Abstract
Introduction
Organized stroke systems of care include preferential emergency medical services (EMS) routing to deliver suspected stroke patients to designated hospitals. To characterize the growth and implementation of EMS routing of stroke nationwide, we describe the proportion of stroke hospitalizations in the United States (U.S.) occurring within regions having adopted these protocols.
Methods
We collected data on ischemic stroke using International Classification of Diseases-9 (ICD-9) coding from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (NIS) database from the years 2000–2010. The NIS contains all discharge data from 1,051 hospitals located in 45 states, approximating a 20% stratified sample. We obtained data on EMS systems of care from a review of archives, reports, and interviews with state emergency medical services (EMS) officials. A county or state was considered to be in transition if the protocol was adopted in the calendar year, with establishment in the year following transition.
Results
Nationwide, stroke hospitalizations remained constant over the course of the study period: 583,000 in 2000 and 573,000 in 2010. From 2000–2003 there were no states or counties participating in the NIS with EMS systems of care. The proportion of U.S. stroke hospitalizations occurring in jurisdictions with established EMS regional systems of acute stroke care increased steadily from 2004 to 2010 (1%, 13%, 28%, 30%, 30%, 34%, 49%). In 2010, 278,538 stroke hospitalizations, 49% of all U.S. stroke hospitalizations, occurred in areas with established EMS routing, with an additional 18,979 (3%) patients in regions undergoing a transition to EMS routing.
Conclusion
In 2010, a majority of stroke patients in the U.S. were hospitalized in states with established or transitioning to organized stroke systems of care. This milestone coverage of half the U.S. population is a major advance in systematic stroke care and emphasizes the need for novel approaches to further extend access to stroke center care to all patients.
INTRODUCTION
Stroke is the fourth leading cause of mortality and a leading cause of morbidity in the United States (U.S.).1 Early evaluation and treatment is vital to improving outcomes because during an acute stroke, approximately 2 million neurons die every minute.2 Delays in seeking medical care lead to underutilization of intravenous thrombolysis.3 The Brain Attack Coalition (BAC), a collaboration of physicians, scientists, and government leaders, established guidelines for organized systems of stroke care including primary stroke center (PSC) certification and preferential emergency medical services (EMS) routing of suspected stroke patients to designated PSCs. Hospitals must meet specific standards for stroke care for certification by the Joint Commission as a PSC. Standards are set for elements pertinent to comprehensive stroke care including, acute stroke teams, neurosurgery, neuroimaging, laboratory services, and emergency medical systems.4
Since the publication of the BAC’s initial recommendations, the Joint Commission in collaboration with the American Stroke Association (ASA) has certified over 925 PSCs nationally. An updated version of the BAC recommendations addressed EMS response to patients showing signs of acute stroke, recommending that EMS personnel should transport patients with acute stroke to primary stroke centers, unless there is another imminent life-threatening condition (level of evidence class I, level B).4,5 This updated classification highlights the importance of rapid identification and transport of stroke patients who seek immediate medical treatment.
There is no national requirement for adoption of EMS preferential routing protocols for stroke. Adoption of routing has been on an individual state or county level. We wanted to describe the rate and the effectiveness in nationwide adoption of stroke-routing protocols by looking at individual stroke hospitalization by location over a time period from 2000–2010. Stroke hospitalizations in states having adopted organized stroke systems of care were compared to those without such protocols for each period of study to determine the rate and extent of state adoption in the U.S.
METHODS
Data Sources
The Nationwide Inpatient Sample (NIS) is the largest publicly available inpatient care database representing 20% of admissions to hospitals across the U.S.6 Data on ischemic stroke using the ninth revision of the International Classification of Diseases (ICD-9) coding (433.01, 433.11, 433.21, 433.31, 433.91, 434.01, 434.11, and 434.91) were collected using patient discharge information from the NIS, Healthcare Cost and Utilization Project (HCUP), and the Agency for Healthcare Research and Quality during the years 2000–2010. The NIS contains data on primary and secondary patient diagnoses, patient demographics (i.e. age, gender, and race), and hospital characteristics, such as size, teaching status, and zip code. We collected the NIS patient and hospital data on 28 states from the year 2000, and on 1,051 hospitals located in 45 states in 2010; this approximates a 20%-stratified sample of U.S. community hospitals. We analyzed EMS transportation systems only for states in the NIS database from 2000–2010. States not in the NIS database as of 2010 include Alabama, Delaware, Idaho, North Dakota, and New Hampshire; they are indicated in black (Figure). Given the increase in the number of states and thus in the number of hospitals covered in the database over the study period, the NIS team specified a sample and weight strategy required for hospitals and number of discharges. We calculated hospital weights based on stratification of hospital type; hospital strata were categorized on geographic location (Northeast, West, Midwest and South), urban or rural region, teaching status, size ((small (<200 beds), medium (201–400 beds), large (>400 beds)), and control (public, voluntary, or proprietary hospital). We compared these hospital subtypes to the national number obtained from the American Hospital Association (AHA) Annual Survey Database in order to extrapolate the NIS sample hospitals to the nationwide hospitals. The number of community hospitals within each stratum in the nationwide hospitals was added to obtain the national hospital weight. Similarly, we developed discharge weights to extrapolate the NIS sample discharges to the nationwide discharge. We obtained the number of discharges on the national level from the AHA.
Figure.
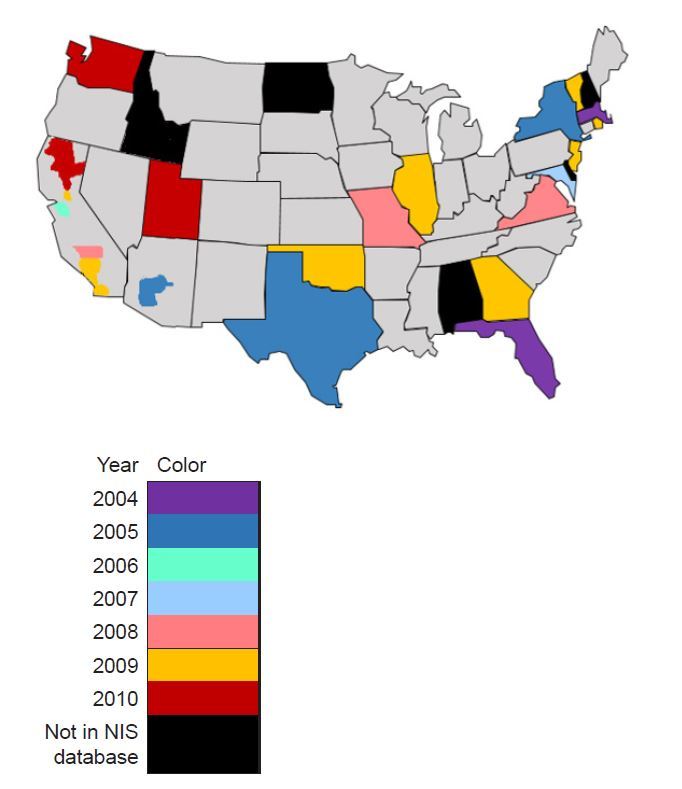
Map of the United States describing year of adoption of state organized stroke systems of care from 2004 to 2010.
NIS, National Impatient Sample
We obtained data on EMS systems of care from a study that reviewed online legislative archives and reports, and interviewed public health or EMS officials from all 50 states at the county-level, and employees at the American Health Association, American Stroke Association and the Centers for Disease Control.7 NIS hospital data is not reported at the county level in the state of Texas. We analyzed all Texas data using the state-reported EMS stroke diversion policy in 2005, even though Harris County began EMS routing in 2000.
Data Analysis
We conducted analyses using Statistical Analysis System (SAS) version 9.2 software. Cases were patients from the NIS discharge database with diagnosed ischemic stroke, identified by a review of ICD-9 discharge diagnoses. Based on the NIS hospital identification number, which denotes the patients’ hospital zip code, the hospital was assigned as an area with or without EMS regional system of acute stroke care by study year (2000–2010). If the protocol for EMS to transport stroke patients to the nearest primary stroke center was initiated in a given year, then the area was said to be in a transition period for that same year to account for the delay of several months for actual implementation of stroke routing on the field. We compared the proportion of stroke patients in jurisdictions with EMS regional system of stroke care to the proportion of stroke patients in other jurisdictions for each year by comparing the frequency of patients in each jurisdiction. The frequency of total ischemic patient transportations for that year is the denominator for comparing the proportions.
RESULTS
Although Texas was the first state to begin routing EMS preferential routing of acute stroke patients to designated hospitals in 2000, due to the lack of county-based reporting we were not able to capture this data. Thus the first transition to EMS routing is 2003. By 2010, the NIS database included 14 states with complete and an additional 3 states with partial (county-specific) adoption of EMS routing protocols for transportation of acute stroke patients to designated stroke centers (Figure).
From 2000 through 2010, there were 6,072,735 unadjusted individual ischemic stroke hospitalizations reported in NIS database. The overall age-adjusted hospitalization rates for ischemic stroke during this period of time declined from 169 per 100,000 population in 2000, to 138 per 100,000 population in 2010. Of the total number of stroke hospitalizations reported to the NIS in the study period 22% were in areas that adhered to EMS regional systems of acute stroke care. The proportion and frequency of U.S. stroke hospitalizations in areas with routing protocols for stroke patients increased throughout the study period (Table 1). The states and counties adopting EMS stroke protocols increased from 2004 to 2010 (Figure). From 2004 to 2010 the rate of increase in the proportion of stroke hospitalizations in regions with EMS diversion was 12%.
Table 1.
National yearly estimates of hospitalization for ischemic stroke with state organized stroke systems of care.
| Frequency of stroke hospitalizations by regional EMS policy adoption | Percentage of total stroke hospitalization by EMS policy | ||||||
|---|---|---|---|---|---|---|---|
| Year | No EMS | EMS | EMS In-transit | Total | No EMS | EMS | EMS In-transit |
| 2000 | 582,954 | 0 | 0 | 582,954 | 100 | 0 | 0 |
| 2001 | 580,078 | 0 | 0 | 580,078 | 100 | 0 | 0 |
| 2002 | 569,887 | 0 | 0 | 569,887 | 100 | 0 | 0 |
| 2003 | 539,705 | 0 | 7938 | 547,643 | 98.55 | 0 | 1.45 |
| 2004 | 459,644 | 7372 | 65,215 | 532,232 | 86.36 | 1.39 | 12.25 |
| 2005 | 367,911 | 69,681 | 88,083 | 525,676 | 69.99 | 13.26 | 16.76 |
| 2006 | 382,256 | 146,074 | 1241 | 529,571 | 72.18 | 27.58 | 0.23 |
| 2007 | 351,403 | 156,695 | 12,227 | 520,326 | 67.54 | 30.11 | 2.35 |
| 2008 | 368,810 | 163,267 | 32,087 | 564,165 | 65.37 | 28.94 | 5.69 |
| 2009 | 264,436 | 187,681 | 95,525 | 547,643 | 48.29 | 34.27 | 17.44 |
| 2010 | 275,043 | 278,538 | 18,979 | 572,560 | 48.04 | 48.65 | 3.31 |
EMS, emergency medical services
DISCUSSION
Adoption of EMS preferential stroke-routing protocols steadily increased during the 2000 to 2010 study period. In 2010, a majority of stroke patients in the U.S. were hospitalized in states or counties with established or transitioning EMS stroke diversion policies, demonstrating progress towards nationwide coverage of stroke care. As the average age of the U.S. population increases, the frequency of stroke is predicted to rise as well,8 and the impact of EMS stroke routing policies is likely to increase. This paper highlights the great success in systematic implementation of the continuum stroke care for policies supporting EMS stroke routing, continued certification of primary stroke centers,9 and use of stroke therapies,10,11 including intravenous recombinant tissue plasminogen activator.12
EMS routing of stroke has followed the lead of similar systems for acute myocardial infarction and trauma. The process of routing patients to the appropriate hospital is complex and involves recognition of stroke symptoms by dispatch operators taking emergency calls. The right prehospital team with training in the use of a stroke recognition instrument has to be dispatched. Instruments commonly used by EMS personnel to identify potential stroke cases include the Los Angeles Prehospital Stroke Screen,13,14 and the Cincinnati prehospital stroke scale.15 Once a potential stroke case has been identified, the individual stroke diversion protocol will have criteria for activation, such as time from onset of symptoms to paramedic evaluation. As stroke diversion is likely to benefit individuals presenting within time periods of eligibility for intravenous thrombolysis, most EMS stroke diversion protocols will apply to individuals with onset less than 2 to 3 hours. There may be secondary considerations, such as patient stability and length of diversion, affecting eligibility. Prehospital notification of incoming acute stroke cases can help mobilize care teams and streamline care.16
We have documented a nationwide trend towards adoption of EMS routing protocols, which may be a mechanism of improving quality of stroke care. For hospitals to participate in these systems they would have to achieve some form of certification, such as local EMS approval or certification from the Joint Commission as a PSC. Adoption of the EMS routing protocols will drive greater EMS provider training in stroke recognition tools and dispatch operator training in stroke recognition.17 A preliminary study in California seems to indicate that EMS routing protocols may be a driver of hospital PSC designation. Once a hospital learns it will be bypassed with the new protocol, there is more incentive to be certified as a PSC to maintain business.18
Future directions of stroke systems of care include expanding systems of comprehensive stroke centers and considerations of t2-tier systems of stroke routing.19 Future directions of research should focus on analysis of patient-level data to understand the effect of adopting of EMS stroke-routing protocols on various stroke outcomes. This would include comparing rate of TPA use per stroke hospitalization and discharge outcomes in areas with and without EMS routing protocols. As greater proportions of acute stroke hospitalizations are occurring in states covered by EMS routing protocols, we can expect improvements in the overall quality of care and greater implementation of the entire spectrum of stroke systems of care, from patient recognition to EMS activation, dispatch, stroke recognition, transport, pre-notification, and ED/hospital treatment.
LIMITATIONS
There are limitations in this study. The category of “stroke” depends on accurate coding of ICD-9CM codes to properly capture pathology. Misidentification may lead to a systemic bias of certain codes in the cerebrovascular population. The legislation adopting EMS regional systems of stroke care was regulated on the state or county level. However, in this study we did not assess or investigate the actual implementation of this practice at the local EMS level; geographic areas implementing EMS stroke protocols includes areas that may not have primary stroke centers available. Another factor to consider is the transportation proportion, which includes patients that were transferred from one hospital to another and includes patients that insisted on a different hospital preference.
CONCLUSION
Over half of the U.S. stroke hospitalizations are in states supported by organized stroke systems of care, demonstrating the progress towards full coverage of stroke care. Extended access to comprehensive stroke care for all stroke patients in the U.S. is an achievable goal, if stroke organization leaders, national EMS and medical directors, and legislators continue to work towards a proficient and an effective stroke care system.
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- 1.Miniño AM, Heron MP, Smith BL. Deaths: Preliminary data for 2004. Natl Vital Stat Rep. 2006;54(19):1–49. [PubMed] [Google Scholar]
- 2.Saver JL. Time is brain--quantified. Stroke. 2006;37:263–266. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]
- 3.Howard VJ, Lackland DT, Lichtman JH, et al. Care seeking after stroke symptoms. Ann Neurol. 2008;63:466–472. doi: 10.1002/ana.21357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alberts MJ, Hademenos G, Latchaw RE, et al. Recommendations for the establishment of primary stroke centers. Brain Attack Coalition. JAMA. 2000;283(23):3102–3109. doi: 10.1001/jama.283.23.3102. [DOI] [PubMed] [Google Scholar]
- 5.Alberts MJ, Latchaw RE, Jagoda A, et al. Revised and updated recommendations for the establishment of primary stroke centers: A summary statement from the Brain Attack Coalition. Stroke. 2011;42:2651–2665. doi: 10.1161/STROKEAHA.111.615336. [DOI] [PubMed] [Google Scholar]
- 6.Pfuntner A, Wier LM, Elixhauser A. Overview of hospital stays in the united states, 2010: Statistical brief #144. [PubMed] [Google Scholar]
- 7.Song S, Saver J. Growth of regional acute stroke systems of care in the United States in the first decade of the 21st century. Stroke. 2012;43:1975–1978. doi: 10.1161/STROKEAHA.112.657809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: A policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 9.Diamond LC, Wilson-Stronks A, Jacobs EA. Do hospitals measure up to the national culturally and linguistically appropriate services standards? Med Care. 2010;48:1080–1087. doi: 10.1097/MLR.0b013e3181f380bc. [DOI] [PubMed] [Google Scholar]
- 10.Wojner AW, Morgenstern L, Alexandrov AV, et al. Paramedic and emergency department care of stroke: Baseline data from a citywide performance improvement study. Am J Crit Care. 2003;12:411–417. [PubMed] [Google Scholar]
- 11.Albers GW, Clark WM, Madden KP, et al. Atlantis trial: Results for patients treated within 3 hours of stroke onset. Alteplase thrombolysis for acute noninterventional therapy in ischemic stroke. Stroke. 2002;33:493–495. doi: 10.1161/hs0202.102599. [DOI] [PubMed] [Google Scholar]
- 12.Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early stroke treatment: Pooled analysis of atlantis, ecass, and ninds rt-pa stroke trials. Lancet. 2004;363:768–774. doi: 10.1016/S0140-6736(04)15692-4. [DOI] [PubMed] [Google Scholar]
- 13.Kidwell CS, Saver JL, Schubert GB, et al. Design and retrospective analysis of the Los Angeles Prehospital Stroke Screen (LAPSS) Prehosp Emerg Care. 1998;2:267–273. doi: 10.1080/10903129808958878. [DOI] [PubMed] [Google Scholar]
- 14.Kidwell CS, Starkman S, Eckstein M, et al. Identifying stroke in the field : Prospective validation of the Los Angeles Prehospital Stroke Screen (LAPSS) Stroke. 2000;31:71–76. doi: 10.1161/01.str.31.1.71. [DOI] [PubMed] [Google Scholar]
- 15.Kothari RU, Pancioli A, Liu T, et al. Cincinnati prehospital stroke scale: Reproducibility and validity. Ann Emerg Med. 1999;33:373–378. doi: 10.1016/s0196-0644(99)70299-4. [DOI] [PubMed] [Google Scholar]
- 16.Lin CB, Peterson ED, Smith EE, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2012;5:514–522. doi: 10.1161/CIRCOUTCOMES.112.965210. [DOI] [PubMed] [Google Scholar]
- 17.Kidwell CS, Saver JL, Schubert GB, et al. Design and retrospective analysis of the Los Angeles Prehospital Stroke Screen (LAPSS) Prehosp Emerg Care. 1998;2:267–273. doi: 10.1080/10903129808958878. [DOI] [PubMed] [Google Scholar]
- 18.Schuberg S, Song S, Saver JL, et al. Impact of emergency medical services stroke routing protocols on primary stroke center certification in California. Stroke. 2013;44(12):3584–3586. doi: 10.1161/STROKEAHA.113.000940. [DOI] [PubMed] [Google Scholar]
- 19.Alberts MJ, Latchaw RE, Selman WR, et al. Recommendations for comprehensive stroke centers. Stroke. 2005;36:1597–1616. doi: 10.1161/01.STR.0000170622.07210.b4. [DOI] [PubMed] [Google Scholar]


