Abstract
Objectives
Rehospitalizations for elderly patients are an increasing health care burden. Nonetheless, we have limited information on unplanned rehospitalizations and the related risk factors in elderly patients admitted to in-hospital rehabilitation facilities after an acute hospitalization.
Setting
In-hospital Rehabilitation and Aged Care Unit
Design
Retrospective cohort study
Participants
Elderly patients ≥65 years admitted to an in-hospital rehabilitation hospital after an acute hospitalization between January 2004 and June 2011.
Measurements
The rate of 30-day unplanned rehospitalization to hospitals was recorded. Risk factors for unplanned rehospitalization were evaluated at rehabilitation admission: age, comorbidity, serum albumin, number of drugs, decline in functional status, delirium, Mini Mental State Examination score, length of stay in the acute hospital. A multivariable Cox proportional regression model was used to identify the effect of the above-mentioned risk factors for time to event within the 30-day follow-up.
Results
Among 2,735 patients, with a median age of 80 years (Interquartile Range 74–85), 98 (4%) were rehospitalized within 30 days. Independent predictors of 30-day unplanned rehospitalization were the use of 7 or more drugs (Hazard Ratio [HR], 3.94; 95% Confidence Interval, 1.62–9.54; P=.002) and a significant decline in functional status (56 points or more at the Barthel Index) compared to the month prior to hospital admission (HR 2.67, 95% CI: 1.35–5.27; P=.005). Additionally, a length of stay in the acute hospital ≥13 days carried a 2 fold higher risk of rehospitalization (HR 2.67, 95% CI: 1.39–5.10); P=.003).
Conclusions
The rate of unplanned rehospitalization was low in this study. Polypharmacy, a significant worsening of functional status compared to the month prior to acute hospital admission and hospital length of stay are important risk factors.
Keywords: rehospitalization, elderly, in-hospital rehabilitation, risk factors
INTRODUCTION
Among high-income countries, older people (age 65 and older) make up a large (15%–20%) proportion of the population and many require hospitalization for aging related diseases.1 In the United States (US), almost one fifth (24.8%) of the government sponsored Medicare beneficiaries discharged from a hospital were hospitalized again within 30 days of their index admission.2,3 Rehospitalizations for elderly patients account for about $15 billion of Medicare expenses4 and an estimated £1.6 billion each year in the United Kingdom.5 A substantial number of older patients leaving the hospital receive Post Acute care (PAC) services in either Skilled Nursing Facilities (SNF) (38% of those who receive services after a hospitalization in the US) or in a hospital rehabilitation setting (9% of all patients in the US who receive services after a hospitalization).6 The rate of 30 day repeat hospitalizations range from 23.5 % in skilled nursing7 and 20% in the inpatient rehab settings.8 Despite these high rates of hospital readmission, there are very few data about the risk factors for readmission from either setting.
One study 9 reported an 18% hospital readmission rate for a heterogeneous group of patients discharged to a SNF in the US and also identified patients with congestive heart failure, urinary tract infection, renal failure and respiratory diseases at the highest risk for readmission. A second study 10 found that a history of a malignant solid tumor, a recent hospitalization involving gastrointestinal diseases and a low serum albumin level were associated with an increased risk for 30-day unplanned rehospitalization from a SNF.
There are no data reported on risk factors for readmission in patients who receive (PAC) services in hospital rehabilitation settings. In order to fill this research gap we examined a cohort of elderly Italian patients admitted to an in-hospital rehabilitation setting after an acute hospitalization, given that in Italy about 58% of beds for PAC services after a hospitalization are in rehabilitation hospital settings.11 Our primary aim was to describe the rate of unplanned rehospitalization occurring within 30 days and to identify clinical risk factors for rehospitalization, considering the importance of controlling the phenomenon to avoid the stress to elderly frail patients induced by repeated hospital readmissions.
METHODS
We performed a retrospective cohort study of patients older than 65 years of age and consecutively admitted to an in-hospital rehabilitation setting following an acute care hospitalization. The in-patient rehabilitation setting was the “Ancelle della Carità” Hospital (Cremona, Italy). Patients were admitted to the Department of Rehabilitation and Aged Care (DRAC), a 90 bed unit staffed by full-time geriatricians, physiatrists, nurses, nurse aids, physical, speech and occupational therapists.12 An on-site physician provided 24 hours medical coverage. We excluded patients who were admitted from non-acute care settings, patients younger than 65 years of age, and those who died during the rehabilitation stay. The DRAC admits patients after an acute hospitalization for surgical procedures (hip fracture surgical repair; hip or knee arthroplasty; abdominal, cardiac, vascular or thoracic surgery), stroke (recent or chronic), acute heart failure, chronic obstructive pulmonary diseases, Parkinson, or gait and balance disorders.12 Patients are considered eligible for the DRAC admission if they are capable of performing a standard rehabilitative program including 2 daily sessions per patient (40 minutes in the morning and 40 minutes in the afternoon) from Monday to Friday and a single session (40 minutes in the morning) on Saturday. Specific training is then required according to the admission diagnosis. The Ethics Committee of Gerontological Sciences of the Geriatric Research Group, Italy, approved the study protocol and the waiver of informed consent.
Data Sources
All data were collected through existing administrative databases.
Risk factors for 30-day unplanned rehospitalization to hospital after admission to DRAC
Risk factors for unplanned rehospitalization were determined a priori according to previous research in acute hospital settings,13 clinical importance, and availability/completeness in the administrative databases. In addition, we focused on factors readily available at the time of admission to rehabilitation in order to provide clinicians with variables useful to identify patients at higher risk of hospitalization
Demographic factors included age. Comorbidity was defined according to the Cumulative illness rating score (CIRS);14 CIRS is a comorbidity index, assessing chronic medical illness burden while taking into account the severity of chronic diseases; the score for each of the 14 conditions can range from 1 (absence of pathology) to 5 (maximum level of severity of the disease). The CIRS severity index is the average score of the first 13 items, whereas the Comorbidity Index total score represents the number of the 14 items with a score ≥3. Admission diagnoses to the in-hospital rehabilitation setting were recorded. Additionally, we recorded the diagnoses related to the readmission in acute hospital and we categorized them by reviewing each patient’s medical records.9 A surrogate measure of nutritional status was measured with albumin levels at the time of DRAC admission. Functional status was assessed with the Barthel Index (BI) through patient and surrogate interview referring to the month before the acute hospital admission, 15,16 at rehabilitation admission and discharge. We examined the change in Barthel Index (Delta Barthel Index) defined as the BI pre-acute hospital admission minus the BI at rehabilitation admission; cognitive assessments at DRAC admission included the presence of delirium evaluated by expert geriatricians with the Confusion Assessment Method-CAM17 and global cognitive performance with the MMSE using the Mini Mental State Examination.18 As per the CAM algorithm delirium was considered as present if there was an acute onset or fluctuating course, inattention, and either disorganized thinking or altered level of consciousness. Medication burden was measured by the total number of drugs at DRAC admission. Finally, health care utilization was measured using length of stay (LOS) at the acute hospital measured in days.
Outcome definition
Rehospitalization was defined as every unplanned readmission to the hospital occurring within 30 days after admission to the DRAC. If a patient’s was re hospitalized more than once, each episode was counted as a separate hospitalization.
Statistical analysis
Demographics and clinical variables were summarized using median and interquartile range (IQR) for continuous variables or proportions for categorical variables. For descriptive purposes the admission diagnoses to the in-hospital rehabilitation and the re-admission diagnoses were reported. A multivariable Cox proportional regression model was used to identify the effect of the above-mentioned risk factors on the time to unplanned rehospitalization within the 30-day follow-up. Patient data were censored at time to hospital re-admission. All the risk factors were first entered in the model as continuous variables, except for delirium at DRAC admission. The variables found to be statistically associated with a higher risk of hospital re-admission (p<0.05) were then categorized in tertiles, according to their distribution, to provide clinicians with actionable thresholds that could be applied in daily practice. Because there is no formal definition of polypharmacy we chose the tertiles cut-off for the number of medication, which resulted similar to a previous publication.19 A test for trend showed an increased the risk of hospitalization across three different risk factors: total number of drugs (p=0.000), the delta-Barthel Index (p=0.002), and the length of stay in the acute hospital (p= 0.000). A test for proportional hazard assumption was also performed (chi2 6.92, df 12; p= 0.8625), which showed that there was no evidence to contradict the proportionality of hazard assumption. Kaplan-Meier analyses and log-rank test were also used to assess the effect of these risk factors on time to hospital re-admission. All statistical analyses were performed using STATA version 11(http://www.stata.com/stata11/).
RESULTS
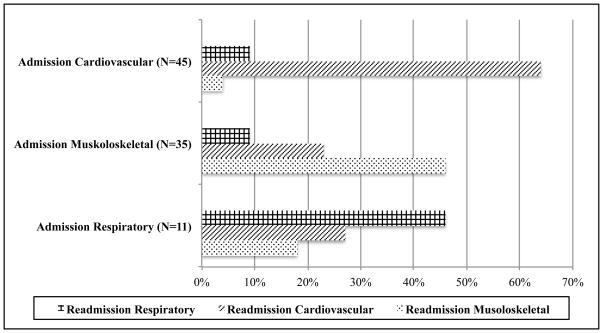
Between January 2004 and June 2011, a total of 6,383 patients were admitted to the DRAC. Of these, 3,648 were excluded: 896 were transferred from other rehabilitation settings, 2144 were admitted from home or skilled nurse facilities, 512 were younger than 65 years of age, and 96 died during the DRAC stay. The remaining cohorts of 2735 patients are described in Table 1. The cohort had a median age of 80 years and the majority (71%) were females. The main overall admission diagnoses to the DRAC were orthopedic (44%), followed by neurologic (16%), respiratory (17%) and cardiologic (10%). The rate of 30-day unplanned rehospitalization was 4% (n=98). In Figure 1 are shown the main causes of readmission to the acute hospital wards. About half of the patients who were admitted to the DRAC with a musculoskeletal (46%), cardiovascular (64%), and respiratory (46%) diagnoses were readmitted with the same diagnosis. (online Appendix 1).
Table 1.
Clinical characteristics and demographics of a population of elderly patients admitted to a Department of Rehabilitation and Aged Care
| Variablea | N= 2735 |
|---|---|
| Age, years | 80 (74–85) |
| Female, n (%) | 1.975 (71%) |
| Barthel index pre-hospital admissionb | 94 (78–100) |
| Barthel index at rehabilitation admission | 44 (26–62) |
| Barthel index at rehabilitation discharge | 82 (57–94) |
| Delta Barthel indexc | 40 (24–56) |
| Cumulative illness rating score severity indexd | 1.62 (1.46–1.84) |
| Number of drugs at rehabilitation admission | 5 (4–7) |
| Albumin at rehabilitation admission, mg/dl | 3.1 (2.8–3.3) |
| Delirium at rehabilitation admission, n (%) | 500 (18%) |
| Mini Mental State Examination at rehabilitation admission | 23 (17–27) |
| Admission diagnoses to the in-hospital rehabilitation setting, n (%) | |
| - Orthopedic | 1204 (44%) |
| - Neurologic | 422 (16%) |
| - Respiratory | 457 (17%) |
| - Cardiologic | 281 (10%) |
| - Gait disturbances | 255 (9%) |
| - Other | 116 (4%) |
| Length of stay acute hospital | 8 (6–13) |
| Length of stay rehabilitation setting | 24 (20–34) |
| Rehospitalization within 30 days, n (%) | 98 (4%) |
Median and interquartile range, unless otherwise noted.
Barthel index a month before the index admission to the acute hospital evaluated through surrogate interview
Delta Barthel index was calculated as the difference of Barthel Index pre-hospital admission (i.e., Barthel index a month before the index acute hospital admission) and the Barthel Index at rehabilitation admission.
Cumulative illness rating score (CIRS) is a screening tool for comorbidity, assessing the chronic medical illness burden while taking into account the severity of chronic diseases; the score for each of the 14 items can range from 1 (absence of pathology) to 5 (maximum level of severity of the disease). The CIRS severity index is the result of the average score of the first 13 items.
Figure 1. Admission and readmission diagnoses.
The figure describes on the y-axis the admission diagnoses to the Department of Rehabilitation and Aged Care for the 112 patients who were readmitted. On the x-axis are reported the main readmission diagnoses. We selected the three more frequents admission diagnoses. Additional data are available in the online Appendix 1.
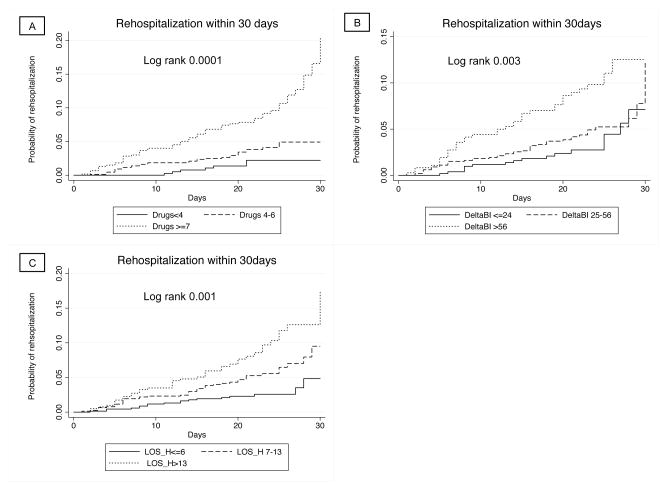
In the multivariable Cox regression models, three clinical variables were independent predictors of time to unplanned re-admission: the total number of drugs, the delta-Barthel Index, and the length of stay in the acute hospital (Table 2). For these variables there was an increasing risk as the dose of exposure increased. Patients taking 7 or more drugs on admission to the DRAC had about a four time higher risk of being rehospitalized (Hazard Ratio [HR] 3.94; 95% Confidence Interval, 1.62–9.54; P=.002), while those taking 4 to 6 drugs had non significant risk of rehospitalization (HR 1.59; 95% Confidence Interval, 0.64–3.94; P=.315) (Figure 2-A). However, the test for trend across categories was statistically significant, indicating the greater number of medications the greater likelihood of readmission. Similarly, those who had the highest decline in functional status (i.e. delta Barthel Index >56) from pre-hospital to DRAC admissions had almost a 3 time higher risk of being rehospitalized (HR 2.67, 95% CI: 1.35–5.27; P=.005), while those with a delta Barthel Index between 25 to 56 did not have an increased risk of rehospitalization (HR 1.48, 95% CI: 0.79–2.75; P=.216), (Figure 2-B). As for the number of medications, the test for trend across Barthel Index categories was statistically significant, indicating the greater functional decline the greater likelihood of readmission. Finally, subjects who had a LOS in the acute hospital longer than 13 days had a more than twofold higher risk of being readmitted to the hospital (HR 2.67, 95% CI: 1.39–5.10; P=.003), while those with a LOS between 7 and 13 days (HR 1.74, 95% CI: 0.93–3.25; P=.080) were not at increased risk of rehospitalization (Figure 2-C). Once again the test for trend across LOS categories was statistically significant, indicating the longer LOS the greater likelihood of readmission.
Table 2.
Risk factors for time to unplanned re-admission to the hospital within 30 days following admission to the Department of Rehabilitation and Aged Care (DRAC).a
| Variable | Hazard Ratio | 95% CI | P value |
|---|---|---|---|
| Age | 1.00 | 0.96–1.03 | .93 |
| CIRS severity index | |||
| 1.46 to 1.84 | 0.98 | 0.45–1.89 | .838 |
| ≥ 1.85 | 1.50 | 0.69–3.28 | .300 |
| Albumin, mg/dl | 0.64 | 0.38–1.05 | .082 |
| Number of drugs at DRAC admission | |||
| <4 drugs | Ref. | ||
| 4 to 6 drugs | 1.59 | 0.64–3.94 | .315 |
| ≥ 7 drugs | 3.94 | 1.62–9.54 | .002 |
| Delta Barthel Index at rehabilitation admissionb | |||
| ≤ 24 | Ref | ||
| 25–56 | 1.48 | 0.79–2.75 | .216 |
| >56 | 2.67 | 1.35–5.27 | .005 |
| Delirium at DRAC admission | 0.77 | 0.40–1.46 | .421 |
| MMSE scorec at DRAC admission | 0.97 | 0.94–1.01 | .128 |
| Length of stay in the acute hospital | |||
| ≤ 6 days | Ref. | ||
| 7–13 days | 1.74 | 0.93–3.25 | .080 |
| >13 days | 2.67 | 1.39–5.10 | .003 |
A multivariable Cox proportional regression model was used to identify the effect of risk factors evaluated at the time of DRAC admission on the time to unplanned readmission to the acute hospital within a 30-day follow-up. All the risk factors were first entered in the model as continuous variables, except for delirium at DRAC admission. The variables found to be statistically associated with a higher risk of hospital re-admission (p<0.05) were then categorized in tertiles, according to their distribution, to provide clinicians with actionable thresholds that could be applied in daily practice.
Delta Barthel index was calculated as the difference of Barthel Index pre-admission (i.e., Barthel index a month before the index acute hospital admission) and the Barthel Index at rehabilitation admission.
Mini Mental State Examination, MMSE
Figure 2.
Probability of unplanned re-admission to the acute hospital according to (A) number of drugs (Drugs) evaluated on the Department of Rehabilitation and Aged Care (DRAC) admission; (B) length of stay in the acute hospital setting (LOS_H); (C) changes in functional status as detected with the delta-Barthel index (deltaBI: Barthel index score pre-hospital admission minus Barthel index score at DRAC admission).
DISCUSSION
In a large cohort of elderly patients admitted to an in-hospital rehabilitation we found a low rate of 4% unplanned rehospitalization. Most of the patients who were admitted to the DRAC with musculoskeletal, cardiovascular, and respiratory diagnoses were readmitted to the acute hospital with the same diagnosis. Among the small but important number of readmitted patients, we found that using 7 or more drugs, having a significant decline in functional performance (i.e., delta Barthel Index ≥ 56 points) in the 30 days before DRAC admission, and having a length of acute hospital stay longer or equal to 13 days were independent predictors of 30-days rehospitalization. These three risk factors are readily accessible at the bedside and offer a potentially simple method to screen for patient risk. Though the data are promising, their role in the prevention of unplanned readmission to hospital needs to be further investigated, evaluating programs to improve transitions of care across different settings.
The topic of short-term unplanned readmissions after discharge from a healthcare facility has received increasing attention. Indeed, the majority of the investigations have studied readmissions among patients leaving the hospital for home,13,20–22 and three studies reported readmissions from the SNFs. 9,10,23 This is the first study, to the best of our knowledge, to report rehospitalization and risk factor data from in hospital PAC rehabilitation facilities.
It is of interest that the readmission rate found in our study is comparable with 30 day readmission data for people discharged home from European acute hospitals 20,21,24 and considerably lower than 30 day readmission rates reported for American patients discharged to all settings. 7,9
There are a variety of potential explanations of these findings. The first relies upon the differences in the acute hospital LOS between Italy and US. Indeed, the average LOS in the US is 5 days,25 while in Italy the overall median acute hospital LOS is about 8 days, similar to other European countries.25 Because previous studies have shown that the shorter the LOS in acute hospital wards, the greater the likelihood of being discharged with unresolved medical issues,26–29 it could be hypothesized that patients transferred from acute hospitals to the PAC rehabilitation settings are more frequently clinically unstable in the US than in the Italian counterpart
An additional explanation relies on the difference in the LOS of in-hospital rehabilitation between US and Italy. Indeed, previous studies 30,31 have shown that not only the median LOS in the American rehabilitation wards fell from 1994 to 2001 from 20 to12 days (exactly the half of median value in our population), but also that this trend 31 was associated with an increased rate of hospital re-admissions in the same period. Therefore, it might be hypothesized that the longer the LOS in the PAC, the lower the risk of being rehospitalized. A plausible explanation of this finding may be that with longer hospital stays, physicians have more time to manage clinical instability, when it develops during the rehabilitation processes.
Third, in the US the in-hospital rehabilitation settings are mainly staffed with physiatrists, while our institution is mainly staffed with geriatricians with the support of physiatrists. Given the advanced age of our population, it might be that a geriatric multidimensional approach provides better care for a frail population with better outcomes, as proven in other settings.32 Indeed, it is interesting to observe that while 18% of our population had delirium on admission to our DRAC, only 2% of the patients were still delirious at the time of discharge. The prevalence of delirium at discharge is lower than previous investigations33,34 in which about 50% of elderly patients who had delirium on admission to PAC still had delirium one month later,33,34 indirectly suggesting a tight clinical surveillance in our setting to prevent and manage conditions possibly related to clinical instability.
Our finding that the longer LOS in acute hospital, the greater risk of hospital readmissions might find an explanation in the concept of “post-hospital syndrome.”35 Patients with a longer LOS are more likely to develop new active medical issues and physical disabilities, suggesting an underlying condition of frailty. These patients should receive a strict clinical surveillance to avoid further complications. In line with this assumption, it has been shown3 by Dharmarajan et al. that the 30-day readmission diagnoses in frail elderly patients is often due to causes involving multiple physiological systems and not only to the conditions related to the initial acute hospitalization. Therefore, as suggested by Ouslander et al.9 patients who are admitted to a rehabilitation setting should be monitored not only for the primary hospital diagnosis, but also for other active medical problems which may lead to rehospitalizations. It is important to underline that our readmission rate was low and that the readmission diagnoses were, in about half of the cases, the same of the hospital admission diagnoses. These data indirectly suggest that the multidimensional geriatric approach in our institution led to an effective clinical management of the frail patients. The avoidance of hospital readmission and the management of the “post-hospital syndrome” in the rehabilitation setting is not only an important marker of the quality of care but it should be on the top list of the clinicians’ priorities to avoid further stress to the patients and family.
In addition to the increased LOS, we found polypharmacy and decline functional status as risk factors for rehospitalization. These findings support previous research from acute hospital settings.21,36–38 Polypharmacy and inappropriate medication prescription are frequent issues in elderly patients and they increase with increasing age and acute hospitalization.39–41 Between 50% and 85% of elderly patients are discharged with potentially or actually inappropriate medications after an acute hospital stay.41,42 Inappropriate medication prescription is associated with greater risk of adverse events such as confusion and falls, as well as increased health care costs, hospitalization, cognitive impairment and mortality.43–46 The association between polypharmacy and rehospitalization might be the expression of the interaction of several drugs and their related adverse reaction,19 though we are unable to support this hypothesis with the data included in our investigation. Additionally, certain offending medications might further explain the adverse association between polypharmacy and rehospitalization. For instance elderly patients are frequently prescribed with proton pump inhibitors for stress ulcer prophylaxis during the acute hospital stay.47 Most of the patients are then discharged on these drugs potentially exposing the patients to a higher risk of pneumonia and clostridium difficile infection.48,49 In our investigation we did not gather this granular information but future investigation should further explore the association between polypharmacy and rehospitalization to explain the underling mechanisms, which should then be target of future interventions.
Finally, the acute decline of functional status also provides clinicians with key information on the patients’ global incapacity to react to a stressful condition as an expression of a baseline frailty.50 The association between functional decline during an acute illness is not just a marker for rehospitalization but can be used at the bedside also to estimates long-term prognosis. 12,51,52
Our study includes a number of notable strengths. It is the first to evaluate the rate of unplanned re-admissions to the hospital, and the related risk factors, in a large population of elderly patients admitted to an in-hospital rehabilitation setting. In addition, our study contains functional and cognitive data obtained from a multidimensional evaluation carried out by expert geriatricians. Findings from this study might represent a basis for National and Regional health systems to stimulate benchmarking policies across post-acute and rehabilitative centers and to implement reimbursement strategies in relation with rehospitalization rates.
Limitations of our study must be considered as well. First, this was a retrospective cohort study carried out in a single center, thus potentially limiting generalizability. In addition, although we examined the total number of medications, we have not addressed whether medication discrepancies, which often occur after the transition from hospital to the setting of discharge, 53 are a risk factor for rehospitalization. Additionally, we were unable to collect information on specific type of drugs (e.g., antipsychotics, sedatives hypnotics). Second, there are additional risk factors we have not accounted for (e.g., social determinants of health such as health literacy, socioeconomic status, caregiver support) that may explain lower rates of re-admission and be important predictors of re-admission. Lastly, the inclusion of admission diagnoses as possible confounding factors should also be included in future studies.
This study provides new important information on the epidemiology of unplanned rehospitalization of elderly patients admitted to an in-hospital rehabilitation setting after an acute hospitalization. Furthermore, it identifies three risk factors of unplanned 30-day rehospitalization, which are easily accessible at the bed-side and should be used as a simple predictive model for clinicians at the time of admission to in-hospital rehabilitation.
Supplementary Material
Acknowledgments
Dr. Vasilevskis is supported by the National Institutes of Health (K23AG040157), the Veterans Affairs Clinical Research Center of Excellence, and the Geriatric Research, Education and Clinical Center (GRECC). The authors’ funding sources did not participate in the planning, collection, analysis or interpretation of data or in the decision to submit for publication. The investigators had full access to the data and were responsible for the study protocol, statistical analysis plan, progress of the study, analysis, reporting of the study and the decision to publish. We would like to acknowledge Dr Sara Morghen and Dr Elena Lucchi for their support in data collection.
Footnotes
Conflict of interests: None
Bibliography
- 1.WHO. Regional Office for Europe’s Health Evidence Network (HEN): Do current discharge arrangements from inpatient hospital care for the elderly reduce readmission rates, the length of inpatient stay or mortality, or improve health status? 2005. [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. The New England journal of medicine. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 3.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA : the journal of the American Medical Association. 2013;309:355–63. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Commission MPA. Report to the Congress: Promoting Greater Efficiency in Medicare. Washington DC: Medicare Payment Advisory Commission; 2007. [Google Scholar]
- 5.Robinson P. Hospitals readmissions and the 30 day threshold. London: CHKS; 2010. [accessed 12 Nov 2012]. http://www.chks.co.uk/assets/files/Hospital_readmissions_and_the_30_day_threshold_final.pdf. [Google Scholar]
- 6.MedPAC. Report to the Congress: Medicare Payment Policy. Washington, DC: Medicare Payment Advisory Commission; 2011. [Google Scholar]
- 7.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health affairs. 2010;29:57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gozalo P, Mor V. Personal Communication. Brown University, Department of Health Services, Policy and Practice; Rates of 30-day rehospitalization by PAC setting. [Google Scholar]
- 9.Ouslander JG, Diaz S, Hain D, Tappen R. Frequency and diagnoses associated with 7-and 30-day readmission of skilled nursing facility patients to a nonteaching community hospital. Journal of the American Medical Directors Association. 2011;12:195–203. doi: 10.1016/j.jamda.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Dombrowski W, Yoos JL, Neufeld R, Tarshish CY. Factors Predicting Rehospitalization of Elderly Patients in a Postacute Skilled Nursing Facility Rehabilitation Program. Archives of physical medicine and rehabilitation. 2012;93:1808–13. doi: 10.1016/j.apmr.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 11.Boldrini M, Di Cesare M, Pennazza F. Dipartimento della Qualità. Direzione Generale del Sistema Informativo; 2003. Rapporto “Riabilitazione 2003”: Ministero della Salute. [Google Scholar]
- 12.Bellelli G, Magnifico F, Trabucchi M. Outcomes at 12 months in a population of elderly patients discharged from a rehabilitation unit. Journal of the American Medical Directors Association. 2008;9:55–64. doi: 10.1016/j.jamda.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 13.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA : the journal of the American Medical Association. 2011;306:1688–98. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parmelee PA, Thuras PD, Katz IR, Lawton MP. Validation of the Cumulative Illness Rating Scale in a geriatric residential population. Journal of the American Geriatrics Society. 1995;43:130–7. doi: 10.1111/j.1532-5415.1995.tb06377.x. [DOI] [PubMed] [Google Scholar]
- 15.Mahoney Fi BD. Functional evaluation: The Barthel index. Md State Med J. 1965;14:61–5. [PubMed] [Google Scholar]
- 16.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- 17.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Annals of internal medicine. 1990;113:941–8. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 18.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of psychiatric research. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 19.Onder G, Petrovic M, Tangiisuran B, et al. Development and validation of a score to assess risk of adverse drug reactions among in-hospital patients 65 years or older: the GerontoNet ADR risk score. Archives of internal medicine. 2010;170:1142–8. doi: 10.1001/archinternmed.2010.153. [DOI] [PubMed] [Google Scholar]
- 20.Bisharat N, Handler C, Schwartz N. Readmissions to medical wards: Analysis of demographic and socio-medical factors. European journal of internal medicine. 2012;23:457–60. doi: 10.1016/j.ejim.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 21.Zamir D, Zamir M, Reitblat T, Zeev W, Polishchuk I. Readmissions to hospital within 30 days of discharge from the internal medicine wards in southern Israel. European journal of internal medicine. 2006;17:20–3. doi: 10.1016/j.ejim.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Bianco A, Mole A, Nobile CG, Di Giuseppe G, Pileggi C, Angelillo IF. Hospital readmission prevalence and analysis of those potentially avoidable in southern Italy. PloS one. 2012;7:e48263. doi: 10.1371/journal.pone.0048263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marcantonio ER, Kiely DK, Simon SE, et al. Outcomes of older people admitted to postacute facilities with delirium. Journal of the American Geriatrics Society. 2005;53:963–9. doi: 10.1111/j.1532-5415.2005.53305.x. [DOI] [PubMed] [Google Scholar]
- 24.Guerini F, Frisoni GB, Morghen S, Speciale S, Bellelli G, Trabucchi M. Clinical instability as a predictor of negative outcomes among elderly patients admitted to a rehabilitation ward. Journal of the American Medical Directors Association. 2010;11:443–8. doi: 10.1016/j.jamda.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 25.OECD. OECD Indicators. 2011. Health at a Glance 2011. [Google Scholar]
- 26.Halm EA, Fine MJ, Kapoor WN, Singer DE, Marrie TJ, Siu AL. Instability on hospital discharge and the risk of adverse outcomes in patients with pneumonia. Archives of internal medicine. 2002;162:1278–84. doi: 10.1001/archinte.162.11.1278. [DOI] [PubMed] [Google Scholar]
- 27.Halm EA, Magaziner J, Hannan EL, et al. Frequency and impact of active clinical issues and new impairments on hospital discharge in patients with hip fracture. Archives of internal medicine. 2003;163:108–13. doi: 10.1001/archinte.163.1.107. [DOI] [PubMed] [Google Scholar]
- 28.Metersky ML, Tate JP, Fine MJ, Petrillo MK, Meehan TP. Temporal trends in outcomes of older patients with pneumonia. Archives of internal medicine. 2000;160:3385–91. doi: 10.1001/archinte.160.22.3385. [DOI] [PubMed] [Google Scholar]
- 29.Qian X, Russell LB, Valiyeva E, Miller JE. ‘Quicker and sicker’ under medicare’s prospective payment system for hospitals: new evidence on an old issue from a natioanl longitudinal survey. Bulletin of economic research. 2011;63:3307–78. doi: 10.1111/j.1467-8586.2010.00369.x. [DOI] [PubMed] [Google Scholar]
- 30.Ottenbacher KJ, Smith PM, Illig SB, Linn RT, Ostir GV, Granger CV. Trends in length of stay, living setting, functional outcome, and mortality following medical rehabilitation. JAMA : the journal of the American Medical Association. 2004;292:1687–95. doi: 10.1001/jama.292.14.1687. [DOI] [PubMed] [Google Scholar]
- 31.Ottenbacher KJ, Smith PM, Illig SB, Fiedler RC, Granger CV. Length of stay and hospital readmission for persons with disabilities. American journal of public health. 2000;90:1920–3. doi: 10.2105/ajph.90.12.1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ellis G, Whitehead MA, O’Neill D, Langhorne P, Robinson D. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane database of systematic reviews. 2011:CD006211. doi: 10.1002/14651858.CD006211.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kiely DK, Bergmann MA, Jones RN, Murphy KM, Orav EJ, Marcantonio ER. Characteristics associated with delirium persistence among newly admitted post-acute facility patients. The journals of gerontology Series A, Biological sciences and medical sciences. 2004;59:344–9. doi: 10.1093/gerona/59.4.m344. [DOI] [PubMed] [Google Scholar]
- 34.Marcantonio ER, Simon SE, Bergmann MA, Jones RN, Murphy KM, Morris JN. Delirium symptoms in post-acute care: prevalent, persistent, and associated with poor functional recovery. Journal of the American Geriatrics Society. 2003;51:4–9. doi: 10.1034/j.1601-5215.2002.51002.x. [DOI] [PubMed] [Google Scholar]
- 35.Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. The New England journal of medicine. 2013;368:100–2. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Philbin EF, DiSalvo TG. Prediction of hospital readmission for heart failure: development of a simple risk score based on administrative data. Journal of the American College of Cardiology. 1999;33:1560–6. doi: 10.1016/s0735-1097(99)00059-5. [DOI] [PubMed] [Google Scholar]
- 37.van Walraven C, Dhalla IA, Bell C, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 2010;182:551–7. doi: 10.1503/cmaj.091117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. Journal of general internal medicine. 2010;25:211–9. doi: 10.1007/s11606-009-1196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Corsonello A, Pedone C, Corica F, Incalzi RA. Polypharmacy in elderly patients at discharge from the acute care hospital. Therapeutics and clinical risk management. 2007;3:197–203. doi: 10.2147/tcrm.2007.3.1.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burgess CL, Holman CD, Satti AG. Adverse drug reactions in older Australians, 1981–2002. The Medical journal of Australia. 2005;182:267–70. doi: 10.5694/j.1326-5377.2005.tb06698.x. [DOI] [PubMed] [Google Scholar]
- 41.Morandi A, Vasilevskis EE, Pandharipande PP, et al. Inappropriate medications in elderly ICU survivors: where to intervene? Archives of internal medicine. 2011;171:1032–4. doi: 10.1001/archinternmed.2011.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Onder G, Landi F, Cesari M, Gambassi G, Carbonin P, Bernabei R. Inappropriate medication use among hospitalized older adults in Italy: results from the Italian Group of Pharmacoepidemiology in the Elderly. European journal of clinical pharmacology. 2003;59:157–62. doi: 10.1007/s00228-003-0600-8. [DOI] [PubMed] [Google Scholar]
- 43.Wright RM, Roumani YF, Boudreau R, et al. Effect of central nervous system medication use on decline in cognition in community-dwelling older adults: findings from the Health, Aging And Body Composition Study. Journal of the American Geriatrics Society. 2009;57:243–50. doi: 10.1111/j.1532-5415.2008.02127.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fick DM, Mion LC, Beers MH, JLW Health outcomes associated with potentially inappropriate medication use in older adults. Research in nursing & health. 2008;31:42–51. doi: 10.1002/nur.20232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hanlon JT, Schmader KE, Samsa GP, et al. A method for assessing drug therapy appropriateness. Journal of clinical epidemiology. 1992;45:1045–51. doi: 10.1016/0895-4356(92)90144-c. [DOI] [PubMed] [Google Scholar]
- 46.Lau DT, Kasper JD, Potter DE, Lyles A, Bennett RG. Hospitalization and death associated with potentially inappropriate medication prescriptions among elderly nursing home residents. Archives of internal medicine. 2005;165:68–74. doi: 10.1001/archinte.165.1.68. [DOI] [PubMed] [Google Scholar]
- 47.Hajjar ER, Hanlon JT, Sloane RJ, et al. Unnecessary drug use in frail older people at hospital discharge. Journal of the American Geriatrics Society. 2005;53:1518–23. doi: 10.1111/j.1532-5415.2005.53523.x. [DOI] [PubMed] [Google Scholar]
- 48.Giuliano C, Wilhelm SM, Kale-Pradhan PB. Are proton pump inhibitors associated with the development of community-acquired pneumonia? A meta-analysis. Expert review of clinical pharmacology. 2012;5:337–44. doi: 10.1586/ecp.12.20. [DOI] [PubMed] [Google Scholar]
- 49.Kwok CS, Arthur AK, Anibueze CI, Singh S, Cavallazzi R, Loke YK. Risk of Clostridium difficile infection with acid suppressing drugs and antibiotics: meta-analysis. The American journal of gastroenterology. 2012;107:1011–9. doi: 10.1038/ajg.2012.108. [DOI] [PubMed] [Google Scholar]
- 50.Sleiman I, Rozzini R, Barbisoni P, et al. Functional trajectories during hospitalization: a prognostic sign for elderly patients. The journals of gerontology Series A, Biological sciences and medical sciences. 2009;64:659–63. doi: 10.1093/gerona/glp015. [DOI] [PubMed] [Google Scholar]
- 51.Inouye SK, Peduzzi PN, Robison JT, Hughes JS, Horwitz RI, Concato J. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA : the journal of the American Medical Association. 1998;279:1187–93. doi: 10.1001/jama.279.15.1187. [DOI] [PubMed] [Google Scholar]
- 52.Bellelli G, Noale M, Guerini F, et al. A prognostic model predicting recovery of walking independence of elderly patients after hip-fracture surgery. An experiment in a rehabilitation unit in Northern Italy. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2012;23:2189–200. doi: 10.1007/s00198-011-1849-x. [DOI] [PubMed] [Google Scholar]
- 53.Coleman EA, Smith JD, Raha D, Min SJ. Posthospital medication discrepancies: prevalence and contributing factors. Archives of internal medicine. 2005;165:1842–7. doi: 10.1001/archinte.165.16.1842. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.