Abstract
Objectives
To assess alcohol-related premature death in people who self-harm compared to the general population, including variation by socioeconomic deprivation.
Design
A retrospective longitudinal cohort analysis from the Multicentre Study of self-harm in England, 1 January 2000 to 31 December 2010, with cause-specific mortality follow-up through to 31 December 2012.
Setting
Six emergency departments in Oxford, Manchester and Derby.
Participants
All individuals aged 15 years or more who presented with self-harm (n = 39,014) to general hospital emergency departments, together with follow-up mortality information from the Data Linkage Service of the Health and Social Care Information Centre.
Main outcome measures
Standardised mortality ratios (observed/expected number of deaths: SMRs) and mean number of years of life lost (YLL) were estimated for alcohol-related mortality. Patients’ characteristics and clinical management following self-harm were also examined.
Results
After 7.5 years’ (median) follow-up, 2695 individuals (6.9%) had died, significantly more males (9.5%) than females (5.0%), including 307 (11.4%) from alcohol-related causes. Alcohol-related death was more frequent than expected in both males (SMR 8.5, 95% CI 7.3 to 9.8) and females (11.6, 9.8 to 13.7), equating to 33.7 YLL (95% CI 32.4 to 35.0) in males and 38.1 YLL (36.6 to 39.6) in females. It was not associated with area-level socioeconomic deprivation. Alcohol-related death was associated with unemployed/sick/disabled status, alcohol use during self-harm, referral to drug/alcohol services and lack of psychosocial assessment following self-harm.
Conclusions
Hospital-presenting self-harm patients should receive assessment following self-ham according to national guidance to enable early identification and treatment of alcohol problems.
Keywords: self-harm, alcohol, alcohol misuse, socio-economic deprivation, mortality follow-up
Introduction
Alcohol misuse is the third leading contributor to the global burden of disease.1 Elevated morbidity and mortality from excessive alcohol consumption is a major public health problem in the UK,2 and elsewhere.1 In England, it is a particular focus of new government initiatives3 and public health strategies to reduce avoidable deaths.4 Alcohol-related deaths in the UK doubled between 1991 and 2004,5 then stabilised during 2002 to 2011, though with persistent geographical differences6 and variation by socioeconomic deprivation.5
Self-harm (SH; intentional self-injury and self-poisoning with or without suicidal intent) is also a major public health problem,7 accounting for approximately 220,000 emergency department (ED) presentations in England annually.8 Alcohol problems occur frequently,9 with half of all SH presentations to EDs involving alcohol,10,11 and a quarter of patients diagnosed with harmful alcohol use.12
Alcohol misuse increases suicide risk in the SH population,13 and contributes to premature mortality from physical causes.14 The exact extent of excess mortality from specific alcohol-related disease5 has not previously been examined in the SH population. Knowledge of patients’ characteristics and aspects of clinical management following SH may inform clinical practice.
We have investigated alcohol-related mortality in relation to:
risks in the SH population relative to the general population using standardised mortality ratios (SMRs) and years of life lost (YLL);
variation in SMRs by area-level socioeconomic deprivation; and
patient characteristics and clinical management following SH.
Method
Setting and sample
The study was undertaken in three centres in the Multicentre Study of SH in England. The study population,15 risks of suicide and accidental death following SH16 and methods used for SH and suicide17 have been described previously. Data were collected on all individuals who presented with non-fatal SH to general hospital EDs in Oxford (one), Manchester (three) and Derby (two) during the 11-year period, 1 January 2000 to 31 December 2010. Non-fatal SH was defined as intentional self-poisoning or self-injury, irrespective of motivation or degree of suicidal intent.18 Following SH, most patients received a psychosocial assessment by specialist psychiatric clinicians (and some by ED staff). Demographic, clinical and hospital management data on each episode (including referral for aftercare) were collected by clinicians using standardised forms or electronic data entry. Patients not receiving an assessment were identified through scrutiny of ED and medical records, from which more limited data were extracted by research clerks, or in one centre by clinicians (including sociodemographic information and methods of SH). Alcohol involvement in SH (ingestion at the time of, or within 6 h prior to SH) was determined during specialist psychosocial or ED assessment, or from medical records.
Indicator of socioeconomic status
SMRs were calculated by quartile of socioeconomic deprivation. Individuals’ residential postcodes at their first episode of SH were linked to the Index of Multiple Deprivation in England (IMD) 2007,19 in which higher scores indicate greater deprivation. Of the 354 local authority areas in England, Manchester was ranked fourth most deprived, Derby 69th and Oxford 155th. Average IMD scores for England ranged from 4.1 to 47.0, with quartiles: <11.8 (25%), 17.3 (50%), 24.5 (75%) and >24.5. Multicentre sample IMD score quartiles were: <14.3 (25%), 29.7 (50%), 49.5 (75%) and >49.5.
Mortality
Mortality information was supplied by the Data Linkage Service of the National Health Service (NHS).20 Data used for tracing included name, sex, date of birth, NHS number and postcode of last address. Individuals were followed up from 1 January 2000 to 31 December 2012. Observation time for individuals ended when they died or emigrated from the UK.
We obtained alcohol-related death5 rates in England from the Office for National Statistics.2 Alcohol-related deaths included ICD-10 classifications: mental and behavioural disorder due to alcohol (F10), degeneration of the nervous system due to alcohol (G31.2), alcoholic polyneuropathy (G62.2), alcoholic cardiomyopathy (I42.6), alcoholic gastritis (K29.2), alcohol liver disease (K70), chronic hepatitis not elsewhere classified (K73), fibrosis and cirrhosis of the liver (K74) (excluding biliary cirrhosis [K74.3-K74.5]), alcohol-induced pancreatitis (K86.0), accidental and intentional poisoning by alcohol (X45, X65), and alcohol poisoning of undetermined intent (Y15). We report age SMR for alcohol-related death, by sex.
Statistical analyses
Standardised mortality ratios
Individuals traced for any length of time were included. SMRs with exact 95% Poisson confidence intervals (CIs) were calculated for individuals aged ≥ 15 years from observed (O)/expected (E) number of deaths (based on general population rates for England), by age groups (15–34, 35–54, 55–74, 75+) and sex, for years 2000 to 2012.
Years of life lost
YLL were calculated from interim life tables 1999–2001 to 2009–2011 for England.21 Life expectancy was extracted for each individual at the age of death in the appropriate year, which corresponds to YLL. Mean values of YLL (total YLL divided by number of deaths) with 95% CIs are reported, and findings by sex and year are presented graphically.
Logistic regression models
A binary logistic regression was undertaken with dependent variable alcohol-related death (yes/no) and independent variables based on information collected at each individual’s first episode of SH. Univariate models were determined initially, then multivariate models as follows: step (i) inclusion of patient characteristic and clinical management variables (age, sex, employment status, method of SH, alcohol involvement, admission, specialist assessment) that were significant in univariate analyses (p < 0.2); step (ii) forward conditional stepwise (p < 0.05) entry of clinical aftercare variables that were significant in univariate analyses (p < 0.2) (referral to GP, current contact or new referral to psychiatric outpatient care, current contact or new referral to drug/alcohol services).
The ‘not known’ category for alcohol involvement was included (as well as yes/no) because it has clinical significance – many of these patients were not assessed, often because they were intoxicated with alcohol.22 Information on general hospital admission following SH presentation was not reliably collected in Centre B during 2000–2004. Data on referrals to drug/alcohol services were not available in Centre A, these referrals being included in other categories of aftercare. Thus two sensitivity analyses were carried out excluding data for these centres. We adjusted the multivariate model for centre differences. Analyses were conducted using SPSS v19.
Results
Sample
During 2000 to 2010, 41,286 individuals presented with SH and were followed up to the end of 2012. Individuals (940, 2.3%) not traced were excluded; 141 individuals were censored due to emigration during follow-up. Of the 40,346 traced individuals, 1285 (3.2%) aged under 15 years and 47 (0.1%) with unknown age were excluded from analyses. Thus the study sample was 39,014 individuals aged ≥ 15 years (including 15 with unknown gender). Characteristics of the individuals at their first episode of SH grouped according to alcohol involvement at the time or within 6 h of SH are given in Table 1.
Table 1.
Characteristics of individuals at the first episode of self-harm (SH) in the study period, 2000 to 2010.
| Alcohol use at the time or within 6 h of the first episode of SH in the study period, n (%) |
||||
|---|---|---|---|---|
| None | Alcohol involved | Not known | Total | |
| Gender* | ||||
| Male | 4614 (28.0) | 7727 (46.8) | 4167 (25.2) | 16,508 |
| Female | 8320 (37.0) | 9045 (40.2) | 5126 (22.8) | 22,491 |
| Age group | ||||
| 15–34 years | 8584 (35.5) | 9530 (39.4) | 6055 (25.1) | 24,169 |
| 35–54 years | 3244 (26.6) | 6311 (51.8) | 2636 (21.6) | 12,191 |
| 55–74 years | 783 (37.6) | 834 (40.0) | 468 (22.4) | 2085 |
| 75+ years | 330 (58.0) | 100 (17.6) | 139 (24.4) | 569 |
| Ethnic group* | ||||
| White | 9460 (36.8) | 12,774 (49.8) | 3442 (13.4) | 25,676 |
| Black | 425 (52.5) | 256 (31.6) | 129 (15.9) | 810 |
| South Asian | 861 (67.3) | 174 (13.6) | 245 (19.1) | 1280 |
| Other | 370 (44.5) | 210 (25.3) | 251 (30.2) | 831 |
| Employment status* | ||||
| Employed | 3703 (35.8) | 5828 (56.3) | 819 (7.9) | 10,350 |
| Unemployed | 3136 (36.8) | 4308 (50.6) | 1069 (12.6) | 8513 |
| Sick/disabled | 1113 (43.7) | 1308 (51.3) | 128 (5.0) | 2549 |
| Household duties/student/retired | 3803 (50.0) | 2490 (32.8) | 1307 (17.2) | 7600 |
| Method of SH | ||||
| Self-poisoning only | 10,783 (34.2) | 14,097 (44.7) | 6677 (21.2) | 31,557 |
| Self-injury only | 1660 (27.3) | 2022 (33.2) | 2406 (39.5) | 6088 |
| Both self-poisoning and self-injury | 498 (36.4) | 656 (47.9) | 215 (15.7) | 1369 |
There were some missing values for gender (n = 15), employment status (25.6%) and ethnic group (26.7%)
Overall, the sample was predominantly female (16,508/39,014, 57.7%), aged between 15 and 34 years (24,169/39,014, 61.9%) and of White ethnicity (25,676/39,014, 89.9%). Most individuals at their first episode of SH in the study period used self-poisoning alone (31,557/39,014, 80.9%), 6088 used self-injury alone (15.6%) and 1369 (3.5%) used both methods (Table 1). The most common method of self-injury was cutting (5827/7457, 78.1%).
The majority of individuals (22,230/39,014, 57.0%) received a specialist psychosocial assessment following SH. The remaining 43.0% (16,784/39,014) received an ED assessment or advice from liaison psychiatry services or had no assessment following SH. Alcohol was involved in 43.0% of first episodes (16,775/39,014), was not involved in 33.2% (12,941/39,014) and in 23.8% (9298/30,914) alcohol involvement was unknown. Of the 16,784 individuals who did not receive a specialist psychosocial assessment, 31.7% had alcohol involved, 22.0% had no alcohol involvement and in 46.3% alcohol involvement was unknown.
Deaths
After a median follow-up of 7.5 years, 6.9% (2695/39,014) of individuals had died. Deaths were more frequent in males (1565/16,508, 9.5%) than females (1130/22,491, 5.0%; χ 2 = 293.9, df = 1, p < 0.001). Alcohol-related deaths, 307/2695 (11.4%) occurred in a similar proportion of males (170/1565, 10.9%) and females (137/1130, 12.1%; χ 2 = 1.03, df = 1, p = 0.309). Alcohol-related deaths were similar in the three centres (Manchester 173/19,237, 0.9% vs. Oxford 57/9043, 0.6% vs. Derby 77/10,734, 0.7%; χ 2 = 6.6, df = 2, p = 0.037).
Of the 307 alcohol-related deaths, 243 (79.2%) were from digestive disease (ICD-10 K00-K93), 36 (11.7%) from mental and behavioural disorder (ICD-10 F00-F99), 20 (6.5%) from accidents (V01-X59), four (1.3%) from circulatory disease (ICD-10 I00-I99) and the remaining three (0.9%) from suicide (X60-X84), of undetermined intent (Y10-Y34) or assault (X85-Y09). Details of the underlying cause of alcohol-related cause of death and alcohol use at the most recent episode of SH are given in Table 2. Two-thirds of those who died had alcohol involvement at their most recent episode of SH, 7.5% had not used alcohol and in 26.1% this information was not known (Table 2).
Table 2.
ICD-10 underlying cause of alcohol-related death and alcohol use at the most recent episode of SH.
| Alcohol use at the time or within 6 h of the most recent episode of SH prior to death, n (%) |
||||
|---|---|---|---|---|
| Underlying cause of alcohol-related death | None | Alcohol involved | Not known | Total |
| K00-K93 digestive system disease | 17 (7.0) | 156 (64.2) | 70 (28.8) | 243 |
| F00-F99 mental and behavioural disorder | 4 (11.1) | 28 (77.8) | 4 (11.1) | 36 |
| V01-X59 accidents | 0 (0.0) | 17 (85.0) | 3 (15.0) | 20 |
| I00-I99 circulatory system disease | 0 (0.0) | 1 (25.0) | 3 (75.0) | 4 |
| G00-G99 nervous system disease | 0 (0.0) | 1 (100.0) | 0 (0.0) | 1 |
| X60-X84 intentional self-harm; Y10-Y34 undetermined intent; X85-Y09 assault | 2 (66.6) | 1 (33.3) | 0 (0.0) | 3 |
| 23 (7.5) | 204 (66.4) | 80 (26.1) | 304 | |
Of all 2695 deaths, 354 (13.1%) were from digestive disease (ICD-10 K00-K93), and of these, 243 (68.6%) were also alcohol-related, and 111 (31.4%) were unrelated to alcohol.
Risk of alcohol-related death compared to the general population
Compared to the expected numbers of alcohol-related deaths based on general population rates, observed deaths were eight times greater in males, 11 times greater in females and nine times greater for the sexes combined (Table 3).
Table 3.
Relative risk of alcohol-related death in self-harm cohort vs. general population in England, 2000 to 2010: standardised mortality ratio (SMR), and the average number of years of life lost (YLL) in individuals who died from alcohol-related causes.
| Observed number of deaths | Expected number of deaths | SMR (95% CI) | Average YLL (95% CI) | |
|---|---|---|---|---|
| Males | 170 | 20.1 | 8.5 (7.3 to 9.8) | 33.7 (32.4 to 35.1) |
| Females | 137 | 11.8 | 11.6 (9.8 to 13.7) | 38.1 (36.6 to 39.6) |
| Persons | 307 | 31.9 | 9.6 (8.6 to 10.8) | 35.7 (34.7 to 36.7) |
CI: confidence interval.
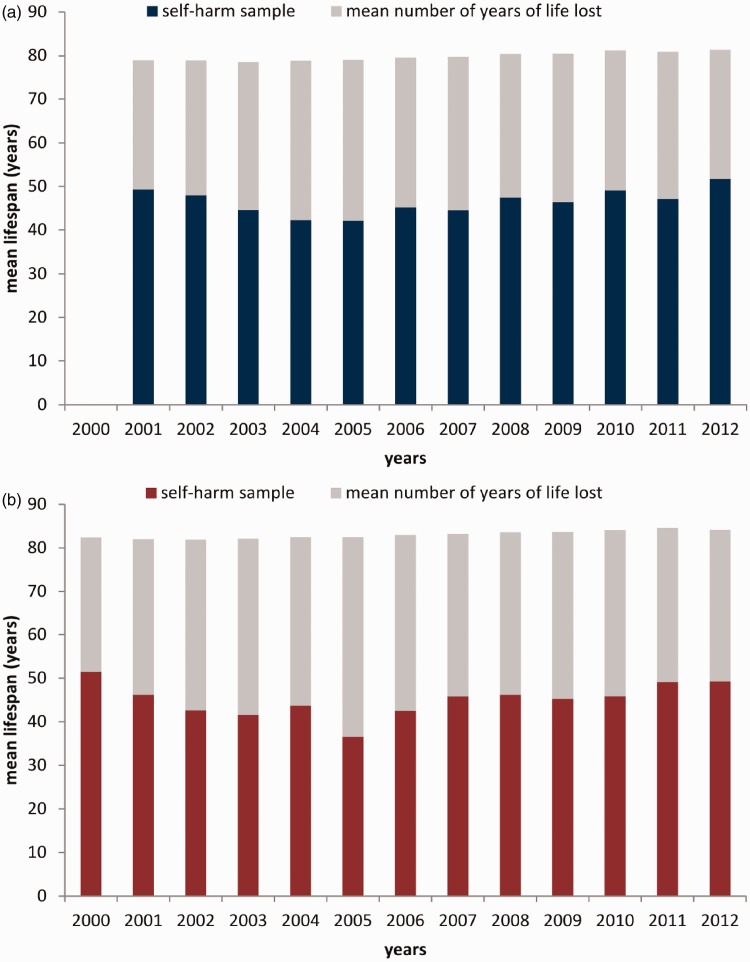
The mean YLL lost for males was 33.7 years (95% CI 32.4 to 35.0), for females was 38.1 (95% CI 36.6 to 39.6) and for the sexes combined was 35.7 (95% CI 35.0 to 36.7) (Table 3). Figure 1 shows YLL for males and females who died, by year.
Figure 1.
Life expectancy of (a) male patients (there were no deaths in year 2000) and (b) female patients who self-harmed and died of alcohol-related disease compared with an age-matched sample of the general population in England.
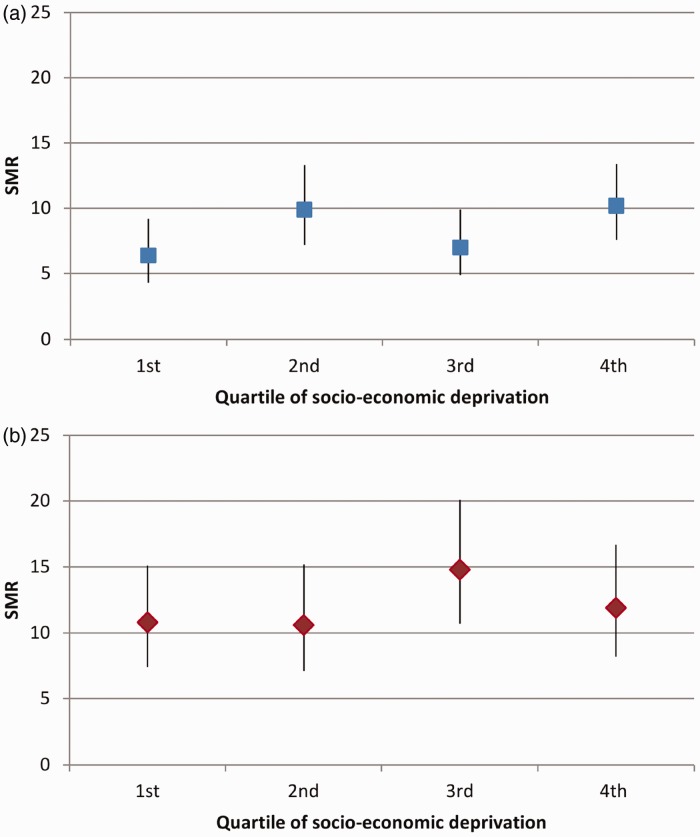
Risk of alcohol-related death compared to the general population, by area-level socioeconomic deprivation at the first episode of SH
IMD scores were unknown for 6.4% of individuals (2505/39,014); however, the proportion with unknown data was similar in those who died from alcohol-related causes (12/307, 3.9%) and in other individuals (2493/38,707, 6.4%, χ 2 = 3.25, df = 1, p = 0.071).
Further examination showed that 58% of the SH sample had IMD scores greater than 24.5, which was the cut-off for the 25% most deprived local authority areas in England.
Alcohol-related mortality showed no relationship with deprivation in males (Figure 2(a)) or females (Figure 2(b)).
Figure 2.
Age-standardised mortality ratios (SMRs) for alcohol-related death by socioeconomic deprivation (Index of Multiple Deprivation, 2007) category in (a) male patients and (b) female patients (bars indicate 95% CIs; IMD 2007 quartiles: scores less than 14.3 (25%), 29.7 (50%), 49.5 (75%), and scores of 49.5 or more; higher scores indicate greater deprivation).
Clinical management and aftercare following SH
We examined associations between alcohol-related deaths (yes/no) and the characteristics and clinical management of patients following SH in person-based analyses (Table 4).
Table 4.
Characteristics of individuals and clinical management at the first episode of self-harm and subsequent alcohol-related death*.
| Binary logistic regression analyses |
|||||
|---|---|---|---|---|---|
| Total N = 39,014, n/N (%) | Univariate, odds ratio (95% CI) | p | Multivariate,† odds ratio (95% CI) | p | |
| Patient characteristics | |||||
| Sex‡ | |||||
| Male | 170/16,508 (1.0) | 1.0 (reference) | 1.0 (reference) | ||
| Female | 137/22,491 (0.6) | 0.59 (0.47–0.74) | <0.001 | 0.80 (0.64–1.01) | 0.143 |
| Age in years | 307/39,014 (0.8) | 1.04 (1.03–1.05) | <0.001 | 1.05 (1.04–1.06) | <0.001 |
| Employment status | |||||
| Employed | 48/10,350 (0.5) | 1.0 (reference) | 1.0 (reference) | ||
| Unemployed | 97/8513 (1.1) | 2.5 (1.7–3.5) | <0.001 | 2.1 (1.5–3.0) | <0.001 |
| Sick or disabled | 45/2549 (1.8) | 3.9 (2.6–5.8) | <0.001 | 2.6 (1.7–4.0) | <0.001 |
| Household/retired/student/other | 23/7600 (0.3) | 0.65 (0.40–1.07) | 0.092 | 0.67 (0.39–1.12) | 0.127 |
| Not known | 94/10,002 (0.9) | 2.0 (1.4–2.9) | <0.001 | 1.6 (1.1–2.5) | 0.024 |
| Method of SH at first episode | |||||
| SP only | 262/31,557 (0.8) | 1.0 (reference) | 1.0 (reference) | ||
| SI only | 36/6088 (0.6) | 0.71 (0.5–1.01) | 0.05 | 0.80(0.56–1.16) | 0.238 |
| SI and SP | 9/1369 (0.7) | 0.79 (0.41–1.54) | 0.489 | 0.99 (0.50–1.93) | 0.965 |
| Alcohol involved in SH | |||||
| None | 23/12,941 (0.2) | 1.0 (reference) | 1.0 (reference) | ||
| Alcohol involved | 212/16,775 (1.3) | 7.2 (4.7–11.1) | <0.001 | 5.9 (3.8–9.1) | <0.001 |
| Not known | 72/9298 (0.8) | 4.4 (2.7–7.0) | <0.001 | 3.5 (2.1–5.9) | <0.001 |
| Clinical management | |||||
| Admission to general hospital | |||||
| None | 66/11,601 (0.6) | 1.0 (reference) | 1.0 (reference) | ||
| Admission | 112/17,469 (0.6) | 1.1 (0.8–1.5) | 0.440 | 1.0 (0.7–1.1.5) | 0.926 |
| Not known/not collected | 129/9944 (1.3) | 2.3 (1.7–3.1) | <0.001 | 2.4 (1.6–3.6) | <0.001 |
| Specialist psychosocial assessment | |||||
| None | 144/1678 (0.9) | 1.0 (reference) | 1.0 (reference) | ||
| Specialist assessment | 163/22,230 (0.7) | 0.85 (0.68–1.07) | 0.168 | 0.64 (0.47–0.88) | 0.005 |
| Referral for aftercare | |||||
| Alcohol or drug service aftercare | |||||
| None | 256/37,269 (0.7) | 1.0 (reference) | 1.0 (reference) | ||
| Current or new referral | 35/1124 (3.1) | 4.6 (3.2–6.6) | <0.001 | 3.2 (2.1–4.7) | <0.001 |
| Told to see | 16/621 (2.6) | 3.8 (2.3–6.4) | <0.001 | 2.5 (1.5–4.4) | 0.001 |
| Psychiatric outpatient aftercare | |||||
| None | 242/29,412 (0.8) | 1.0 (reference) | – | ||
| Current or new referral | 65/9602 (0.7) | 0.82 (0.62–1.08) | 0.161 | ||
| Psychiatric inpatient aftercare | |||||
| None | 293/37,021 (0.8) | 1.0 (reference) | – | ||
| Current or new referral | 14/1993 (0.7) | 0.89 (0.52–1.52) | 0.662 | ||
| Self-discharge after SH episode | |||||
| None | 279/36,161 (0.8) | 1.0 (reference) | – | ||
| Took self-discharge | 28/2853 (1.0) | 1.30 (0.86–1.90) | 0.223 | ||
| GP referral aftercare | |||||
| None | 134/19,135 (0.7) | 1.0 (reference) | – | ||
| Referral by letter or phone contact | 164/18,362 (0.9) | 1.30 (1.02–1.61) | 0.036 | ||
| Told to see | 9/1517 (0.6) | 0.85 (0.43–1.67) | 0.629 | ||
| Other aftercare agency | |||||
| None | 258/32,598 (0.8) | 1.0 (reference) | – | ||
| Formal contact | 25/3388 (0.7) | 0.93 (0.62–1.41) | 0.737 | ||
| Told to see | 24/3028 (0.8) | 1.00 (0.66–1.52) | 0.995 | ||
| Adjustment for centre differences | |||||
| Centre A | 57/9043 (0.6) | 1.0 (reference) | 1.0 (reference) | ||
| Centre B | 173/19,237 (0.9) | 1.43 (1.06–1.93) | 0.019 | 0.58 (0.38–0.87) | 0.010 |
| Centre C | 77/10,734 (0.7) | 1.14 (0.81–1.61) | 0.480 | 0.85 (0.58–1.25) | 0.416 |
SH: self-harm; SP: self-poisoning; SI: self-injury; CI: confidence interval
Logistic regression for outcome of alcohol-related death (yes, no).
Multivariate analysis. Step 1: direct entry of patient characteristic and clinical management variables significant in univariate models at p < 0.2; Step 2: forward conditional entry (p < 0.05) of referral for aftercare variables that were significant at p < 0.2 in univariate models. Final model χ 2 = 405.2, df = 17, p < 0.001; Nagelkerke R square = 0.118.
For 15 individuals sex was not known.
Univariate models (Table 4) show strong associations of alcohol-related death with unemployment and sick/disability status (vs. employed), alcohol involvement during SH, and unknown alcohol involvement (vs. none), and general hospital admission status unknown (vs. not admitted); and a weak association with self-poisoning (vs. self-injury).
The multivariate model (Table 4) shows that after controlling for age, sex, method of SH and centre differences, alcohol-related death was strongly associated with unemployment and sick/disability status, alcohol involvement at SH or unknown alcohol involvement, referral to drug/alcohol services and with lack of psychosocial assessment following SH (36% less likely).
Sensitivity analyses
Sensitivity analyses excluding data from 2000 to 2004 in one centre where admission data were unreliable, and from another centre where information on referrals to specific drug/alcohol services was not known, showed little change in findings.
Discussion
Individuals who presented to hospital with SH (intentional self-injury or self-poisoning) between 2000 and 2010 had greater risk of alcohol-related death than the general population, with a relative risk greater in females (O/E, 11.6) than males (O/E, 8.5). Females in our study who died from alcohol-related disease lost on average 38 years of life (YLL), and males 34 YLL. This risk approaches the 40 YLL found for external causes in a UK SH population,14 and exceeds 11–17 YLL found in British23 and 20 YLL in Australian24 substance use disorder patients for all-cause death. In the SH population, mortality from specific alcohol-related causes in females is greater than from digestive disease or other physical illnesses, though in males, mortality from digestive disease and specific alcohol-related disease are comparable.14 Our findings indicate a gender difference in the adverse consequences of alcohol use, in support of a German study where elevated death rates in alcohol-dependent women (4.6-fold) were greater than in men (1.9-fold).25
We found no relationship between alcohol-related mortality and area-level socioeconomic deprivation. This was unexpected, given marked differences in alcohol-related mortality by geographic region6 and social inequality26 in the general population. Our SH sample is disproportionately disadvantaged, with deprivation scores for more than half of our sample equivalent to those of the 25% most deprived areas in England. This may have reduced group differences based on IMD score, or indicates possibly that alcohol misuse is equally widespread amongst all individuals who SH, not necessarily concentrated in the most socioeconomically deprived areas. Further, unemployed and sick/disabled individuals had greater alcohol-related mortality than employed individuals, thus social inequality and exclusion are also probably involved.
Our finding that many individuals dying of alcohol-related disease were offered referral to drug/alcohol services indicates that the seriousness of their alcohol use was identified at assessment following SH. Participation in specialised alcohol dependence treatment compared to detoxification only or no treatment, however, did not extend survival time in alcohol-dependent individuals in Germany, suggesting that co-occurring health risk behaviour and treatment too late after disease progression may have masked treatment effects.25 Thus early intervention is vital.
Following SH presentation, an opportunity exists to assess physical health and risk behaviour, as well as mental health needs and risks. UK studies have shown that tackling alcohol misuse was key to recovery from SH behaviour in some individuals,27 and brief interventions in inpatient and ED settings may help reduce alcohol use,28 especially where injury is attributed to alcohol use.29
We also identified individuals at increased risk of alcohol-related mortality who did not receive specialist assessment following SH, on whom information was lacking. SH patients taking early discharge30 and those not assessed22 are more likely to have consumed alcohol prior to SH or have been intoxicated on presentation. Temporary admission and delayed assessment to allow recovery have been suggested to alleviate this problem.31
Strengths and weaknesses
Our sample includes all ED presentations for SH over an 11-year period. The large size and high proportion (97.7%) of individuals traced during a two to 13-year follow-up add weight to our findings.
The definition of alcohol-related death5 includes diseases most directly due to alcohol consumption, excluding those with only some causal relationship, such as oesophageal and liver cancer and ulcers. Therefore our findings may underestimate the true extent of alcohol-related mortality in this population.
Our data on alcohol involvement at the time of or prior to SH were based upon clinicians’ assessment of individuals’ self-reported alcohol use rather than use of an itemised scale. Some data required for secondary analyses on clinical management following SH were missing, but in sensitivity analyses excluding these data, the main findings were essentially unchanged.
Clinical implications
The UK government’s strategy3 encourages use of effective interventions to tackle alcohol misuse such as brief interventions, specialised treatment for alcohol dependence and alcohol liaison nurses sited within the ED. Thus, all SH patients should receive assessment in line with guidance (e.g. National Institute for Clinical Excellence32), to enable early identification of alcohol problems and appropriate intervention. Our findings fully endorse those recommendations.
Declarations
Competing interests
None declared
Funding
The authors acknowledge financial support from the Department of Health, including the Policy Research Programme.
Ethical approval
The monitoring systems in Oxford and Derby have approval from local Health/Psychiatric Research Ethics Committees to collect data on SH for local and multicentre projects. Self-harm monitoring in Manchester is part of a clinical audit system and has been ratified by the local Research Ethics Committee. All three monitoring systems are fully compliant with the Data Protection Act of 1998. All centres have approval under Section 251 of the National Health Service Act 2006 to collect patient identifiable information without patient consent, and to release patient details to the Data Linkage Service for the retrieval of mortality information. All patients had access to an information leaflet about the study.
Guarantor
KH
Contributorship
KH proposed the study. HB, RW and KH designed the analysis, HB, KH, RW, JC, SS, MH, JN and NK interpreted the data, HB undertook the analysis and wrote the first draft. All authors contributed to the final draft.
Acknowledgements
The authors thank members of the general hospital psychiatric services and other clinical services, hospital administrative staff and members of the research teams in all three centres for assistance with data collection. The authors declare no financial relationships with commercial interests. KH is a National Institute for Health Research Senior Investigator. The Department of Health had no role in study design, the collection, analysis and interpretation of data, the writing of the report and the decision to submit the paper for publication. The views and opinions expressed herein do not necessarily reflect those of the Department of Health.
Provenance
Not commissioned; editorial review with anonymised peer reviewers' comments from a previous submission to another journal.
References
- 1. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013; 380: 2224–2260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Office for National Statistics. Alcohol-Related Deaths in the United Kingdom, 2010. 2012. See http://www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-249220 (last checked 15 May 2013)
- 3. Drugs and Alcohol Unit. The Goverment's Alcohol Strategy. 2012. See https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/98121/alcohol-strategy.pdf (last checked 16 May 2013)
- 4. Public Health Policy and Strategy Unit/NHS Commissioning Unit. Living Well for Longer: a Call to Action to Reduce Avoidable Premature Mortality. 2013. See https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/181103/Living_well_for_longer.pdf. (last checked 15 May 2013)
- 5. Breakwell C, Baker A, Griffiths C, Jackson G, Fegan G, Marshall D. Trends and geographical variations in alcohol-related deaths in the United Kingdom, 1991–2004. Health Stat Q 2007; 33: 6–24 [PubMed] [Google Scholar]
- 6. Office for National Statistics. Alcohol-Related Deaths in the United Kingdom, 2011. Statistical Bulletin. 2013. See http://www.ons.gov.uk/ons/rel/subnational-health4/alcohol-related-deaths-in-the-united-kingdom/2011/alcohol-related-deaths-in-the-uk–2011.html (last checked 21 May 2013)
- 7. Schmidtke A, Bille Brahe U, De Leo D, et al. Attempted suicide in Europe: rates, trends and sociodemographic characteristics of suicide attempters during the period 1989–1992. Results of the WHO/EURO multicentre study on parasuicide. Acta Psychiatr Scand 1996; 93: 327–338 [DOI] [PubMed] [Google Scholar]
- 8. Hawton K, Bergen H, Casey D, et al. Self-harm in England: a tale of three cities. Multicentre study of self-harm. Soc Psychiatry Psychiatr Epidemiol 2007; 42: 513–521 [DOI] [PubMed] [Google Scholar]
- 9. Haw C, Hawton K, Casey D, Bale E, Shepherd A. Alcohol dependence, excessive drinking and deliberate self-harm: trends and patterns in Oxford, 1989–2002. Soc Psychiatry Psychiatr Epidemiol 2005; 40: 964–971 [DOI] [PubMed] [Google Scholar]
- 10. Touquet R, Csipke E, Holloway P, et al. Resuscitation room blood alcohol concentrations: one-year cohort study. Emerg Med J 2008; 25: 752–756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Horrocks J, Price S, House A, Owens D. Self-injury attendances in the accident and emergency department: clinical database study. Br J Psychiatry 2003; 183: 34–39 [DOI] [PubMed] [Google Scholar]
- 12. Haw C, Houston K, Townsend E, Hawton K. Deliberate self-harm patients with alcohol disorders: characteristics, treatment, and outcome. Crisis 2001; 22: 93–101 [DOI] [PubMed] [Google Scholar]
- 13. Pirkola ST, Suominen K, Isomets ET. Suicide in alcohol-dependent individuals: epidemiology and management. CNS Drugs 2004; 18: 423–436 [DOI] [PubMed] [Google Scholar]
- 14. Bergen H, Hawton K, Waters K, et al. Premature death after self-harm: a multicentre cohort study. Lancet 2012; 380: 1568–1574 [DOI] [PubMed] [Google Scholar]
- 15. Bergen H, Hawton K, Waters K, Cooper J, Kapur N. Epidemiology and trends in non-fatal self-harm in three centres in England, 2000 to 2007. Br J Psychiatry 2010; 197: 493–498 [DOI] [PubMed] [Google Scholar]
- 16. Bergen H, Hawton K, Kapur N, et al. Shared characteristics of suicides and other unnatural deaths following non-fatal self-harm? A multicentre study of risk factors. Psychol Med 2011; 42: 727–741 [DOI] [PubMed] [Google Scholar]
- 17. Bergen H, Hawton K, Waters K, et al. How do methods of non-fatal self-harm relate to eventual suicide? J Affect Disord 2011; 136: 526–533 [DOI] [PubMed] [Google Scholar]
- 18. Hawton K, Harriss L, Hall S, Simkin S, Bale E, Bond A. Deliberate self-harm in Oxford, 1990–2000: a time of change in patient characteristics. Psychol Med 2003; 33: 987–996 [DOI] [PubMed] [Google Scholar]
- 19. Office for National Statistics. Index of Multiple Deprivation (IMD), 2007. See http://data.gov.uk/dataset/index_of_multiple_deprivation_imd_2007 (last checked 12 December 2012)
- 20. Health and Social Care Information Centre. Data Linkage Service, 2013. See http://www.hscic.gov.uk/datalinkage (last checked 21 May 2013)
- 21. Office for National Statistics. England, Interim Life Tables, 1980–82 to 2009–11. 2013 (04/06/2013). See http://www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-274529 (last checked 4 June 2013)
- 22. Hickey L, Hawton K, Fagg J, Weitzel H. Deliberate self-harm patients who leave the accident and emergency department without a psychiatric assessment. A neglected population at risk of suicide. J Psychosom Res 2001; 50: 87–93 [DOI] [PubMed] [Google Scholar]
- 23. Hayes RD, Chang CK, Fernandes A, et al. Associations between substance use disorder sub-groups, life expectancy and all-cause mortality in a large British specialist mental healthcare service. Drug Alcohol Depend 2011; 118: 56–61 [DOI] [PubMed] [Google Scholar]
- 24. Lawrence D, Hancock K, Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. BMJ 2013; 346: f2539–f2539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. John U, Rumpf HJ, Bischof G, Hapke U, Hanke M, Meyer C. Excess mortality of alcohol-dependent individuals after 14 years and mortality predictors based on treatment participation and severity of alcohol dependence. Alcohol: Clin Exp Res 2013; 37: 156–163 [DOI] [PubMed] [Google Scholar]
- 26. Siegler V, Al-Hama A, Johnson B, Wells C, Sheron N. Social inequalities in alcohol-related mortality by national statistics socio-economic classification, England and Wales, 2001–03. Health Stat Q 2011; 50: 4–39 [DOI] [PubMed] [Google Scholar]
- 27. Sinclair J, Green J. Understanding resolution of deliberate self harm: qualitative interview study of patients’ experiences. BMJ 2005; 330: 1112–1115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mdege ND, Fayter D, Watson JM, Stirk L, Sowden A, Godfrey C. Interventions for reducing alcohol consumption among general hospital inpatient heavy alcohol users: a systematic review. Drug Alcohol Depend 2013; 131: 1–22 [DOI] [PubMed] [Google Scholar]
- 29. Walton MA, Goldstein AL, Chermack ST, et al. Brief alcohol intervention in the emergency department: Moderators of effectiveness. J Stud Alcohol Drugs 2008; 69: 550–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Barr W, Leitner M, Thomas J. Self-harm patients who take early discharge from the accident and emergency department: how do they differ from those who stay? Accid Emerg Nurs 2004; 12: 108–113 [DOI] [PubMed] [Google Scholar]
- 31. Royal College of Psychiatrists. Better Services for People Who Self-Harm. Quality Standards for Healthcare Professionals, 2006. See http://www.rcpsych.ac.uk/pdf/self-harm%20quality%20standards.pdf (last checked 24 June 2013)
- 32. National Collaborating Centre for Mental Health. Self-Harm: the Short-Term Physical and Psychological Management and Secondary Prevention of Self-Harm in Primary and Secondary care (full guideline). Clinical Guideline 16, London: National Institute for Clinical Excellence, 2004 [Google Scholar]