Abstract
Background
Variation in rates of breast reconstruction after mastectomy has raised concerns about the quality of decisions about reconstruction. We sought to evaluate patient decision making about reconstruction, using a validated measure of knowledge and preferences related to reconstruction.
Methods
A cross-sectional survey of early-stage breast cancer survivors from four university medical centers was conducted. The survey included measures of knowledge about specific reconstruction facts, personal goals and concerns, and involvement in decision making. A multivariable linear regression model of characteristics associated with knowledge and a logistic regression model of factors associated with having reconstruction were developed.
Results
84 patients participated (59% response rate). Participants answered 37.9% of knowledge questions correctly. Higher education (beta 15%, p=0.003) and having reconstruction (beta 21%, p<0.0001) were associated with higher knowledge. The goals “use your own tissue to make a breast” (OR 1.53, 95% CI 1.15, 2.05) and “wake up after mastectomy with reconstruction underway” (OR 1.66, 95% CI 1.30, 2.12) were associated with reconstruction. The goal “avoid putting foreign material in your body” was associated with no reconstruction (OR 0.64, 95% CI 0.48, 0.86). Most patients reported they mainly made the decision or made the decision with the doctor equally (93%, 95%CI 85-97%), and that their degree of involvement was about right (85%, 95%CI 75-91%).
Conclusion
Women treated with mastectomy in this study were not well-informed about breast reconstruction. Treatments were associated with patients' goals and concerns, however, and patients were highly involved in their decisions. Knowledge deficits suggest that breast cancer patients would benefit from interventions to support their decision making.
Introduction
Rates of breast reconstruction and geographic variation in rates of reconstruction,1, 2 have raised concerns about the quality of decisions that determine who gets breast reconstruction.3 Decisions about breast reconstruction are sensitive to the preferences of the patient because the right choice depends primarily upon the patient's personal preferences, rather than medical characteristics.4 For preference sensitive decisions, a growing international consensus defines decision quality as the extent to which the treatment choice reflects the preferences of an informed patient.5 Thus, a high-quality decision about breast reconstruction requires that patients: (1) have knowledge about reconstruction, including its risks and benefits, (2) receive treatment that is consistent with their preferences and goals, and (3) are involved in making decisions about their care.
Little is known about patients' specific knowledge about reconstruction or the degree to which their treatments reflect their preferences. Up to twenty percent of breast cancer survivors have reported they were never told about reconstruction,6, 7 and ethnic minority women appear to be least informed about reconstruction.8 Patients who have had reconstruction have expressed regret about having it and the feeling that their goals were not met.9 A significant shortcoming of prior studies is the lack of validated instruments to measure these aspects of the decision making process.
The objective of this study was to evaluate decisions about breast reconstruction among women with early stage breast cancer, using a validated measure of decision quality. Specifically, we sought to measure women's knowledge about reconstruction and to evaluate the degree to which treatments reflected patients' goals and preferences. A secondary objective was to identify factors associated with knowledge and to describe the degree of patient involvement in decision making about reconstruction.
Methods
Study design
We conducted a cross-sectional survey of breast cancer survivors at four university medical centers. The survey was part of a larger study designed to validate decision quality survey instruments for breast reconstruction, breast cancer surgery, and adjuvant therapy. This paper reports on the subset of participants who responded to the reconstruction survey.
Patient population
Subjects included a sample of adult women who had been treated with mastectomy for early-stage invasive breast cancer (Stage I, II) at one of four institutions (Dana Farber Cancer Institute, Massachusetts General Hospital, University of California San Francisco, and University of North Carolina Chapel Hill) and who were between one and three years from treatment at the time of contact. Because we were interested in studying decision making, we attempted to include only patients who actually had a choice about mastectomy versus lumpectomy, reconstruction, and systemic therapy. Thus, women with ductal carcinoma in situ only or bilateral breast cancer, those who received neoadjuvant systemic therapy, and those undergoing treatment for a second primary were excluded.
Eligible participants were identified through each institution's cancer registry. We estimated the number of patients we needed to contact to fulfill sample size requirements and then identified a sample of consecutive patients meeting inclusion criteria. Purposive sampling was used in an attempt to achieve adequate representation in 4 key subgroups for the overall trial– age greater than 60, non-White race, mastectomy treatment, and study site.
Enrollment
A letter was mailed to each eligible participant's primary breast cancer provider, informing them of the intent to contact their patients and offering the opportunity to opt out any patient because of exclusion criteria or for other reasons. A modified Dillman survey method was then followed.10 Eligible participants were mailed a packet containing an introductory letter, the survey instrument, consent forms, an opt-out postcard, and a packet of breast cancer postal stamps worth approximately ten dollars. Follow-up phone calls were made to those who did not return the survey or opt-out card. A reminder packet with the survey and consent form was sent to non-responders. Another packet of stamps was mailed to women who completed the survey.
Measures
The survey instrument included questions about demographics, medical and treatment history, the Breast Reconstruction Decision Quality Instrument (DQI), the patient's preferred treatment, and how informed the patient felt. We also collected demographic, medical, and treatment data from each institution's cancer registry. When a patient's report conflicted with the registry on a medical or treatment issue (eg. stage of disease), we examined the medical record to resolve the issue.
Breast Reconstruction Decision Quality Instrument (DQI)
The DQI contains three sections.
Knowledge: 7 multiple choice items. In this sample, the knowledge items had good internal consistency (0.81 Cronbach's alpha), moderate short term retest reliability (0.57 intraclass correlation coefficient), and good discriminant validity.11
Goals and concerns: 13 items. Goals and concerns were rated on an importance scale from 0 (not at all important) to 10 (extremely important) for the decision about reconstruction. Respondents also selected their three most important goals/concerns.
Involvement in decision making: 8 multiple choice items covered the following four issues: a) was the patient offered a choice; b) were the pros of reconstruction discussed; c) were the cons of reconstruction discussed; and d) did the provider ask the patient what she wanted.
The DQI development process has been described before.12 It included evidence review, elicitation of key facts and goals from patients and providers, drafting of items, and cognitive testing of items.
Treatment preference
This single item asked, “Which option was your personal preference?” with responses “No breast reconstruction”, “Breast reconstruction with an implant”, “Breast reconstruction with a flap”, or “I'm not sure”.
Perception of being informed
This single item asked, “On a scale from 0 to 10, where 10 means extremely well informed and 0 means not informed at all, how informed did you feel about breast reconstruction options for breast cancer?”
Statistical analysis
Descriptive summary statistics, including means and standard deviation for continuous variables and frequencies for categorical variables, were calculated.
Knowledge
The percentage of knowledge questions answered correctly was calculated. An “I am not sure” response was scored as incorrect, and missing responses were imputed with 1/k, where k was the number of possible responses. A knowledge score was calculated for every respondent who completed at least 4 of the 7 items.
To identify characteristics associated with higher knowledge, two-sample t-tests were first used. For each patient characteristic, the sample was divided into two groups (e.g., white and non-white), and the mean knowledge score for each group was compared using a t-test. The final multivariable linear regression model included only those significant at p≤0.05 level.
Goals and concerns
Two-sample t-tests were used to compare the importance ratings for each of the goals, between those who had reconstruction and those who did not.
Predictors of treatment
We developed a multivariable logistic regression model to identify the independent predictors of having reconstruction. We examined demographic characteristics, medical factors, involvement, and goals in bivariate analyses. Due to sample size constraints, the final model only included the combination of three predictors with the highest likelihood score. The percentage of patients receiving treatment that was not concordant with their preference (ie, wanted reconstruction but did not have it, or wanted no reconstruction but did have it) was also calculated.
Results
Patient characteristics
The sample consisted of 84 women who had undergone mastectomy for treatment of early stage breast cancer between 2004 and 2007 (Table 1). The average age was 54.9 years (SD 10.6), 80% of respondents were white, 66% had a college degree, and 31% had Stage I disease. Participants were an average of 31 months from treatment at the time of the study. Sixty-one percent of respondents had undergone reconstruction – 21% with a flap (including patients who had a flap and implant at the same time) and 39% with an implant. In the larger study, the response rate was 59%, and providers opted out 26 of 780 (3%) potentially eligible patients for unspecified reasons. Responders were more likely to be white than non-responders (85.2% vs. 71%, chi-square p<0.0001).
Table 1. Demographic and treatment characteristics of study sample (N=84).
| All | Reconstruction | No reconstruction | |||
|---|---|---|---|---|---|
|
|
|
|
|||
| N % | Flap* N (%) | Implant N (%) | N (%) | ||
| All patients | 84** | 18 | 33 | 33 | |
| Age in years, mean (SD) | 54.9 (10.6) | 54.6 (8.8) | 51.5 (9.2) | 58.4 (11.8) | |
| Months since diagnosis, mean (SD) | 31.5 (10.1) | 33.9 (11.6) | 31.5 (9.2) | 30.1 (10.1) | |
| Race | |||||
| White | 67 (79.8) | 15 (83.3) | 28 (84.8) | 24 (72.7) | |
| Black | 6 (7.1) | 0 (0) | 2 (6.1) | 4 (12.1) | |
| Other | 11 (13.1) | 3 (16.7) | 3 (9.1) | 5 (15.2) | |
| Education | |||||
| High school or less | 10 (11.9) | 3 (16.7) | 2 (6.1) | 5 (15.2) | |
| Some College | 19 (22.6) | 2 (11.1) | 10 (30.3) | 7 (21.2) | |
| College Graduate | 55 (65.5) | 13 (72.2) | 21 (63.6) | 21 (63.6) | |
| Income | |||||
| less than $15,0000 | 4 (4.8) | 0 (0) | 1 (3.0) | 3 (9.1) | |
| $15,000 to $29,999 | 5 (6.0) | 2 (11.1) | 2 (6.1) | 1 (3.0) | |
| $30,000 to $59,999 | 17 (20.2) | 3 (16.7) | 2 (6.1) | 12 (36.4) | |
| $60,000 to $99,999 | 15 (17.9) | 5 (27.8) | 4 (12.1) | 6 (18.2) | |
| $100,000 or more | 37 (44.0) | 7 (38.9) | 21 (63.6) | 9 (27.3) | |
| Marital Status | |||||
| Partnered | 60 (71.4) | 14 (77.8) | 28 (84.8) | 18 (54.5) | |
| Single/divorced/widowed | 24 (28.6) | 4 (22.2) | 5 (15.2) | 15 (45.5) | |
| Breast cancer stage | |||||
| I | 26 (31.0) | 5 (27.8) | 10 (30.3) | 11 (33.3) | |
| II | 58 (69.0) | 13 (72.2) | 23 (69.7) | 22 (66.7) | |
| Reconstruction timing | 51 | ||||
| Immediate | 36 (70.6) | 12 (66.7) | 24 (72.7) | NA | |
| Delayed | 15 (29.4) | 6 (33.3) | 9 (27.3) | NA | |
| Radiation treatment | |||||
| None | 65 (77.4) | 14 (77.8) | 26 (78.8) | 25 (75.8) | |
| Had radiation | 19 (22.6) | 4 (22.2) | 7 (21.2) | 8 (24.2) | |
Includes patients who had a flap and implant at the same time.
Not all items add to 84 if data were missing.
NA = not applicable
Knowledge
Overall, participants answered 37.9% (SD=24.1) of the knowledge questions correctly (Table 2). 34% of participants were able to answer at least 50% of questions correctly. Knowledge was highest for questions about the definition of implant reconstruction and the relative recovery time from implants versus flaps. Knowledge was lowest for questions about the rate of complications after reconstruction and satisfaction after implants versus flaps.
Table 2.
Knowledge of specific reconstruction topics.
| Question and possible response (correct response in italics) | Number who chose this response N* (%) |
|---|---|
| In general, which women are more satisfied with their breast reconstruction? | |
| a. Women who have reconstruction at the time of the mastectomy | 23 (27.4) |
| b. Women who delay reconstruction | 1 (1.2) |
| c. They are both equally satisfied | 28 (33.3) |
| d. I am not sure | 30 (35.7) |
| After which type of breast reconstruction are women more satisfied with the look and feel of the reconstructed breast? | |
| a. Implants | 5 (6.0) |
| b. Flaps | 13 (15.5) |
| c. Both are about the same | 25 (29.8) |
| d. I am not sure | 38 (45.2) |
| Mark whether or not it is true for breast reconstruction with an implant. | |
| a. Uses fat and tissue from other parts of the body to make a breast.** | 11 (13.1) |
| Mark whether or not it is true for breast reconstruction with a flap. | |
| b. Usually requires more than one surgery.** | 24 (28.6) |
| Which breast reconstruction surgery is easier on the body, that is, heals faster? | |
| a. Implants are easier | 48 (57.1) |
| b. Flaps are easier | 2 (2.4) |
| c. Implants and flaps are equally easy | 2 (2.4) |
| d. I am not sure | 29 (34.5) |
| Out of every 100 women who have breast reconstruction, about how many will have a major complication, such as needing hospitalization or an unplanned procedure, within 2 years? | |
| a. Few than 25 | 46 (54.8) |
| b. 25-50 | 3 (3.6) |
| c. 50-75 | 1 (1.2) |
| d. More than 75 | 1 (1.2) |
| e. I am not sure | 31 (36.9) |
| How does breast reconstruction affect future screening for breast cancer? | |
| a. Makes it harder to find cancer | 16 (19.0) |
| b. Makes it easier to find cancer | 36 (42.9) |
| c. Has little or no effect on finding cancer | 30 (35.7) |
| d. I am not sure | 2 (2.4) |
|
| |
| Total | 37.9 |
Not all items add to 84 if responses were missing.
The original question tested 4 statements. 3 statements were deleted after survey validation. For this question, this table presents the number who answered correctly.
On multivariable analysis (Table 3), education and treatment were the only significant predictors of knowledge score. Higher education (regression coefficient 15%, p=0.003) and having reconstruction (regression coefficient 21%, p<0.0001) were associated with higher knowledge.Overall, participants perceived that they were well informed about breast reconstruction (mean 9.4 on scale 0 to 10). The perception of being informed was weakly correlated with actual knowledge (Pearson's correlation coefficient 0.28).
Table 3.
Univariate (two-sample t-test) and multivariable (linear regression) analyses of factors associated with knowledge.
| Characteristic | Mean | Univariate | Multivariable | |
|---|---|---|---|---|
| Knowledge (% correct) | p | Regression coefficient | p | |
| Age at diagnosis | 0.23 | |||
| <50 years | 41.7 | |||
| >=50 years | 35.2 | |||
| Race | 0.068 | |||
| White | 40.6 | |||
| Non-white | 27.7 | |||
| Marital status | 0.062 | |||
| Partnered | 41.1 | |||
| Single/divorced/widowed | 29.8 | |||
| Education | 0.01 | 0.0026 | ||
| <College graduate | 27.7 | |||
| >=College graduate | 43.2 | 14.99 | ||
| Yearly income | 0.002 | |||
| <$60,000 | 24.6 | |||
| >=$60,000 | 43.8 | |||
| Reconstruction treatment | <0.0001 | <0.0001 | ||
| No | 24.4 | |||
| Yes | 46.1 | 21.36 | ||
| Stage | 0.96 | |||
| I | 37.7 | |||
| II | 38.0 | |||
| Months since Diagnosis | 0.76 | |||
| <24 months | 36.4 | |||
| >=24 months | 38.4 | |||
| Radiation Treatment | 0.78 | |||
| No | 37.5 | |||
| Yes | 39.3 | |||
Goals and concerns
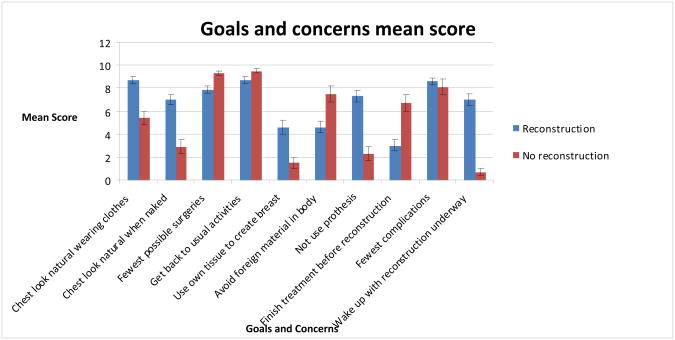
The majority of women felt it was very important to get back to their usual activities and have the fewest complications (mean 9.0 on scale 0 to 10) – whether or not they had had reconstruction (Figure 1). Women who had reconstruction also felt strongly about having a natural appearance in clothing (mean 8.7, SD 2.2) and not using a prosthesis (mean 7.3, SD 3.3). On the other hand, women who did not have reconstruction also felt strongly about having the fewest possible surgeries (mean 9.3, SD 1.4).
Figure 1.
Patient ratings of the importance of goals and concerns, on a scale from 0 (not important) to 10 (extremely important). The wording of the goals and concerns has been shortened to fit this graph. Error bars depict the standard error.
Involvement in decision making
Participants reported a substantial amount of involvement in decision making about reconstruction. The majority of women reported that they mainly made the final decision about reconstruction or made the decision with the doctor equally (93%, 95%CI 85-97%) and that their degree of involvement in decision making was about right (85%, 95%CI 75-91%). Many participants (69%, 95%CI 58-79%) reported that their providers discussed the pros of reconstruction, whereas a smaller minority (23%, 95%CI 14-33%) reported that their providers discussed the cons.
Predictors of reconstruction
We sought to identify which of the above variables (demographics, goals and concerns) were associated with having reconstruction (Table 4). On multivariable analysis, two goals were associated with having reconstruction: “use your own tissue to make a breast” (OR 1.53, 95% CI 1.15, 2.05) and “wake up after mastectomy with reconstruction underway” (OR 1.66, 95% CI 1.30, 2.12). The goal “avoid putting foreign material in your body” was associated with not having reconstruction (OR 0.64, 95% CI 0.48, 0.86).
Table 4.
Multivariable logistic regression model of factors associated with reconstruction.
| Characteristic | OR | 95% CI |
|---|---|---|
| Use your own tissue to make a breast | 1.53 | 1.15, 2.05 |
| Avoid foreign material in the body | 0.64 | 0.48, 0.86 |
| Wake up with reconstruction complete or underway | 1.66 | 1.30, 2.12 |
Three women (3.6%) received treatment that was not concordant with their stated preference about reconstruction. One person preferred to have reconstruction but did not have it and the other two preferred to have a flap but received an implant instead.
Discussion
Breast cancer survivors treated with mastectomy in this study showed low overall knowledge about breast reconstruction. Their decisions about reconstruction appeared to be associated more with personal goals and concerns, rather than demographic or medical characteristics, and reflected a high degree of patient involvement.
Knowledge
Our finding of low knowledge about breast reconstruction is consistent with previous findings. Given that our patient sample had a higher-than-average education level and rate of reconstruction, we believe that knowledge levels in breast cancer survivors in general may be lower than in this sample. A recent population-based study of 1,844 breast cancer survivors in Detroit and Los Angeles found that only 11% could correctly answer three questions about the number of operations for reconstruction, the effect of reconstruction on surveillance, and sensation after reconstruction.7
One might expect a patient to have lower knowledge about a specific issue if that issue were not a great concern for her, but our findings suggest otherwise. Participants were most concerned about getting back to usual activities and avoiding complications, but their knowledge about these areas was lacking − 39% of women could not correctly answer questions about recovery with implants versus flaps. Participants also expressed a high level of concern about avoiding complications, but nearly all (96%) participants could not correctly identify the approximate rate of complications from reconstruction.
One of the reasons for low knowledge about reconstruction may have been inadequate discussion by providers about reconstruction as an option. Twenty-six percent of our sample of women did not recall any provider mentioning reconstruction as an option for them, a finding consistent with other studies. The population-based study of breast cancer survivors in Detroit and Los Angeles found that 25% of women did not recall a discussion of reconstruction.7 In the National Comprehensive Cancer Network, 60% of women did not have a discussion about reconstruction documented in their record.13 In that study, younger, more educated women not having radiation were more likely to have had such a discussion. More recently, another population-based study of survivors in Los Angeles found that 19% reported no discussion of reconstruction with their provider.6 Lower-income women in that study were less likely to have discussed reconstruction with their provider.
Another possible explanation for the finding of low knowledge levels is poor recall of the informed consent discussion. Several studies have found that surgical patients forget much of the information they discuss with their surgeon,14, 15 even within hours of the discussion.16 In a study of patients undergoing breast reduction, patients recalled an average of 3 out of 12 facts about breast reduction, six days after the procedure.17 In our study, patients had undergone surgery an average of 2.4 years prior to contact.
We measured patients' knowledge of specific facts but not their ability to apply that knowledge to make good decisions about their care. Nonetheless, having a basic fund of knowledge about the treatment options is a necessary minimum for a high-quality treatment decision. The finding of relatively poor knowledge in this study raises concern about the quality of patients' decisions about reconstruction.
Patients felt highly informed about reconstruction, even though they had low levels of knowledge about it, a finding that is consistent with several other studies.18-20 Each of these studies has found that people's perceptions of their knowledge about a specific topic tend to be higher than their actual knowledge levels. This tendency to overestimate one's knowledge underscores the importance of knowledge measures that ask questions about specific facts, rather than asking only how informed a person feels. It also highlights the importance of surgeons providing detailed information about reconstruction, even to patients who believe they are adequately informed.
Goals and concerns
We suspect that breast cancer survivors may have more practical and realistic goals about reconstruction than their providers realize. Participants were most concerned, on average, about getting back to their usual activities and about having the fewest number of complications, regardless of whether or not they had reconstruction. Although women who had reconstruction expressed concern about appearance with or without clothing, they expressed equal or greater concern about return to usual activities, minimizing complications, and minimizing the number of surgeries. Other studies have found that patients who chose not to have breast reconstruction had substantial concerns about complications or about needing more surgery.21, 22
Breast surgeons and plastic surgeons ought to explicitly ask each patient how she feels about key goals and concerns, early in the surgical decision making process. Patients in this study who valued using their own tissue were more likely to have reconstruction, and patients who wanted to avoid foreign material in their body were less likely to have reconstruction. In another study that identified patients' goals of reconstruction, fear of surgery was associated with not having reconstruction, and concern about body image was associated with reconstruction.23 These findings affirm the importance of discussing specific goals and concerns, including types of breast reconstruction, early in the decision making process about whether or not to have reconstruction.
Are patients getting what they want?
We found that breast cancer patients' decisions about reconstruction were, in fact, associated with their personal goals, rather than personal characteristics such as age, race, or income. A few participants (4%), however, did not have the treatment they wanted. Although clinical factors (such as need for post-mastectomy radiation or severe co-morbidities) may have posed contraindications to reconstruction, we suspect that some patients are not aware of reconstruction as an option or are not explicitly asked for their preference. Breast cancer survivors have reported not being asked for their preferences about treatment in other studies,24 and breast cancer providers frequently cannot predict their patients' treatment preferences.25 Interestingly, all of the women in this study who reported a preference for no reconstruction did not have reconstruction, suggesting that breast reconstruction was not over-used.
Concordance between treatment and patients' preferences has been associated with better clinical outcomes among women deciding about breast cancer surgery (breast conservation versus mastectomy).26 Among women who are concerned about appearance, having breast conservation is associated with better postoperative mental health. By contrast, having mastectomy despite a preference for breast conservation is associated with poorer postoperative mental health and body image.
We are uncertain what women's informed preferences about breast reconstruction are at this point. If participants had been more fully informed about the facts about reconstruction, their preferences and goals about reconstruction might have been differently distributed. For example, women may have rated goals related to complications and recovery more highly, had they been fully informed. Similarly, some women who stated a preference for reconstruction may actually have preferred no reconstruction, had they been fully informed.
Limitations
Participants were an average of 2.4 years out from their decisions at the time of the study. Although knowledge was likely higher at the time of decision making, we believe substantial deficits in key areas did exist. In our current phase of investigation, we are measuring patient knowledge closer to the time of decision making. Participants' positive or negative experiences may also have affected their ratings for the goals and concerns. We are unsure of the direction of this possible bias in our results.
Although we found a trend toward women with higher knowledge being more likely to have had reconstruction, we cannot infer any causality between knowledge and treatment choice. Women who had reconstruction may have been more likely to seek information about reconstruction or to retain knowledge about it.
This sample came from a population of women treated at university cancer centers, and the rate of reconstruction (59%) was relatively high, compared to national averages of about 30-40%.1, 2 We believe that knowledge and concordance between treatment and preferences in this study may be higher than in the broader population of women undergoing mastectomy. The sample was also relatively well-educated and primarily White. Another study found that low-acculturated Latina women were less likely to undergo reconstruction despite having a relatively strong desire for it,8 suggesting that levels of preference concordance in our study may be higher than in the broader population of mastectomy patients.
Conclusion
Women treated with mastectomy for early stage breast cancer in this study were not well-informed about post-mastectomy breast reconstruction. Participants were most concerned about returning to usual activities and minimizing complications when deciding whether to have reconstruction. The decision about breast reconstruction is in fact associated with a patient's specific goals and concerns, rather than merely demographic or clinical characteristics. Patients making decisions about reconstruction would benefit from evidence-based decision support interventions, such as patient decision aids.
Acknowledgments
This study was supported by a grant from the Foundation for Informed Medical Decision Making.
Dr. Lee was supported by NIH/HCRR 1KL2RR025746
Footnotes
Financial Disclosure and Products: None of the authors have a conflict of interest.
References
- 1.Alderman AK, McMahon L, Jr, Wilkins EG. The national utilization of immediate and early delayed breast reconstruction and the effect of sociodemographic factors. Plastic & Reconstructive Surgery. 2003;111(2):695–703. doi: 10.1097/01.PRS.0000041438.50018.02. discussion 704-695. [DOI] [PubMed] [Google Scholar]
- 2.Joslyn SA. Patterns of care for immediate and early delayed breast reconstruction following mastectomy. Plast Reconstr Surg. 2005 Apr 15;115(5):1289–1296. doi: 10.1097/01.prs.0000156974.69184.5e. [DOI] [PubMed] [Google Scholar]
- 3.Are breast cancer patients being kept in the dark? http://www.plasticsurgery.org/Media/Press_Releases/Are_Breast_Cancer_Patients_Being_Kept_In_The_Dark/Are_Breast_Cancer_Patients_Being_Kept_In_The_Dark.html.
- 4.Wennberg J, Fisher E, Skinner J. Geography and the debate over Medicare reform. Health Affairs. 2002;(Web Exclusives):W94–114. doi: 10.1377/hlthaff.w2.96. [DOI] [PubMed] [Google Scholar]
- 5.Sepucha KR, Fowler FJ, Jr, Mulley AG., Jr Policy support for patient-centered care: the need for measurable improvements in decision quality. Health affairs (Project Hope) 2004;(Web Exclusive):VAR54–62. doi: 10.1377/hlthaff.var.54. [DOI] [PubMed] [Google Scholar]
- 6.Chen JY, Malin J, Ganz PA, et al. Variation in physician-patient discussion of breast reconstruction. J Gen Intern Med. 2009 Jan;24(1):99–104. doi: 10.1007/s11606-008-0855-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrow M, Mujahid M, Lantz PM, et al. Correlates of breast reconstruction: results from a population-based study. Cancer. 2005 Dec 1;104(11):2340–2346. doi: 10.1002/cncr.21444. [DOI] [PubMed] [Google Scholar]
- 8.Alderman AK, Hawley ST, Janz NK, et al. Racial and ethnic disparities in the use of postmastectomy breast reconstruction: results from a population- based study. J Clin Oncol. 2009 Nov 10;27(32):5325–5330. doi: 10.1200/JCO.2009.22.2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nissen MJ, Swenson KK, Kind EA. Quality of life after postmastectomy breast reconstruction. Oncol Nurs Forum. 2002 Apr;29(3):547–553. doi: 10.1188/02.ONF.547-553. [DOI] [PubMed] [Google Scholar]
- 10.Dillman D. Mail and Telephone Surveys: The Total Design Method. New York: John Wiley; 1978. [Google Scholar]
- 11.Sepucha K, Belkora J, Chang Y, et al. Decision quality: measuring knowledge for three breast cancer decisions Abstract J-3; Paper presented at: 31st Annual Meeting of the Society for Medical Decision Making; October 21, 2009; 2009. [Google Scholar]
- 12.Lee CN, Dominik R, Levin CA, Barry MJ, Cosenza C, O'Connor AM, Mulley AG, Sepucha K. Development of instruments to measure the quality of breast cancer treatment decisions. Health Expectations. :29. doi: 10.1111/j.1369-7625.2010.00600.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greenberg CC, Schneider EC, Lipsitz SR, et al. Do variations in provider discussions explain socioeconomic disparities in postmastectomy breast reconstruction? J Am Coll Surg. 2008 Apr;206(4):605–615. doi: 10.1016/j.jamcollsurg.2007.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Madan AK, Tichansky DS, Taddeucci RJ. Postoperative laparoscopic bariatric surgery patients do not remember potential complications. Obes Surg. 2007 Jul;17(7):885–888. doi: 10.1007/s11695-007-9164-5. [DOI] [PubMed] [Google Scholar]
- 15.Hutson MM, Blaha JD. Patients' recall of preoperative instruction for informed consent for an operation. J Bone Joint Surg Am. 1991 Feb;73(2):160–162. [PubMed] [Google Scholar]
- 16.Krupp W, Spanehl O, Laubach W, Seifert V. Informed consent in neurosurgery: patients' recall of preoperative discussion. Acta Neurochir (Wien) 2000;142(3):233–238. doi: 10.1007/s007010050030. discussion 238-239. [DOI] [PubMed] [Google Scholar]
- 17.Godwin Y. Do they listen? A review of information retained by patients following consent for reduction mammoplasty. Br J Plast Surg. 2000 Mar;53(2):121–125. doi: 10.1054/bjps.1999.3220. [DOI] [PubMed] [Google Scholar]
- 18.Crosby RA, Yarber WL. Perceived versus actual knowledge about correct condom use among U.S. adolescents: results from a national study. J Adolesc Health. 2001 May;28(5):415–420. doi: 10.1016/s1054-139x(00)00213-5. [DOI] [PubMed] [Google Scholar]
- 19.Cunningham AE, Perry KE, Stanovich KE, Stanovich PJ. Disciplinary knowledge of K-3 teachers and their knowledge calibration in the domain of early literacy. Ann Dyslexia. 2004 Jun;54(1):139–167. doi: 10.1007/s11881-004-0007-y. [DOI] [PubMed] [Google Scholar]
- 20.Ferguson E, Cox T, Irving K, Leiter M, Farnsworth B. A measure of knowledge and confidence in relation to HIV and AIDS: reliability and validity. AIDS Care. 1995;7(2):211–228. doi: 10.1080/09540129550126722. [DOI] [PubMed] [Google Scholar]
- 21.Handel N, Silverstein MJ, Waisman E, Waisman JR. Reasons why mastectomy patients do not have breast reconstruction. Plast Reconstr Surg. 1990 Dec;86(6):1118–1122. discussion 1123-1115. [PubMed] [Google Scholar]
- 22.Reaby LL. Reasons why women who have mastectomy decide to have or not to have breast reconstruction. Plast Reconstr Surg. 1998 Jun;101(7):1810–1818. doi: 10.1097/00006534-199806000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Ananian P, Houvenaeghel G, Protiere C, et al. Determinants of patients' choice of reconstruction with mastectomy for primary breast cancer. Ann Surg Oncol. 2004 Aug;11(8):762–771. doi: 10.1245/ASO.2004.11.027. [DOI] [PubMed] [Google Scholar]
- 24.Fallowfield L. Offering choice of surgical treatment to women with breast cancer. Patient Educ Couns. 1997 Mar;30(3):209–214. doi: 10.1016/s0738-3991(96)00947-0. [DOI] [PubMed] [Google Scholar]
- 25.Bruera E, Willey JS, Palmer JL, Rosales M. Treatment Decisions for Breast Carcinoma: Patient Preferences and Physician Perceptions. Cancer. 2002;94(7):2076–2080. doi: 10.1002/cncr.10393. [DOI] [PubMed] [Google Scholar]
- 26.Figueiredo MI, Cullen J, Hwang YT, Rowland JH, Mandelblatt JS. Breast cancer treatment in older women: does getting what you want improve your long-term body image and mental health? J Clin Oncol. 2004 Oct 1;22(19):4002–4009. doi: 10.1200/JCO.2004.07.030. [DOI] [PubMed] [Google Scholar]