Abstract
Background:
Given the paucity of research in this area, this study attempted to assess attitudes toward antipsychotic medications and its correlates among patients with schizophrenia, either on first-generation antipsychotics (FGAs) or second-generation antipsychotics (SGAs) medications.
Materials and Methods:
Structured assessments of attitudes to antipsychotics, psychopathology, insight and side-effects were carried out in 120 patients with DSM-IV schizophrenia; 89 of these were on SGAs and 31 on FGAs.
Results:
Patients had predominantly positive attitudes toward antipsychotics. Severity of side-effects was the principal correlate of attitudes, explaining 19.5% of the variance, followed by greater insight (4.2% of the variance). Other factors such as younger age, male gender, employment, higher family income, urban residence and lower symptom-severity explained only a negligible proportion of the variance (0.2%) in attitudes. Patients on SGAs had more positive views of their medications than those on FGAs. They felt more normal on their medications, believed that their thoughts were clearer on medications, felt that good things about their medications outweighed the bad and believed that their medications helped them from falling ill again. In addition, they did not feel as tired and sluggish on their medications and did not believe that medications were unnatural or controlled their bodies.
Conclusions:
Positive attitudes toward antipsychotics were common among patients with schizophrenia. Attitudes were principally determined by severity of side-effects and insight levels. Patients on SGAs had better attitudes, possibly because of less severe side-effects and greater insight among them. The importance of exploring patients’ attitudes toward their antipsychotics is highlighted by this study.
Keywords: Antipsychotics, attitudes, first-generation, schizophrenia, second-generation
INTRODUCTION
The patient's perspective of antipsychotic treatment was largely neglected until the advent of atypical or second-generation antipsychotics (SGAs) in the 1990s.[1,2] Since then, subjective experiences of antipsychotic treatment, including constructs such as attitudes toward medications, have been increasingly acknowledged as being critical to adherence and the eventual outcome of antipsychotic treatment.[2,3] It was anticipated that SGAs, which promised a similar efficacy along with a better side-effect profile than first-generation antipsychotics (FGAs), would lead to more positive attitudes toward treatment. Though the initial clinical trials seemed to suggest a trend toward superiority of SGAs in this regard,[1,4,5,6] this assumption has not been consistently borne out by empirical data. The more recent large-scale effectiveness studies have also not been able to resolve the issue of differences between FGAs and SGAs on patients’ attitudes to medications, with some suggesting more positive attitudes among those on SGAs,[7,8] whereas others failing to find any differences between FGAs and SGAs.[9,10] Even if there are differences between the two groups of antipsychotics, the underlying factors mediating these differences in attitudes are not clear. A person's attitudes to treatment can be influenced by a number of different factors. Demographic characteristics of patients appear to have little impact on attitudes, whereas psychopathology, insight, side-effects, health-beliefs and the doctor-patient relationship have been more consistently linked with attitudes across different studies.[2,3,11,12,13,14] However, whether these factors help discriminate FGAs from SGAs with regard to attitudes toward antipsychotics is not clear.
Given these considerations, the present study attempted to examine attitudes toward antipsychotics and its correlates among patients of schizophrenia either on SGAs, or FGAs. It also sought to compare patients on FGAs and SGAs on their attitudes toward antipsychotics.
MATERIALS AND METHODS
Approval and consent
The study-protocol was approved by the Research and Ethics committees of the institute. Written informed consent was obtained from all participants prior to inclusion and other ethical safeguards were also maintained during the study.
Participants
Patients aged between 18 and 60 years with a diagnosis of schizophrenia, confirmed by the Structured Clinical Interview for DSM-IV Axis I Disorders-Clinical Version I[15] were included if they had been on treatment with the same antipsychotic for a minimum of 3 months prior to inclusion. Patients with organic brain syndromes or comorbid psychiatric illnesses and substance dependence (except nicotine) and patients on antipsychotic combinations or depot preparations were excluded, as were those who were too ill to take part in the study.
Over a period of about a year 120 patients, 89 on SGAs and 31 on FGAs, who fulfilled selection criteria were identified and included in the study. The majority of these patients (n = 111) were outpatients when they took part in the study.
Assessments
Symptoms were rated on the Positive and Negative Syndrome Scale (PANSS).[16] Insight was rated based on scores on item 12 of the General Psychopathology subscale of the PANSS. The Udvalg for Kliniske Undersogelser Side-effect Rating Scale (UKU)[17] was the chief instrument employed to rate psychic, neurological, autonomic and other side-effects; the Barnes Akathisia Rating Scale (BARS)[18] was used to evaluate Akathisia and the Abnormal Involuntary Movements Scale (AIMS)[19] was used for the assessment of dyskinesia. Attitudes toward antipsychotics were evaluated using the 10-item version of the Drug Attitude Inventory-10 (DAI-10)[20,21] The DAI-10 is a patient-report measure comprising of ten “yes/no” statements reflecting patients’ experiences, attitudes and beliefs about medication. Each response is scored as +1 if correct, or −1 if incorrect; the final score is the sum of all positive and negative scores.
Analysis of data
Data were analyzed using the Statistical Package for Social Scientists, version fourteen (SPSS-14- SPSS Inc., Chicago, IL, USA). Chi-square, Student's t and Mann-Whitney tests were used to compare the two groups on different parameters. Two tailed P values were used for checking significance. A stepwise multiple regression analyses was conducted to examine the association between attitudes toward antipsychotics and other variables in the entire sample of 120 patients. Independent variables included demographic parameters (age, gender, marital status, occupational status, family income and residence), illness duration, antipsychotic dose, PANSS scores, insight scores and the UKU, AIMS and BARS scores. The DAI-10 score was the dependent variable.
RESULTS
Patient profiles
The demographic, clinical and treatment profiles of patients included in the study are depicted in Tables 1 and 2.
Table 1.
Patient profiles
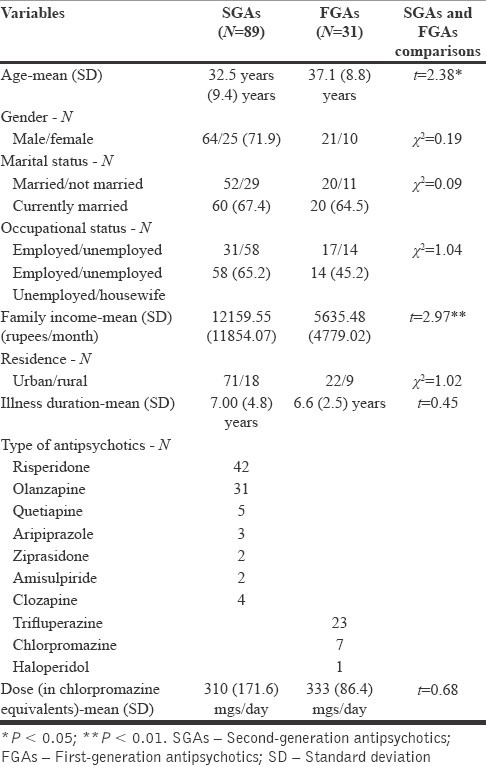
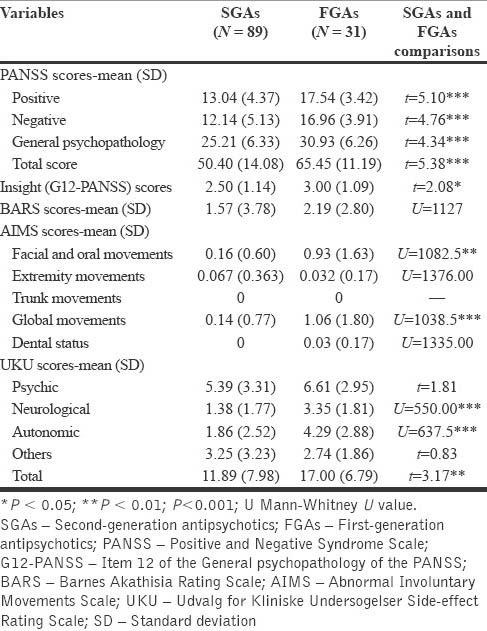
Table 2.
Psychopathology, insight and side-effects
Patients on FGAs were significantly older and came from families with significantly lower incomes. However, these differences in income were most probably a consequence of the prevailing prescribing practices. Since only FGAs are available from the hospital free of cost, clinicians generally tend to prescribe these medications as a first option to patients with low incomes, who are often unable to afford the more expensive SGAs.
Patients on FGAs were more severely ill as reflected by their significantly higher PANSS scores. They also had poorer insight into their illness than patients on SGAs. Side-effects were also more severe in the FGA group. On the AIMS, patients on FGAs had significantly higher scores on facial/oral and global movements. This was mirrored by significantly higher scores on the neurological subscale of the UKU. In addition, patients on FGAs had significantly higher scores on the autonomic subscale of the UKU. Consequently, total UKU scores were also significantly higher in the FGA group.
Attitudes toward antipsychotics
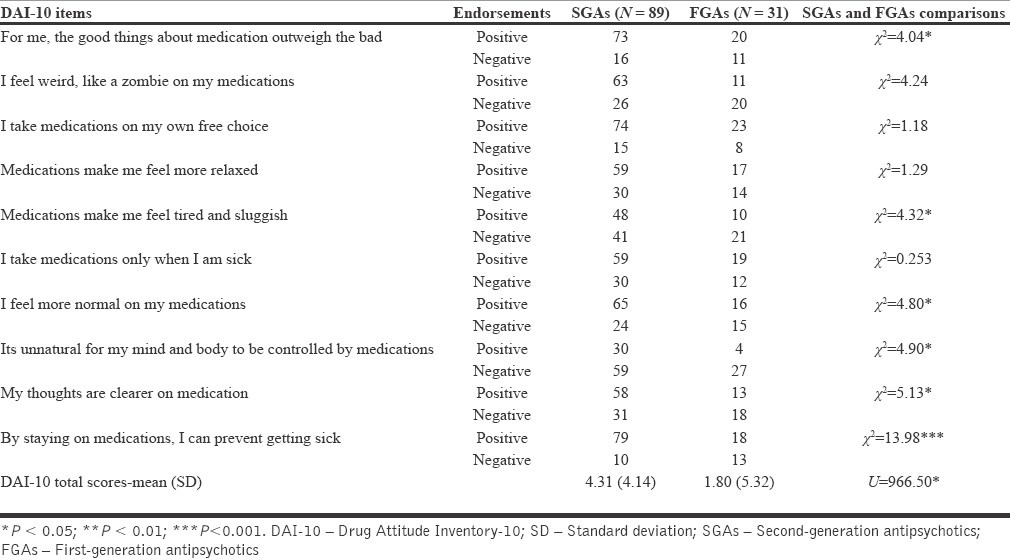
Average DAI-10 scores were positive in both antipsychotic groups. This indicated that patients in both groups had predominantly positive attitudes toward their medications. However, total DAI-10 scores were significantly higher in the SGA group. Analysis of individual items of the DAI-10 revealed the following significant differences: Patients on SGAs felt more normal on their medications, believed that their thoughts were clearer on medications, felt that good things about their medications outweighed the bad and believed that their medications helped them from falling ill again. In addition, they did not feel as tired and sluggish on their medications and did not believe that medications were unnatural or controlled their bodies. These results are depicted in Table 3.
Table 3.
Attitudes toward antipsychotics-DAI-10
Correlates of attitudes toward antipsychotics
Results of the stepwise multiple regression analysis, which was used to examine the association between attitudes toward antipsychotics and several demographic and clinical variables are depicted in Table 4.
Table 4.
Correlates of attitudes toward antipsychotics: Results of the stepwise multiple regression analysis
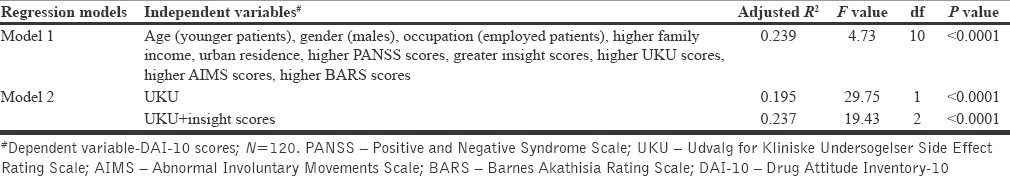
In the first step, younger age, male gender, employment, higher family income, urban residence, higher scores on insight and lower scores on the PANSS, UKU, AIMS and BARS all demonstrated significant and positive associations with DAI-10 scores. The variance in DAI-10 scores explained by all these variables was 23.9%.
In the next step, all other variables apart from UKU and insight scores were excluded. The maximum variance in DAI-10 scores was accounted for by the UKU scores (19.5%), while insight scores explained 4.2% of the variance. Thus, all the other independent variables, which had been excluded, explained only 0.2% of the variance in DAI-10 scores.
DISCUSSION
Patients of this study had predominantly positive attitudes toward their antipsychotic medications, whether they were on FGAs or SGAs. Results of previous studies have been variable, with many reporting a similar pattern of predominantly positive attitudes among their patients,[2,3,11,12,14,22,23] while others have indicated that negative attitudes to antipsychotics are also very common.[24,25] The predominance of positive attitudes could be a function of the sample of the current study, which was mainly made up of chronic, moderately ill and relatively stable patients. Such patients are more likely to have positive views about their medications than acutely ill patients,[25] or those with more severe psychopathology.[2,12] Moreover, such a sample often excludes patients who are non-adherent and therefore, likely to have more negative views about their medications.[22,26]
The results of this study regarding the correlates of attitudes toward antipsychotics reflected certain important trends in the literature on this subject. Several factors, which can potentially influence patients’ attitudes toward antipsychotics, have been identified in earlier studies.[2,3,11,12,13,14] Among all these variables, severity of symptoms and side-effects, level of insight, level of functioning, the doctor-patient relationship, personal health beliefs and attitudes of family members have emerged as the ones most likely to influence attitudes of patients toward antipsychotics. Demographic parameters, apart from employment and other clinical or treatment variables appear to have less influence on attitudes. In the present study, side-effects of medications turned out to be the major determinant of attitudes toward antipsychotics among patients. Since the major difference between the two antipsychotic groups was in the frequency of extrapyramidal and autonomic side-effects (more severe in the FGA group), it can be concluded that these side-effects were principal determinants of patients’ attitudes in this study. Moreover, they were most likely to explain the differences in attitudes between the FGA and SGA group. The finding that patients with higher side-effect burden tended to have more negative attitudes toward the medication is in agreement with several previous studies.[3,11,12,22,27,28] However, others have failed to demonstrate an association between side-effects and attitudes.[23,29,30,31,32] In studies reporting an association between side-effects and attitudes, extrapyramidal side-effects, sedation and sexual dysfunctions have emerged as major correlates of negative attitudes. This is partly due to the fact that that either all,[11,12] or a large proportion of patients in these studies were being treated with FGAs.[22] In the current study, greater insight was also associated with more positive attitudes to antipsychotics among patients. This was consistent with the results of several previous studies on this aspect.[2,12,13,14,23,33] However, unlike other studies,[2,3,11,12,13,14,22,23,29,33] severity of symptoms explained only a negligible proportion of the variance in attitudes in the present study. This could be attributed to the nature of the sample, which largely consisted of chronically ill, but stable patients with moderate levels of psychopathology. Though the association with demographic factors such as younger are, male gender and employment in this study was in line with some of the earlier ones,[2,3,34] on the whole these variables did not appear to make a significant contribution to patients’ attitudes. This too was in keeping with the predominant trend in much of the previous research. Finally, results of the regression analysis indicated that less than a quarter of the variance in attitudes could be attributed to the combined effect of all these variables. This suggests that attitude toward antipsychotics is a complex and multi-faceted construct with many potential determinants, some of which have still to be explored.[2,31]
Whether patients on SGAs have more positive attitudes toward these medications, than those on FGAs, has been a matter of some controversy. The evidence from randomized clinical trials as well as naturalistic comparisons of these two groups of antipsychotics is equivocal, with about half of them finding in favor of SGAs while the other half revealing no differences between FGAs and SGAs. Reviews based on these studies have also yielded inconsistent findings.[1,4,5,6,35] Though many of these have concluded that patients on SGAs have better attitudes, some have only found suggestive, but not conclusive evidence of the superiority of SGAs in this regard, while others have failed to find any differences between the two groups. The more recent effectiveness studies have also yielded inconsistent findings while comparing attitudes among patients on FGAs and SGAs.[7,8,9,10] Finally, surveys of patients’ views on the matter have usually revealed a strong preference for SGAs, despite side-effects such as weight gain or sexual dysfunction.[36] In the current study patients on SGAs had more positive views of their medications than those on FGAs. Analysis of individual items on the DAI-10 revealed differences mainly on items concerning subjective tolerability or response,[21] such as believing that good things about their medications outweighed the bad, feeling more normal, less tired and with clearer thoughts on medications. This was in line with the finding that side-effects emerged as most important determinant of attitudes among both groups of patients. In addition, items concerning beliefs about medications such as medications protected against relapse and that medications were not unnatural, also differed significantly between the two groups. These could be due to better insight among patients with SGAs since insight also emerged as a significant correlate of attitude toward antipsychotics. However, patients on FGAs were older, came from poorer families and were more severely ill, variables which also demonstrated significant associations with attitudes toward antipsychotics. Then again, these variables explained a negligible part of the variance in attitudes. Thus, it was unlikely that differences between the two antipsychotic groups on attitudes could be explained by differences in age, income or severity of symptoms.
The results of this study need to be treated with caution because of several methodological limitations. Principal among these were the small sample size, inclusion of patients from a single center, the chronic and stable nature of the patients’ illnesses and the omission of many of the potential correlates of attitudes toward antipsychotics. Thus, these findings can only be considered preliminary and cannot be readily generalized to other populations such as acutely and more severely ill patients, or those who are non-adherent.
Nevertheless, this study highlights the importance of attitudes to antipsychotics among patients with schizophrenia and the complex relationships between attitudes and its potential determinants. Attitudes of patients toward their antipsychotics influence their adherence with treatment and a number of other parameters such as quality of life, treatment outcomes, suicidal behavior and substance abuse.[2,3] Moreover, it is possible to modify attitudes by paying more attention to factors such as symptom relief, insight and side-effects.[11] Therefore, the need for further exploration of this area is amply clear.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Awad AG. Antipsychotic medications: Compliance and treatment. Curr Opin Psychiatry. 2004;17:75–80. [Google Scholar]
- 2.Rocca P, Crivelli B, Marino F, Mongini T, Portaleone F, Bogetto F. Correlations of attitudes toward antipsychotic drugs with insight and objective psychopathology in schizophrenia. Compr Psychiatry. 2008;49:170–6. doi: 10.1016/j.comppsych.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 3.Kuroda N, Sun S, Lin CK, Morita N, Kashiwase H, Yang F, et al. Attitudes toward taking medication among outpatients with schizophrenia: Cross-national comparison between Tokyo and Beijing. Environ Health Prev Med. 2008;13:288–95. doi: 10.1007/s12199-008-0043-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corrigan PW, Reinke RR, Landsberger SA, Charate A, Toombs GA. The effects of atypical antipsychotic medications on psychosocial outcomes. Schizophr Res. 2003;63:97–101. doi: 10.1016/s0920-9964(02)00379-1. [DOI] [PubMed] [Google Scholar]
- 5.Awad AG, Voruganti LN. New antipsychotics, compliance, quality of life, and subjective tolerability — Are patients better off? Can J Psychiatry. 2004;49:297–302. doi: 10.1177/070674370404900504. [DOI] [PubMed] [Google Scholar]
- 6.Voruganti LP, Baker LK, Awad AG. New generation antipsychotic drugs and compliance behaviour. Curr Opin Psychiatry. 2008;21:133–9. doi: 10.1097/YCO.0b013e3282f52851. [DOI] [PubMed] [Google Scholar]
- 7.García-Cabeza I, Gómez JC, Sacristán JA, Edgell E, González de Chavez M. Subjective response to antipsychotic treatment and compliance in schizophrenia. A naturalistic study comparing olanzapine, risperidone and haloperidol (EFESO Study) BMC Psychiatry. 2001;1:7. doi: 10.1186/1471-244X-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Novick D, Haro JM, Suarez D, Vieta E, Naber D. Recovery in the outpatient setting: 36-month results from the Schizophrenia Outpatients Health Outcomes (SOHO) study. Schizophr Res. 2009;108:223–30. doi: 10.1016/j.schres.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Agius M, Davis A, Gilhooley M, Chapman S, Zaman R. What do large scale studies of medication in schizophrenia add to our management strategies? Psychiatr Danub. 2010;22:323–8. [PubMed] [Google Scholar]
- 10.Foussias G, Remington G. Antipsychotics and schizophrenia: From efficacy and effectiveness to clinical decision-making. Can J Psychiatry. 2010;55:117–25. doi: 10.1177/070674371005500302. [DOI] [PubMed] [Google Scholar]
- 11.Lambert M, Conus P, Eide P, Mass R, Karow A, Moritz S, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19:415–22. doi: 10.1016/j.eurpsy.2004.06.031. [DOI] [PubMed] [Google Scholar]
- 12.Adewuya AO, Ola BA, Mosaku SK, Fatoye FO, Eegunranti AB. Attitude towards antipsychotics among out-patients with schizophrenia in Nigeria. Acta Psychiatr Scand. 2006;113:207–11. doi: 10.1111/j.1600-0447.2005.00745.x. [DOI] [PubMed] [Google Scholar]
- 13.Rossi A, Pacifico R, Stratta P. Attitudes toward medication and the clinical variables in schizophrenia: Structural equation models. Patient Prefer Adherence. 2009;3:305–9. doi: 10.2147/ppa.s5590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haq F, Behan C, McGlade N, Mulkerrin U, O’Callaghan E, Kinsella A, et al. Factors that influence patients’ attitudes to antipsychotic medication. Ir J Psychol Med. 2009;26:6–11. doi: 10.1017/S0790966700000045. [DOI] [PubMed] [Google Scholar]
- 15.First MB, Spitzer RL, Gibson M, William JB. Washington, DC: American Psychiatric Press; 1996. The Structured Clinical Interview for DSM-IV Axis I Disorders Clinical Version. [Google Scholar]
- 16.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 17.Lingjaerde O, Ahlfors UG, Bech P, Dencker SJ, Elgen K. The UKU side effect rating scale. A new comprehensive rating scale for psychotropic drugs and a cross-sectional study of side effects in neuroleptic-treated patients. Acta Psychiatr Scand Suppl. 1987;334:1–100. doi: 10.1111/j.1600-0447.1987.tb10566.x. [DOI] [PubMed] [Google Scholar]
- 18.Barnes TR. A rating scale for drug-induced akathisia. Br J Psychiatry. 1989;154:672–6. doi: 10.1192/bjp.154.5.672. [DOI] [PubMed] [Google Scholar]
- 19.Guy W. Washington DC: US Department of Health Education and Welfare; 1976. ECDEU Assessment Manual for Psychopharmacology-Revised. [Google Scholar]
- 20.Awad AG. Subjective response to neuroleptics in schizophrenia. Schizophr Bull. 1993;19:609–18. doi: 10.1093/schbul/19.3.609. [DOI] [PubMed] [Google Scholar]
- 21.Hogan TP, Awad AG, Eastwood R. A self-report scale predictive of drug compliance in schizophrenics: Reliability and discriminative validity. Psychol Med. 1983;13:177–83. doi: 10.1017/s0033291700050182. [DOI] [PubMed] [Google Scholar]
- 22.Hofer A, Kemmler G, Eder U, Honeder M, Hummer M, Fleischhacker WW. Attitudes toward antipsychotics among outpatient clinic attendees with schizophrenia. J Clin Psychiatry. 2002;63:49–53. doi: 10.4088/jcp.v63n0110. [DOI] [PubMed] [Google Scholar]
- 23.Freudenreich O, Cather C, Evins AE, Henderson DC, Goff DC. Attitudes of schizophrenia outpatients toward psychiatric medications: Relationship to clinical variables and insight. J Clin Psychiatry. 2004;65:1372–6. doi: 10.4088/jcp.v65n1012. [DOI] [PubMed] [Google Scholar]
- 24.Lesser IM, Friedmann CT. Attitudes toward medication change among chronically impaired psychiatric patients. Am J Psychiatry. 1981;138:801–3. doi: 10.1176/ajp.138.6.801. [DOI] [PubMed] [Google Scholar]
- 25.Gerlach J, Larsen EB. Subjective experience and mental side-effects of antipsychotic treatment. Acta Psychiatr Scand Suppl. 1999;395:113–7. doi: 10.1111/j.1600-0447.1999.tb05990.x. [DOI] [PubMed] [Google Scholar]
- 26.Rettenbacher MA, Hofer A, Eder U, Hummer M, Kemmler G, Weiss EM, et al. Compliance in schizophrenia: Psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65:1211–8. doi: 10.4088/jcp.v65n0908. [DOI] [PubMed] [Google Scholar]
- 27.Van Putten T, May PR, Marder SR, Wittmann LA. Subjective response to antipsychotic drugs. Arch Gen Psychiatry. 1981;38:187–90. doi: 10.1001/archpsyc.1981.01780270073010. [DOI] [PubMed] [Google Scholar]
- 28.Hogan TP, Awad AG. Subjective response to neuroleptics and outcome in schizophrenia: A re-examination comparing two measures. Psychol Med. 1992;22:347–52. doi: 10.1017/s0033291700030282. [DOI] [PubMed] [Google Scholar]
- 29.Cabeza IG, Amador MS, López CA, González de Chávez M. Subjective response to antipsychotics in schizophrenic patients: Clinical implications and related factors. Schizophr Res. 2000;41:349–55. doi: 10.1016/s0920-9964(99)00079-1. [DOI] [PubMed] [Google Scholar]
- 30.Ritsner M, Ponizovsky A, Endicott J, Nechamkin Y, Rauchverger B, Silver H, et al. The impact of side-effects of antipsychotic agents on life satisfaction of schizophrenia patients: A naturalistic study. Eur Neuropsychopharmacol. 2002;12:31–8. doi: 10.1016/s0924-977x(01)00128-6. [DOI] [PubMed] [Google Scholar]
- 31.Day JC, Bentall RP, Roberts C, Randall F, Rogers A, Cattell D, et al. Attitudes toward antipsychotic medication: The impact of clinical variables and relationships with health professionals. Arch Gen Psychiatry. 2005;62:717–24. doi: 10.1001/archpsyc.62.7.717. [DOI] [PubMed] [Google Scholar]
- 32.Hofer A, Rettenbacher MA, Edlinger M, Kemmler G, Widschwendter CG, Fleischhacker WW. Subjective response and attitudes toward antipsychotic drug therapy during the initial treatment period: A prospective follow-up study in patients with schizophrenia. Acta Psychiatr Scand. 2007;116:354–61. doi: 10.1111/j.1600-0447.2007.01087.x. [DOI] [PubMed] [Google Scholar]
- 33.Mohamed S, Rosenheck R, McEvoy J, Swartz M, Stroup S, Lieberman JA. Cross-sectional and longitudinal relationships between insight and attitudes toward medication and clinical outcomes in chronic schizophrenia. Schizophr Bull. 2009;35:336–46. doi: 10.1093/schbul/sbn067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schennach-Wolff R, Jäger M, Seemüller F, Obermeier M, Messer T, Laux G, et al. Attitude towards adherence in patients with schizophrenia at discharge. J Psychiatr Res. 2009;43:1294–301. doi: 10.1016/j.jpsychires.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 35.Awad AG, Voruganti LN. Neuroleptic dysphoria: Revisiting the concept 50 years later. Acta Psychiatr Scand. 2005;111(Suppl. 427):6–13. doi: 10.1111/j.1600-0447.2005.00539.x. [DOI] [PubMed] [Google Scholar]
- 36.Castle D, Morgan V, Jablensky A. Antipsychotic use in Australia: The patients’ perspective. Aust N Z J Psychiatry. 2002;36:633–41. doi: 10.1046/j.1440-1614.2002.01037.x. [DOI] [PubMed] [Google Scholar]


