Abstract
Dietary and endogenously modified lipids modulate inflammation by functioning as intra- and intercellular signaling molecules. Proinflammatory lipid mediators such as the eicosanoids compete against the signaling actions of newly discovered modified fatty acids that act to resolve inflammation. In inflammatory bowel disease, multiple aberrancies in lipid metabolism have been discovered, which shed further light on the pathogenesis of intestinal inflammation. Mechanisms by which lipids modulate inflammation, abnormalities of lipid metabolism in the setting of inflammatory bowel disease, and potential therapeutic application of lipid derivatives in this setting are discussed.
Keywords: inflammatory bowel disease, fatty acids, metabolism, inflammation, therapy
LIPIDS AND INFLAMMATORY BOWEL DISEASE
Lipids, once considered to be static metabolic energy reserves, have emerged as important components of cellular signal transduction pathways. Their roles in modulating host inflammatory responses are of clinical interest as agents of both promotion and resolution. Dietary lipids are implicated in the pathogenesis of chronic intestinal inflammation, including inflammatory bowel disease (IBD), and lipid-mediated signaling has been the focus of research in mucosal immunity over the past two decades. At present, there is rapidly expanding insight into novel lipid mediators that function to regulate inflammation. Recent developents in understanding the pro- and antiinflammatory actions of lipid signaling molecules are discussed herein. Lipids in chronic intestinal inflammation are addressed, focusing on dietary lipids, the role of lipids in mucosal immunity, lipids in inflammatory signal transduction, alterations in lipids associated with the emergence of chronic inflammation, and lipid-based therapies undergoing exploration in IBD.
IBD BACKGROUND, MUCOSAL IMMUNITY, THE ICROFLORA, GENETIC RISK, AND THE NVIRONMENT
IBD is a group of chronic, immune dysregulation disorders of the gut, typically classified as Crohn’s disease (CD) or ulcerative colitis (UC). These disorders have risen rapidly over the second half of the 20th century, with a preponderance in Westernized nations.1–3 Although the exact etiology of IBD is unknown, it is a multifactorial process and comprehensive reviews of IBD pathogenesis have been recently published.1,4,5 While a genetic predisposition does exist, environmental factors such as enteric infections, smoking, and diet have also been implicated. The typical Western diet, which is high in fat and refined carbohydrates and low in fiber, has been linked to many chronic illnesses, including IBD.6
The immune system of the gut must maintain a fine balance between pro- and antiinflammatory processes. The epithelial and immune cells of the gut need to correctly identify “normal,” or commensal, bacteria that reside in the colon from pathologic bacteria that cause disease. In brief, epithelial and antigen-presenting cells, such as dendritic cells, are constantly sampling the luminal contents of the intestine. Bacterial products of pathogens bind to pattern recognition receptors (PRRs), such as Toll-like receptors (TLRs) and nucleotide oligomerization domain (NOD) proteins, and are processed by the cell. This in turn activates nuclear factor-κB (NF-κB), a transcription factor, which produces inflammatory cytokines such as tumor necrosis factor (TNF)-α and interleukin (IL)-1β, resulting in recruitment of T helper (Th)-1, Th-2, and Th-17 cells and further stimulation of the inflammatory response to ward off infection.4 When the cells correctly identify commensal bacteria, predominantly antiinflammatory cytokines are produced, including IL-10 and transforming growth factor-β TGF-β), which prime T cells into T-regulatory cells.7 This mechanism keeps inflammation in check. When commensal bacteria are inappropriately recognized as pathogenic bacteria, also known as loss of tolerance, proinflammatory signaling cascades are stimulated. In IBD, multiple steps along this chain of events can be aberrant, including inappropriate binding of PRRs, dysregulation of Th cell differentiation, and exaggerated proinflammatory cytokine signaling (TNF-α, IL-6, IL-23, etc.).4,8 Acute inflammation can lead to local cell injury and death, release of reactive oxygen species, and further activation of the inflammatory cascade, resulting in a vicious cycle. As we learn more about the dysregulation of the immune response in IBD, it is becoming increasing clear that lipids direct both the type and degree of inflammatory responses mounted in the intestine.9
BRIEF OVERVIEW OF FATTY ACID NOMENCLATURE
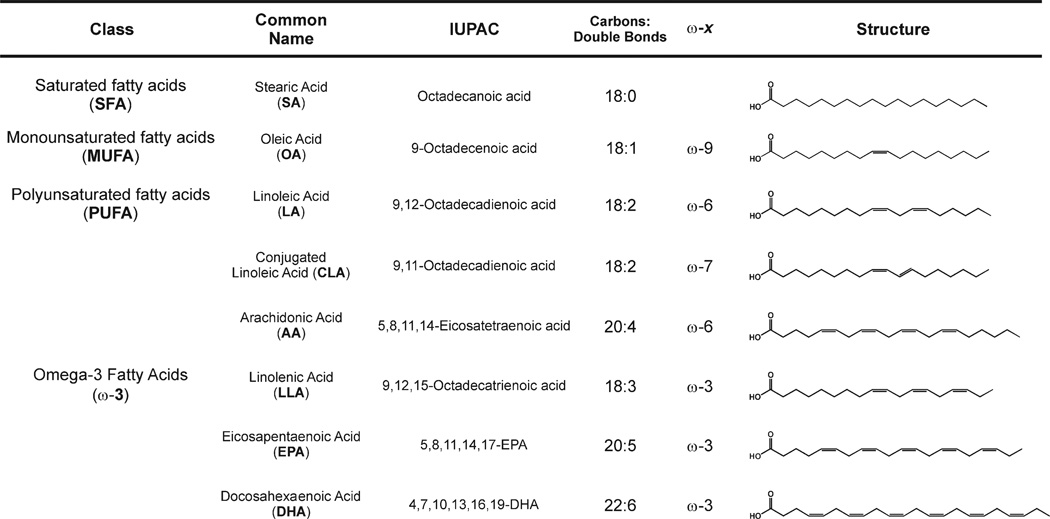
Fatty acids (FAs) are hydrocarbon chains with a terminal carboxylic acid functional group. They are generally notated by carbon length, the presence or absence of double bonds, and the location(s) of the double bond(s). Short chain fatty acids (SCFAs) have six carbons or less, medium chain fatty acids (MCFAs) have 6–12 carbons, long chain fatty acids (LCFAs) have 12–20 carbons, and very long chain fatty acids (VLCFAs) have greater than 22 carbons. Saturated fatty acids (SFAs) have no double bonds, monounsaturated fatty acids (MUFAs) have one double bond, and polyunsaturated fatty acids (PUFAs) have more than one double bond. The position of the double bond, counting from the terminal methyl carbon, is denoted as the “omega” position, and is written as ω-X. For example, an omega-3 FA (ω-3) will have a double bond on the third carbon from the terminal end of the fatty acid chain. Figure 1 provides a description of the FA commonly addressed herein.
FIGURE 1.
Fatty acid nomenclature and structures. The nomenclature used to describe fatty acids has evolved to such an extent that multiple conventions are used in the literature. Common names, IUPAC nomenclature, informal denotation, and structures are defined for the fatty acids described herein.
LIPIDS AS SIGNALING MOLECULES
Proinflammatory Eicosanoids
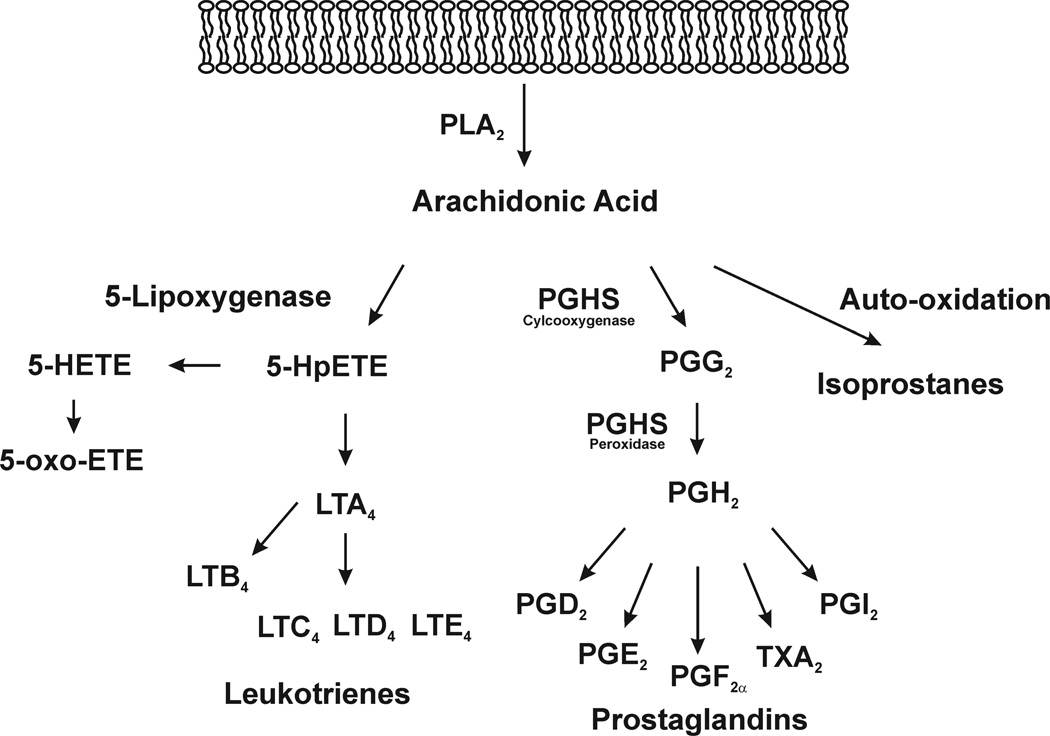
Lipids are now recognized as key components of multiple signal transduction cascades, including those associated with the regulation of inflammation. Fatty acids incorporated into phospholipids of the membrane bilayer are substrates for multiple members of the phospholipase family of hydrolytic enzymes. In general, unsaturated fatty acids are located on the sn-2 carbon of the phospholipid glycerol backbone and are hydrolyzed by a phospholipase A2 (PLA2) during host inflammatory responses. Arachidonic acid (AA), a 20-carbon fatty acid containing four double bonds, is a primary target of regulated PLA2 hydrolysis, and is the precursor to a vast array of lipid signaling molecules10 (Fig. 2). PLA2-mediated hydrolysis of AA is a tightly controlled process that involves two PLA2 isoforms: the 85 kDa cytosolic PLA2 (cPLA2) and the calcium-independent PLA2 (iPLA2).11 These enzymes are activated during host inflammatory responses, being primarily regulated by the mitogen-activated protein kinase (MAP kinase) signaling cascades. Cyclooxygenases (COX) 1/2 oxidize AA, and to a lesser extent other PUFAs, to generate the prostaglandin family of oxidized fatty acids. Lipoxygenases catalyze fatty acid hydroxylation, cytochrome P450 also hydroxylates fatty acids, and AA can undergo auto-oxidation reactions to form the isoprostanes. In general, these lipid species are proinflammatory, propagating their signaling actions via receptor-mediated mechanisms and are responsible for many of the phenomena of inflammation, including fever, increased vascular permeability, chemotaxis, edema, and tissue damage.12,13
FIGURE 2.
Eicosanoid formation. During host immune responses, arachidonic acid is hydrolyzed from membrane phospholipids and is converted to multiple oxidized fatty acid metabolites via enzymatic and autocatalytic mechanisms. In general, eicosanoids mediate proinflammatory cell signaling pathways and are involved in the pathogenesis of IBD.
Antiinflammatory Mediators
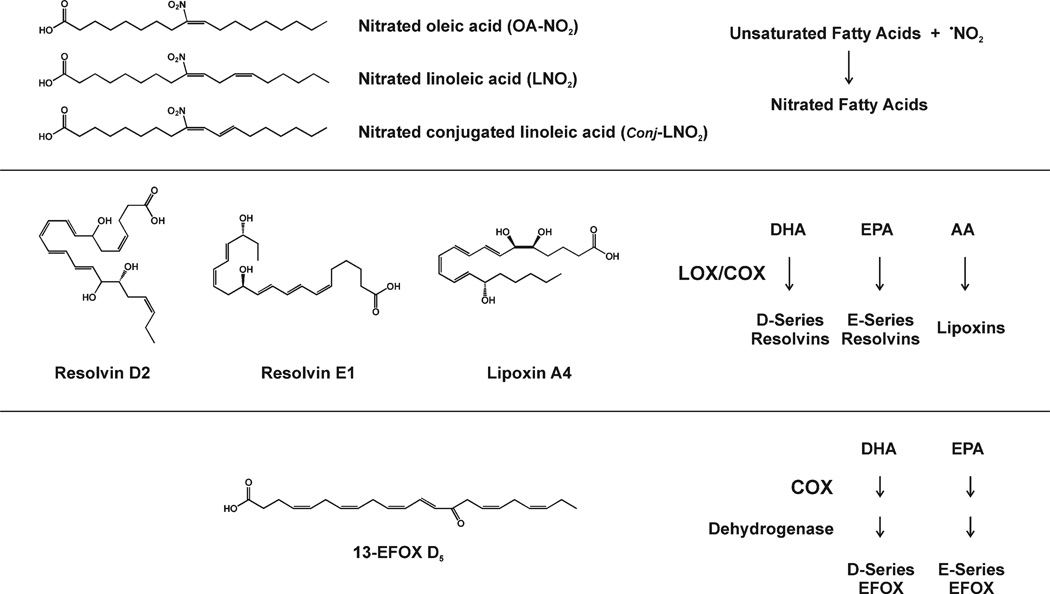
The role of oxidized lipids as proinflammatory mediators is well established. However, in the past decade several classes of lipid mediators have been discovered whose signaling actions act to resolve rather than promote inflammation (Fig. 3). The D- and E-series of resolvins (trihydroxy derivatives of docosahexaenoic [DHA] and eicosatetraenoic [EPA] acids), lipoxins (trihydroxy derivatives of AA), protectins (conjugated triene derivatives of DHA), nitroalkenes (fatty acids nitrated at a site of unsaturation), and EFOX (electrophilic oxo-derivatives), a recently discovered class of enzymatically oxidized omega-3 fatty acids containing an α,β-unsaturated keto moiety, represent the growing field of endogenous lipid mediators that work either via receptor-mediated signaling pathways or by protein posttranslational modification to downregulate inflammatory responses. These molecules are currently the subject of intense research, as they represent an emerging generation of investigational new drugs to address inflammatory diseases, including IBD.
FIGURE 3.
Antiinflammatory lipid mediators. Recent advances in inflammatory and lipid research have identified promising lipid mediators in vivo that appear to resolve inflammation, including nitrated fatty acids, resolvins, and lipoxins, and electrophilic oxo-fatty acid derivatives (EFOX).
Lipids as Electrophiles
The location of an electron-withdrawing functional group (e.g., a nitro or a keto functional group) on a carbon–carbon double bond makes the carbon-β to the electron-withdrawing group electron-poor, enabling it to react with nucleophiles, such as the amino acids cysteine, histidine, and lysine. This chemical reactivity is termed electrophilicity. Electrophilic lipids have been shown to form rotein adducts through the reaction of lipid aldehydes with nucleophilic amino acid residues to form Schiff base products.14 Alternatively, protein adducts can be formed by Michael addition reactions between protein thiolate anions and electrophilic carbons. The posttranslational modification of proteins by electrophiles has been reported in several model systems, wherein exogenously added electrophilic lipids covalently modify target proteins.15–19 Covalent, posttranslational modifications by electrophilic fatty acids alter the structure, trafficking, and catalytic activity of proteins such as cathepsin B,20 Keap1,17 insulin,21 and glyceraldehyde-3-phosphate dehydrogenase (GAPDH).22,23 A key tissue defense against xenobiotics and oxidants is the regulated expression of phase II proteins (antioxidant enzymes), which is mediated by electrophilic interactions, particularly with Nrf2 (nuclear factor erythroid 2-related factor 2, a member of the basic-leucine zipper NF-E2 family of transcription factors) and the electrophile-reactive, cysteine-rich cytoplasmic suppressor protein Keap-1 (Kelch-like ECH-associating protein).24 This widespread mechanism, conserved in both plants and animals, protects against pathogens and metabolic or inflammatory stress.
Antiinflammatory electrophilic lipid mediators are highly reactive small molecules that react with nucleophilic centers in biomolecules, which makes their detection in blood and tissue as free fatty acids problematic. However, “bottom-up” proteomic approaches using mass spectrometry have enabled the identification of electrophilic protein adducts. Electrophiles appear to have selective and specific protein targets and only adduct a portion of the seemingly available sites, which is likely due to the chemical environment of the protein site surrounding the nucleophilic center and the strength and chemical properties of the electrophile.25
DIETARY INFLUENCES ON INFLAMMATION
In the United States, oils from corn and soybeans are found in most fast and processed foods, and in the feed given to domesticated animals used for meat and dairy products. These oils are high in linoleic acid (LA), an 18-carbon, omega-6 (ω-6) PUFA. LA is readily converted to AA, which, as described above, can be metabolized into the proinflammatory prostaglandins (PG), thromboxanes (TX), and leukotrienes (LT). The Western diet is also typically low in the omega-3 (ω-3) fatty acids (e.g., DHA, and EPA, respectively), which are thought to promote antiinflammatory responses. This growing proportion of potentially inflammatory dietary lipids is thought to increase the risk of developing IBD.6
It is intuitive that higher intake of LA from the diet will increase the levels of AA present in membrane phospholipids, and therefore augment the proportion of ω-6 end products formed during inflammation. Indeed, a prospective cohort study followed participants over 4 years and found that a high intake of LA was associated with a greater risk of developing UC.26 Along the same line, another study demonstrated that human IBD intestinal smooth muscle and control smooth muscle cells incubated with AA had elevated levels of IL-8 and other markers of oxidative stress, whereas incubation with oleic acid (OA) appeared to be protective.27 Administering AA directly through the diet did not change the degree of colitis in a murine experimental colitis study wherein mice were given diets rich in OA versus AA versus fish oil for 6 weeks prior to inducing colitis, even though the colonic content of AA was higher in the AA-fed group.28 These results suggest that dietary fatty acid content can affect host inflammatory responses.
LIPID METABOLISM IN IBD
Lipids are critical to cell membrane structure and fluidity, mucus production and barrier integrity, eicosanoid production (Fig. 3), and intra- and intercellular signaling. Given that anomalies in any of these functions could propagate inflammation and tissue destruction, it stands to reason that perturbations in lipid metabolism could contribute to the development of IBD. Indeed, abnormalities of lipid metabolism in patients with IBD are seen at multiple levels, and are summarized in Table 1.
TABLE 1.
Fatty Acid Metabolism in IBD
| Abnormal Finding in Colonic Tissue | Proposed Effects | References |
|---|---|---|
| ↑ Long chain fatty acids | ↑ Eicosanoid production | 29–33 |
| ↓ Essential fatty acids | ↑ Eicosanoid production | 29–30 |
| ↑ Phospholipase A2 (PLA2) | ↑ Pool of free arachidonic acid | 38 |
| ↑ Fatty acid binding protein (FABP) | ↑ Fatty acid intracellular utilization | 46 |
| ↑ Leukotriene B4 (LTB4) | ↑ Inflammatory signaling | 39–41 |
| ↑ Prostaglandin E2 (PGE2) | ↑ Inflammatory signaling; possible mitigating agent | 13, 42–43 |
| ↓ Phosphatidylcholine (PC) | ↑ Abnormal mucous production and barrier function | 50 |
| ↑ Ceramide | ↑ PLA2 and NF-κB activities | 56–57 |
| ↑ Matrix metalloproteinase (MMP) | ↑ Intra- and extracellular destruction | 57–62 |
Summary of proposed mechanisms by which abnormal lipid metabolism may contribute to the pathogenesis of IBD.
Fatty Acid Levels in Tissue and Cells
Inflammation alters lipid utilization in the intestine. Some general trends of this alteration are seen in the mucosal tissue in both humans and rodents, regardless of the etiology of the inflammation. In a study comparing colonic biopsies of patients with active and inactive UC versus healthy controls, the UC patients had a significantly higher proportion of SFA and long-chain ω-3 and ω-6 PUFA with a concomitant decline in essential FA and MUFA, specifically due to decreased OA levels.29 These same findings of elevated SFA plus lower MUFA and essential FA are also seen in active and inactive CD patients, with a significant rise in end product ω-3 and ω-6 PUFA in one group30 and a nonsignificant increase of these FA in the other study.29 Both ileal and colonic tissue were similar in the CD patients, and although the degree of change was less in those with inactive versus active disease, even “normal-appearing” tissue differed from controls.29,30 All of the above subjects reported typical Western or mixed Western/ Mediterranean diets and were not taking fish oil supplements to explain the increase in ω-3 FA. Similar results were seen in two other studies, where a larger proportion AA was detected in the phospholipid component from colonic biopsies of both UC and CD patients with active disease.31,32 Low levels of OA were again noted. Diet was not mentioned in these studies. Rodent studies using 2,4,6-trinitrobenzene sulfonic acid (TNBS) to induce colitis also demonstrated greater end product LCFA compared to controls despite no difference in diet; however, the changes in SFA and MUFA differed among the two studies.29,33
These studies taken together indicate that there is a reproducible pattern of intestinal lipid metabolism with active inflammation in the setting of IBD. Overall, both ω-3 and ω-6 LCFA end products are found in higher proportions in the intestinal epithelium, whereas the “building-block” essential FA are diminished, suggesting consumption in the course of eicosanoid production. This shift in FA patterns may be a response to inflammation rather than an etiological factor, although the extent and duration of eicosanoid production may prove to be problematic in IBD. OA levels are routinely reduced, and SFA are seen in greater proportion, although the significance of this is uncertain. Stearic acid and other long-chain SFA have been shown to inhibit endothelial cell growth, as well as induce inflammation, apoptosis, and accentuate intercellular adhesion molecule 1 (ICAM-1) expression.34 Similar actions may also be occurring in the intestinal tissue.
In both rodent and human studies, plasma FA levels differ from controls but do not reflect the mucosal changes described above. Linolenic acid (an ω-3 precursor) is elevated in both UC and CD (active and inactive), and the polyunsaturated LCFAs are lower compared to controls, which is the opposite of what is seen in the mucosal tissue.35,36 All study subjects reported a typical Western diet. Erythrocyte membrane phospholipids in IBD patients had higher concentrations of LA and total ω-6 FA compared to controls, despite an overall lower dietary lipid intake. There was no difference in ω-3 levels in the erythrocyte phospholipids.37
To support the hypothesis that a preferential ω-6 LCFA metabolism occurs in the intestine, increased phospholipid turnover and elevated levels of phospholipase A2 have been reported in both UC and CD mucosal biopsies,38 which results in an increase in AA hydrolysis and the downstream generation of proinflammatory oxidized AA lipid mediators. For example, elevations in LTB4, as well as the enzymes necessary for its production, have been detected in colonic biopsies of IBD patients.39,40 Neutrophils from patients with IBD also have enhanced release of LTB4 compared to controls, despite similar extent of AA-uptake by the cells.41 Since inflamed mucosa is highly infiltrated with activated neutrophils, this likely contributes to the overall increase in LTB4 levels present in colonic samples. Other AA-derived eicosanoids, such as PGE2, also rise in colonic mucosa, especially in severely inflamed mucosa from UC patients.42 Interestingly, PGE2 was important in resolving colitis in a mouse model, suggesting it may function as both an instigator and alleviator of inflammation.43
Fatty Acid Metabolism Gene Expression
Alterations in the expression of genes responsible for FA metabolism occur in IBD. Fatty acids can diffuse across cell membranes, but transmembrane fatty acid transport proteins (FATP), including CD36, likely facilitate and regulate specific FA entry into the cell, especially LCFA and VLCFA. Once the FA crosses the cell membrane, it can reversibly bind to fatty acid binding proteins (FABP) for further metabolism.44,45 Serum levels of intestinal FABP rise in severe UC,46 suggesting that essential FA and other LCFA may be selectively metabolized intracellularly during inflammation. Microarray analysis of pooled IBD colonic specimens showed higher expression of FABP compared to controls. In addition, there was an increase in acyl-CoA synthetase and a reduction in fatty acid synthase.44 In a microarray study of IL-10 knockout mice (a murine model of chronic colitis), fatty acid metabolism genes were predominantly downregulated, while inflammatory response genes were upregulated during inflammation, although the specific genes were not identified.47 Once these mice displayed clinical and histologic improvement after treatment with a probiotic (an oral commensal bacteria product), there was a concurrent upregulation of peroxisome proliferator-activated response-γ (PPAR-γ), LA, and AA metabolic genes as inflammation resolved.
Mucus and Phospholipid Alterations
The integrity of gut epithelial cells is essential to function as a physical barrier against pathogens. A layer of mucus adheres to the surface of the epithelium and is formed largely of phospholipids, predominantly phosphatidylcholine (PC) and lysophosphatidylcholine (LPC).48 It is hypothesized that defective mucus leads to increased interactions between the epithelium and luminal antigens/pathogens, stimulating an immune response associated with IBD.49 Analysis of colonic tissue from patients with IBD who were clinically in remission displayed significantly less PC among UC patients, compared to those with CD and controls.50 The FA composition of PC was similar among all groups. The UC group also had a higher ratio of LPC to PC, which may result in greater detergent activity by LPC and greater tissue destruction. Another study using cultured enterocytes showed that PLA2 (which is increased in IBD patients), converts PC to LPC, leading to increased tight junction permeability and bacterial translocation.51 Several animal studies have shown protection from experimental colitis when given exogenous sources of PC in the diet.52,53 Another key component of mucus is mucin (a glycoprotein) that has also been found to be selectively abnormal in UC patients, but not those with colitis from CD, infection, or ischemia.54,55
Ceramide and Metalloproteinase-1
Mucosal destruction can arise from the action of sphingomyelinase, which generates ceramide, a lipid molecule that acts as an intracellular second messenger. Ceramide is a component of sphingomyelin, which is found in the cell membrane and is associated with a wide variety of cellular functions, including differentiation, growth, and apoptosis. Ceramide modulates AA metabolism by increasing PLA2 activity or by directly activating NF-κB, depending on the type of sphingomyelinase employed by the cell.56 In two types of experimental chronic colitis in mice, ceramide rose substantially in the intestinal epithelial cells as inflammation evolved. Caco-2 intestinal cells were also stimulated with exogenous sphingomyelinase, which resulted in a robust production of matrix metalloproteinase-1 (MMP-1). Inhibition of the sphingomyelinase also inhibited MMP-1 production.57 MMPs are a family of proteases that degrade the extracellular matrix and can disrupt the epithelial basement membrane, leading to tissue damage, loss of cells, and impaired wound healing, and are of particular interest in the pathogenesis of IBD.58,59 Elevated levels of MMP have been found in the ulcerated tissue of patients with IBD, and the allelic composition of MMP genes may influence CD phenotype with regard to stricture formation.60–62 MMPs are also involved in chemotaxis and cell adhesion, and appear to be activated by inflammatory cells and their cytokines, such as TNF-α.58,59,62
Cholesterol and Lipoprotein Metabolism
Changes in cholesterol and apolipoprotein metabolism occur during IBD as well. Hypocholesterolemia has previously been noted during times of acute inflammation, including active IBD,63–66 and can be used as a marker of disease severity. Other general trends include elevated triglycerides and decreased high-density lipoprotein (HDL) levels.65,66 Apolipoprotein A-1 (ApoA-1), which mediates cholesterol efflux from peripheral tissues, is also decreased in patients with IBD.65,66 One possible mechanism of action is that ApoA-1 is displaced by the acute phase reactants, C-reactive protein and serum amyloid A, which are elevated during times of active IBD.67 These impairments could lead to atherosclerosis, which is associated with IBD68,69.
LIPIDS AS THERAPY FOR IBD
Omega-3 Fatty Acids and Oleic Acid
While a diet high in LA can promote a proinflammatory cascade in IBD, other fats may help limit inflammation. The dietary intake of OA or ω-3 FA appears to competitively inhibit AA for eicosanoid production. Omega-3 FA from dietary fish oil is incorporated into colonic tissue in as little as 3 weeks, and eicosanoid production is altered over a 12-week period in patients with IBD.70 OA was also increased in the colonic mucosa by 12 weeks in patients given olive oil, but no change in eicosanoid production was seen. Despite the protection afforded by consuming ω-3 FA in other models and clinical situations, studies of ω-3 supplementation in IBD have had mixed results. A recent review of this literature was done by Calder71 and several other systematic reviews have been published.72–76 Results from animal studies show greater therapeutic effect—this may be due to the relatively higher doses of ω-3 FA given to animals compared with human trials. Also, the “placebo” oils used in some the human trials, such as OA, may have antiinflammatory properties themselves, which confounds interpretation of the results. A recent G-protein-coupled receptor has been identified that functions as an ω-3 FA receptor.77 These receptors are highly expressed in macrophages, and the antiinflammatory effects of ω-3 FA supplementation are lost in knockout mice that do not possess these receptors. It is interesting to speculate whether these receptors are abnormal in certain IBD populations, which may affect responsiveness to ω-3 supplementation. Another consideration is the complexity of diet in general. It may not be enough to simply supplement one lipid without changing to an overall healthier diet with limited processed foods.
Enteral Nutrition
Complete enteral nutrition can be a first-line treatment for CD, although it is more effective and better tolerated in children than adults.78,79 The mechanism by which this diet leads to clinical improvement and mucosal healing is uncertain and is likely multifactorial, but one hypothesis is that the fat content, which is high in MUFA, is less inflammatory. Studies have shown that manipulating the fat in enteral formulas changes the remission rate, but the optimal lipid composition is still uncertain and results have been contradictory. In one study, adult patients with active CD were randomized to receive elemental diets with varying amounts of fat, predominantly from LCFA: low (3 g/ day), medium (16 g/day), or high (30 g/day). The remission rates were 80%, 40%, and 20%, respectively, suggesting the lower the LCFA intake, the better.80 They did not evaluate how differing amounts of mixed FA would be tolerated. It is also worth noting that even the “high” amount of fat in this study is about half the daily intake of a regular diet. In another study of adult patients with active CD, the groups received an enteral diet with 35 g/1000 kcal of lipid as either high OA/low LA versus low OA/high LA, or steroids and a regular diet. After adjusting for poor compliance to the enteral diets, the 4-week remission rates were 27%, 63%, and 79%, respectively, with the group receiving low OA/high LA doing better than the other diet group.81 In another adult study of active CD, patients received enteral formulas with either 5% or 30% of calories coming from LCFA. The total calories from fat was identical and the remainder was comprised of MCFA. Thirty-nine percent of the patients withdrew from the study due to intolerance to the diet. Of those that continued with treatment, the remission rate was similar between both groups (46% and 45%, respectively).82 Similar studies have not been carried out in pediatric patients, where enteral feeding is more efficacious.
Short Chain Fatty Acids
Short chain fatty acids, such as butyrate, proprionate, and acetate, are produced by colonic bacteria as they digest fiber and other nonabsorbable sugars. These SCFA are integral to healthy epithelial cells, as they are used by the cells as an energy source and help maintain homeostasis and regulate inflammation. Human studies are sparse, but other studies suggest SCFA may directly inhibit NF-κB activation or bind PPAR-γ receptors.83,84 Although other factors are also involved, SCFAs are needed to help repair the damaged epithelium associated with IBD.85 Various abnormalities of SCFA have been seen in both active and inactive phases of IBD, but it is not clear if there is a problem with SCFA utilization by the epithelial cells or if there is abnormal production by colonic bacteria.86
While clinical studies focusing on nutritional intake have been difficult to control and follow over long periods of time, manipulating dietary lipid intake is still attractive as a therapeutic intervention for IBD. At the biochemical level, lipids may attenuate inflammation by undergoing reactions that favor the formation of derivatives displaying antiinflammatory actions. Table 2 lists potentially therapeutic lipids.
TABLE 2.
Lipids as Potential Therapeutic Agents to Treat IBD
| Lipid Treatment | Clinical Outcome | References |
|---|---|---|
| ω-3 Fatty acids | ↓ Colitis in rodents; mixed results in humans | 71–76 |
| Short chain fatty acids | Induced epithelium repair in human intestinal tissue | 85 |
| Resolvins | ↓ Colitis in rodents | 92–94 |
| Nitro-oleic acid | ↓ Colitis in rodents | 110 |
| Conjugated linoleic acid | ↓ Colitis in rodents↓; colitis in pigs | 113–135 |
Free fatty acids have been used to treat IBD in animal models of the disease as well as in humans.
PRO-RESOLVING LIPID MODULATORS
Lipoxins and Resolvins
The conversion of AA to proinflammatory eicosanoid products is well defined; however, AA and other PUFAs can also be modified via alternative mechanisms to form signaling molecules involved in resolution of inflammation. The role these mediators play in modulating the pathology of IBD is an emerging area of interest.87 Examining exu-dates from animal models with resolving, self-limited inflammation revealed that AA metabolites undergo a “class switch,”88 wherein rather than being used as a substrate for eicosanoid synthesis, AA is modified by lipoxygenases or aspirin-acetylated COX-2 to form lipoxins (Lx). These products are generated by leukocyte, platelet, and endothelial/epithelial cell-to-cell interactions. Intestinal epithelial cells have lipoxin receptors that when bound suppress inflammatory gene expression via the NF-κB pathway. They also resolve local inflammation by dampening chemotaxis, leukocyte adhesion, and transcellular migration of neutrophils.89 Mononuclear cells are then recruited to help clean up cellular debris. Patients with UC do have lower levels of Lx in their colonic tissue compared to healthy controls,90 although it is uncertain if this is due to overwhelming inflammation or a decreased ability to produce Lx. Notably, the isolated UC colonic cells did respond to aspirin by producing lipoxins in vitro.
Resolvins are molecules that are structurally similar to Lx (i.e., trihydroxy fatty acid derivatives), but are derived from ω-3 FA: Resolvin E (RvE) species stem from EPA, and Resolvin D (RvD) are generated from DHA. Resolvins are formed in vivo, but their production is enhanced by the presence of aspirin. They also play a role in neutrophil trafficking and clearance of neutrophils from the mucosa.88,91 Studies of experimental colitis in a murine model have shown clinical and histologic improvement by treating with synthetic RvE1.92–94
Electrophilic Oxo-derivatives
A recent study has identified another class of antiinflammatory keto-fatty acid mediators derived from ω-3 FA: EFOX.95 These products are formed by macrophages and neutrophils activated by multiple agonists including phorbol myristate acetate (PMA), LPS, and interferon-γ (IFN-γ), with concentrations of up to 20–200 nM poststimulation. The roles that these molecules play in mediating inflammation are not fully understood, but studies indicate that EFOX induce Nrf-2 nuclear accumulation and expression of the Nrf-2-regulated cytoprotective enzymes HO-1, glutamate-cysteine ligase subunit (GCLM), and nicotinamide adenine dinucleotide phosphate (NADPH):quinine oxidoreductase 1 (NQO1). Furthermore, EFOX suppresses the expression of IL-6, monocyte chemotactic protein 1 (MCP-1), IL-10, and inducible nitric oxide synthase (iNOS). The formation of these antiinflammatory mediators derived from ω-3 FA may play an important role in the resolution of IBD, especially in animals and patients given dietary supplements of DHA and EPA.
Nitrated Fatty Acids
Nitrated fatty acids (NO2-FA) are also a recently discovered class of antiinflammatory lipid mediators.96,97 These molecules are present endogenously and are defined as electrophilic fatty acids containing a nitro functional group attached to a carbon–carbon double bond.98 Fatty acid nitration can occur in an acidic milieu,99,100 such as ischemic environments,101 and may be formed in the acidic gastric compartment with dietary nitrite and PUFA. These molecules are believed to be the product of reactions between free radical reactive nitrogen species and PUFAs. In vitro, nitrated linoleic acid (LNO2) has been shown to regulate vessel relaxation by cyclic guanosine monophosphate (cGMP)-dependent and -independent mechanisms and to modulate inflammatory responses, including inhibition of neutrophil function and platelet activation via a mechanism involving cyclic adenosine monophosphate (cAMP).102,103 Nitrated oleic acid (OA-NO2) and LNO2 have also been shown to: 1) upregulate heme-oxygenase 1 (HO-1) expression104; 2) serve as potent PPAR-α, δ, and γ ligands that rival or exceed fibrates and thiazolidinediones in their ability to mediate PPAR activation98,105,106; 3) react as strong electrophiles that covalently bind biological nucleophiles such as glutathione and protein His and Cys residues, thus implicating them in regulation of protein structure/function107,108; 4) inhibit cytokine release in LPS stimulated inflammatory cells via adduction to the p65 unit of NF-κB109; and, importantly, 5) inhibit the onset of induced IBD in rodent models.110
LIPIDS AND THE ANTIINFLAMMATORY PPAR-γ PATHWAY
PPAR-γ is a member of the superfamily of nuclear hormone receptors that function as transcription factors, modulating glucose and lipid metabolism, inflammation, and cell proliferation. PPAR-γ forms heterodimers with retinoid X receptors, which bind to PPAR response elements, and regulates transcription of target genes. The mechanisms by which PPAR-γ attenuates inflammation are complex and incompletely understood, with PPAR-γ activation believed, in part, to repress NF-κB.111 Although present in several tissues, PPAR-γ is highly concentrated in the colon and plays a role in IBD.112 Abnormally low PPAR-γ expression occurs in patients with UC,113 and mice with disrupted PPAR-γ gene expression in epithelial cells have significantly greater disease activity and inflammatory cytokine production compared to littermates with normal PPAR-γ expression.114 In another study, PPAR-γ deficient mice had increased intestinal ischemia/reperfusion injury.115 Also of interest, the PPAR-γ expressing mice displayed downregulated ICAM-1 expression when given a synthetic PPAR-γ activating ligand.115
PPAR-γ agonists are potential therapeutic agents for treating IBD. Well-known synthetic ligands include the antidiabetic thiazolidinediones and 5-aminosalicylic acid (5-ASA).116,117 5-ASAs have widely been used in the treatment of IBD, and there is also a potential role for their use in the treatment of colon cancer, for which IBD patients are at greater risk.112,118 A small clinical trial has also shown potential therapeutic benefit from Rosiglitazone, a thiazolidinedione, in UC patients.119
Many lipids and eicosanoids are plausible endogenous ligands for PPAR-γ, although clinically relevant ligands have been difficult to identify. Not all lipids that dock at the ligand binding domain cause a conformational change in the receptor. Electrophilic lipids that can bind with a critical thiol (Cys285) within the ligand binding domain, thereby forming a covalent bond and prolonging receptor activation, appear to be the best candidates.120,121 The most studied endogenous eicosanoid is 15-deoxy-prostaglandin J2. PPAR-γ in the colon may work as a lipid “sampler,” able to bind many lipids (including more than one at a time) derived from the diet and local bacterial metabolism, and then dictate various transcription processes, depending on which ligands bind the receptor.111 Recently, two new classes of endogenous PPAR-γ ligands have been identified: nitrated fatty acids and EFOX.122–124 These molecules are strongly electrophilic and rival the thiazolidinediones for potency. These ligands differ significantly from Rosaglitazone in that they appear to be “partial” agonists that induce selective gene expression, which is an aspect of growing importance in the field of PPAR-γ drug discovery. Potential dietary ligands include ω-3 FA, LA, curcumin (from turmeric), capsaicin (from peppers), several flavonoids, and conjugated linoleic acid (CLA).125
CLA is a group of naturally occurring fatty acids that are positional isomers of LA that are typically found in meat and dairy products from grass-fed ruminants. The isomer that shows most promise as an antiinflammatory signaling molecule is c9-t11-CLA, although some degree of a racemic mixture may be biologically important.126 Several studies have shown that CLA decreases TNF-α and other inflammatory cytokines from various cell types after exposure to LPS, including intestinal epithelia cells (Caco-2),127 bone marrow-derived dendritic cells (BMDC),128 and peripheral blood mononuclear cells.129,130 In a murine model of LPS-induced inflammation, mice fed diets rich in CLA had less of a rise in some serum proinflammatory cytokines, and their BMDC had increased IL-10 and less TLR4 mRNA compared to mice on a low-CLA diet. Nuclear expression of PPAR-γ was higher in CLA-fed mice before and after LPS stimulation. The TLR4 expression, but not that of the coreceptor, was reversed when the cells were treated with a PPAR-γ inhibitor, suggesting that CLA induction of PPAR-γ may suppress TLR4.131 In a contradictory study, intestinal cells (Caco-2) were given an inflammatory stimulus in the presence of various lipids. IL-6 and IL-8 production was decreased and PPAR-γ expression was increased by troglitazone and ω-3 PUFA, but no effect was seen with CLA.132 These effects were reversed in the presence of PPAR-γ antagonist.
Murine models of IBD suggest that CLA does activate PPAR-γ.133 In an experimental colitis mouse model using dextran sodium sulfate, mice were fed a diet supplemented with CLA. These mice had decreased clinical and histological colitis, increased mRNA expression of PPAR-γ, and decreased expression of TNF-α and NF-κB. The same experiment was performed with colonic PPAR-γ null mice, and the protective effects from CLA were not seen in this group.134 In a similar study, mice (including immune cell/colonic PPAR-γ null mice) were given agents to induce colitis as well as colorectal cancer while being supplemented with CLA. The PPAR-γ expressing mice had milder colitis and reduced adenocarcinoma, which was not seen in the null mice.135 To date, no studies of CLA have been carried out in humans with IBD.
CONCLUSION
Unsaturated fatty acid-derived mediators contribute to both the generation and resolution of inflammation. The high LA content of the Western diet may promote the development of IBD and other chronic inflammatory conditions, at least in part through arachidonic acid-derived eicosanoid production. In IBD, abnormalities in lipid utilization and metabolism alter cell signaling along multiple pathways, resulting in inappropriate perpetuation of inflammation and likely contribute to its pathogenesis. The impairments in lipid metabolism associated with IBD result in defective mucous production and intestinal barrier function, altered FA uptake for eicosanoid production, and overproduction of inflammatory signaling molecules by various cellular mechanisms.
There are multiple studies in animal models that demonstrate the efficacy of ω-3 FA and CLA as dietary-based treatments for IBD. However, there has been little insight generated as to the mechanism of their antiinflammatory properties. These antiinflammatory FA may directly compete as substrate for eicosanoid production, or may be converted into modified FA such as lipoxins, resolvins, nitrated fatty acids, and EFOX derivatives. The recent discovery of an ω-3 FA receptor with downstream antiinflammatory signaling actions is another possible explanation. In this regard, current studies in our laboratory and elsewhere are addressing these important signaling molecules in the context of pathological inflammation. Additionally, the ideal balance of dietary lipids in the context of IBD is an area of active investigation; dietary manipulation of fat may help attenuate inflammation and maintain remission in IBD. As more is discovered about the functions of individual lipids during inflammation, more directed therapies for IBD may become available.
REFERENCES
- 1.Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361:2066–2078. doi: 10.1056/NEJMra0804647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peyrin-Biroulet L, Loftus EV, Jr., Colombel JF, et al. The natural history of adult Crohn’s disease in population-based cohorts. Am J Gas-troenterol. 2010;105:289–297. doi: 10.1038/ajg.2009.579. [DOI] [PubMed] [Google Scholar]
- 3.Marrero F, Qadeer MA, Lashner BA. Severe complications of inflammatory bowel disease. Med Clin North Am. 2008;92:671–686. doi: 10.1016/j.mcna.2007.12.002. ix. [DOI] [PubMed] [Google Scholar]
- 4.Kaser A, Zeissig S, Blumberg RS. Inflammatory bowel disease. Annu Rev Immunol. 2010;28:573–621. doi: 10.1146/annurev-immunol-030409-101225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shih DQ, Targan SR, McGovern D. Recent advances in IBD pathogenesis: genetics and immunobiology. Curr Gastroenterol Rep. 2008;10:568–575. doi: 10.1007/s11894-008-0104-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weisburger JH. Dietary fat and risk of chronic disease: mechanistic insights from experimental studies. J Am Diet Assoc. 1997;97:S16–S23. doi: 10.1016/s0002-8223(97)00725-6. [DOI] [PubMed] [Google Scholar]
- 7.Huibregtse IL, van Lent AU, van Deventer SJ. Immunopathogenesis of IBD: insufficient suppressor function in the gut? Gut. 2007;56:584–592. doi: 10.1136/gut.2006.103523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abraham C, Cho J. Interleukin-23/Th17 pathways and inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:1090–1100. doi: 10.1002/ibd.20894. [DOI] [PubMed] [Google Scholar]
- 9.Wolowczuk I, Verwaerde C, Viltart O, et al. Feeding our immune system: impact on metabolism. Clin Dev Immunol. 2008;2008:639803. doi: 10.1155/2008/639803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leslie CC. Regulation of arachidonic acid availability for eicosanoid production. Biochem Cell Biol. 2004;82:1–17. doi: 10.1139/o03-080. [DOI] [PubMed] [Google Scholar]
- 11.Cathcart MK. Signal-activated phospholipase regulation of leukocyte chemotaxis. J Lipid Res. 2009;50(suppl):S231–S236. doi: 10.1194/jlr.R800096-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Calder PC. Dietary modification of inflammation with lipids. Proc Nutr Soc. 2002;61:345–358. doi: 10.1079/pns2002166. [DOI] [PubMed] [Google Scholar]
- 13.Ferrer R, Moreno JJ. Role of eicosanoids on intestinal epithelial homeostasis. Biochem Pharmacol. 2010;80:431–438. doi: 10.1016/j.bcp.2010.04.033. [DOI] [PubMed] [Google Scholar]
- 14.Zmijewski JW, Landar A, Watanabe N, et al. Cell signalling by oxidized lipids and the role of reactive oxygen species in the endothe-lium. Biochem Soc Trans. 2005;33:1385–1389. doi: 10.1042/BST20051385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gayarre J, Sanchez D, Sanchez-Gomez FJ, et al. Addition of electrophilic lipids to actin alters filament structure. Biochem Biophys Res Commun. 2006;349:1387–1393. doi: 10.1016/j.bbrc.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Sanchez-Gomez FJ, Gayarre J, Avellano MI, et al. Direct evidence for the covalent modification of glutathione-S-transferase P1-1 by electrophilic prostaglandins: implications for enzyme inactivation and cell survival. Arch Biochem Biophys. 2007;457:150–159. doi: 10.1016/j.abb.2006.10.032. [DOI] [PubMed] [Google Scholar]
- 17.Levonen AL, Landar A, Ramachandran A, et al. Cellular mechanisms of redox cell signalling: role of cysteine modification in controlling antioxidant defences in response to electrophilic lipid oxidation products. Biochem J. 2004;378:373–382. doi: 10.1042/BJ20031049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shibata T, Yamada T, Ishii T, et al. Thioredoxin as a molecular target of cyclopentenone prostaglandins. J Biol Chem. 2003;278:26046–26054. doi: 10.1074/jbc.M303690200. [DOI] [PubMed] [Google Scholar]
- 19.Yu X, Egner PA, Wakabayashi J, et al. Nrf2-mediated induction of cytoprotective enzymes by 15-deoxy-Delta12,14-prostaglandin J2 is attenuated by alkenal/one oxidoreductase. J Biol Chem. 2006;281:26245. doi: 10.1074/jbc.M604620200. [DOI] [PubMed] [Google Scholar]
- 20.Crabb JW, O’Neil J, Miyagi M, et al. Hydroxynonenal inactivates cathepsin B by forming Michael adducts with active site residues. Protein Sci. 2002;11:831–840. doi: 10.1110/ps.4400102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uchida K, Stadtman ER. Modification of histidine residues in proteins by reaction with 4-hydroxynonenal. Proc Natl Acad Sci U S A. 1992;89:4544–4548. doi: 10.1073/pnas.89.10.4544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ishii T, Tatsuda E, Kumazawa S, et al. Molecular basis of enzyme inactivation by an endogenous electrophile 4-hydroxy-2-nonenal: identification of modification sites in glyceraldehyde-3-phosphate de-hydrogenase. Biochemistry. 2003;42:3474–3480. doi: 10.1021/bi027172o. [DOI] [PubMed] [Google Scholar]
- 23.Uchida K, Stadtman ER. Covalent attachment of 4-hydroxynonenal to glyceraldehyde-3-phosphate dehydrogenase. A possible involvement of intra- and intermolecular cross-linking reaction. J Biol Chem. 1993;268:6388–6393. [PubMed] [Google Scholar]
- 24.Holtzclaw WD, Dinkova-Kostova AT, Talalay P. Protection against electrophile and oxidative stress by induction of phase 2 genes: the quest for the elusive sensor that responds to inducers. Adv Enzyme Regul. 2004;44:335–367. doi: 10.1016/j.advenzreg.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 25.Liebler DC. Protein damage by reactive electrophiles: targets and consequences. Chem Res Toxicol. 2008;21:117–128. doi: 10.1021/tx700235t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tjonneland A, Overvad K, Bergmann MM, et al. Linoleic acid, a dietary n-6 polyunsaturated fatty acid, and the aetiology of ulcerative colitis: a nested case-control study within a European prospective cohort study. Gut. 2009;58:1606–1611. doi: 10.1136/gut.2008.169078. [DOI] [PubMed] [Google Scholar]
- 27.Alzoghaibi MA, Walsh SW, Willey A, et al. Linoleic acid, but not oleic acid, upregulates the production of interleukin-8 by human intestinal smooth muscle cells isolated from patients with Crohn’s disease. Clin Nutr. 2003;22:529–535. doi: 10.1016/s0261-5614(03)00083-9. [DOI] [PubMed] [Google Scholar]
- 28.Ramakers JD, Mensink RP, Verstege MI, et al. An arachidonic acid-enriched diet does not result in more colonic inflammation as compared with fish oil- or oleic acid-enriched diets in mice with experimental colitis. Br J Nutr. 2008;100:347–354. doi: 10.1017/S0007114507901257. [DOI] [PubMed] [Google Scholar]
- 29.Fernandez-Banares F, Esteve-Comas M, Mane J, et al. Changes in mucosal fatty acid profile in inflammatory bowel disease and in experimental colitis: a common response to bowel inflammation. Clin Nutr. 1997;16:177–183. doi: 10.1016/s0261-5614(97)80003-9. [DOI] [PubMed] [Google Scholar]
- 30.Buhner S, Nagel E, Korber J, et al. Ileal and colonic fatty acid profiles in patients with active Crohn’s disease. Gut. 1994;35:1424–1428. doi: 10.1136/gut.35.10.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pacheco S, Hillier K, Smith C. Increased arachidonic acid levels in phospholipids of human colonic mucosa in inflammatory bowel disease. Clin Sci (Lond) 1987;73:361–364. doi: 10.1042/cs0730361. [DOI] [PubMed] [Google Scholar]
- 32.Nishida T, Miwa H, Shigematsu A, et al. Increased arachidonic acid composition of phospholipids in colonic mucosa from patients with active ulcerative colitis. Gut. 1987;28:1002–1007. doi: 10.1136/gut.28.8.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nieto N, Giron MD, Suarez MD, et al. Changes in plasma and colonic mucosa fatty acid profiles in rats with ulcerative colitis induced by trinitrobenzene sulfonic acid. Dig Dis Sci. 2009;1998(43):2688–2695. doi: 10.1023/a:1026607428716. [DOI] [PubMed] [Google Scholar]
- 34.Harvey KA, Walker CL, Pavlina TM, et al. Long-chain saturated fatty acids induce pro-inflammatory responses and impact endothelial cell growth. Clin Nutr. 2010;29:492–500. doi: 10.1016/j.clnu.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 35.Esteve-Comas M, Nunez MC, Fernandez-Banares F, et al. Abnormal plasma polyunsaturated fatty acid pattern in non-active inflammatory bowel disease. Gut. 1993;34:1370–1373. doi: 10.1136/gut.34.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Esteve-Comas M, Ramirez M, Fernandez-Banares F, et al. Plasma polyunsaturated fatty acid pattern in active inflammatory bowel disease. Gut. 1992;33:1365–1369. doi: 10.1136/gut.33.10.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ueda Y, Kawakami Y, Kunii D, et al. Elevated concentrations of linoleic acid in erythrocyte membrane phospholipids in patients with inflammatory bowel disease. Nutr Res. 2008;28:239–244. doi: 10.1016/j.nutres.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 38.Morita H, Nakanishi K, Dohi T, et al. Phospholipid turnover in the inflamed intestinal mucosa: arachidonic acid-rich phosphatidyl/plas-menyl-ethanolamine in the mucosa in inflammatory bowel disease. J Gastroenterol. 1999;34:46–53. doi: 10.1007/s005350050215. [DOI] [PubMed] [Google Scholar]
- 39.Jupp J, Hillier K, Elliott DH, et al. Colonic expression of leukotri-ene-pathway enzymes in inflammatory bowel diseases. Inflamm Bowel Dis. 2007;13:537–546. doi: 10.1002/ibd.20094. [DOI] [PubMed] [Google Scholar]
- 40.Sharon P, Stenson WF. Enhanced synthesis of leukotriene B4 by co-lonic mucosa in inflammatory bowel disease. Gastroenterology. 1984;86:453–460. [PubMed] [Google Scholar]
- 41.Nielsen OH, Ahnfelt-Ronne I, Elmgreen J. Abnormal metabolism of arachidonic acid in chronic inflammatory bowel disease: enhanced release of leucotriene B4 from activated neutrophils. Gut. 1987;28:181–185. doi: 10.1136/gut.28.2.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wiercinska-Drapalo A, Flisiak R, Prokopowicz D. Mucosal and plasma prostaglandin E2 in ulcerative colitis. Hepatogastroenterol-ogy. 1999;46:2338–2342. [PubMed] [Google Scholar]
- 43.Sasaki S, Hirata I, Maemura K, et al. Prostaglandin E2 inhibits lesion formation in dextran sodium sulphate-induced colitis in rats and reduces the levels of mucosal inflammatory cytokines. Scand J Immunol. 2000;51:23–28. doi: 10.1046/j.1365-3083.2000.00623.x. [DOI] [PubMed] [Google Scholar]
- 44.Heimerl S, Moehle C, Zahn A, et al. Alterations in intestinal fatty acid metabolism in inflammatory bowel disease. Biochim Biophys Acta. 2006;1762:341–350. doi: 10.1016/j.bbadis.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 45.Schwenk RW, Holloway GP, Luiken JJ, et al. Fatty acid transport across the cell membrane: regulation by fatty acid transporters. Pros-taglandins Leukot Essent Fatty Acids. 2010;82:149–152. doi: 10.1016/j.plefa.2010.02.029. [DOI] [PubMed] [Google Scholar]
- 46.Wiercinska-Drapalo A, Jaroszewicz J, Siwak E, et al. Intestinal fatty acid binding protein (I-FABP) as a possible biomarker of ileitis in patients with ulcerative colitis. Regul Pept. 2008;147:25–28. doi: 10.1016/j.regpep.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 47.Reiff C, Delday M, Rucklidge G, et al. Balancing inflammatory, lipid, and xenobiotic signaling pathways by VSL#3, a biotherapeutic agent, in the treatment of inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:1721–1736. doi: 10.1002/ibd.20999. [DOI] [PubMed] [Google Scholar]
- 48.Lichtenberger LM. The hydrophobic barrier properties of gastrointestinal mucus. Annu Rev Physiol. 1995;57:565–583. doi: 10.1146/annurev.ph.57.030195.003025. [DOI] [PubMed] [Google Scholar]
- 49.Podolsky DK. Inflammatory bowel disease. N Engl J Med. 2002;347:417–429. doi: 10.1056/NEJMra020831. [DOI] [PubMed] [Google Scholar]
- 50.Ehehalt R, Wagenblast J, Erben G, et al. Phosphatidylcholine and lysophosphatidylcholine in intestinal mucus of ulcerative colitis patients. A quantitative approach by nanoElectrospray-tandem mass spectrometry. Scand J Gastroenterol. 2004;39:737–742. doi: 10.1080/00365520410006233. [DOI] [PubMed] [Google Scholar]
- 51.Sawai T, Drongowski RA, Lampman RW, et al. The effect of phospholipids and fatty acids on tight-junction permeability and bacterial translocation. Pediatr Surg Int. 2001;17:269–274. doi: 10.1007/s003830100592. [DOI] [PubMed] [Google Scholar]
- 52.Fabia R, Ar’Rajab A, Willen R, et al. Effects of phosphatidylcholine and phosphatidylinositol on acetic-acid-induced colitis in the rat. Digestion. 1992;53:35–44. doi: 10.1159/000200969. [DOI] [PubMed] [Google Scholar]
- 53.Mourelle M, Guarner F, Malagelada JR. Polyunsaturated phosphati-dylcholine prevents stricture formation in a rat model of colitis. Gastroenterology. 1996;110:1093–1097. doi: 10.1053/gast.1996.v110.pm8612998. [DOI] [PubMed] [Google Scholar]
- 54.Podolsky DK, Isselbacher KJ. Composition of human colonic mucin. Selective alteration in inflammatory bowel disease. J Clin Invest. 1983;72:142–153. doi: 10.1172/JCI110952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Podolsky DK, Isselbacher KJ. Glycoprotein composition of colonic mucosa. Specific alterations in ulcerative colitis. Gastroenterology. 1984;87:991–998. [PubMed] [Google Scholar]
- 56.Ballou LR, Laulederkind SJ, Rosloniec EF, et al. Ceramide signalling and the immune response. Biochim Biophys Acta. 1996;1301:273–287. doi: 10.1016/0005-2760(96)00004-5. [DOI] [PubMed] [Google Scholar]
- 57.Bauer J, Liebisch G, Hofmann C, et al. Lipid alterations in experimental murine colitis: role of ceramide and imipramine for matrix metalloproteinase-1 expression. PLoS One. 2009;4:e7197. doi: 10.1371/journal.pone.0007197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sengupta N, MacDonald TT. The role of matrix metalloproteinases in stromal/epithelial interactions in the gut. Physiology (Bethesda) 2007;22:401–409. doi: 10.1152/physiol.00027.2007. [DOI] [PubMed] [Google Scholar]
- 59.Ravi A, Garg P, Sitaraman SV. Matrix metalloproteinases in inflammatory bowel disease: boon or a bane? Inflamm Bowel Dis. 2007;13:97–107. doi: 10.1002/ibd.20011. [DOI] [PubMed] [Google Scholar]
- 60.Meijer MJ, Mieremet-Ooms MA, van der Zon AM, et al. Increased mucosal matrix metalloproteinase-1, −2, −3 and −9 activity in patients with inflammatory bowel disease and the relation with Crohn’s disease phenotype. Dig Liver Dis. 2007;39:733–739. doi: 10.1016/j.dld.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 61.Meijer MJ, Mieremet-Ooms MA, van Hogezand RA, et al. Role of matrix metalloproteinase, tissue inhibitor of metalloproteinase and tumor necrosis factor-alpha single nucleotide gene polymorphisms in inflammatory bowel disease. World J Gastroenterol. 2007;13:2960–2966. doi: 10.3748/wjg.v13.i21.2960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pedersen G, Saermark T, Kirkegaard T, et al. Spontaneous and cytokine induced expression and activity of matrix metalloprotei-nases in human colonic epithelium. Clin Exp Immunol. 2009;155:257–265. doi: 10.1111/j.1365-2249.2008.03836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hrabovsky V, Zadak Z, Blaha V, et al. Cholesterol metabolism in active Crohn’s disease. Wien Klin Wochenschr. 2009;121:270–275. doi: 10.1007/s00508-009-1150-6. [DOI] [PubMed] [Google Scholar]
- 64.Chiarla C, Giovannini I, Giuliante F, et al. Severe hypocholesterolemia in surgical patients, sepsis, and critical illness. J Crit Care. 2010;25:361. doi: 10.1016/j.jcrc.2009.08.006. e7–361. e12. [DOI] [PubMed] [Google Scholar]
- 65.Levy E, Rizwan Y, Thibault L, et al. Altered lipid profile, lipoprotein composition, and oxidant and antioxidant status in pediatric Crohn disease. Am J Clin Nutr. 2000;71:807–815. doi: 10.1093/ajcn/71.3.807. [DOI] [PubMed] [Google Scholar]
- 66.Ripolles Piquer B, Nazih H, Bourreille A, et al. Altered lipid, apolipoprotein, and lipoprotein profiles in inflammatory bowel disease: consequences on the cholesterol efflux capacity of serum using Fu5AH cell system. Metabolism. 2006;55:980–988. doi: 10.1016/j.metabol.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 67.Malle E, Steinmetz A, Raynes JG. Serum amyloid A (SAA): an acute phase protein and apolipoprotein. Atherosclerosis. 1993;102:131–146. doi: 10.1016/0021-9150(93)90155-n. [DOI] [PubMed] [Google Scholar]
- 68.Jousilahti P, Salomaa V, Rasi V, et al. The association of c-reactive protein, serum amyloid a and fibrinogen with prevalent coronary heart disease—baseline findings of the PAIS project. Atherosclerosis. 2001;156:451–456. doi: 10.1016/s0021-9150(00)00681-x. [DOI] [PubMed] [Google Scholar]
- 69.Dagli N, Poyrazoglu OK, Dagli AF, et al. Is inflammatory bowel disease a risk factor for early atherosclerosis? Angiology. 2010;61:198–204. doi: 10.1177/0003319709333869. [DOI] [PubMed] [Google Scholar]
- 70.Hillier K, Jewell R, Dorrell L, et al. Incorporation of fatty acids from fish oil and olive oil into colonic mucosal lipids and effects upon eicosanoid synthesis in inflammatory bowel disease. Gut. 1991;32:1151–1155. doi: 10.1136/gut.32.10.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Calder PC. Polyunsaturated fatty acids, inflammatory processes and inflammatory bowel diseases. Mol Nutr Food Res. 2008;52:885–897. doi: 10.1002/mnfr.200700289. [DOI] [PubMed] [Google Scholar]
- 72.Belluzzi A. Polyunsaturated fatty acids (n-3 PUFAs) and inflammatory bowel disease (IBD): pathogenesis and treatment. Eur Rev Med Pharmacol Sci. 2004;8:225–229. [PubMed] [Google Scholar]
- 73.Feagan BG, Sandborn WJ, Mittmann U, et al. Omega-3 free fatty acids for the maintenance of remission in Crohn disease: the EPIC Randomized Controlled Trials. JAMA. 2008;299:1690–1697. doi: 10.1001/jama.299.14.1690. [DOI] [PubMed] [Google Scholar]
- 74.MacLean CH, Mojica WA, Newberry SJ, et al. Systematic review of the effects of n-3 fatty acids in inflammatory bowel disease. Am J Clin Nutr. 2005;82:611–619. doi: 10.1093/ajcn.82.3.611. [DOI] [PubMed] [Google Scholar]
- 75.Turner D, Zlotkin SH, Shah PS, et al. Omega 3 fatty acids (fish oil) for maintenance of remission in Crohn’s disease. Cochrane Database Syst Rev. 2009:CD006320. doi: 10.1002/14651858.CD006320.pub2. [DOI] [PubMed] [Google Scholar]
- 76.Turner D, Steinhart AH, Griffiths AM. Omega 3 fatty acids (fish oil) for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev. 2007:CD006443. doi: 10.1002/14651858.CD006443.pub2. [DOI] [PubMed] [Google Scholar]
- 77.Oh da Y, Talukdar S, Bae EJ, et al. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell. 2010;142:687–698. doi: 10.1016/j.cell.2010.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Akobeng AK, Thomas AG. Enteral nutrition for maintenance of remission in Crohn’s disease. Cochrane Database Syst Rev. 2007:CD005984. doi: 10.1002/14651858.CD005984.pub2. [DOI] [PubMed] [Google Scholar]
- 79.Smith PA. Nutritional therapy for active Crohn’s disease. World J Gastroenterol. 2008;14:4420–4423. doi: 10.3748/wjg.14.4420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bamba T, Shimoyama T, Sasaki M, et al. Dietary fat attenuates the benefits of an elemental diet in active Crohn’s disease: a randomized, controlled trial. Eur J Gastroenterol Hepatol. 2003;15:151–157. doi: 10.1097/00042737-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 81.Gassull MA, Fernandez-Banares F, Cabre E, et al. Fat composition may be a clue to explain the primary therapeutic effect of enteral nutrition in Crohn’s disease: results of a double blind randomised multicentre European trial. Gut. 2002;51:164–168. doi: 10.1136/gut.51.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Leiper K, Woolner J, Mullan MM, et al. A randomised controlled trial of high versus low long chain triglyceride whole protein feed in active Crohn’s disease. Gut. 2001;49:790–794. doi: 10.1136/gut.49.6.790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hamer HM, Jonkers D, Venema K, et al. Review article: the role of butyrate on colonic function. Aliment Pharmacol Ther. 2008;27:104–119. doi: 10.1111/j.1365-2036.2007.03562.x. [DOI] [PubMed] [Google Scholar]
- 84.Kles KA, Chang EB. Short-chain fatty acids impact on intestinal adaptation, inflammation, carcinoma, and failure. Gastroenterology. 2006;130:S100–S105. doi: 10.1053/j.gastro.2005.11.048. [DOI] [PubMed] [Google Scholar]
- 85.Sturm A, Dignass AU. Epithelial restitution and wound healing in inflammatory bowel disease. World J Gastroenterol. 2008;14:348–353. doi: 10.3748/wjg.14.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Treem WR, Ahsan N, Shoup M, et al. Fecal short-chain fatty acids in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 1994;18:159–164. doi: 10.1097/00005176-199402000-00007. [DOI] [PubMed] [Google Scholar]
- 87.Weylandt KH, Kang JX, Wiedenmann B, et al. Lipoxins and resolvins in inflammatory bowel disease. Inflamm Bowel Dis. 2007;13:797–799. doi: 10.1002/ibd.20109. [DOI] [PubMed] [Google Scholar]
- 88.Serhan CN. Systems approach to inflammation resolution: identification of novel antiinflammatory and pro-resolving mediators. J Thromb Haemost. 2009;7(suppl 1):44–48. doi: 10.1111/j.1538-7836.2009.03396.x. [DOI] [PubMed] [Google Scholar]
- 89.Goh J, Godson C, Brady HR, et al. Lipoxins: pro-resolution lipid mediators in intestinal inflammation. Gastroenterology. 2003;124:1043–1054. doi: 10.1053/gast.2003.50154. [DOI] [PubMed] [Google Scholar]
- 90.Mangino MJ, Brounts L, Harms B, et al. Lipoxin biosynthesis in inflammatory bowel disease. Prostaglandins Other Lipid Mediat. 2006;79:84–92. doi: 10.1016/j.prostaglandins.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 91.Levy BD. Resolvins and protectins: natural pharmacophores for resolution biology. Prostaglandins Leukot Essent Fatty Acids. 2010;82:327–332. doi: 10.1016/j.plefa.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Arita M, Yoshida M, Hong S, et al. Resolvin E1, an endogenous lipid mediator derived from omega-3 eicosapentaenoic acid, protects against 2,4,6-trinitrobenzene sulfonic acid-induced colitis. Proc Natl Acad Sci U S A. 2005;102:7671–7676. doi: 10.1073/pnas.0409271102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ishida T, Yoshida M, Arita M, et al. Resolvin E1, an endogenous lipid mediator derived from eicosapentaenoic acid, prevents dextran sulfate sodium-induced colitis. Inflamm Bowel Dis. 2010;16:87–95. doi: 10.1002/ibd.21029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Campbell EL, MacManus CF, Kominsky DJ, et al. Resolvin E1-induced intestinal alkaline phosphatase promotes resolution of inflammation through LPS detoxification. Proc Natl Acad Sci U S A. 2010;107:14298–14303. doi: 10.1073/pnas.0914730107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Groeger A, Cipollina C, Cole M, et al. Cyclooxygenase-2 generates anti-inflammatory mediators from omega-3 fatty acids. Nat Chem Biol. 2010;6:433–441. doi: 10.1038/nchembio.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Baker PR, Schopfer FJ, Sweeney S, et al. Red cell membrane and plasma linoleic acid nitration products: synthesis, clinical identification, and quantitation. Proc Natl Acad Sci U S A. 2004;101:11577–11582. doi: 10.1073/pnas.0402587101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Baker PRS, Lin Y, Schopfer FJ, et al. Fatty acid transduction of nitric oxide signaling: multiple nitrated unsaturated fatty acid derivatives exist in human blood and urine and serve as endogenous PPAR ligands. J Biol Chem. 2005;280:42464–42475. doi: 10.1074/jbc.M504212200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Baker PR, Schopfer FJ, O’Donnell VB, et al. Convergence of nitric oxide and lipid signaling: anti-inflammatory nitro-fatty acids. Free Radic Biol Med. 2009;46:989–1003. doi: 10.1016/j.freeradbiomed.2008.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Napolitano A, Camera E, Picardo M, et al. Acid-promoted reactions of ethyl linoleate with nitrite ions: formation and structural characterization of isomeric nitroalkene, nitrohydroxy, and novel 3-nitro-1,5-hexadiene and 1,5-dinitro-1, 3-pentadiene products. J.Org.Chem. 2000;65:4853–4860. doi: 10.1021/jo000090q. [DOI] [PubMed] [Google Scholar]
- 100.Napolitano A, Crescenzi O, Camera E, et al. The acid-promoted reaction of ethyl linoleate with nitrite. New insights from 15N–label-ing and peculier reactivity of a model skipped diene. Tetrahedron. 2004;58:5061–5067. [Google Scholar]
- 101.Nadtochiy SM, Baker PRS, Freeman BA, et al. Nitration of linoleic acid in mitochondria during ischemic preconditioning: cardioprotec-tion via activation of mitochondrial Hþ leak. Cardiovasc Res. 2008 [Epub ahead of print] [Google Scholar]
- 102.Coles B, Bloodsworth A, Clark SR, et al. Nitrolinoleate inhibits superoxide generation, degranulation, and integrin expression by human neutrophils: novel antiinflammatory properties of nitric oxide-derived reactive species in vascular cells. Circ Res. 2002;91:375–381. doi: 10.1161/01.res.0000032114.68919.ef. [DOI] [PubMed] [Google Scholar]
- 103.Coles B, Bloodsworth A, Eiserich JP, et al. Nitrolinoleate inhibits platelet activation by attenuating calcium mobilization and inducing phosphorylation of vasodilator-stimulated phosphoprotein through elevation of cAMP. J Biol Chem. 2002;277:5832–5840. doi: 10.1074/jbc.M105209200. [DOI] [PubMed] [Google Scholar]
- 104.Wright MM, Schopfer FJ, Baker PR, et al. Fatty acid transduction of nitric oxide signaling: nitrolinoleic acid potently activates endothelial heme oxygenase 1 expression. Proc Natl Acad Sci U S A. 2006;103:4299–4304. doi: 10.1073/pnas.0506541103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Li Y, Zhang J, Schopfer FJ, et al. Molecular recognition of nitrated fatty acids by PPAR gamma. Nat Struct Mol Biol. 2008;15:865–867. doi: 10.1038/nsmb.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Schopfer FJ, Lin Y, Baker PR, et al. Nitrolinoleic acid: an endogenous peroxisome proliferator-activated receptor gamma ligand. Proc Natl Acad Sci U S A. 2005;102:2340–2345. doi: 10.1073/pnas.0408384102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Baker LM, Baker PR, Golin-Bisello F, et al. Nitro-fatty acid reaction with glutathione and cysteine. Kinetic analysis of thiol alkylation by a Michael addition reaction. J Biol Chem. 2007;282:31085–31093. doi: 10.1074/jbc.M704085200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Batthyany C, Schopfer FJ, Baker PR, et al. Reversible post-transla-tional modification of proteins by nitrated fatty acids in vivo. J Biol Chem. 2006;281:20450–20463. doi: 10.1074/jbc.M602814200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cui T, Schopfer FJ, Zhang J, et al. Nitrated fatty acids: Endogenous anti-inflammatory signaling mediators. J Biol Chem. 2006;281:35686–35698. doi: 10.1074/jbc.M603357200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Borniquel S, Jansson EA, Cole MP, et al. Nitrated oleic acid up-regulates PPAR-gamma and attenuates experimental inflammatory bowel disease. Free Radic Biol Med. 2010;48:499–505. doi: 10.1016/j.freeradbiomed.2009.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Varga T, Nagy L. Nuclear receptors, transcription factors linking lipid metabolism and immunity: the case of peroxisome proliferator-activated receptor gamma. Eur J Clin Invest. 2008;38:695–707. doi: 10.1111/j.1365-2362.2008.02022.x. [DOI] [PubMed] [Google Scholar]
- 112.Dubuquoy L, Rousseaux C, Thuru X, et al. PPAR-gamma as a new therapeutic target in inflammatory bowel diseases. Gut. 2006;55:1341–1349. doi: 10.1136/gut.2006.093484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Dubuquoy L, Jansson EA, Deeb S, et al. Impaired expression of peroxisome proliferator-activated receptor gamma in ulcerative colitis. Gastroenterology. 2003;124:1265–1276. doi: 10.1016/s0016-5085(03)00271-3. [DOI] [PubMed] [Google Scholar]
- 114.Adachi M, Kurotani R, Morimura K, et al. Peroxisome proliferator activated receptor gamma in colonic epithelial cells protects against experimental inflammatory bowel disease. Gut. 2006;55:1104–1113. doi: 10.1136/gut.2005.081745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Nakajima A, Wada K, Miki H, et al. Endogenous PPAR gamma mediates anti-inflammatory activity in murine ischemia-reperfusion injury. Gastroenterology. 2001;120:460–469. doi: 10.1053/gast.2001.21191. [DOI] [PubMed] [Google Scholar]
- 116.Chen Q, Chen J, Sun T, et al. A yeast two-hybrid technology-based system for the discovery of PPARgamma agonist and antagonist. Anal Biochem. 2004;335:253–259. doi: 10.1016/j.ab.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 117.Rousseaux C, Lefebvre B, Dubuquoy L, et al. Intestinal antiinflamma-tory effect of 5-aminosalicylic acid is dependent on peroxisome pro-liferator-activated receptor-gamma. J Exp Med. 2005;201:1205–1215. doi: 10.1084/jem.20041948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Stolfi C, Pellegrini R, Franze E, et al. Molecular basis of the potential of mesalazine to prevent colorectal cancer. World J Gastroen-terol. 2008;14:4434–4439. doi: 10.3748/wjg.14.4434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lewis JD, Lichtenstein GR, Deren JJ, et al. Rosiglitazone for active ulcerative colitis: a randomized placebo-controlled trial. Gastroenter-ology. 2008;134:688–695. doi: 10.1053/j.gastro.2007.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Elbrecht A, Chen Y, Adams A, et al. L-764406 is a Partial agonist of human peroxisome proliferator-activated receptor gamma. The role of Cys313 in ligand binding. J Biol Chem. 1999;274:7913–7922. doi: 10.1074/jbc.274.12.7913. [DOI] [PubMed] [Google Scholar]
- 121.Leesnitzer LM, Parks DJ, Bledsoe RK, et al. Functional consequences of cysteine modification in the ligand binding sites of peroxisome proliferator activated receptors by GW9662. Biochemistry. 2002;41:6640–6650. doi: 10.1021/bi0159581. [DOI] [PubMed] [Google Scholar]
- 122.Schopfer FJ, Cole MP, Groeger AL, et al. Covalent peroxisome pro-liferator-activated receptor gamma adduction by nitro-fatty acids: selective ligand activity and anti-diabetic signaling actions. J Biol Chem. 2010;285:12321–12333. doi: 10.1074/jbc.M109.091512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Schopfer FJ, Lin Y, Baker PR, et al. Nitrolinoleic acid: an endogenous peroxisome proliferator-activated receptor gamma ligand. Proc Natl Acad Sci U S A. 2005;102:2340–2345. doi: 10.1073/pnas.0408384102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Groeger AL, Cipollina C, Cole MP, et al. Cyclooxygenase-2 generates anti-inflammatory mediators from omega-3 fatty acids. Nat Chem Biol. 2010;6:433–441. doi: 10.1038/nchembio.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Marion-Letellier R, Dechelotte P, Iacucci M, et al. Dietary modulation of peroxisome proliferator-activated receptor gamma. Gut. 2009;58:586–593. doi: 10.1136/gut.2008.162859. [DOI] [PubMed] [Google Scholar]
- 126.Reynolds CM, Roche HM. Conjugated linoleic acid and inflammatory cell signalling. Prostaglandins Leukot Essent Fatty Acids. 2010;82:199–204. doi: 10.1016/j.plefa.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 127.Reynolds CM, Loscher CE, Moloney AP, et al. Cis-9, trans-11-con-jugated linoleic acid but not its precursor trans-vaccenic acid attenuate inflammatory markers in the human colonic epithelial cell line Caco-2. Br J Nutr. 2008;100:13–17. doi: 10.1017/S0007114508894329. [DOI] [PubMed] [Google Scholar]
- 128.Loscher CE, Draper E, Leavy O, et al. Conjugated linoleic acid suppresses NF-kappa B activation and IL-12 production in dendritic cells through ERK-mediated IL-10 induction. J Immunol. 2005;175:4990–4998. doi: 10.4049/jimmunol.175.8.4990. [DOI] [PubMed] [Google Scholar]
- 129.Zhao L, Yin J, Li D, et al. Conjugated linoleic acid can prevent tumor necrosis factor gene expression by inhibiting nuclear factor binding activity in peripheral blood mononuclear cells from weaned pigs challenged with lipopolysaccharide. Arch Anim Nutr. 2005;59:429–438. doi: 10.1080/17450390500353333. [DOI] [PubMed] [Google Scholar]
- 130.Changhua L, Jindong Y, Defa L, et al. Conjugated linoleic acid attenuates the production and gene expression of proinflammatory cytokines in weaned pigs challenged with lipopolysaccharide. J Nutr. 2005;135:239–244. doi: 10.1093/jn/135.2.239. [DOI] [PubMed] [Google Scholar]
- 131.Reynolds CM, Draper E, Keogh B, et al. A conjugated linoleic acid-enriched beef diet attenuates lipopolysaccharide-induced inflammation in mice in part through PPARgamma-mediated suppression of toll-like receptor 4. J Nutr. 2009;139:2351–2357. doi: 10.3945/jn.109.113035. [DOI] [PubMed] [Google Scholar]
- 132.Marion-Letellier R, Butler M, Dechelotte P, et al. Comparison of cytokine modulation by natural peroxisome proliferator-activated receptor gamma ligands with synthetic ligands in intestinal-like Caco-2 cells and human dendritic cells—potential for dietary modulation of peroxisome proliferator-activated receptor gamma in intestinal inflammation. Am J Clin Nutr. 2008;87:939–948. doi: 10.1093/ajcn/87.4.939. [DOI] [PubMed] [Google Scholar]
- 133.Bassaganya-Riera J, Hontecillas R. Dietary conjugated linoleic acid and n-3 polyunsaturated fatty acids in inflammatory bowel disease. Curr Opin Clin Nutr Metab Care. 2010;13:569–573. doi: 10.1097/MCO.0b013e32833b648e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bassaganya-Riera J, Reynolds K, Martino-Catt S, et al. Activation of PPAR gamma and delta by conjugated linoleic acid mediates protection from experimental inflammatory bowel disease. Gastroenterology. 2004;127:777–791. doi: 10.1053/j.gastro.2004.06.049. [DOI] [PubMed] [Google Scholar]
- 135.Evans NP, Misyak SA, Schmelz EM, et al. Conjugated linoleic acid ameliorates inflammation-induced colorectal cancer in mice through activation of PPARgamma. J Nutr. 2010;140:515–521. doi: 10.3945/jn.109.115642. [DOI] [PMC free article] [PubMed] [Google Scholar]