Abstract
Traumatic rupture of the diaphragm (TDR) presents diagnostic difficulty, with basic radiological investigations discovering less than half of all cases. As a consequence, complications of diaphragmatic rupture may present long after the initial injury has occurred—the time delay obscuring diagnosis. Once discovered repair is necessary with previous reports advocating open repair. Here, we report a case of traumatic diaphragmatic rupture causing small bowel obstruction 20 years after initial injury. The patient, a young woman, underwent successful laparoscopic assisted diaphragmatic repair with small bowel resection. TDR is an unusual but important differential diagnosis of an acute abdomen. A high index of suspicion is required to avoid delayed diagnosis and increased mortality.
INTRODUCTION
TDR remains a diagnostic challenge for radiologists and surgeons. No longer an uncommon occurrence, its incidence has steadily increased with the rising number of blunt traumas secondary to road-traffic accidents [1]. Presentation can be acute or delayed. Delayed presentation is associated with high mortality of up to 25% [2].
Here, we report a case of traumatic diaphragmatic rupture causing small bowel obstruction 20 years after initial injury. The patient, a middle-aged woman, underwent successful laparoscopic assisted diaphragmatic repair with small bowel resection.
This case illustrates the importance of vigilance when confronted with abdominal pain and a past history of significant blunt abdominal trauma. Finally, the case demonstrates the ability to manage these cases laparoscopically, which has not previously been reported.
CASE REPORT
A 40-year-old woman was referred by her GP. She reported 2 days of absolute constipation and mild abdominal distension. The night prior to admission she had been awoken from sleep with severe pleuritic pain and dyspnoea. Her medical history was unremarkable except for a road-traffic accident (RTA) 20 years previously.
On examination she was anxious and slightly short of breath. She had a regular tachycardia of 100 and her BP was 124/70. Auscultation of the chest revealed crepitation's at the right base and marked epigastric tenderness on examination of the abdomen. Her calves were soft and not tender. An electrocardiogram revealed a sinus tachycardia and a CXR revealed right-sided basal shadowing.
Relevant blood tests were as follows: Hb 15 g/dl, WCC 14.9 × 109/l, CRP 63 mg/l, amylase 40 U/l. Arterial blood gases on 28% oxygen pH 7.39, pO2 16.9 kPa, pCO2 4.5 kPa, HCO3− 21.5 mmol/l, Lactate 2.6 mmol/l, BE −3.7 mmol/l. In the light of her pleuritic pain a d-dimer was performed which was raised at 564 ng/ml.
In light of her clinical presentation she was suspected of having suffered a pulmonary embolism. A CTPA was performed which revealed a large defect in the right hemi diaphragm and small bowel in the thorax with evidence of small bowel obstruction (see Fig. 1).
Figure 1:
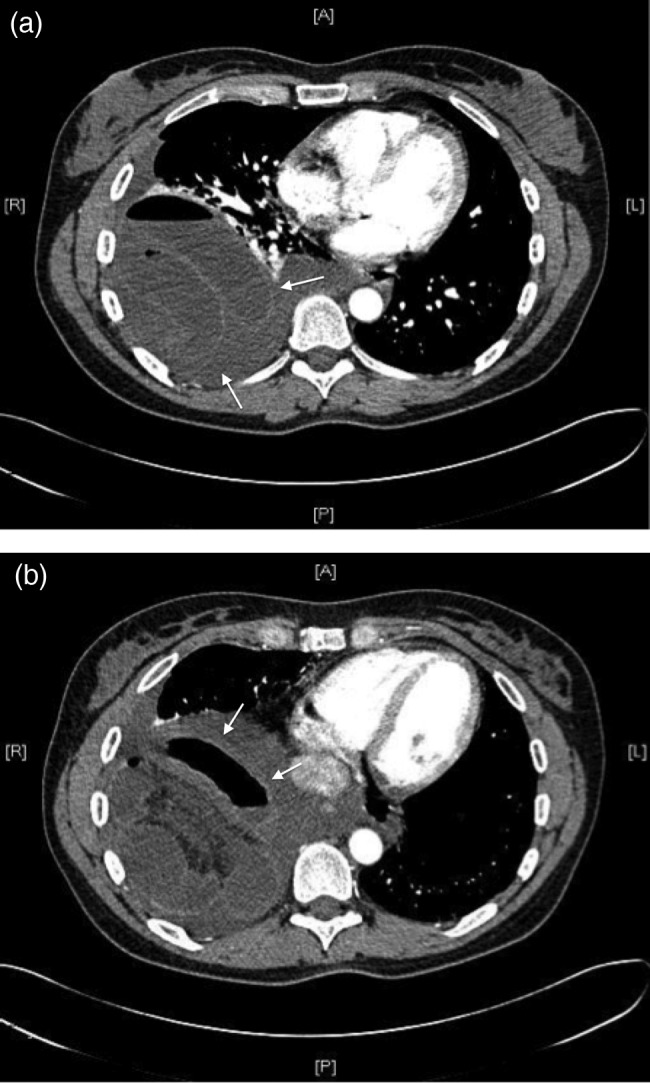
(a) and (b) Large right-sided diaphragmatic hernia with obstructed bowel (white arrows) evident on CTPA.
Her previous RTA had been a 40 by 40 m.p.h. head-to-head collision on a country lane. She had hit the steering wheel hard and her foot had become stuck in the foot well. When examined in hospital she had suffered a broken wrist, four broken ribs on the left and a laceration to the liver which was managed conservatively. She had left hospital after 1 week.
After an initial resuscitation she underwent laparoscopic repair of a diaphragmatic hernia and resection of strangulated jejunum. At laparoscopy, there was a large 5 × 5 cm defect noted posterolaterally on the right hemidiaphragm. To reduce the herniated small bowel, the defect first had to be enlarged with diathermy. Careful bowel handling was necessary to avoid bowel perforation and prevent pleural and peritoneal contamination. The defect was then primarily closed with 0 PDS continuous suture, the small bowel resection was then performed through a protected mini-laparotomy (see Fig. 2).
Figure 2:
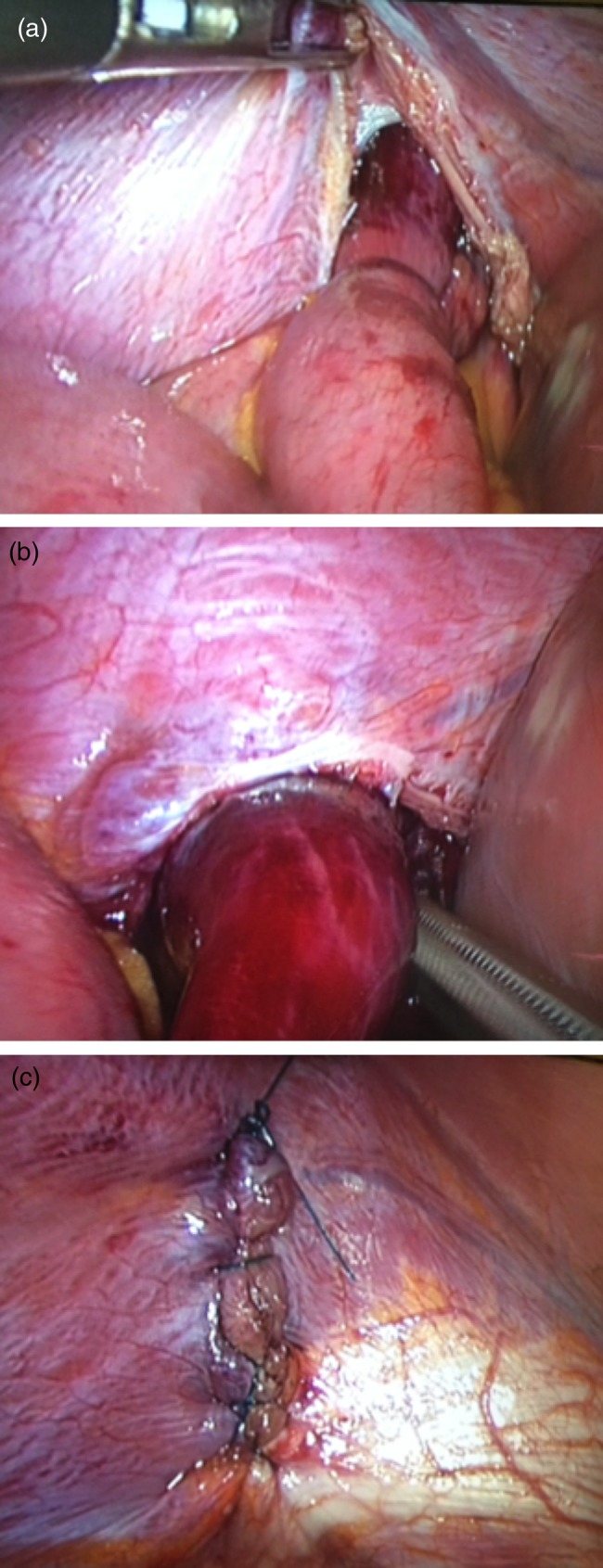
Laparoscopic images of diaphragmatic hernia repair. Images demonstrate (a) right hemidiaphragmatic defect containing a loop of small bowel the distal end of which is ischaemic, (b) extraction of the bowel loop from the diaphragmatic defect and (c) laparoscopic repair of the defect with 0 PDS.
DISCUSSION
Blunt trauma is responsible for the majority of TDRs. However, the incidence is low, occurring in only 0.8–1.6% of blunt injury trauma [1]. This incidence may be higher as the diagnosis is often missed. Left-sided rupture is more common than right, but there is an increasing frequency of right-sided ruptures. This may reflect an increased survival of patients with severe trauma in who right-sided TDR is more common [3].
Clinical presentation can be divided into three phases: acute, latent and obstructive. The latter two phases being grouped as ‘delayed’ presentation [4]. Diagnosis in the acute phase is usually incidental. A high frequency of associated injuries (95–100% of cases) often distracts from the diaphragmatic injury [5]. If not recognized during the acute phase the patient may remain asymptomatic, suffer from chronic abdominal pain or breathing difficulties or present in crisis with signs of obstruction and strangulation. The majority of cases of strangulation occur within 3 years of the initial trauma [6].
Chest radiography is the primary imaging modality with a sensitivity of 27–56% for left sided, but only 17% for right-sided injuries [7]. The most specific radiographic sign is an air containing viscus in the thorax, with focal constriction of the viscus at the site of herniation (‘collar sign’). Findings suggestive of rupture include elevation of a hemidiaphragm, compression atelectasis of the lower lobe, and irregularity of the diaphragmatic outline [7]. Helical CT scanning is a more valuable tool with a sensitivity of 70% for left-sided, 50% for right-sided injuries and a specificity of 100%. While not appropriate in the acute setting, MRI allows for optimum visualization of the hemidiaphragm [8].
The parietoperitoneal pressure gradient results in a tendency for enlargement of the defect and herniation of abdominal viscera. Early surgical repair is therefore appropriate with the surgical approach often dictated by associated injuries. In the delayed presentation, surgical intervention is complicated by adhesions between abdominal viscera and thoracic organs, with authors therefore recommending a thoracotomy [9]. Authors have also reported difficulties in attempting a laparoscopic approach including difficulty retracting the liver and establishing a pneumoperitoneum [10].
CONCLUSIONS
TDR is increasing in incidence and although usually associated with major blunt trauma can occur after much smaller injuries. The diagnosis of a ruptured diaphragm is frequently missed during the acute phase with a high mortality during delayed presentations. A high index of suspicion is required and the diagnosis should always be considered in those with a history of blunt abdominal or chest trauma who develop gastrointestinal symptoms. Chest radiography is a useful tool with CT gaining increasing recognition as the primary diagnostic investigation. Vigilance should be especially acute for right-sided injuries which remain underdiagnosed. Early surgical intervention is recommended which as this case has demonstrated can be performed via a laparoscopic approach thereby aiding post-operative recovery.
REFERENCES
- 1.Shah R, Sabanathan S, Mearns AJ, Chodhury AK. Traumatic rupture of diaphragm. Ann Thorac Surg. 1995;60:1444–9. doi: 10.1016/0003-4975(95)00629-Y. [DOI] [PubMed] [Google Scholar]
- 2.Degiannis E, Levy RD, Sofianos C, Potokar T, Florizoone MGC, Saadia R. Diaphragmatic herniation after penetrating trauma. BJS. 1996;83:88–91. doi: 10.1002/bjs.1800830128. [DOI] [PubMed] [Google Scholar]
- 3.Goh BK, Wong AS, Tay KH, Hoe MN. Delayed presentation of a patient with a ruptured diaphragm complicated by gastric incarceration and perforation after apparently minor blunt trauma. CJEM. 2004;6:277–80. doi: 10.1017/s148180350000926x. [DOI] [PubMed] [Google Scholar]
- 4.Strug B, Noon GP, Beall AC. Traumatic diaphragmatic hernia. Ann Thorac Surg. 1974;17:444. doi: 10.1016/s0003-4975(10)65678-0. [DOI] [PubMed] [Google Scholar]
- 5.Hill LD. Injuries of the diaphragm following blunt trauma. Surg Clin N Am. 1972;52:611–24. doi: 10.1016/s0039-6109(16)39736-5. [DOI] [PubMed] [Google Scholar]
- 6.McCune RP, Roda CP, Eckert C. Rupture of the diaphragm caused by blunt trauma. J Trauma. 1976;16:531–7. doi: 10.1097/00005373-197607000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Shanmuganathan K, Mirvis SE. Imaging diagnosis of nonaortic thoracic injury. Radiol Clin North Am. 1999;37:533–51. doi: 10.1016/s0033-8389(05)70110-x. [DOI] [PubMed] [Google Scholar]
- 8.Lochum S, Ludig T, Walter F, Sebbag H, Grosdidier G, Blum AG. Imaging of diaphragmatic injury: a diagnostic challenge? Radiographics. 2002;22:S103–16. doi: 10.1148/radiographics.22.suppl_1.g02oc14s103. [DOI] [PubMed] [Google Scholar]
- 9.Laws HL, Hawkins ML. Diaphragmatic injury. Adv Trauma. 1987;2:207–28. [Google Scholar]
- 10.Lindsey I, Woods SD, Nottle PD. Laparoscopic management of blunt diaphragmatic injury. Aust N Z J Surg. 1997;67:619–21. doi: 10.1111/j.1445-2197.1997.tb04609.x. [DOI] [PubMed] [Google Scholar]


