Abstract
IMPORTANCE
The suicide rate among US Army soldiers has increased substantially in recent years.
OBJECTIVES
To estimate the lifetime prevalence and sociodemographic, Army career, and psychiatric predictors of suicidal behaviors among nondeployed US Army soldiers.
DESIGN, SETTING, AND PARTICIPANTS
A representative cross-sectional survey of 5428 nondeployed soldiers participating in a group self-administered survey.
MAIN OUTCOMES AND MEASURES
Lifetime suicidal ideation, suicide plans, and suicide attempts.
RESULTS
The lifetime prevalence estimates of suicidal ideation, suicide plans, and suicide attempts are 13.9%, 5.3%, and 2.4%. Most reported cases (47.0%–58.2%) had pre-enlistment onsets. Pre-enlistment onset rates were lower than in a prior national civilian survey (with imputed/simulated age at enlistment), whereas post-enlistment onsets of ideation and plans were higher, and post-enlistment first attempts were equivalent to civilian rates. Most reported onsets of plans and attempts among ideators (58.3%–63.3%) occur within the year of onset of ideation. Post-enlistment attempts are positively related to being a woman (with an odds ratio [OR] of 3.3 [95% CI, 1.5–7.5]), lower rank (OR = 5.8 [95% CI, 1.8–18.1]), and previously deployed (OR = 2.4–3.7) and are negatively related to being unmarried (OR = 0.1–0.8) and assigned to Special Operations Command (OR = 0.0 [95% CI, 0.0–0.0]). Five mental disorders predict post-enlistment first suicide attempts in multivariate analysis: pre-enlistment panic disorder (OR = 0.1 [95% CI, 0.0–0.8]), pre-enlistment posttraumatic stress disorder (OR = 0.1 [95% CI, 0.0–0.7]), post-enlistment depression (OR = 3.8 [95% CI, 1.2–11.6]), and both pre- and post-enlistment intermittent explosive disorder (OR = 3.7–3.8). Four of these 5 ORs (posttraumatic stress disorder is the exception) predict ideation, whereas only post-enlistment intermittent explosive disorder predicts attempts among ideators. The population-attributable risk proportions of lifetime mental disorders predicting post-enlistment suicide attempts are 31.3% for pre-enlistment onset disorders, 41.2% for post-enlistment onset disorders, and 59.9% for all disorders.
CONCLUSIONS AND RELEVANCE
The fact that approximately one-third of post-enlistment suicide attempts are associated with pre-enlistment mental disorders suggests that pre-enlistment mental disorders might be targets for early screening and intervention. The possibility of higher fatality rates among Army suicide attempts than among civilian suicide attempts highlights the potential importance of means control (ie, restricting access to lethal means [such as firearms]) as a suicide prevention strategy.
Suicide is among the leading causes of death worldwide.1,2 Historically, the suicide rate among US Army soldiers has been below the general population rate. However, the Army suicide rate has increased dramatically in recent years, while the civilian rate has remained fairly stable.3 The reason for this increase is unknown. Although several recent studies have examined patterns and correlates of Army suicides in an effort to increase our understanding of risk factors,4,5 none carefully examined pre- vs post-enlistment risk factors. Such an analysis might help identify soldiers near the time of their enlistment who are at risk for later suicidal behavior so that they could be targeted for preventive interventions. Nor have previous military studies distinguished risk factors for suicidal ideation vs attempts among ideators, a distinction shown to be important in civilian studies.6,7 Herein, we examine the associations of lifetime mental disorders having pre- and post-enlistment onsets with subsequent onsets of suicidal ideation, suicide plans, and suicide attempts in a representative sample of nondeployed US Army soldiers participating in Army STARRS (http://www.armystarrs.org), a large epidemiological-neurobiological study of Army suicides and their correlates.8
Methods
Sample
Data came from the April to December 2011 Army STARRS All-Army Study (AAS), a de-identified representative cross-sectional survey of active duty Army personnel exclusive of soldiers in Basic Combat Training or deployed to a combat theater excluding personnel in units of fewer than 30 soldiers (representing less than 2% of all Army personnel). The 5428 respondents considered herein consist of Regular Army personnel (ie, excluding activated Army National Guard and Army Reserve) who completed a group-administered self-report questionnaire survey and agreed to have their administrative records linked to their survey responses. Written informed consent was obtained prior to data collection. Informed consent and human subjects protection procedures were approved by the Human Subjects Committees of all collaborating organizations.
Although all unit members were ordered to report to informed consent sessions, 23.5% were absent owing to conflicting duty assignments. Most attendees (96.0%) consented to the survey, 98.0% of consenters completed the survey, 72.4% of those who completed the survey (hereafter referred to as completers) provided written consent for record linkage, and 95.6% of consenters were successfully linked. The survey completion-successful linkage cooperation rate was 65.1% (0.96 × 0.98 × 0.724 × 0.956), and the response rate was 49.8% ([1 − 0.235] × 0.651),9 based on the American Association of Public Opinion Research COOP1 and RR1 calculation methods.10 Although we were prohibited from attempting refusal conversion or obtaining individual-level administrative data for re-fusers, de-identified administrative data were provided for the entire Army and for survey respondents who agreed to linkage, allowing 2 weights to be created to adjust for nonresponse bias. Weight 1 adjusted for discrepancies in survey responses between survey completers with and without record linkage. Weight 2 adjusted for discrepancies between multivariate administrative record profiles of weighted (weight 1) survey completers with record linkage and the target population. Doubly weighted (weight 1 × weight 2) data were used in analyses. A more detailed description of AAS weighting is presented elsewhere, despite the fact that these differences were modest in substantive terms.11 More detailed descriptions of the AAS design,8 field procedures,9 and weighting11 are presented elsewhere. See Kessler et al12 in this issue for the distributions of sociodemographic and Army career variables in the AAS compared with the target population of the entire active duty Regular Army.
Measures
Suicidal Behaviors
Suicidal behaviors were assessed using a modified version of the Columbia–Suicide Severity Rating Scale13 assessing lifetime occurrence and age at onset of suicidal ideation (“Did you ever in your life have thoughts of killing yourself?” or “Did you ever wish you were dead or would go to sleep and never wake up?”) and, among respondents who reported lifetime ideation, suicide plans (“Did you ever have any intention to act [on these thoughts/on that wish]?” and, if so, “Did you ever think about how you might kill yourself [eg, taking pills, shooting yourself] or work out a plan of how to kill yourself?”) and attempts (“Did you ever make a suicide attempt [ie, purposefully hurt yourself with at least some intention to die]?”).
DSM-IV Mental Disorders
The lifetime prevalence estimates of 12 common lifetime DSM-IV mental disorders were assessed: 8 internalizing disorders (major depressive disorder [MDD], bipolar disorder, panic disorder, generalized anxiety disorder, posttraumatic stress disorder [PTSD], specific phobia, social phobia, and obsessive-compulsive disorder), 3 externalizing disorders (attention-deficit/hyperactivity disorder, intermittent explosive disorder [IED], and substance use disorders, including alcohol and drug abuse and dependence), and a screening question for any other serious mental illness (“Did you ever in your life have any other serious mental illness, emotional problem, or nervous breakdown?”). The bipolar disorder assessment included bipolar I disorder, bipolar II disorder, and sub-threshold bipolar disorder (hypomania without a history of major depression or subthreshold hypomania).14 Screening scales from the Composite International Diagnostic Interview15 were used to assess bipolar disorder, panic disorder, attention-deficit/hyperactivity disorder, and IED, and a revised self-report version of the Family History Screen (FHS)16 modified to assess personal, rather than family, history of these disorders was used to assess the remaining disorders. The Composite International Diagnostic Interview screening scales have good concordance with independent clinical diagnoses in the AAS (area under the receiver operating characteristic curve of 0.69–0.79 across diagnoses).17 The FHS has been shown to have acceptableconcordancewithbest-estimateclinicaldiagnoses,16 although the items used in the AAS yielded implausibly high prevalence estimates, and diagnoses based on the FHS should consequently be considered combinations of threshold and subthreshold disorders. Respondents were asked to estimate age at onset of each lifetime disorder.
Sociodemographic and Army Career Variables
The sociodemographic variables considered herein include age, sex, race/ethnicity, and marital status. Race and ethnicity were assessed in 2 questions, the first asking respondents if they were Spanish, Hispanic, or Latino (yes or no) and the second asking respondents to record their race by checking all applicable categories (white, black or African American, American Indian or Native American, Asian [eg, Chinese, Filipino, or Indian], and Native Hawaiian or other Pacific Islander) and/or by providing an open-ended response to the race category of “other.” Responses were collapsed into the summary categories of non-Hispanic black, non-Hispanic white, Hispanic, and other. Race and ethnicity were assessed as part of an effort to obtain a comprehensive sociodemographic profile of soldiers. Army career variables include age at enlistment, rank, number of deployments to a combat theater (0, 1, 2, ≥3), and command assignment. The functional form of the association between each continuous predictor variable and suicide attempts was examined before collapsing the continuous variable, to guarantee that the categories described herein capture the nonlinearities in these associations.
Analysis Methods
Retrospective age-at-onset reports were analyzed using the 2-part actuarial method to estimate survival curves, a method differing from the Kaplan-Meier method18 in using a more accurate way of estimating onsets within a given year.19 Both absolute morbid risk (cumulative lifetime risk of ever having suicidal ideation, developing a suicide plan, or attempting suicide) and relative morbid risk (the proportion of total morbid risk at each age) are reported for each outcome. Discrete-time survival analysis (with person-years the unit of analysis, time-varying predictors, and a logistic link function20) was used to examine associations of temporally prior predictors with subsequent onset of post-enlistment suicidal behavior. A distinction was made between mental disorders that started at an earlier age than age at enlistment vs after enlistment. Survival coefficients were exponentiated to create odds ratios (ORs) with 95% CIs.18,19 Simulation methods (described in Cox and Li21) were used to calculate population-attributable risk proportions (PARPs), which describe the proportions of observed suicidal outcomes associated with subsets of predictors.22 Because the AAS data are both clustered and weighted, the design-based Taylor series linearization method was used to produce standard errors.23 Multivariate significance was examined using design-based Wald χ2 tests.
Results
Lifetime Prevalence and Age at Onset of Suicidal Behaviors
The lifetime prevalence estimates of suicidal ideation, suicide plans, and suicide attempts are 13.9%, 5.3%, and 2.4%, respectively (Table 1). Prevalence estimates are significantly higher among women than men. More than one-third (38.5%) of ideators developed suicide plans, and 17.1% attempted suicide. Roughly one-third (34.4%) of ideators with a plan went on to make attempts compared with 6.3% of ideators without a plan, resulting in roughly 80% of first attempts being planned.
Table 1.
Lifetime Prevalence of Suicidal Behavior in the April to December 2011 Army STARRS AAS
| Variable | % (SE) of Soldiers
|
||||||
|---|---|---|---|---|---|---|---|
| Total Sample (N = 5428)
|
Lifetime Ideators
|
||||||
| Ideation | Plan | Attempt | Plan | Attempt | Attempt by Those With a Plan |
Attempt by Those Without a Plan |
|
| Lifetime prevalence | |||||||
|
| |||||||
| Total | 13.9 (0.4) | 5.3 (0.4) | 2.4 (0.2) | 38.5 (2.6) | 17.1 (1.2) | 34.4 (2.3) | 6.3 (1.1) |
|
| |||||||
| Men | 12.9 (0.5) | 4.8 (0.5) | 2.1 (0.2) | 37.3 (3.3) | 16.0 (1.1) | 33.5 (2.9) | 5.6 (1.0) |
|
| |||||||
| Women | 19.9 (1.5) | 8.6 (1.1) | 4.3 (0.8) | 43.2 (4.9) | 21.5 (3.6) | 37.6 (5.7) | 9.3 (3.8) |
|
| |||||||
| Lifetime cases with pre-enlistment onsets | |||||||
|
| |||||||
| Total | 58.2 (2.1) | 52.9 (4.1) | 47.0 (5.6) | 52.9 (4.1) | 47.0 (5.6) | 50.6 (6.7) | 34.4 (2.7) |
|
| |||||||
| Men | 58.3 (2.8) | 54.9 (3.9) | 49.8 (5.7) | 54.9 (3.9) | 49.8 (5.7) | 54.5 (6.4) | 33.1 (2.6) |
|
| |||||||
| Women | 57.6 (4.2) | 45.9 (11.5) | 38.6 (8.1) | 45.9 (11.5) | 38.6 (8.1) | 38.8 (10.7) | 37.7 (2.0) |
Abbreviations: AAS, All-Army Survey; Army STARRS, Army Study to Assess Risk and Resilience in Servicemembers.
Age-at-onset curves were used to estimate that the proportions of soldiers who will ever have suicidal ideation, develop a suicide plan, or attempt suicide (morbid risk, as opposed to the proportions that ever did so up to the time of interview) are 21.0%, 9.0%, and 4.1%, respectively. These curves also show that lifetime prevalence is low through the early teens and then increases linearly through the mid-40s, with median age at onset in the early-20s (Figure). Overlap among curves suggests that transitions from ideation to plan and attempt typically are quite rapid. Speed-of-transition curves (available on request) show that 62.4% of transitions from ideation to plans and 58.3% of transitions from ideation to attempts occur within 1 year of onset of ideation, whereas 63.3% of transitions from plans to attempts occur within 1 year of onset of plans.
Figure. Age-at-Onset Distributions of Lifetime Suicidal Ideation, Suicide Plans, and Suicide Attempts.
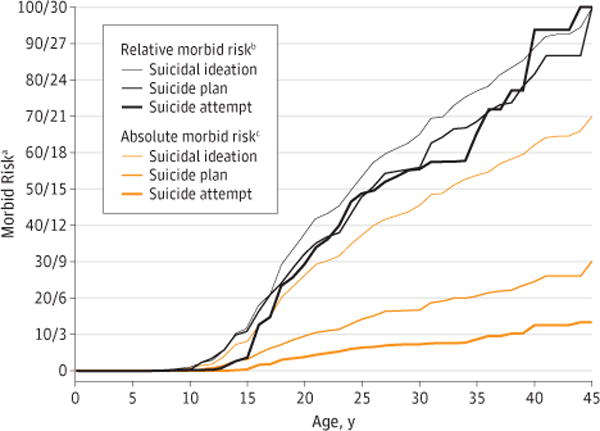
aThe numbers on the left indicate relative morbid risk, and those on the right indicate absolute morbid risk. bCumulative lifetime risk of ever having suicidal ideation, developing a suicide plan, and attempting suicide. cProportions of total morbid risk as of each age.
The majority of lifetime prevalent suicidal ideation began prior to age at enlistment (58.3% of men vs 57.6% of women; , P = .91). The same was true of plans (54.9% of men vs 45.9% of women; , P = .45). Approximately half of men’s lifetime first attempts (49.8%) and 38.6% of women’s lifetime attempts occurred prior to age at enlistment ( , P = .24).
Sociodemographic and Army Career Predictors of Suicidal Behavior
Using additive multivariate survival equations, we examined associations of sociodemographic and Army career variables with subsequent first onsets of suicidal behavior. The results are reported herein for post-enlistment onsets (Table 2).
Table 2.
Associations of Sociodemographic and Army Career Variables With Post-Enlistment Onset of Suicidal Behavior in the April to December 2011 Army STARRS AASa
| Variable | Odds Ratio (95% CI) | ||
|---|---|---|---|
| Ideation (n = 4897) |
Plans (n = 5239) |
Attempts (n = 5324) |
|
| Age, y | |||
| 17–19 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 20–24 | 0.8 (0.4–1.7) | 0.6 (0.3–1.2) | 1.1 (0.3–3.4) |
| ≥25 | 0.7 (0.3–2.0) | 0.5 (0.1–1.7) | 0.3 (0.1–2.0) |
| Value | 0.4 | 1.8 | 3.9 |
| Sex | |||
| Men | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Women | 2.1 (1.4–3.1)b | 2.7 (1.5–5.1)b | 3.3 (1.5–7.5)b |
| Value | 13.8b | 10.0b | 8.6b |
| Race/ethnicity | |||
| Non-Hispanic white | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Non-Hispanic black | 0.4 (0.2–0.7)b | 0.7 (0.3–1.3) | 0.5 (0.2–1.3) |
| Hispanic | 1.0 (0.7–1.4) | 0.8 (0.4–1.8) | 1.2 (0.4–3.8) |
| Other | 0.4 (0.1–1.3) | 0.6 (0.1–3.0) | 1.4 (0.3–6.1) |
| Value | 11.1b | 1.8 | 2.4 |
| Marital status | |||
| Married | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Previously married | 0.2 (0.0–1.7) | 0.5 (0.1–3.4) | 0.1 (0.0–0.4)b |
| Never married | 1.0 (0.8–1.2) | 0.8 (0.4–1.5) | 0.8 (0.3–1.7) |
| Value | 2.1 | 1.0 | 7.4b |
| Age at enlistment, y | |||
| 17–18 | 1.3 (0.7–2.5) | 1.4 (0.4–4.4) | 0.5 (0.1–2.5) |
| 19–20 | 1.1 (0.6–2.1) | 2.0 (0.8–5.4) | 0.8 (0.2–3.5) |
| 21–23 | 0.7 (0.4–1.1) | 0.9 (0.3–2.6) | 0.4 (0.1–1.8) |
| ≥24 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Value | 9.4b | 4.2 | 2.8 |
| Rank of enlisted soldier | |||
| Lower rank (grades E1–E4) | 2.5 (1.3–5.0)b | 4.5 (1.4–14.0)b | 5.8 (1.8–18.1)b |
| Higher rank (grades E5–E9) | 1.2 (0.8–1.7) | 1.8 (0.7–4.5) | 2.5 (0.9–7.3) |
| Officer (grades W1–W5 or O1–O9) | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Value | 7.4b | 10.7b | 16.4b |
| Valuec | 5.5b | 10.0b | 13.4b |
| Deployments, No. | |||
| 0 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1 | 1.6 (1.0–2.7) | 1.7 (0.7–4.0) | 1.3 (0.5–3.2) |
| 2 | 1.9 (0.8–4.8) | 2.2 (0.7–6.9) | 2.4 (1.2–5.1)b |
| ≥3 | 1.8 (0.8–3.7) | 2.7 (1.0–7.7) | 3.7 (0.9–16.1) |
| Value | 4.1 | 3.9 | 7.5 |
| Command | |||
| FORSCOM | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Area Service Component Commandsd | 1.3 (0.8–2.1) | 1.9 (0.6–5.4) | 0.8 (0.3–1.8) |
| USASOC | 0.7 (0.2–2.1) | 0.3 (0.0–1.8) | 0.0 (0.0–0.0)b |
| MEDCOM | 0.8 (0.3–2.1) | 1.2 (0.2–7.0) | 0.7 (0.1–3.9) |
| TRADOC | 0.7 (0.3–1.6) | 1.4 (0.8–2.6) | 0.5 (0.1–2.7) |
| All other regular Army Commandse | 0.8 (0.5–1.4) | 1.4 (0.6–3.3) | 0.6 (0.2–2.1) |
| Value | 3.6 | 7.3 | 2040.8b |
Abbreviations: AAS, All-Army Survey; Army STARRS, Army Study to Assess Risk and Resilience in Servicemembers; FORSCOM, US Army Forces Command; MEDCOM, US Army Medical Command; TRADOC, US Army Training and Doctrine Command; USASOC, US Army Special Operations Command.
Based on a series of discrete-time survival models with a logistic link function to predict first lifetime onset of suicidal ideation, suicide plan, and suicide attempt in the years subsequent to enlistment, with all the predictors in the same model. Sample sizes are successively larger in predicting the 3 component outcomes owing to some respondents having first onsets of either (1) ideation but not plans or (2) plans but not attempts prior to their age at enlistment.
Significant at the .05 level, determined by use of a 2-sided test.
Tests for the significance of the difference between lower-ranking and higher-ranking enlisted soldiers.
The complete set of Area Commands includes US Army Africa, Central, North, South, Europe, and Pacific.
Including US Army Materiel Command, all other Army Service Component Commands, and all other Direct Reporting Units. See http://www.army.mil/info/organization/ for a complete description of the US Army Command Structure.
Age
Among soldiers with no pre-enlistment history of suicidal behavior, age is unrelated to post-enlistment onset ( , P = .14–.81). However, age is positively related to rank, which is a significant predictor of post-enlistment suicidal behavior.
Sex
Women soldiers have significantly elevated odds of suicidal ideation (OR = 2.1 [95% CI, 1.4–3.1]), suicide plans (OR = 2.7 [95% CI, 1.5–5.1]), and suicide attempts (OR = 3.3 [95% CI, 1.5–7.5]).
Race/Ethnicity
Race/ethnicity is significantly associated with post-enlistment onset of suicidal ideation ( , P = .011), but not suicide plans ( , P = .62) or suicide attempts ( , P = .49). The only individually significant ORs associated with race/ethnicity are lower odds of ideation (OR = 0.4 [95% CI, 0.2–0.7]) among non-Hispanic blacks.
Marital Status
Although never married and previously married soldiers have lower odds than married soldiers of all 3 outcomes (OR = 0.1–1.0), the association of marital status with suicidal behavior is statistically significant only for suicide attempts ( , P = .02). This is due to the significantly reduced odds of attempts among previously married vs married soldiers (OR = 0.1 [95% CI, 0.0–0.4]).
Age at Enlistment
Age at enlistment is significantly associated with post-enlistment onset of suicidal ideation ( , P = .02); however, this is due to a nonmonotonic pattern of elevated odds among soldiers who enlisted at 17 to 18 years of age (OR = 1.3 [95% CI, 0.7–2.5]) and decreased odds among those who enlisted at 21 to 23 years of age (OR = 0.7 [95% CI, 0.4–1.1]), neither of which is significantly different from the odds among soldiers who enlisted at 24 years of age or older (OR = 1.0). Age at enlistment is not significantly associated with either plans or attempts ( , P = .24–.42).
Rank
Rank is a consistently significant predictor of post-enlistment suicidal behavior ( , P ≤ .001–.03) owing to elevated odds among lower-rank enlisted soldiers (grades E1–E4) vs officers (OR = 2.5–5.8). Odds for higher-rank enlisted soldiers (grades E5–E9) are also elevated compared with officers (OR = 1.2–2.5), but not significantly. A more detailed analysis (results available on request) shows that rank is primarily associated with ideation (ie, it is not significantly associated with the transitions from ideation to plans [ , P = .12] or from ideation to attempts when controlling for plans [ , P = .14]).
Deployment History
Two-thirds of AAS respondents had a history of deployment. Although the number of deployments is not significantly associated with suicidal behavior overall ( , P = .06–.27), ORs are consistently elevated among soldiers who were ever deployed vs those who were never deployed (OR = 1.3–3.7), significantly so for 2 deployments predicting attempts (OR = 2.4 [95% CI, 1.2–5.1]) and the highest for 3 or more deployments predicting attempts (OR = 3.7 [95% CI, 0.9–16.1]).
Army Command
Army Command assignment is not significantly associated with suicidal ideation or suicide plans ( , P = .61–.20), but is significantly associated with suicide attempts owing to a virtual absence of attempts in Special Operations Command. All other Commands have insignificantly lower odds of attempts than US Army Forces Command (OR = 0.5–0.8).
Associations of Lifetime Mental Disorders With Post-Enlistment Onset of Suicide Attempts
Four pre-enlistment–onset disorders and 10 post-enlistment– onset disorders have significant ORs in bivariate models (ie, considering only 1 disorder at a time) predicting subsequent (to the age at onset of the disorder) first suicide attempts after enlistment (Table 3). All these ORs other than the one for pre-enlistment panic disorder (OR = 0.1 [95% CI, 0.0–0.7]) are positive (OR = 3.3–7.4). Most ORs become attenuated in multivariate models (ie, considering all disorders simultaneously), with only 5 multivariate ORs that were statistically significant: pre-enlistment panic disorder (inverse association), PTSD (inverse association), and IED and post-enlistment MDD and IED.
Table 3.
Prevalence and Associations of Lifetime Mental Disorders Having Pre-and Post-Enlistment Onsets With the Occurrence of Subsequent Post-Enlistment First Suicide Attempts in the April to December 2011 Army STARRS AASa
| Disorder | % of Solders (SE)
|
Odds Ratio (95% CI)
|
||||
|---|---|---|---|---|---|---|
| Lifetime Prevalence of Mental Disorders (n = 5324) |
Bivariate Associations
|
Multivariate Associations
|
||||
| Pre-Enlistment Disorders |
Post-Enlistment Disorders |
Pre-Enlistment Disorders |
Post-Enlistment Disorders |
Pre-Enlistment Disorders |
Post-Enlistment Disorders |
|
| Internalizing disorders | ||||||
|
| ||||||
| MDDa | 11.6 (0.5) | 10.3 (0.7) | 1.9 (0.6–6.3) | 6.5 (2.3–18.8)b | 1.6 (0.6–4.4) | 3.8 (1.2–11.6)b |
|
| ||||||
| BPD | 1.9 (0.3) | 1.8 (0.3) | Not shownc | 4.1 (1.4–11.8)b | Not shownc | 1.5 (0.5–5.2) |
|
| ||||||
| PD | 3.1 (0.4) | 8.3 (0.5) | 0.1 (0.0–0.7)b | 3.8 (1.2–11.8)b | 0.1 (0.0–0.8)b | 0.9 (0.3–2.6) |
|
| ||||||
| GADa | 13.5 (0.8) | 18.9 (0.9) | 1.3 (0.5–3.3) | 3.5 (1.1–11.1)b | 1.0 (0.4–2.3) | 0.9 (0.3–2.9) |
|
| ||||||
| PTSD | 11.2 (0.6) | 22.7 (1.0) | 0.3 (0.1–1.3) | 3.3 (1.6–6.8)b | 0.1 (0.0–0.7)b | 1.1 (0.4–3.1) |
|
| ||||||
| OCDa | 4.3 (0.4) | 7.7 (0.4) | 4.1 (1.1–15.7)b | 4.0 (1.4–11.7)b | 4.2 (1.0–17.6) | 1.0 (0.4–2.4) |
|
| ||||||
| Specific phobiad | 9.6 (0.7) | 4.1 (0.3) | 0.5 (0.2–1.7) | 6.1 (1.8–21.4)b | 0.5 (0.2–1.6) | 2.9 (0.7–11.6) |
|
| ||||||
| Social phobiad | 12.2 (0.8) | 6.1 (0.6) | 1.7 (0.6–4.6) | 2.8 (1.0–8.0) | 1.0 (0.4–2.6) | 0.8 (0.2–3.0) |
|
| ||||||
| Externalizing disorders | ||||||
|
| ||||||
| ADHDe | 7.0 (0.6) | Restrictede | 4.3 (2.3–8.1)b | Restrictede | 1.8 (0.5–6.9) | Restrictede |
|
| ||||||
| IED | 15.5 (0.7) | 4.8 (0.5) | 3.9 (2.1–7.3)b | 5.9 (2.2–15.4)b | 3.7 (1.7–8.3)b | 3.8 (1.2–11.6)b |
|
| ||||||
| SUD | 6.7 (0.5) | 8.1 (0.4) | 1.2 (0.3–4.8) | 3.9 (1.4–10.8)b | 0.8 (0.2–2.8) | 2.0 (0.7–6.2) |
|
| ||||||
| Other disorders | ||||||
|
| ||||||
| Other SMIa | 2.8 (0.2) | 5.9 (0.4) | 2.1 (0.7–6.2) | 7.4 (1.9–27.9)b | 1.4 (0.4–4.8) | 2.1 (0.8–5.9) |
Abbreviations: AAS, All-Army Survey; ADHD, attention-deficit/hyperactivity disorder; Army STARRS; Army Study to Assess Risk and Resilience in Servicemembers; BPD, bipolar disorder; GAD, generalized anxiety disorder; IED, intermittent explosive disorder; MDD, major depressive disorder; OCD, obsessive-compulsive disorder; PD, panic disorder; PTSD, posttraumatic stress disorder; SMI, serious mental illness; SUD, substance use disorder.
Based on discrete-time survival models with person-years as the unit of analysis and a logistic link function to predict first lifetime onset of suicide attempts in the years subsequent to enlistment in the subsample of AAS respondents who reported never having attempted suicide prior to age at enlistment.
Significant at the .05 level, determined by use of a 2-sided test.
Small cell sizes for BPD with pre-enlistment onsets (results not shown).
Threshold and subthreshold spectrum disorders assessed with a self-report version of the Family History Screen questions.17
All cases of ADHD had pre-enlistment onsets. In addition, the assessment of ADHD, unlike that of the other disorders, was restricted to current (at the time of interview) cases.
Disaggregation of Associations Through Proximal Outcomes
It is instructive to trace out the association of the 5 significant mental disorders predicting post-enlistment attempts through ideation, plans among ideators, and attempts among ideators (controlling for presence vs absence of a plan) (Table 4). All 3 component associations involving pre-enlistment panic disorder are inverse (OR = 0.1–0.4), and 2 are significant. All component associations involving pre-enlistment PTSD are also inverse (OR = 0.2–0.8) but insignificant. The association with ideation is significant for the 3 other disorders (pre- and post-enlistment IED and post-enlistment MDD; OR = 2.2–2.6), but none of the disorders is associated with plans among ideators, and only post-enlistment IED is associated with attempts among ideators (OR = 5.0 [95% CI, 1.4–18.0]).
Table 4.
Disaggregation of Significant Multivariate Associations of Lifetime Mental Disorders Having Pre- and Post-Enlistment Onsets With the Occurrence of Subsequent Post-Enlistment First Suicide Attempts Through Intermediate Outcomes in the April to December 2011 Army STARRS AASa
| Disorder | Odds Ratio (95% CI) | |||
|---|---|---|---|---|
| Ideation (n = 4897) |
Plans Among Ideators (n = 612) |
Attempt Among Ideators, Controlling for Plan (n = 697) |
Attempt (n = 5324) |
|
| Pre-enlistment PD | 0.3 (0.1–0.8)b | 0.4 (0.1–3.0) | 0.1 (0.0–1.0)b | 0.1 (0.0–0.8)b |
| Pre-enlistment PTSD | 0.8 (0.3–2.2) | 0.4 (0.1–1.0) | 0.2 (0.0–1.5) | 0.1 (0.0–0.7)b |
| Post-enlistment MDD | 2.6 (1.2–5.7)b | 0.7 (0.3–1.9) | 1.0 (0.3–2.9) | 3.8 (1.2–11.6)b |
| Pre-enlistment IED | 2.6 (1.7–4.0)b | 1.4 (0.7–2.7) | 1.6 (0.6–3.9) | 3.7 (1.7–8.3)b |
| Post-enlistment IED | 2.2 (1.3–3.9)b | 0.3 (0.0–1.6) | 5.0 (1.4–18.0)b | 3.8 (1.2–11.6)b |
Abbreviations: AAS, All-Army Survey; Army STARRS; Army Study to Assess Risk and Resilience in Servicemembers; IED, intermittent explosive disorder; MDD, major depressive disorder; PD, panic disorder; PTSD, posttraumatic stress disorder.
Based on discrete-time survival models with person-year as the unit of analysis and a logistic link function to predict first lifetime onset of suicidal ideation, suicide plans among ideators, and suicide attempts among ideators controlling for plan in the years subsequent to enlistment in the subsample of AAS respondents who reported never having had the outcome prior to age at enlistment. Sample sizes are successively larger in predicting the 3 component outcomes owing to some respondents having first onset of either (1) ideation but not plans or (2) plans but not attempts prior to their age at enlistment.
Significant at the .05 level, determined by use of a 2-sided test.
Population-Attributable Risk Proportions
Population-Attributable Risk Proportions Population-attributable risk proportions (PARPs) were calculated for post-enlistment first suicide attempts among soldiers who never made a pre-enlistment attempt. The PARP estimates are 31.3% for pre-enlistment onset disorders, 41.2% for post-enlistment onset disorders, and 59.9% for all disorders.
Discussion
Four limitations are noteworthy. First, sample vs population discrepancies (exclusions of soldiers in basic training or deployed coupled with incomplete response among target respondents) and the low response rate limit the external validity of the findings. Second, some respondents might have failed to report their mental disorders or suicidal behavior, or they provided inaccurate age-at-onset reports. Third, the Composite International Diagnostic Interview screening scales and self-report FHS are fully structured, thus yielding less textured diagnoses than those based on semistructured clinical interviews, whereas the FHS additionally includes subthreshold cases. Finally, the AAS did not include all potentially relevant DSM-IV disorders, thus making the prevalence and PARP estimates conservative.
Within the context of these limitations, 13.9% of US soldiers are estimated to have a history of suicidal ideation, 5.3% are estimated to have a history of suicide plans, and2.4%areestimated to have a history of suicide attempts, with 47% to 60% of these outcomes first occurring prior to enlistment. It is striking that nearly half of the soldiers who reported lifetime suicide attempts reported their first attempt occurring prior to the age at enlistment because history of suicide attempts is asked about in recruitment interviews, and applicants who report such a history are excluded from service. In the absence of methods to assess history of suicidal behaviors that do not require honest self-reports, the most practical implication of this finding might be that the Army should develop outreach and treatment programs for new soldiers based on the realization that a nontrivial proportion of its new recruits come into the Army with a history of suicidal behavior and mental disorders that are risk factors for suicidal behaviors. It is striking in this regard that the pre-enlistment mental disorders considered herein are associated with more than one-third of post-enlistment first suicide attempts.
The AAS lifetime suicide ideation and plan prevalence estimates are virtually identical to those in a recent study24 of suicidal behavior in a nationally representative civilian sample weighted to be sociodemographically comparable to the US Army, although a broader definition of ideation is used herein. Interestingly, the proportions of these outcomes in the AAS beginning prior to enlistment (58.2%–52.9%) are substantially lower than in the civilian sample based on a simulated age-at-enlistment distribution (82.4%–68.4%), whereas post-enlistment onsets are considerably higher in the AAS than the matched civilian sample for ideation (5.8% vs 2.5%) and plans (2.5% vs 1.7%). Post-enlistment first suicide attempts are the same in the AAS (1.3%) and civilian sample (1.2%). The lower AAS pre-enlistment rates of suicidal behavior are consistent with the fact that the Army may reject applicants with a known history of suicidal behavior, although our results show that a meaningful proportion of recruits have a history of suicidal behavior that is not known to the Army, despite the fact that Army recruiters ask about past suicidal behaviors in recruitment screening interviews. The suggestion that post-enlistment first onsets of suicidal ideation and suicide plans are higher among soldiers than civilians is consistent with soldiers being exposed to more severe stressors than civilians.25 These stressors can lead to suicidal behavior.26,27 It is less clear, though, why prevalence estimates of post-enlistment nonfatal suicide attempts would be no higher among soldiers than civilians, especially in light of clear evidence that the Army suicide rate has been on the rise in recent years and now exceeds the civilian population rate.3 One possibility is that the lethality of suicide attempts might be higher among soldiers than civilians, perhaps owing to the fact that a higher percentage of service members (61%) than civilians (50.5%) use firearms to kill themselves.28,29 This possibility highlights the potential importance of means control (ie, restricting access to lethal means [such as firearms]) as a suicide prevention intervention strategy.
The results regarding sociodemographic6,30 and Army career4,31 predictors of suicidal behavior are generally consistent with previous research. One important exception is the lower odds of suicide attempts among unmarried soldiers, which is inconsistent with the lower rates of suicidal behaviors among married vs unmarried civilians.30,32 This discrepancy might mean that marriage is less protective among soldiers than civilians, a possibility consistent with evidence of special marital stressors among military personnel (eg, deployments and frequent moves)33 and higher rates of mental illness among married vs unmarried AAS respondents.12 We need to see if this pattern replicates in additional Army STARRS data and, if so, to investigate why the protective effects of marriage are eroded among soldiers. Our finding of a low number of suicide attempts among Special Operations soldiers may reflect a lower baseline risk of suicidal behavior or high level of resilience among soldiers selected for this command.34,35
These results provide a more fine-grained picture than previous studies of the associations between mental disorders and subsequent suicidal behavior among soldiers. It is noteworthy that most post-enlistment–onset disorders were associated with significantly elevated odds of first post-enlistment suicide attempts in bivariate models, but that only MDD and IED remained significant in multivariate models. This reflects the high comorbidity among mental disorders and suggests that only a few disorders are critical predictors of suicidal behavior. Although IED might not be foremost in the minds of clinicians as a risk factor for suicide attempts among new soldiers, it is important to note that it is the most prevalent pre-enlistment disorder of all those assessed, has a strong association with suicide attempts, and has been consistently associated with attempts in prior studies.7,36,37 Intermittent explosive disorder was also the only pre-enlistment disorder associated with significantly elevated risk of post-enlistment first suicide attempts. These results suggest that screening Army applicants for IED and providing early treatment for new soldiers with IED might be valuable ways to reduce suicidal behaviors among soldiers, especially given that post-enlistment IED is also a significant predictor of post-enlistment suicide attempts.
Disaggregation of the 5 significant associations between mental disorders and post-enlistment suicide attempts revealed that 4 of the 5 associations (ie, pre-enlistment panic disorder and IED and post-enlistment MDD and IED) predict suicidal ideation, but only post-enlistment IED predicts the transition from ideation to suicide attempts. The finding that MDD predicts ideation but not plans or attempts among soldiers with ideation mirrors the resultsfromcivilianstudies,7 whereas IED has consistently been found to predict suicide attempts in the few previous studies in which it was considered.7,36,37
Conclusions
The finding that pre-enlistment panic disorder and PTSD were both associated with lower odds of post-enlistment first suicide attempts is inconsistent with previous civilian studies,7,37–39 although one large-scale study of veterans also found a decreased risk of suicide among those with PTSD,40,41 which was interpreted as being due to the provision of enhanced PTSD treatment for veterans. Importantly, disaggregation herein showed that these significant negative associations were quite consistent in predicting ideation in the total sample, plans among ideators, and attempts among ideators controlling for plans, which argues against the otherwise plausible possibility that 2 significant negative coefficients might have occurred by chance in the examination of such a large number of associations. Another possibility is that pre-enlistment histories of PTSD and panic disorder might be markers of resilience among people who enlist in the Army, even though they are markers of vulnerability in the general population.7 Although an empirical investigation of this possibility exceeds the scope of the present report, it warrants further examination in future studies given the strength and consistency of these associations.
Acknowledgments
Funding/Support: Army STARRS was sponsored by the Department of the Army and funded under cooperative agreement U01MH087981 with the US Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health (NIMH).
Role of the Sponsor: The sponsors specified the topic in the request for proposal but had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. However, as a cooperative agreement, collaborating scientists appointed to the project by the NIMH (Drs Colpe and Schoenbaum) and Army liaisons/consultants (COL Steven Cersovsky, MD, MPH [USAPHC], and Kenneth Cox, MD, MPH [USAPHC]) participated in the refinement of the study protocol originally proposed by Drs Ursano, Kessler, and Heeringa. Dr Colpe additionally collaborated in the creation of the data collection instruments and supervision of Army STARRS AAS data collection, while Dr Schoenbaum collaborated in the acquisition of the administrative data that are linked to AAS survey reports. None of the Army or NIMH collaborators was involved in planning or supervising data analyses for this report, but Drs Colpe and Schoenbaum both read the first draft and offered suggestions for revision. Although a draft of this manuscript was submitted to the Army and NIMH for review and comment prior to submission, this was with the understanding that comments would be no more than advisory.
Footnotes
Author Contributions: Dr Kessler had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Nock, Heeringa, Ursano, Colpe, Naifeh, Schoenbaum, Kessler.
Acquisition of data: Nock, Heeringa, Ursano, Schoenbaum, Kessler.
Analysis and interpretation of data: Nock, Stein, Heeringa, Ursano, Fullerton, Hwang, Sampson, Schoenbaum, Zaslavsky, Kessler.
Drafting of the manuscript: Nock, Stein, Ursano, Kessler.
Critical revision of the manuscript for important intellectual content: Nock, Stein, Heeringa, Colpe, Fullerton, Hwang, Naifeh, Sampson, Schoenbaum, Zaslavsky, Kessler.
Statistical analysis: Heeringa, Hwang, Sampson, Schoenbaum, Zaslavsky.
Obtained funding: Nock, Heeringa, Ursano, Schoenbaum, Kessler.
Administrative, technical, and material support: Nock, Heeringa, Ursano, Colpe, Fullerton, Naifeh, Sampson, Schoenbaum, Kessler.
Study supervision: Nock, Ursano, Sampson, Kessler.
Conflict of Interest Disclosures: In the past 5 years, Dr Kessler has been a consultant for Eli Lilly, GlaxoSmithKline, Integrated Benefits Institute, Ortho-McNeil Janssen Scientific Affairs, Pfizer, sanofi-aventis, Shire US, and Transcept Pharmaceuticals and has served on advisory boards for Johnson & Johnson. Dr Kessler received research support for his epidemiological studies during this period from Eli Lilly, EPI-Q, GlaxoSmithKline, Ortho-McNeil Janssen Scientific Affairs, sanofi-aventis, Shire US, and Walgreens. Dr Kessler owns a 25% share in DataSta. In the last 3 years, Dr Stein has been a consultant for Healthcare Management Technologies and received research support for pharmacological imaging studies from Janssen. No other disclosures were reported.
The Army STARRS Collaborators: The Army STARRS collaborators consist of coprincipal investigators: Robert J. Ursano, MD (Uniformed Services University of the Health Sciences) and Murray B. Stein, MD, MPH (University of California, San Diego, and VA San Diego Healthcare System); site principal investigators Steven Heeringa, PhD (University of Michigan) and Ronald C. Kessler, PhD (Harvard Medical School); NIMH collaborating scientists Lisa J. Colpe, PhD, MPH. and Michael Schoenbaum, PhD; and Army liaisons/consultants COL Steven Cersovsky, MD, MPH (USAPHC), and Kenneth Cox, MD, MPH (USAPHC). Other team members included Pablo A. Aliaga, MA (Uniformed Services University of the Health Sciences); COL David M. Benedek, MD (Uniformed Services University of the Health Sciences); Susan Borja, PhD (NIMH); Gregory G. Brown, PhD (University of California, San Diego); Laura Campbell-Sills, PhD (University of California, San Diego); Catherine L. Dempsey, PhD, MPH (Uniformed Services University of the Health Sciences); Richard Frank, PhD (Harvard Medical School); Carol S. Fullerton, PhD (Uniformed Services University of the Health Sciences); Nancy Gebler, MA (University of Michigan); Robert K. Gifford, PhD (Uniformed Services University of the Health Sciences); Stephen E. Gilman, ScD (Harvard School of Public Health); Marjan G. Holloway, PhD (Uniformed Services University of the Health Sciences); Paul E. Hurwitz, MPH (Uniformed Services University of the Health Sciences); Sonia Jain, PhD (University of California, San Diego); Tzu-Cheg Kao, PhD (Uniformed Services University of the Health Sciences); Karestan C. Koenen, PhD (Columbia University); Lisa Lewandowski-Romps, PhD (University of Michigan); Holly Herberman Mash, PhD (Uniformed Services University of the Health Sciences); James E. McCarroll, PhD, MPH (Uniformed Services University of the Health Sciences); Katie A. McLaughlin, PhD (Harvard Medical School); James A. Naifeh, PhD (Uniformed Services University of the Health Sciences); Matthew K. Nock, PhD (Harvard University); Rema Raman, PhD (University of California, San Diego); Nancy A. Sampson, BA (Harvard Medical School); LCDR Patcho Santiago, MD, MPH (Uniformed Services University of the Health Sciences); Michaelle Scanlon, MBA (NIMH); Jordan Smoller, MD, ScD (Harvard Medical School); Nadia Solovieff, PhD (Harvard Medical School); Michael L. Thomas, PhD (University of California, San Diego); and Alan M. Zaslavsky, PhD (Harvard Medical School).
Disclaimer: The content of this article is solely the responsibility of the authors and does not necessarily represent the views of the Department of Health and Human Services, the National Institute of Mental Health, the Department of the Army, or the Department of Defense.
Additional Information: A complete list of Army STARRS publications can be found at http://www.armystarrs.org.
References
- 1.Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE, editors. Reducing Suicide: A National Imperative. Washington, DC: The National Academies Press; 2002. [PubMed] [Google Scholar]
- 2.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30(1):133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nock MK, Deming CA, Fullerton CS, et al. Suicide among soldiers: a review of psychosocial risk and protective factors. Psychiatry. 2013;76(2):97–125. doi: 10.1521/psyc.2013.76.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bachynski KE, Canham-Chervak M, Black SA, Dada EO, Millikan AM, Jones BH. Mental health risk factors for suicides in the US Army, 2007–8. Inj Prev. 2012;18(6):405–412. doi: 10.1136/injuryprev-2011-040112. [DOI] [PubMed] [Google Scholar]
- 5.Haney EM, O’Neil ME, Carson S, et al. Suicide Risk Factors and Risk Assessment Tools: A Systematic Review. Portland, OR: Department of Veterans Affairs; 2012. [PubMed] [Google Scholar]
- 6.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(8):868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kessler RC, Colpe LJ, Fullerton CS, et al. Design of the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) Int J Methods Psychiatr Res. 2013;22(4):267–275. doi: 10.1002/mpr.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heeringa SG, Gebler N, Colpe LJ, et al. Field procedures in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) Int J Methods Psychiatr Res. 2013;22(4):276–287. doi: 10.1002/mpr.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. Deerfield, IL: American Association for Public Opinion Research; 2009. [Google Scholar]
- 11.Kessler RC, Heeringa SG, Colpe LJ, et al. Response bias, weighting adjustments, and design effects in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) Int J Methods Psychiatr Res. 2013;22(4):288–302. doi: 10.1002/mpr.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Heeringa SG, Stein MB, et al. Army STARRS Collaborators Thirty-day prevalence of DSM-IV mental disorders among nondeployed soldiers in the US Army: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) [published online March 5, 2014] JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2014.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Posner K, Brown GK, Stanley B, et al. The Columbia–Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–1277. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Merikangas KR, Jin R, He JP, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68(3):241–251. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: the family history screen. Arch Gen Psychiatry. 2000;57(7):675–682. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, Santiago PN, Colpe LJ, et al. Clinical reappraisal of the Composite International Diagnostic Interview Screening Scales (CIDI-SC) in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) Int J Methods Psychiatr Res. 2013;22(4):303–321. doi: 10.1002/mpr.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 19.Halli SS, Rao KV. Advanced Techniques of Population Analysis. New York, NY: Plenum; 1992. [Google Scholar]
- 20.Efron B. Logistic regression, survival analysis, and the Kaplan-Meier curve. J Am Stat Assoc. 1988;83(402):414–425. doi: 10.1080/01621459.1988.10478612. [DOI] [Google Scholar]
- 21.Cox C, Li X. Model-based estimation of the attributable risk: a loglinear approach. Comput Stat Data Anal. 2012;56(12):4180–4189. doi: 10.1016/j.csda.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rothman K, Greenland S. Modern Epidemiology. 2. Philadelphia, PA: Lippincott Williams & Wilkins; 1998. [Google Scholar]
- 23.Wolter KM. Introduction to Variance Estimation. New York, NY: Springer-Verlag; 1985. [Google Scholar]
- 24.Gadermann AM, Gilman SE, McLaughlin KA, et al. Projected rates of psychological disorders and suicidality among soldiers based on simulations of matched general population data. Mil Med. 2012;177(9):1002–1010. doi: 10.7205/milmed-d-12-00092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wells TS, Miller SC, Adler AB, Engel CC, Smith TC, Fairbank JA. Mental health impact of the Iraq and Afghanistan conflicts: a review of US research, service provision, and programmatic responses. Int Rev Psychiatry. 2011;23(2):144–152. doi: 10.3109/09540261.2011.558833. [DOI] [PubMed] [Google Scholar]
- 26.Bryan CJ, Rudd MD. Life stressors, emotional distress, and trauma-related thoughts occurring in the 24 h preceding active duty U.S. soldiers’ suicide attempts. J Psychiatr Res. 2012;46(7):843–848. doi: 10.1016/j.jpsychires.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 27.Stein DJ, Chiu WT, Hwang I, et al. Cross-national analysis of the associations between traumatic events and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS One. 2010;5(5):e10574. doi: 10.1371/journal.pone.0010574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bush NE, Reger MA, Luxton DD, et al. Suicides and suicide attempts in the U.S. Military, 2008–2010. Suicide Life Threat Behav. 2013;43(3):262–273. doi: 10.1111/sltb.12012. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC) Injury prevention and control: data and statistics (WISQARS) CDC website. http://www.cdc.gov/injury/wisqars/index.html. Accessed January 31, 2014.
- 30.Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuehn BM. Military probes epidemic of suicide: mental health issues remain prevalent. JAMA. 2010;304(13):1427–1430. 1429–1430. doi: 10.1001/jama.2010.1327. [DOI] [PubMed] [Google Scholar]
- 32.Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: a national register-based study of all suicides in Denmark, 1981–1997. Am J Psychiatry. 2003;160(4):765–772. doi: 10.1176/appi.ajp.160.4.765. [DOI] [PubMed] [Google Scholar]
- 33.Reinkober Drummet A, Coleman M, Cable S. Military families under stress: implications for family life education. Fam Relat. 2003;52(3):279–287. doi: 10.1111/j.1741-3729.2003.00279.x. [DOI] [Google Scholar]
- 34.Morgan CA, III, Wang S, Mason J, et al. Hormone profiles in humans experiencing military survival training. Biol Psychiatry. 2000;47(10):891–901. doi: 10.1016/s0006-3223(99)00307-8. [DOI] [PubMed] [Google Scholar]
- 35.Vythilingam M, Nelson EE, Scaramozza M, et al. Reward circuitry in resilience to severe trauma: an fMRI investigation of resilient special forces soldiers. Psychiatry Res. 2009;172(1):75–77. doi: 10.1016/j.pscychresns.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.James A, Lai FH, Dahl C. Attention deficit hyperactivity disorder and suicide: a review of possible associations. Acta Psychiatr Scand. 2004;110(6):408–415. doi: 10.1111/j.1600-0447.2004.00384.x. [DOI] [PubMed] [Google Scholar]
- 37.Nock MK, Hwang I, Sampson N, et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med. 2009;6(8):e1000123. doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brenner LA, Betthauser LM, Homaifar BY, et al. Posttraumatic stress disorder, traumatic brain injury, and suicide attempt history among veterans receiving mental health services. Suicide Life Threat Behav. 2011;41(4):416–423. doi: 10.1111/j.1943-278X.2011.00041.x. [DOI] [PubMed] [Google Scholar]
- 39.Wilcox HC, Storr CL, Breslau N. Posttraumatic stress disorder and suicide attempts in a community sample of urban American young adults. Arch Gen Psychiatry. 2009;66(3):305–311. doi: 10.1001/archgenpsychiatry.2008.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pfeiffer PN, Ganoczy D, Ilgen M, Zivin K, Valenstein M. Comorbid anxiety as a suicide risk factor among depressed veterans. Depress Anxiety. 2009;26(8):752–757. doi: 10.1002/da.20583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zivin K, Kim HM, McCarthy JF, et al. Suicide mortality among individuals receiving treatment for depression in the Veterans Affairs health system: associations with patient and treatment setting characteristics. Am J Public Health. 2007;97(12):2193–2198. doi: 10.2105/AJPH.2007.115477. [DOI] [PMC free article] [PubMed] [Google Scholar]


