Abstract
Objective
In certain countries, it is not uncommon to turn to professionals outside the conventional health care system for psychological problems. As this situation is not well documented in Europe, we assessed use of nonconventional care for mental health in 6 European countries.
Method
A cross-sectional survey was conducted in representative samples of, noninstitutionalized adults in 6 European countries. Participants (n = 8796) completed a survey, which included, among other items, the Composite International Diagnostic Interview 3.0 and in-depth questions about lifetime consultations for mental health problems.
Results
Among the respondents (n = 2928) who reported having already sought help in their lifetime for psychological problems (20.0%), 8.6% turned to complementary and alternative medicine (CAM) providers, such as chiropractors and herbalists, and a similar proportion (8.4%) to religious advisers such as ministers, priests, or rabbis. Only a small proportion (2.9%) consulted only these professionals for their problems. CAM providers were more frequently used in the Netherlands (13.5%) and Germany (9.4%), while religious advisers were more often consulted in Italy (12.6%) and Germany (11.6%). Multivariate analyses confirmed differences between countries and revealed that people turning to religious advisers tended to be older, foreign born, and with alcohol problems, whereas those consulting CAM providers were younger, wealthier, and more frequently depressed.
Conclusions
In Europe, patients who turn to CAM therapists and those who seek help from religious advisers for psychological problems are not exactly the same. In addition, these professionals are not consulted frequently in most countries, and are almost always associated with more traditional follow-up when used.
Keywords: use of services, nonconventional professionals, mental problems
Recent studies conducted in the United States and in Europe have indicated that demand for care for common mental disorders has increased considerably in the last decades,1,2 although their prevalence has remained relatively stable.1–4 One of the reasons for this growing demand may be changes in public attitudes.5 Seeking help for nonpsychotic symptoms has become more acceptable and perceived stigma has declined. Recourse to health professionals for psychological problems, especially to mental health specialists, and its determinants are well documented in the literature. In particular, several studies have indicated that people who turn to mental health specialists for their problems are relatively young, with a higher educational level than those followed in general practice.6,7 However, other care providers, who are not in the conventional health care sector, may also be involved in the treatment of psychological problems, but little is known about them, and particularly about how their care articulates with more traditional medical follow-up.
Recent national epidemiologic surveys have shown the particular importance of nonhealth professionals in the management of mental health problems in certain countries, notably the United States, where the proportion of the population seeking help from this sector is one of the highest in the world.8 The National Comorbidity Survey Replication revealed that 2.8% of Americans had turned at least once in the previous year to CAM providers, such as chiropractors and herbalists, and 3.4% turning to human services (that is, clergy and social workers or counsellors practising outside the specialty mental health sector) for problems with their emotions or nerves or their use of alcohol or drugs.7,8 Among the Americans surveyed who suffered from a mental condition, the proportion of users ranged from 4.5% to 6.8% for CAM, and was around 8.1% for human services.7,9 In addition, certain studies have indicated that the use of such providers may vary depending on the type of mental problem, notably with higher consultation rates for mood disorders.7,10
For Europe, the ESEMeD, which is part of the WHO WMH Survey Initiative, provides the opportunity to study recourse to this sector in 6 European countries and to compare extent of use with the United States, the definitions used for the 2 categories of nonhealth professionals being, however, slightly different. Although some information on prevalence rates has been published previously,8 no in-depth study has been performed. The specific aims of the present study were 3-fold: first, to assess the frequency of use of these professionals in the management of mental problems; second, to identify the personal, health-related, and social factors associated with the use of such care, and finally to determine if such services were complements to, or substitutes for, more traditional follow-up, in particular for people with a diagnosis of mental illness who are the most in need.
Methods
The ESEMeD is part of the WHO WMH Survey Initiative.11 Briefly, ESEMeD is a cross-sectional survey based on random samples representative of the noninstitutionalized adult population of 6 European countries. A detailed description of the sampling methods is provided elsewhere.12 Eligible people were interviewed face-to-face by trained lay interviewers at their homes after they had given consent. The questionnaire, subdivided into 38 different sections, was administered using computer-assisted interview techniques. To optimize the interviewing process and reduce cost, a 2-stage interview procedure was used. The first part of the questionnaire assessed diagnosis of the most common mood and anxiety disorders, health-related quality of life, health services use and demographics in all respondents. The second stage of the interview only concerned subjects who reported more than a prespecified number of symptoms of specific mood or anxiety disorders, as well as a random 25% of the rest of the sample. This second part of the questionnaire included, among other items, an in-depth interview about additional mental disorders, self-reported chronic physical conditions, and risk factors.
Sample
In total, 21 425 people were interviewed between January 2001 and August 2003. The overall response rate in the 6 countries was 61.2%, with the highest rates observed in Spain (78.6%) and Italy (71.2%) and the lowest in Germany (57.8%), the Netherlands (56.4%), Belgium (50.6%), and France (45.9%). In this analysis, only subjects participating in the second stage of the interview have been considered (n = 8796).
Lifetime Use of Health Services for Mental Health Problems
One section of the questionnaire was devoted to questions on use of services for mental health problems. Respondents were asked first if they had previously consulted for a mental health problem:
SR1. The next question is about speaking with professionals about problems with emotions or mental health. By professionals, we mean medical doctors, nurses, psychologists, social workers, spiritual advisers, herbalists, and any other healing professionals. With this definition in mind, did you ever in your life talk to a medical doctor or other professional about any problem with your emotions or mental health?
People reporting any contact with a provider for a mental health problem were asked to select whom they consulted from a list of health professionals (including psychiatrists; other mental health professionals; general practitioners; other medical specialists; other health professionals), and of nonhealth care professionals:
| SR2. | Did you ever in your life talk to any of the following types of professionals about problems with your emotions or mental health: |
| SR2a. | A psychiatrist? |
| SR2b. | Any other mental health professional, such as a psychologist, psychotherapist, social worker, or counsellor? |
| SR2c. | A general family doctor? |
| SR2d. | Any other doctor, such as a cardiologist? |
| SR2e. | Any other health professional, such as a nurse or a nutritionist? |
| SR2f. | A religious or spiritual adviser, such as a minister, priest, or rabbi? |
| SR2g. | Any other healer, such as an herbalist, chiropractor, or spiritualist? |
In the WMH surveys, nonhealth care professionals were divided into 2 categories as described previously in Wang et al,8 namely, human services (religious or spiritual advisers, social workers, or counsellors in any setting other than a specialty mental health setting) and, conversely, CAM providers (any other type of healers such as herbalists, chiropractors, or spiritualists, participation in an Internet support group, or participation in a self-help group). However, the European version of the WMH survey questionnaire (ESEMeD) only mentioned religious or spiritual advisers for human services and did not collect information on use of Internet support groups or self-help groups for inclusion in CAM providers.
Mental Health Disorders
Information on mental health was collected using the CIDI 3.0, which was developed and adapted by the WHO Coordinating Committee for their WMH Survey Initiative.13 The diagnostic sections were expanded in CIDI 3.0 to include a measure of impairment, which allows the severity of any mental disorders to be assessed. The diagnosis of mental disorders was made using the criteria of the DSM-IV. A clinical reappraisal conducted in parallel to the main ESEMeD survey showed that diagnoses assigned with the CIDI 3.0 were concordant with clinical diagnoses based on the Structured Clinical Interview for DSM-IV Diagnosis (Axis I).14 The mental disorders considered in this study were: mood disorders (major depression and dysthymia), anxiety disorders (social phobia, specific phobia, generalized anxiety disorder. agoraphobia with or without panic disorder, panic disorder, and posttraumatic disorder), and alcohol-related disorders (dependence and abuse).
Statistical Analysis
The chi-square test was used to evaluate differences between proportions for 2 or more groups and the adjusted Wald test to assess equality of 2 proportions. Multiple logistic regression analyses were used to assess the influence of demographic variables, clinical variables, and country on the use of services. A probability level of 0.05 was deemed statistically significant.
Data for individual subjects were weighted to account for the known probabilities of selection as well as to restore the age and sex distribution of the population within countries and the relative sample size between countries. All the results presented here are weighted. The weighting procedure is described in detail elsewhere.12 The Taylor linearized variance estimator was used for statistical inference to take into account the complexity of the sampling design. The statistical analysis was performed using Stata software.15
Results
In all countries, the majority of respondents were women (51.8%). All other sociodemographic characteristics differed between countries, notably the proportion of people living in a rural area (P < 0.001).
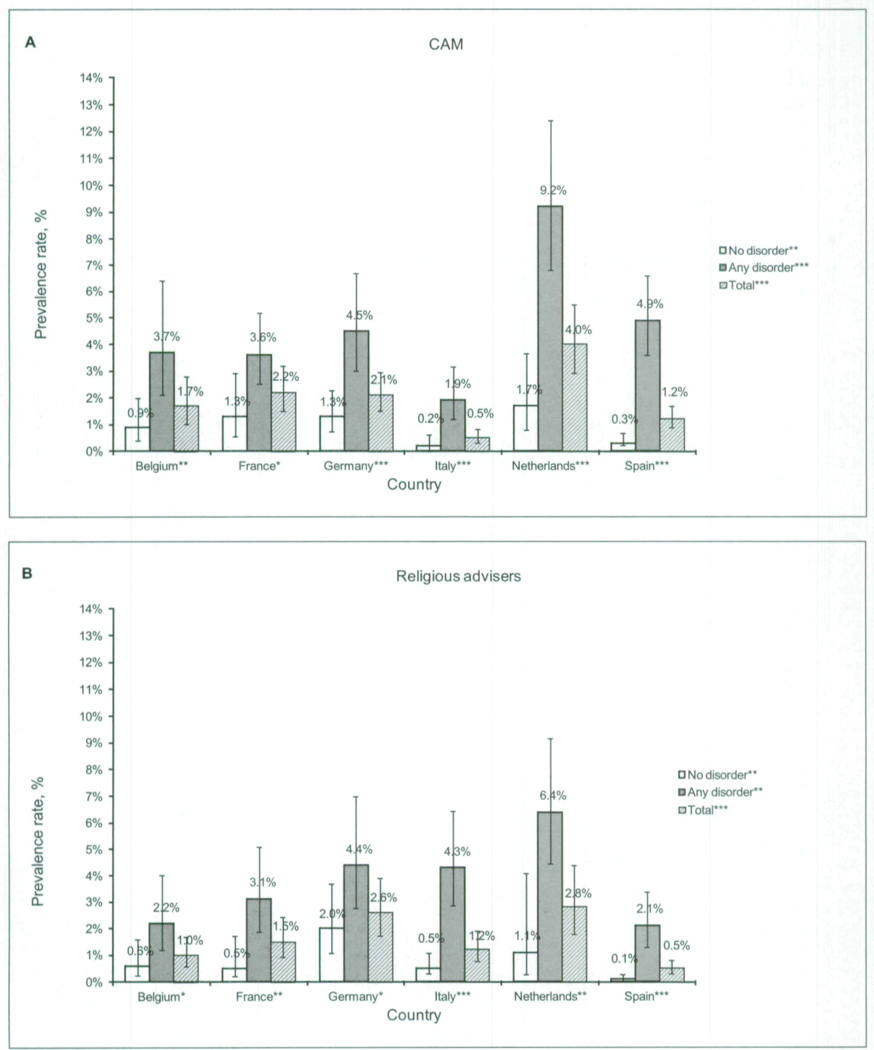
Among the 8796 respondents, 2928 (20.0%) declared having already contacted a professional for a psychological problem. Subjects reporting having sought help outside the conventional health care system were relatively few, with the same proportion of respondents (1.7%) found for CAM therapists and for religious advisers. However, as shown in Figure 1, significant variations between countries were found (P < 0.001, for both types of providers), with the lowest rates observed in Italy (0.5%) for CAM therapists and in Spain (0.5%) for religious advisers and the highest in the Netherlands for both types of providers (4.0% and 2.8%, respectively). As expected, in all countries, higher rates of contact were observed in people having been diagnosed with a mental disorder. For instance, in the Netherlands, nearly 1 person out of 10 with a diagnosis of mental illness (9.2%) reported having turned to CAM therapists to deal with their problems.
Figure 1.
Proportion of participants reporting lifetime consultations either with CAM providers (A) or religious advisers (B) for mental health problems in the total study sample, by country and mental health status according to DSM-IV criteria (n = 8796)
Inter-group and -country differences were assessed using the chi-square test (* P < 0.05; ** P < 0.01 ; *** P < 0.001).
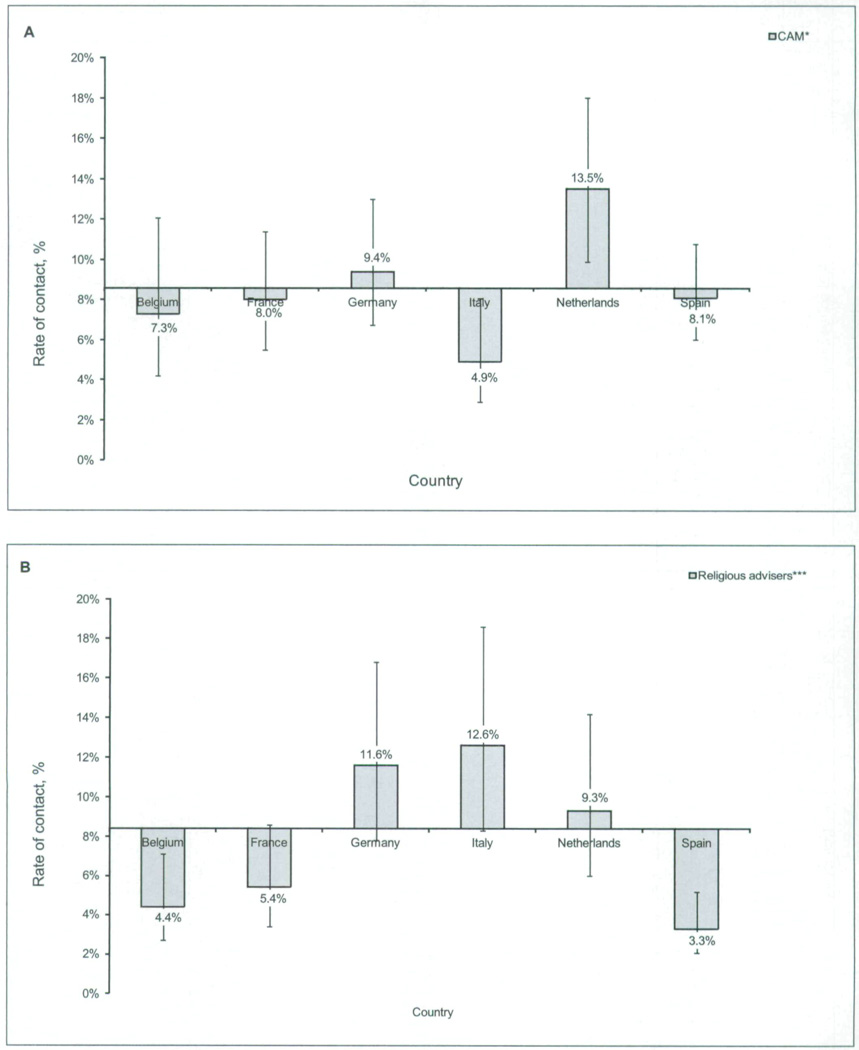
To account for the differences between countries in the proportion of subjects seeking help for their psychological problems, with Italians 3 times less likely to have consulted than Netherlanders (9.7% and 29.9%, respectively), we also examined prevalence rates among the 2928 respondents reporting contacts with any professional. CAM providers (8.6%) were consulted as frequently as religious advisers (8.4%), with wide variation between countries observed, both for CAM providers (P = 0.02) and for religious advisers (P < 0.001). As shown in Figure 2, rates of contact with CAM providers were highest in the Netherlands (13.5%) and Germany (9.4%), while contact with religious advisers were highest in Italy (12.6%), Germany (11.6%), and the Netherlands (9.3%). The lowest contact rate was observed in Italy (4.9%) for CAM providers and in Spain (3.3%) for religious advisers. No significant difference in rates of contact according to mental health status was found, with the exception of Spain, where people diagnosed with a mental illness had higher rates of contact with CAM therapists (11.0% and 4.1%, respectively; χ2 = 33.3, df= 1, P = 0.01) or religious advisers (4.7% and 1.5%, respectively; χ2 = 17.3, df=1,P = 0.01) than those without any mental disorder (data not presented).
Figure 2.
Estimated prevalence rates, with 95% CIs and mean, of participants who reported consulting with either a CAM provider (A) or a religious adviser (B) for mental health problems in their lifetime (n = 2928)
The mean prevalence rate, represented by the horizontal line, in the 6 countries studied was 8.6% for CAM providers and 8.4% for religious advisers. For each type of provider, potential differences in prevalence rates between countries were assessed using the χ2 test. The adjusted Wald test for equality of 2 proportions revealed that rates of contact with CAM providers were significantly different between the Netherlands and each other country except Germany and between Germany and Italy. For religious advisers, significant differences were found between Italy or Germany and each other country and between the Netherlands and Belgium or Spain.
Multiple logistic regression analysis was performed to assess the influence of sociodemographic and clinical variables on the use of professionals outside the conventional health care system in case of a psychological problem (Table 1). Variables associated with an increased likelihood of seeking help from these sources, compared with from health professionals only, included female sex, higher education, high income, living in a rural area, and suffering from depression. However, when comparing the profile of the users of CAM providers with that of people who contact religious advisers, some differences, sometimes close to significance, were identified, especially regarding age, country of birth, and mental health status. Indeed, people who sought help from CAM providers were younger, less likely to be born in a foreign country, and less frequently affected by problems with alcohol than those who turned to religious advisers. In addition, this analysis confirmed the higher probability of using both types of nonhealth professionals in Germany and in the Netherlands, as well as a lower probability of using CAM providers combined with a higher probability of contacting religious advisers in Italy, and a lower probability of contacting religious advisers in Spain.
Table 1.
Factors associated with lifetime consultation with professionals outside the conventional health care system in the ESEMeD countries, compared with consultation with health professionals only (n = 2423)
| CAM provider n = 331 |
Religious adviser n = 227 |
Any nonhealth professional n = 505 |
||||
|---|---|---|---|---|---|---|
| Characteristic | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Sociodemographic variable | ||||||
| Sex | ||||||
| Male | 1.00 | 1.00 | 1.00 | |||
| Female | 1.48 | 0.95–2.31 | 1.48 | 0.89–2.47 | 1.52 | 1.04–2.21 |
| Age, years | ||||||
| 18 to 39 | 1.03 | 0.66–1.59 | 1.02 | 0.61–1.70 | 1.13 | 0.78–1.62 |
| 40 to 59 | 1.00 | 1.00 | 1.00 | |||
| ≥60 | 0.53 | 0.27–1.05 | 1.76 | 0.94–3.29 | 1.07 | 0.66–1.73 |
| Marital status | ||||||
| Married, cohabiting with someone | 1.00 | 1.00 | 1.00 | |||
| Separated, widow, divorced, or single | 1.05 | 0.67–1.65 | 1.38 | 0.85–2.22 | 1.13 | 0.78–1.63 |
| Educational level | ||||||
| Primary or secondary | 1.00 | 1.00 | 1.00 | |||
| Post-secondary | 1.31 | 0.82–2.09 | 1.87 | 1.05–3.33 | 1.54 | 1.03–2.32 |
| Born in the country of residence | ||||||
| Yes | 1.00 | 1.00 | 1.00 | |||
| No | 0.25 | 0.13–0.47 | 0.71 | 0.26–1.93 | 0.50 | 0.22–1.10 |
| Income level | ||||||
| Low | 0.69 | 0.42–1.14 | 1.14 | 0.63–2.06 | 0.94 | 0.61–1.45 |
| Average | 1.00 | 1.00 | 1.00 | |||
| High | 1.78 | 1.08–2.94 | 1.44 | 0.77–2.70 | 1.57 | 1.00–2.45 |
| Population size of community | ||||||
| <10 000 | 1.88 | 1.15–3.08 | 1.54 | 0.82–2.87 | 1.66 | 1.07–2.56 |
| 10 000 to 100 000 | 1.00 | 1.00 | 1.00 | |||
| > 100 000 | 1.04 | 0.65–1.68 | 1.32 | 0.76–2.30 | 1.10 | 0.73–1.65 |
| Countrya | ||||||
| Belgium | 0.89 | 0.54–1.46 | 0.65 | 0.39–1.07 | 0.73 | 0.50–1.08 |
| France | 0.81 | 0.57–1.16 | 0.69 | 0.45–1.07 | 0.72 | 0.53–0.98 |
| Germany | 1.46 | 1.02–2.07 | 1.97 | 1.28–3.03 | 1.66 | 1.21–2.29 |
| Italy | 0.52 | 0.31–0.88 | 1.64 | 1.02–2.64 | 1.00 | 0.66–1.50 |
| The Netherlands | 2.06 | 1.43–2.98 | 1.61 | 0.98–2.63 | 1.79 | 1.29–2.48 |
| Spain | 0.89 | 0.63–1.24 | 0.43 | 0.27–0.68 | 0.64 | 0.47–0.86 |
| Clinical variableb | ||||||
| Mood disorder during lifetime | ||||||
| Yes | 1.62 | 1.11–2.37 | 1.22 | 0.79–1.88 | 1.44 | 1.05–1.97 |
| No | 1.00 | 1.00 | 1.00 | |||
| Anxiety disorder during lifetime | ||||||
| Yes | 1.25 | 0.88–1.79 | 1.05 | 0.68–1.63 | 1.19 | 0.87–1.63 |
| No | 1.00 | 1.00 | 1.00 | |||
| Alcohol disorder during lifetime | ||||||
| Yes | 0.58 | 0.31–1.08 | 0.98 | 0.41–2.36 | 0.80 | 0.44–1.47 |
| No | 1.00 | 1.00 | 1.00 | |||
ORs were calculated with respect to the overall mean.
The presence of mental disorders was assessed over lifetime.
Table 2 compares subjects who consulted CAM providers only (n = 278) with those who contacted religious advisers only (n = 174). The results confirm the differences between the 2 clienteles observed previously. Subjects who turned to CAM providers were much younger and less likely to be foreign born than those who contacted religious advisers. Moreover, when people with alcohol use disorders turned to professionals outside the conventional health care system, they were less likely to seek help from CAM providers than from religious advisers. Another trend indicated that people who turned to CAM providers may have been wealthier. Finally, these results illustrate the strong contrast between the types of nonhealth professionals consulted in Italy and Spain, with Spaniards being much more inclined to seek help from CAM providers than from religious advisers, and the opposite being true with Italians.
Table 2.
Association with lifetime consultation with CAM only (n = 278), compared with religious advisers only (n = 174), among participants having outside the conventional health care system in their lifetime sought help from professionals (n = 505)
| Characteristic | OR | 95% CI |
|---|---|---|
| Sociodemographic variable | ||
| Sex | ||
| Male | 1.00 | |
| Female | 0.82 | 0.37–1.83 |
| Age, years | ||
| 18 to 39 | 1.29 | 0.64–2.60 |
| 40 to 59 | 1.00 | |
| ≥60 | 0.11 | 0.04–0.31 |
| Marital status | ||
| Married, cohabiting with someone | 1.00 | |
| Separated, widow, divorced, or single | 0.68 | 0.32–1.43 |
| Educational level | ||
| Primary, secondary | 1.00 | |
| Post-secondary | 0.59 | 0.28–1.25 |
| Born in the country of residence | ||
| Yes | 1.00 | |
| No | 0.18 | 0.04–0.74 |
| Income level | ||
| Low | 0.46 | 0.20–1.06 |
| Average | 1.00 | |
| High | 1.78 | 0.62–5.10 |
| Population size of community | ||
| <10 000 | 1.58 | 0.68–3.66 |
| 10 000 to 100 000 | 1.00 | |
| >100 000 | 0.70 | 0.31–1.57 |
| Countrya | ||
| Belgium | 1.75 | 0.70–4.34 |
| France | 1.70 | 0.86–3.38 |
| Germany | 0.66 | 0.36–1.20 |
| Italy | 0.15 | 0.07–0.32 |
| The Netherlands | 1.19 | 0.51–2.76 |
| Spain | 2.94 | 1.36–6.33 |
| Clinical variableb | ||
| Mood disorder | ||
| Yes | 1.34 | 0.68–2.64 |
| No | 1.00 | |
| Anxiety disorder | ||
| Yes | 1.45 | 0.72–2.95 |
| No | 1.00 | |
| Alcohol disorder | ||
| Yes | 0.26 | 0.07–0.88 |
| No | 1.00 | |
ORs were calculated with respect to the overall mean.
The presence of mental disorders was assessed over lifetime.
Finally, when users of services (n = 2928) are divided according to the type of providers consulted (Table 3), people having talked only to health professionals represent the majority of users (84.7%). However, significant variations between countries exist (P < 0.001), with the highest rates being observed in Spain (90.0%), Belgium (89.5%), and France (88.0%), and the lowest in the Netherlands (79.1%). People having consulted only professionals outside the health care system for their problems are very few (2.9%), although they represent 4.5% of the users in Germany and 3.7% in the Netherlands. However, a substantial proportion of users (12.4%) reported contacts with both types of providers, varying significantly (P = 0.02) from 8.9% in Spain to a 2-fold higher rate in the Netherlands (17.2%), a rate which is even higher in those diagnosed with a mental illness (22.7%). Interestingly, most of those who reported contacts with both types of providers have benefited from specialized care in the conventional health care sector.
Table 3.
Breakdown of the users of services according to the different types of providers they turned to, by country and mental health status according to DSM-IV criteria (%)
| Mental HPs with any non-HP | HPs not specialized in mental health only with any non-HP |
Non-HPs only | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | n | HP | CAM | RA | Both | Any | CAM | RA | Both | Any | CAM | RA | Both | Any |
| Total | ||||||||||||||
| No disorder | 645 | 86.1 | 3.1 | 3.0 | 1.5 | 7.6 | 1.0 | 1.6 | 0.0 | 2.6 | 1.5 | 1.8 | 0.4 | 3.7 |
| Any disorder | 2283 | 83.7 | 5.6 | 4.2 | 1.4 | 11.2 | 1.1 | 1.7 | 0.1 | 2.9 | 1.2 | 1.0 | 0.0 | 2.2 |
| Total | 2928 | 84.7 | 4.5 | 3.7 | 1.4 | 9.6 | 1.1 | 1.7 | 0.0 | 2.8 | 1.3 | 1.4 | 0.2 | 2.9 |
| Belgium | ||||||||||||||
| No disorder | 92 | 91.1 | 3.0 | 2.3 | 1.5 | 6.8 | 1.8 | 0.0 | 0.3 | 2.1 | 0.0 | 0.0 | 0.0 | 0.0 |
| Any disorder | 281 | 88.4 | 5.1 | 1.8 | 0.6 | 7.5 | 1.6 | 2.1 | 0.1 | 3.8 | 0.3 | 0.0 | 0.0 | 0.3 |
| Total | 373 | 89.5 | 4.2 | 2.0 | 10 | 7.2 | 1.7 | 1.2 | 0.2 | 3.1 | 0.2 | 0.0 | 0.0 | 0.2 |
| France | ||||||||||||||
| No disorder | 108 | 90.2 | 1.5 | 1.7 | 1.3 | 4.5 | 2.3 | 0.2 | 0.0 | 2.5 | 2.8 | 0.0 | 0.0 | 2.8 |
| Any disorder | 494 | 86.8 | 4.6 | 3.6 | 1.3 | 9.5 | 1.0 | 1.4 | 0.2 | 2.6 | 0.8 | 0.3 | 0.0 | 1.1 |
| Total | 602 | 88.0 | 3.5 | 2.9 | 1.3 | 7.7 | 1.5 | 1.0 | 0.1 | 2.6 | 1.6 | 0.1 | 0.0 | 1.7 |
| Germany | ||||||||||||||
| No disorder | 123 | 80.6 | 3.9 | 4.0 | 2.3 | 10.2 | 0.7 | 3.6 | 0.0 | 4.3 | 1.0 | 2.8 | 1.0 | 4.8 |
| Any disorder | 326 | 81.7 | 5.9 | 4.4 | 0.8 | 11.1 | 0.9 | 2.0 | 0.0 | 2.9 | 2.1 | 2.2 | 0.0 | 4.3 |
| Total | 449 | 81.2 | 4.9 | 4.2 | 1.6 | 10.7 | 0.8 | 2.8 | 0.0 | 3.6 | 1.5 | 2.5 | 0.5 | 4.5 |
| Italy | ||||||||||||||
| No disorder | 68 | 87.0 | 2.1 | 8.0 | 0.9 | 11.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 2.0 | 0.0 | 2.0 |
| Any disorder | 230 | 82.1 | 1.7 | 6.3 | 1.7 | 9.7 | 2.0 | 3.0 | 0.3 | 5.3 | 0.4 | 2.3 | 0.2 | 2.9 |
| Total | 298 | 84.2 | 1.8 | 7.0 | 1.4 | 10.2 | 1.2 | 1.7 | 0.2 | 3.1 | 0.2 | 2.2 | 0.1 | 2.5 |
| The Netherlands | ||||||||||||||
| No disorder | 101 | 83.7 | 7.5 | 0.2 | 0.0 | 7.7 | 0.0 | 1.2 | 0.0 | 1.2 | 2.1 | 5.3 | 0.0 | 7.4 |
| Any disorder | 425 | 76.0 | 10.0 | 64 | 2.6 | 19.0 | 1.7 | 1.6 | 0.4 | 3.7 | 1.3 | 0.0 | 0.0 | 1.3 |
| Total | 526 | 79.1 | 9.0 | 3.9 | 1.6 | 14.5 | 1.0 | 1.5 | 0.2 | 2.7 | 1.6 | 2.1 | 0.0 | 3.7 |
| Spain | ||||||||||||||
| No disorder | 153 | 94.7 | 1.8 | 0.8 | 0.3 | 2.9 | 0.6 | 0.0 | 0.0 | 0.6 | 1.4 | 0.4 | 0.0 | 1.8 |
| Any disorder Total | 527 | 86.4 | 7.6 | 1.9 | 2.0 | 11.5 | 0.8 | 0.7 | 0.1 | 1.6 | 0.5 | 0.0 | 0.0 | 0.5 |
| Total | 680 | 90.0 | 5.1 | 1.4 | 1.3 | 7.8 | 0.7 | 0.4 | 0.0 | 1.1 | 0.9 | 0.2 | 0.0 | 1.1 |
All data are presented as percentages.
HP = health professional; RA = religious adviser
Discussion
This study shows first that recourse to professionals outside the conventional health care system for psychological problems in Europe is less frequent than in the United States, although significant differences exist between European countries. Dutch and German interviewees were the most inclined to turn to either CAM professionals or religious advisers. Otherwise, markedly different profiles were seen between countries. For example, in Italy, people were much more likely to seek help from religious advisers than from CAM providers, whereas the opposite was true in Spain. Our results also reveal interesting differences between people who contacted religious advisers and those who contacted CAM providers. In particular, people who turned to religious advisers were more likely to be older, foreign born, and suffering from problems with alcohol, whereas those consulting CAM providers tended to be younger, wealthier, and more frequently depressed. However, both types of professionals attract a predominantly female clientele living in a rural area who were typically well educated, depressed, and with a relatively high income.
Some of the differences in recourse to these nonconventional providers between countries may be explained by differences in the availability of these professionals as well as in eligibility for reimbursement by health insurance (the latter is only relevant for CAM). For example, a recent study on religious advisers in Europe reports that their availability is particularly high in Italy and in Germany, and low in Spain.16 Moreover, regarding CAM, regulation of practice varies widely in Europe.17–19 In most European countries, including Belgium, France, Italy, and Spain, the practice of medicine is theoretically restricted to legally qualified health professionals only, whereas in the Netherlands and in Germany, it may be extended to practitioners without allopathic medical or paramedical training. Between-country differences in patterns of provision have been discussed extensively elsewhere in the context of the complexity of the legal and regulatory framework.17,18 Available data show that access to CAM practitioners is particularly high in Germany and in the Netherlands. In addition, although all countries in Europe have some form of insurance coverage for CAM, at least for treatments offered by qualified and licensed allopathic health professionals, the countries with the broadest coverage correspond to those with the highest density of professionals, namely, Gennany and the Netherlands.18,19
The only studies reporting factors associated with the use of CAM that have been published previously did not address the management of mental health problems specifically. However, note that some of the factors identified in these studies are similar to those identified here. An English study comparing patients of CAM therapists to patients frequenting more traditional services shows that people consulting CAM therapists were more likely to be female and better educated.20 Other studies evaluating use of alternative medicine therapies, rather than consultation of CAM providers, have yielded similar findings. For instance, being a woman and having a high educational level,21 as well as suffering from depression,22,23 have been found to be linked with higher uptake of these therapies, as have suffering from a long-term medical condition,21 or from anxiety.22,23 Conversely, little information is available on factors associated with contacts with human services professionals, particularly with religious advisers. Unsurprisingly, faith and religiosity were factors favouring recourse to the clergy.16 Conversely, other factors were also important, such as age,16,24 ethnicity, education, and type of disorder, a higher likelihood of such contact having been found for depressive and anxiety disorders.24
Interestingly, our study shows that, in Europe, professionals outside the conventional health care sector do not challenge conventional medical treatment of people suffering from psychological problems, especially for those with a diagnosis of mental illness. The intervention of such providers is most often complementary to conventional care. Indeed, only very few people interviewed in this survey reported having only turned to these providers to deal with their mental health problems. This contrasts with the situation in the United States, where recourse to such providers without any medical follow-up represents a significant mode of seeking help, even though a recent study has shown that the number of people using this sector has decreased during the last 10 years.25
Numerous limitations should be taken into account in interpreting these results. First, visits to professionals for a mental health problem were self-reported. Besides introducing recall bias, this method of ascertainment leads to a risk that some users of services for a mental health problem might not have considered they had such problem and thus could have skipped this section of the survey interview, which would lead to an underestimate of the number of users. Second, when administering the questionnaire, some respondents might have been confused about the different types of professionals. Third, the aim of our paper is to assess the use of categories of nonhealth care professionals to deal with mental health problems. The religious advisers category is relatively unambiguous. However, the CAM provider category is relatively less well characterized. In particular, the borderline between unconventional and conventional therapists may differ between countries (for example, the status of osteopaths) and some professionals in the conventional health care sector may offer alternative or complementary therapies (such as acupuncture, herbal medicine. aromatherapy, homeopathy, and hypnosis). Fourth, the power of some of the statistical analyses in our study may have been limited owing to the small number of users of each type of professionals in certain countries. Fifth, the severity of mental health problems was assessed only through the DSM-IV criteria in the 12 months preceding the interview. Moreover, our survey was limited to the most frequent mental disorders. Sixth, in Italy, there was a selection bias regarding immigrants as survey participants were randomly selected through electoral registries, which implies a high social integration of immigrants selected for participating in the ESEMeD survey. Finally, the response rate was relatively low in France.
Conclusion
In the European countries studied, CAM therapists and religious advisers attract different populations with different psychological problems. For public health, the situation this creates does not seem to present a major challenge to conventional care, as they appear to be essentially complementary to conventional medical follow-up. However, in some countries, such as the Netherlands and Germany, nonconventional care may play a significant role, notably for the most severe patients. However, to guide public health care policy, further studies are needed to explore further how such unconventional follow-up may coexist with traditional medical treatment, and the impact of such practices, together with their motivations and costs, on the effectiveness of, and compliance with, medical treatments with proven efficacy.
Ciinical implications.
CAM therapists and religious advisers attract different populations with different psychological problems.
Recourse to such providers is most often complementary to conventional medical treatment.
Limitations
Visits to CAM therapists and religious advisers were self-reported.
The borderline between conventional and unconventional therapists may vary between countries.
Acknowledgements
The ESEMeD survey was supported by the European Commission (Contracts QLG5–1999–01042; SANCO 2004123), the Piedmont Region (Italy), Fondo de Investigación Sanitaria, Instituto de Salud Carlos III, Spain (FIS 00/0028), Ministerio de Ciencia y Tecnología, Spain (SAF 2000–158-CE), Departament de Salut, Generalitat de Catalunya, Spain, and other local agencies and by an unrestricted educational grant from GlaxoSmittiKline.
This survey was carried out in conjunction with the WHO WMH Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the United States National Institute of Mental Health (R01MH070884), the John D and Catherine T MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R0I-MH069864, and ROl DA016558), the Fogarty International Center (FIRCA R01-TW00648I), the Pan American Health Organization, the Eli Lilly & Company, Ortho-McNeil Pharmaceutical, Inc, GlaxoSmithKline, Bristol Myers Squibb.
Abbreviations used in this article
- CAM
complementary and alternative medicine
- CIDI
Composite International Diagnostic Interview
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- ESEMeD
European Study of the Epidemiology of Mental Disorders
- WHO
World Health Organization
- WMH
World Mental Health
References
- 1.Kessler RC, Dernier O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352:2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kovess-Masféty V, Briffault X, Sapinho D. Prevalence, risk factors and use of health care in depression: a survey in a large region of France between 1991 and 2005. Can J Psychiatry. 2009;54(10):701–709. doi: 10.1177/070674370905401007. [DOI] [PubMed] [Google Scholar]
- 3.Ferriman A. Levels of neurosis remained static in the 1990s. BMJ. 2001;323:130. [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy JM, Horton NJ, Laird NM, et al. Anxiety and depression: a 40-year perspective on relationships regarding prevalence, distribution, and comorbidity. Acta Psyehiatr Scand. 2004;109:355–375. doi: 10.1111/j.1600-0447.2003.00286.x. [DOI] [PubMed] [Google Scholar]
- 5.Mojtabai R. Americans’ attitudes toward mental health treatment seeking: 1990–2003. Psyehiatr Serv. 2007;58:642–651. doi: 10.1176/ps.2007.58.5.642. [DOI] [PubMed] [Google Scholar]
- 6.Kovess-Masféty V, Alonso J, Brugha TS, et al. Differences in lifetime use of services for mental health problems in six European countries. Psyehiatr Serv. 2007;58:213–220. doi: 10.1176/ps.2007.58.2.213. [DOI] [PubMed] [Google Scholar]
- 7.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 8.Wang PS, Aguilar-Gaxiola S, Alonso J, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370:841–850. doi: 10.1016/S0140-6736(07)61414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Druss BG, Rosenheck RA. Use of practitioner-based complementary therapies by persons reporting mental conditions in the United States. Arch Gen Psyehiatry. 2000;57:708–714. doi: 10.1001/archpsyc.57.7.708. [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Soukup J, Davis RB, et al. The use of complementary and alternative therapies to treat anxiety and depression in the United States. Am J Psychiatry. 2001;158:289–294. doi: 10.1176/appi.ajp.158.2.289. [DOI] [PubMed] [Google Scholar]
- 11.Harvard Medical School. The world mental health survey initiative [Internet] Boston (MA): Harvard School of Medicine; 2004. Dec, [cited 2009 Sep 1]. Available from: http://www.hcp.med.harvard.edu/wmh. [Google Scholar]
- 12.Alonso J, Angermeyer MC, Bemert S, et al. Sampling and methods of the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psyehiatr Seand. 2004;109(Suppl 420):8–20. doi: 10.1111/j.1600-0047.2004.00326. [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psyehiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, et al. Coneordance of the Composite Intemational Diagnostic Interview version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psyehiatr Res. 2006;15:167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.StataCorp. Version 9.2 [statistical software) College Station (TX): StataCorp; 2005. STATA/SE. [Google Scholar]
- 16.Kovess-Masfety V, Dezetter A, de Graaf R, et al. Religious advisors’ role in mental health care in the European Study of the Epidemiology of Mental Disorders survey. Soc Psychiatry Psyehiatr Epidemiol. 2009 Oct 2; doi: 10.1007/s00127-009-0143-0. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 17.Fisher P, Ward A. Medicine in Europe: complementary medicine in Europe. BMJ. 1994;309:107–111. doi: 10.1136/bmj.309.6947.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Legal status of traditional medicine and complementary/alternative medieine: a worldwide review. Geneva (CH): WHO; 2001. [Google Scholar]
- 19.Bodeker G, Ong CK, Grundy C, et al. WHO global atlas of traditional, complementary and alternative medicine: text volume. Kobe (JP): World Health Organization Centre for Health Development; 2005. [Google Scholar]
- 20.Fumham A, Beard R. Health, just world beliefs and coping style preferences in patients of complementary and orthodox medicine. Soc Sei Med. 1995;40:1425–1432. doi: 10.1016/0277-9536(94)00263-s. [DOI] [PubMed] [Google Scholar]
- 21.Wang JL, Patten SB, Russell ML. Alternative medicine use by individuals with major depression. Can J Psychiatry. 2001;46:528–533. doi: 10.1177/070674370104600607. [DOI] [PubMed] [Google Scholar]
- 22.Unutzer J, Klap R, Sturm R, et al. Mental disorders and the use of alternative medicine: results from a national survey. Am J Psychiatry. 2000;157:1851–1857. doi: 10.1176/appi.ajp.157.11.1851. [DOI] [PubMed] [Google Scholar]
- 23.Parslow RA, Jorm AF. Use of prescription medications and complementary and alternative medicines to treat depressive and anxiety symptoms: results from a community sample. J Affeet Disord. 2004;82:77–84. doi: 10.1016/j.jad.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 24.Wang PS, Berglund PA, Kessler RC. Patterns and correlates of contacting clergy for mental disorders in the United States. Health Serv Res. 2003;38:647–673. doi: 10.1111/1475-6773.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang PS, Demler O, Olfson M, et al. Changing profiles of service sectors used for mental health care in the United States. Am J Psychiatry. 2006;163:1187–1198. doi: 10.1176/appi.ajp.163.7.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]