Pieters IY, Martens LC, Verbeeck RMH. Fracture resistance and reinforcement of immature roots with gutta percha, mineral trioxide aggregate and calcium phosphate bone cement: a standardized in vitro model. Dent Traumatol. 2010;26(2):137–42. doi: 10.1111/j.1600-9657.2010.00869.x. [DOI] [PubMed] [Google Scholar]
- 46.Amini Ghazvini S, Abdo Tabrizi M, Kobarfard F, Akbarzadeh Baghban A, Asgary S. Ion release and pH of a new endodontic cement, MTA and Portland cement. Iran Endod J. 2009;4(2):74–8. [PMC free article] [PubMed] [Google Scholar]