Summary
A 22-year-old female student presented with a history of recurrent pancreatitis. The commonest causes of pancreatitis, including drugs, gallstones, corticosteroids, excess alcohol and hypertriglyceridaemia, were excluded. She was found to have an elevated serum calcium level that was considered to be the cause of her pancreatitis, with a detectable serum parathyroid hormone (PTH). An initial diagnosis of primary hyperparathyroidism was made. However, two neck explorations failed to reveal a parathyroid adenoma. She was referred to our unit three years later as her episodes of pancreatitis were becoming more frequent and her calcium level remained persistently elevated. Her investigations were as follows: elevated adjusted calcium level of 2.79 mmol/l (2.2–2.58), PTH level of 4.2 pmol/l (0.6–6.0), low 24 h urine calcium of 0.3 mmol/l and a urine calcium:creatinine ratio of <0.003. A clinical diagnosis of familial hypocalciuric hypercalcaemia (FHH) was made and confirmed on genetic testing that showed a c.1703 G>A mutation in the calcium-sensing receptor gene. Although the hypercalcaemia of FHH is usually without sequelae due to the generalised changes in calcium sensing, in the presence of this complication she was started on cinacalcet 30 mg daily. She had one further episode of pancreatitis with calcium levels ranging between 2.53 and 2.66 mmol/l. Her cinacalcet was gradually increased to 30 mg three times daily, maintaining her calcium levels in the range of 2.15–2.20 mmol/l. She has not had a further episode of pancreatitis for more than 2 years.
FHH is usually a benign condition with minimal complications from hypercalcaemia. Pancreatitis has been reported rarely, and no clear management strategy has been defined in these cases. Cinacalcet was successfully used in treating recurrent pancreatitis in a patient with FHH by maintaining calcium levels in the lower part of the reference range. Whether or not this is an effective long-term treatment remains yet to be seen.
Learning points
FHH is an important differential diagnosis for hypercalcaemia.
FHH can rarely cause pancreatitis.
No clear strategy is available to help in the management of patients with pancreatitis due to FHH.
Cinacalcet was effective in lowering serum calcium levels and reducing the frequency of pancreatitis in our patient with FHH.
Background
This case highlights the management of a rare complication of a condition, which is usually benign.
Case presentation
In 2007, a 22-year-old female university student, presented to a local hospital with severe epigastric pain and vomiting. As her amylase level was significantly elevated, she was diagnosed with acute pancreatitis. She was managed conservatively with analgesia and i.v. fluids and made an uneventful recovery. The commonest causes of pancreatitis including drugs, gallstones, corticosteroids, excess alcohol and hypertriglyceridaemia were excluded. However, she was noted to have an elevated calcium level, which was thought to be the cause of her pancreatitis. As her parathyroid hormone (PTH) level was detectable, an initial diagnosis of primary hyperparathyroidism was made. She subsequently underwent two neck explorations, which failed to reveal a parathyroid adenoma. She also had detailed imaging of her pancreas including a magnetic resonance pancreatography, that ruled out any anatomical causes of pancreatitis.
She continued to have recurrent episodes of pancreatitis requiring admission to hospital. In 2010, the episodes of pancreatitis were becoming more frequent, limiting her activities and education. Her serum calcium levels remained persistently elevated, and she was referred to our centre for a second opinion.
Investigation
Her investigations performed at our institution were as follows: elevated adjusted serum calcium level of 2.79 mmol/l (reference range, 2.2–2.58), PTH level of 4.2 pmol/l (0.6–6.0), low 24 h urine calcium of 0.3 mmol/l and a urine calcium:creatinine ratio of <0.03. A clinical and biochemical diagnosis of familial hypocalciuric hypercalcaemia (FHH) was made. Genetic testing confirmed the diagnosis and showed a G to A (c.1703G>A) nucleotide substitution in exon 6 of calcium-sensing receptor (CASR).
Treatment
She was initially started on 30 mg of cinacalcet daily. Although her calcium levels improved (2.53–2.66 mmol/l) and her frequency of pancreatitis significantly reduced, she was not free from attacks. Her dose of cinacalcet was subsequently increased to 30 mg twice daily and her corresponding calcium levels dropped further to 2.24 mmol/l. After 8 months of being symptom free on the latter dose, she had a further episode of pancreatitis. At this point, her cinacalcet dose was increased to 30 mg three times daily, aiming for a serum calcium level at the lower end of the reference range.
Outcome and follow-up
The cinacalcet was well tolerated throughout. Figure 1 shows a decrease in the frequency of her pancreatitis attacks as her serum calcium levels dropped with an increase in cinacalcet dose. She has not had an episode of pancreatitis for more than 2 years and her latest calcium levels remain at 2.10 mmol/l. She is being followed up annually with a repeat serum calcium level as well as 24 h urine calcium level before analysis in the clinic.
Figure 1.
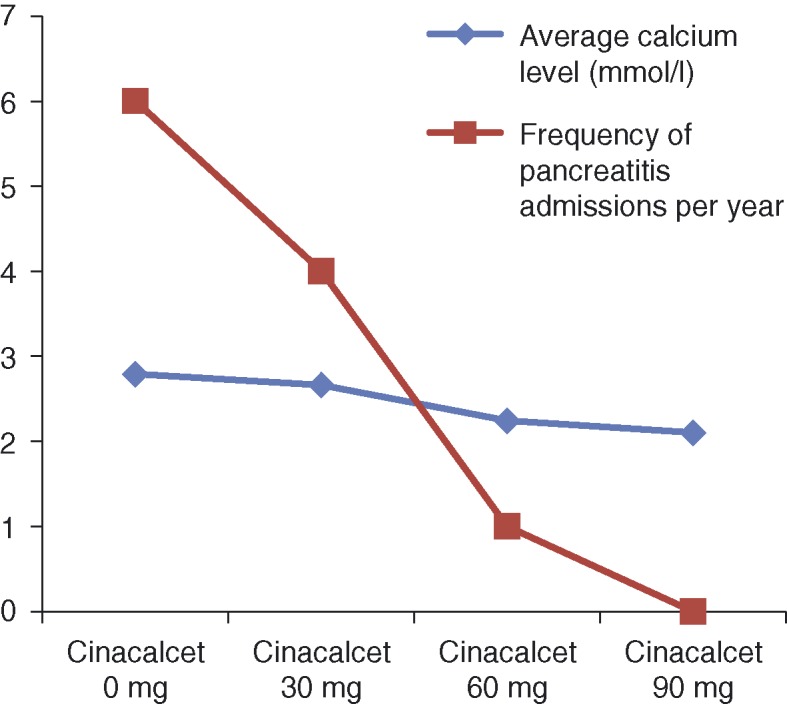
Reduction in the frequency of pancreatitis attacks with a drop in serum calcium level.
Discussion
FHH is usually a benign inherited condition, which is usually associated with minimal sequelae from hypercalcaemia. Pancreatitis has been reported rarely (1) (2). Other complications include chondrocalcinosis, gallstones and osteoporosis (3). It is well established that FHH is caused by inactivating mutations in the CASR gene, which reduce sensitivity to extracellular calcium. However, the mechanism of pancreatitis in this condition is poorly understood. Although the link between FHH and pancreatitis had previously been questioned (4), more recent papers have associated it with variant mutations of the CASR (1) possibly due to a combination of CASR mutation and a coexisting SPINK1 mutation, which predisposes to chronic pancreatitis (5). Theoretically, improving the sensitivity of mutant CASR to extracellular calcium would improve calcium homoeostasis and may offer effective treatment for patients with symptomatic FHH.
Calcimimetic agents such as cinacalcet are allosteric activators of CASR, which lower its activation threshold to extracellular calcium (6). Although commonly used in the management of secondary hyperparathyroidism, inoperable parathyroid adenomas and carcinomas (6), it has also been a successful treatment for patients with symptomatic FHH (3) (7). Mutations of the CASR in FHH also have various degrees of responsiveness to calcimimetics (8). Therefore, the response to cinacalcet and the dose required are likely to be unpredictable.
Whether or not cinacalcet can be used as a long-term therapy in these patients remains yet to be determined. One long-term case series (9) in which patients with FHH were treated with cinacalcet for up to 3 years showed that not only was it well tolerated but there was also a sustained improvement in serum calcium levels as well as PTH levels.
Our patient responded well to a moderate dose of cinacalcet. This case highlights the effective use of cinacalcet and the potential strategy in managing FHH patients presenting with recurrent pancreatitis. It also draws attention to getting the right diagnosis in order to avoid unnecessary surgical intervention in these patients.
Patient consent
Written informed consent was obtained from the patient for publication.
Author contribution statement
Dr M Druce is the patient's main physician and is a co-author.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- 1.Pearce SH, Wooding C, Davies M, Tollefsen SE, Whyte MD & Thakker RV. 1996Calcium sensing receptor mutations I familial hypocalciuric hypercalcaemia with recurrent pancreatitis. Clinical Endocrinology. 20: 675–680 10.1046/j.1365-2265.1996.750891.x [DOI] [PubMed] [Google Scholar]
- 2.Davies M, Klimiuk PS, Adams PH, Lumb GA, Large DM & Anderson DC. 1981Familial hypocalciuric hypercalcaemia and acute pancreatitis. BMJ. 282: 1023–1025 10.1136/bmj.282.6269.1023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Timmers HJ, Karperien M, Hamdy NA, De Boer H & Hermus AR. 2006Normalization of serum calcium by cinalcalcet in a patient with hypercalcaemia due to a de novo inactivating mutation of the calcium-sensing receptor. Journal of Internal Medicine. 260: 177–182 10.1111/j.1365-2796.2006.01684.x [DOI] [PubMed] [Google Scholar]
- 4.Stuckey BGA, Kent GN, Gutterirge DH & Reed WD. 1990Familial hypocalciuric hypercalcaemia and pancreatitis: no causal link proven. Australia and New Zealand Journal of Medicine. 20: 718–719 10.1111/j.1445-5994.1990.tb00407.x [DOI] [PubMed] [Google Scholar]
- 5.Felderbauer P, Hoffman P, Einwachter H, Bulut K, Ansorge N, Schmitz F & Schmidt WE. 2003A novel mutation of the calcium sensing receptor gene is associated with chronic pancreatitis in a family with heterozygous SPINK1 mutations. BMC Gastroenterology. 3: 34. 10.1186/1471-230X-3-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown ED. 2010Clinical utility of calcimimetics targeting the extracellular calcium-sensing receptor (caSR). Biochemical Pharmacology. 80: 297–307 10.1016/j.bcp.2010.04.002 [DOI] [PubMed] [Google Scholar]
- 7.Festen-Spanjer B, Haring CM, Koster JB & Mudde AH. 2007Correction of hypercalcaemia by cinacalcet I familial hypocalciuric hypercalcaemia. Clinical Endocrinology. 68: 321–325 10.1111/j.1365-2265.2007.03027.x [DOI] [PubMed] [Google Scholar]
- 8.Rus R, Haag C, Bumke-Vogt C, Bahr V, Mayr B, Mohlig M, Schulze E, Frank-Raue K, Raue F & Schofl C. 2008Novel inactivating mutations of the calcium-sensing receptor: The calcimimetic NPS R-568 improves signal transduction of mutant receptors. Journal of Clinical Endocrinology and Metabolism. 93: 4797–4803 10.1210/jc.2008-1076 [DOI] [PubMed] [Google Scholar]
- 9.Rasmussen AQ, Jorgensen NR & Schwartz P. 2011Clinical and biochemical outcomes of cinacalcet treatment of familial hypocalciuric hypercalcaemia: a case series. Journal of Medical Case Reports. 5: 564. 10.1186/1752-1947-5-564 [DOI] [PMC free article] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a