Abstract
Objective
In this study, we examined whether the benefits of spousal assistance for patient well-being and physical functioning depend on the fit between amount of assistance provided and the personal importance of completing activities independently.
Methods
Individuals with osteoarthritis of the hip or knee were assessed for independence centrality, depressive symptoms, self-efficacy for managing pain, and physical functioning (N = 159 to 230). Spouses reported the amount of support provided with daily tasks.
Results
As predicted, moderation analyses indicated that spousal support was associated with greater self-efficacy for managing pain in patients with low independence centrality, but was not associated with self-efficacy in patients with high independence centrality. Also consistent with our hypotheses, spousal support was associated with greater depressive symptoms and slower walk time in patients with high independence centrality, but there were no effects of spouse support on these outcomes for patients with low independence centrality.
Conclusions
Our findings demonstrate the implications of miscarried spousal support for patient well-being and physical functioning, and they suggest a means of tailoring couple-oriented interventions for chronic illness.
Keywords: spousal support, chronic illness, independence, physical functioning
Chronic illnesses account for more than 75% of medical care costs in the United States (National Center for Health Statistics, 2010). Close family members are a critical source of emotional support and assistance to chronically ill individuals; however, their attempts to help do not always promote adaptive functioning (Martire & Schulz, 2001). In this study we examined whether the benefits of spouse assistance for patients’ psychological well-being and physical functioning depend on the fit between amount of assistance provided and the personal importance (i.e., centrality) of completing activities independently.
Support in the form of assistance with daily activities may backfire and have negative effects (Burg & Seeman, 1994). Several studies have shown that high levels of support are associated with more depressive symptoms, even after controlling for the effects of illness-related factors (Silverstein, Chen, & Heller, 1996). Miscarried support also seems to have implications for physical health. Assistance with tasks has been linked with an increased risk for new or recurrent physical disability (Seeman, Bruce, & McAvay, 1996). In addition, individuals with chronic pain exhibit more pain behaviors and become less active when their family members provide unnecessary assistance (e.g., Romano et al., 1992). An important but unanswered question is, what are the conditions under which these negative effects are most likely to occur?
There is converging evidence that the personal centrality of functional independence (i.e., carrying out activities on one’s own) plays a role in negative reactions to support. Early experimental studies showed that individuals who receive assistance in a domain that is highly central to them respond with more negative emotions than those for whom the task is not highly central (e.g., DePaulo, Brittingham, & Kaiser, 1983). Research on rheumatoid arthritis indicates that patients who appraise this illness as a challenge (rather than a threat) have poorer well-being when they receive high levels of instrumental, emotional, and informational support from their husband (Schiaffino & Revenson, 1995). Our own previous arthritis research showed that female patients with low independence centrality had less negative self-evaluations in response to more assistance from their husband (Martire, Stephens, Druley, & Wojno, 2002).
Research emerging from Self-Determination Theory (SDT) has addressed this issue in a somewhat different manner, by examining the effects of autonomy support on individuals who are faced with managing illness and making lifestyle changes (e.g., smoking cessation, weight loss). Autonomy support refers to behaviors that are characterized by warmth, empathy, and understanding for an individual’s situation; patient-centered communication; and the provision of choices for making health behavior changes. Individuals with Type 2 diabetes whose health care providers are more supportive of their autonomy feel that they are better able to regulate their blood glucose, and subsequently show improved glucose control over 1 year (Williams, Freedman, & Deci, 1998). In addition, nursing home residents report greater life satisfaction when they receive autonomy support from family members and nursing home staff (Kasser & Ryan, 1999).
According to SDT, autonomy is a universal need that individuals have across a multitude of life domains. In contrast, the importance of being functionally independent is circumscribed to one domain and likely to vary more across individuals. That is, there are likely to be individuals for whom functional independence is not highly central and who are relatively comfortable with assistance received as a result of illness, and there are other individuals who are distressed by being dependent on others. In the current study we examined the fit between amount of spousal assistance and independence centrality among individuals who experience disability from hip or knee osteoarthritis (OA), focusing on the consequences of fit for psychological well-being and physical functioning. Our hypothesis was that higher levels of assistance from the spouse would be related to poorer well-being and functioning among those patients with high independence centrality (i.e., centrality would act as a moderator). Conversely, it was expected that more assistance would be related to better well-being and functioning among patients who ascribe less importance to being independent.
Method
Participants
For this study we used baseline data from patients and their spouses who were participating in a psychosocial intervention study for OA. Participants were recruited through the University of Pittsburgh Medical Center. To be eligible for the study, individuals with arthritis had to be 50 years of age or older, married, and diagnosed with hip or knee OA. Additional criteria were that the individual had experienced pain of at least moderate intensity on most days over the past month, had difficulty with at least one instrumental activity of daily living (IADL; e.g., household tasks, driving), and received assistance from the spouse with at least one IADL.
Of the 1,145 patients who were interested in participating and screened for eligibility, 262 were eligible and 883 were ineligible. The most common reason for ineligibility was that the patient was unmarried or not living with the spouse (n = 420, or 48% of those who were ineligible). Well-being measures were collected during an in-home interview or by mailed questionnaire, and physical functioning was assessed at the University of Pittsburgh Medical Center. The number of couples with data for the outcome variables was 230 (self-efficacy, depressive symptoms), 190 (timed walk), and 159 (timed chair rises).
Patients’ average age was 69 years (SD = 7.8; range = 50–87), and spouses’ average age was 70 years (SD = 8.3; range = 47–90). Approximately 72% of patients were female, and couples had been married for an average of 41.2 years (SD = 13.0). A total of 90% of the sample was Caucasian and 8% was African American. Approximately half of the sample had education beyond high school. Current household income was $40,000–49,999, on average.
Measures
Spousal Instrumental Support
Spouses were asked to indicate the frequency with which they assisted patients with four IADLs during the past month due to arthritis (i.e., shopping for groceries, preparing meals, laundry, and other household activities), on a scale ranging from 1 (never) to 6 (several times a day) (M = 13.7; SD = 3.8; range = 4–24). Cronbach’s alpha for this measure was .61. Female spouses reported providing more support than male spouses (M = 14.9 vs. 13.1, respectively; p < .001).
Independence Centrality
Patients responded to eight statements regarding the personal centrality of completing four IADLs with minimum assistance from others (see above), on a scale from 1 (strongly disagree) to 4 (strongly agree) (Martire et al., 2002). Examples of items from this scale include “Being able to do these activities on your own is very important to you,” and “Having to rely on others for help with these activities does not bother you” (reverse coded) (M = 23.4; SD = 3.8, range = 10–32). Cronbach’s alpha was .70. There was no gender difference in independence centrality.
Psychological Well-Being
Self-efficacy for managing pain
Using the five-item pain subscale of the Arthritis Self-Efficacy scale (Lorig, Chastain, Ung, Shoor, & Holman, 1989), patients rated their confidence in managing their arthritis pain on a scale from 1 (not at all confident) to 10 (totally confident) (M = 32.8; SD = 9.7, range = 9–50). Cronbach’s alpha was .77.
Depressive symptoms
Depressive symptoms during the past week were assessed with a 10-item version of the Centers for Epidemiologic Studies—Depression scale (CES–D) (Andresen, Malmgren, Carter, & Patrick, 1994; Radloff, 1977). Patients reported how often they experienced specific symptoms during the past week, on a scale from 0 (rarely or none of the time) to 3 (most of the time), yielding a range of 0 to 30 (M = 6.6; SD = 4.8, range = 0–26) and Cronbach’s alpha was .74. Approximately 22% of patients scored at or above a score of 10, which is considered at risk for depression on the 10-item version of the CES–D.
Physical Functioning
We used two standardized measures of mobility and lower body strength commonly administered in epidemiologic studies of older adults (Guralnik, Ferrucci, Simonsick, Salive, & Wallace, 1995). Assessments were carried out at a medical center by a trained interviewer.
Timed walk
Patients were asked to walk to the end of a preset distance of 8 feet, at their normal walking speed. Patients were timed and the faster of two walks was recorded. The average time to complete this test was 4.8 seconds (SD = 2.3; range = 2.1–22.0).
Timed chair rises
Patients were asked to fold their arms across their chests and to stand from a sitting position once; if they successfully rose from the chair, they were asked to stand up and sit down five times as quickly as possible. The timed task consisted of the five chair rises, and patients were timed from the first of these sittings to the final standing position. The average time to complete this test was 17.7 seconds (SD = 6.8; range = 4.9–50.2).
Analysis Plan
Regression analyses were conducted for each of the dependent variables. All analyses included four covariates that are often associated with arthritis patient well-being and functioning—OA severity (assessed with the Western Ontario and McMaster University Osteoarthritis Index; Bellamy, Buchanan, Goldsmith, Campbell, & Stitt, 1988); patient marital satisfaction (assessed with the Marital Adjustment Test; Locke & Wallace, 1959); patient gender; and household income. Covariates were entered into the first block of each analysis along with support and independence centrality. An interaction term representing the product of spousal support and independence centrality was entered into the second and final block of each analysis. Prior to creating the interaction term, both support and centrality were centered.
A significant R2 change (p < .05) for the interaction term was considered indicative of a moderating effect of independence centrality, and the slope of support on patient outcomes at high and low levels of centrality (1 SD above and below the mean, respectively) was examined using unstandardized regression coefficients (Aiken & West, 1991).
Results
Zero-order correlations among the four dependent variables ranged from r = −.11 (ns) to −.37 (p < .001). Independence centrality was associated with less self-efficacy and more depressive symptoms (r = −.18 and .16, respectively, p < .01), suggesting that ascribing more importance to being independent may be maladaptive for individuals with a disabling chronic illness.
The top half of Table 1 shows that there was a statistically significant interaction between spousal support and patient independence centrality in predicting depressive symptoms (β = .16, p < .01). This effect accounted for 3% of the variance in depressive symptoms, a relatively strong moderation effect in field research. Figure 1 shows that the slope of depressive symptoms on spousal support was significantly different from zero at high centrality, t(226) = 4.38, p < .001. As predicted, among patients who reported high independence centrality, more support was associated with more depressive symptoms, with an average CES–D score of 10.7 for this group (equivalent to a score of approximately 21 on the 20-item CES–D). Patients with low independence centrality experienced fewer depressive symptoms at higher levels of support, but this slope was not statistically significant, t(226) = −1.53, p = .13.
Table 1.
Findings From Regression Analyses for Psychological Well-Being and Physical Functioning
| Pain self-efficacy
|
Depressive symptoms
|
|||||
|---|---|---|---|---|---|---|
| Predictor | B | SE | ß | B | SE | ß |
| Arthritis Severity | −.25 | .04 | −.41*** | .12 | .02 | .38*** |
| Marital Satisfaction | −.01 | .02 | −.02 | −.04 | .01 | −.25*** |
| Gender | −.70 | 1.33 | −.03 | −.81 | .61 | −.08 |
| Household Income | −.39 | .24 | −.10 | −.10 | .11 | −.06 |
| Spousal Support | .21 | .16 | .08 | .10 | .07 | .08 |
| Independence Centrality | −.17 | .16 | −.07 | .06 | .08 | .05 |
| R2 | .18*** | .26*** | ||||
| Support × Centrality | −.09 | .04 | −.13* | .06 | .02 | .16** |
| Total R2 | .20*** | .29*** | ||||
|
| ||||||
| Timed Walk
|
Timed Chair Rises
|
|||||
| Arthritis Severity | .06 | .01 | .38*** | .10 | .04 | .23** |
| Marital Satisfaction | .00 | .01 | −.00 | .03 | .02 | .11 |
| Gender | −.16 | .35 | −.03 | −2.38 | 1.22 | −.15* |
| Household Income | −.03 | .06 | −.03 | −.28 | .21 | −.11 |
| Spousal Support | .07 | .04 | .13+ | .21 | .14 | .12 |
| Independence Centrality | −.03 | .04 | −.04 | .16 | .16 | .08 |
| R2 | .18*** | .13*** | ||||
| Support × Centrality | .02 | .01 | .12+ | −.01 | .04 | −.01 |
| Total R2 | .19*** | .13*** | ||||
Note. N = 230 couples for self-efficacy and depressive symptoms; 190 for the timed walk task and 159 for the chair rise task. Patient gender: 1 = female, 2 = male.
p = .08.
p < .05.
p < .01.
Figure 1.
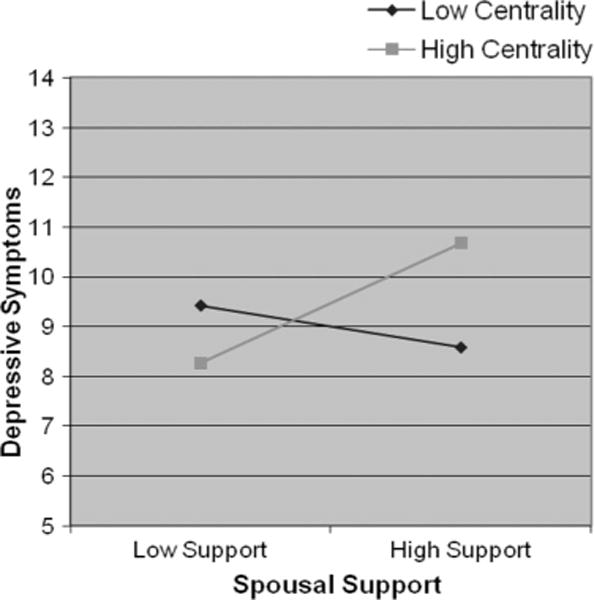
The moderating effect of independence centrality for the outcome of patient depressive symptoms (10-item CES–D; range = 0–30). The high centrality slope is significant whereas the low centrality slope is not.
Analyses also revealed a significant interaction between spousal support and patient independence centrality in the prediction of self-efficacy (β = −.13, p < .05). The slope of self-efficacy on support was significantly different from zero at low centrality, t(226) = 2.52, p < .01 but not at high centrality, t(226) = −.49. Consistent with our prediction, more spousal support was associated with greater self-efficacy in patients with low independence centrality (see Figure 2).
Figure 2.
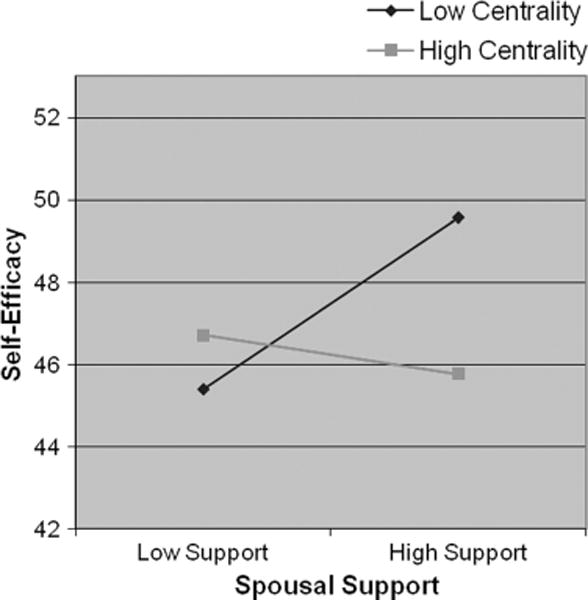
The moderating effect of independence centrality for the outcome of patient self-efficacy. The low centrality slope is significant whereas the high centrality slope is not.
The bottom half of Table 1 shows that, contrary to prediction, independence centrality did not moderate the effects of support on patients’ speed in completing the chair rise task. However, there was a trend level interaction between support and centrality for the timed walk (β = .12, p = .08). As predicted, patients who reported high independence centrality and who received more spousal support took longer to complete the timed walk, t(186) = 2.82, p < .01, whereas the slope at low centrality was not significant, t(186) = −.05.
Discussion
Consistent with our hypothesis, arthritis patients felt more efficacious in managing their pain when receiving more spousal help if independence in doing activities was less central. In contrast, patients with high independence centrality appeared to have more depressive symptoms and poorer physical functioning when receiving more spousal assistance. These effects were more robust for psychological than physical functioning outcomes, suggesting that the primary consequences of this mismatch are psychological. Over time, we would expect the psychological effects to increasingly manifest as behavioral effects that undermine physical functioning. Our findings extend prior literature by demonstrating the implications of miscarried spousal support for patient health and well-being. It is likely that patients with low independence centrality may be more open to receiving help from their spouse than those who prefer to do tasks on their own. Consistent with this idea, a recent review concluded that partners may benefit in a multitude of ways when they work together to manage chronic illness (Berg & Upchurch, 2007).
A limitation of this study is the low internal consistency of the spousal support measure. In addition, it is important to acknowledge that data are cross-sectional. Longitudinal research is needed in order to determine how spouse support and patient independence centrality change over time and subsequently impact patient outcomes. For example, recent research indicates that individuals downgrade the importance of goals in the health domain as a means of protecting themselves from losses in this domain (Rothermund & Brandtstadter, 2003; Wrosch, Schulz, Miller, Lupien, & Dunne, 2007).
The findings of this study suggest interesting avenues for psychosocial or behavioral intervention. Specifically, addressing issues such as preferences for amount and timing of assistance in particular domains may be highly useful in couple-oriented interventions for chronic illness (Martire, Schulz, Helgeson, Small, & Saghafi, 2010). Moreover, this intervention approach may be optimized by targeting the needs of individual couples in regard to needs for independence and other moderators of the relationship between marriage and health.
Acknowledgments
This research was supported by Grant HL65111-65112 (Pittsburgh Mind-Body Center).
Contributor Information
Lynn M. Martire, Department of Human Development and Family Studies, Penn State University
Mary Ann Parris Stephens, Department of Psychology, Kent State University.
Richard Schulz, Department of Psychiatry and University Center for Social and Urban Research, University of Pittsburgh.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES–D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventive Medicine. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip and knee. Journal of Rheumatology. 1988;15:1833–1840. [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133(6):920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Burg MM, Seeman TE. Families and health: The negative side of social ties. Annals of Behavioral Medicine. 1994;16(2):109–115. [Google Scholar]
- DePaulo BM, Brittingham GL, Kaiser MK. Receiving competence-relevant help: Effects on reciprocity, affect, and sensitivity to the helper’s nonverbally expressed needs. Journal of Personality and Social Psychology. 1983;45:1045–1060. [Google Scholar]
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. New England Journal of Medicine. 1995;332(9):556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasser VG, Ryan RM. The relation of psychological needs for autonomy and relatedness to vitality, well-being, and mortality in a nursing home. Journal of Applied Social Psychology. 1999;29:935–954. [Google Scholar]
- Locke H, Wallace K. Short marital-adjustment and prediction tests: Their reliability and validity. Marriage and Family Living. 1959;21:251–255. [Google Scholar]
- Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis and Rheumatism. 1989;32(1):37–44. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- Martire LM, Schulz R. Informal caregiving to older adults: Health effects of providing and receiving care. In: Baum A, Revenson T, Singer J, editors. Handbook of health psychology. Mahwah, NJ: Erlbaum; 2001. pp. 477–493. [Google Scholar]
- Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi E. Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine. 2010;40:325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Stephens MAP, Druley JA, Wojno WC. Negative reactions to received spousal care: Predictors and consequences of miscarried support. Health Psychology. 2002;21:167–176. [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2009: With Special Feature on Medical Technology. 2010. [PubMed] [Google Scholar]
- Radloff LS. The CES–D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Romano JM, Turner JA, Friedman LS, Bulcroft RA, Jensen MP, Hops H, Wright SF. Sequential analysis of chronic pain behaviors and spouse responses. Journal of Consulting and Clinical Psychology. 1992;60(5):777–782. doi: 10.1037//0022-006x.60.5.777. [DOI] [PubMed] [Google Scholar]
- Rothermund K, Brandtstadter J. Coping with deficits and losses in later life: From compensatory action to accommodation. Psychology and Aging. 2003;18(4):896–905. doi: 10.1037/0882-7974.18.4.896. [DOI] [PubMed] [Google Scholar]
- Schiaffino KM, Revenson TA. Relative contributions of spousal support and illness appraisals to depressed mood in arthritis patients. Arthritis Care and Research. 1995;8(2):80–87. doi: 10.1002/art.1790080205. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Bruce ML, McAvay GJ. Social network characteristics and onset of ADL disability: MacArthur studies of successful aging. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1996;51(4):S191–200. doi: 10.1093/geronb/51b.4.s191. [DOI] [PubMed] [Google Scholar]
- Silverstein M, Chen X, Heller K. Too much of a good thing? Intergenerational social support and the psychological well-being of older parents. Journal of Marriage and Family. 1996;58:970–982. [Google Scholar]
- Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21(10):1644–1651. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Schulz R, Miller GE, Lupien S, Dunne E. Physical health problems, depressive mood, and cortisol secretion in old age: Buffer effects of health engagement control strategies. Health Psychology. 2007;26(3):341–349. doi: 10.1037/0278-6133.26.3.341. [DOI] [PubMed] [Google Scholar]


