Abstract
Congenital midgut malrotation is a complex gastrointestinal anomaly, which could easily lead to midgut volvulus and gastrointestinal obstruction. Large studies on congenital midgut malrotation in adults are rarely investigated. The current study aimed to explore the clinical profile and diagnostic modalities of congenital midgut malrotation in Chinese adult patients. Clinical and radiological data of eight adult patients with intestinal malrotation were retrospectively analyzed and related literatures were simultaneously reviewed. Mean age of patients was 41.25 years range, 14 to 63 years. Abdominal radiography and computerized tomography (CT) were conducted for all studied patients prior to surgery, and the diagnosis of congenital midgut malrotation was confirmed during surgery. All patients underwent volvulus reduction, Ladd’s band loosening, and stage I appendectomy. In addition, three patients received additional extensive intestinal adhesion loosening, and one patient received resection of bowel up to 50 cm. All patients recovered well after surgery, and no recurrence and adhesive intestinal obstruction were reported. All three patients with malnutrition prior to surgery had gained significant weight. Thus, we consider that adult congenital intestinal malrotation accompanied with midgut volvulus should be treated with surgery as soon as possible. Preoperative colour ultrasonography and CT are helpful for definitive diagnosis.
Keywords: Congenital intestinal malrotation, midgut volvulus, computed tomography
Introduction
Congenital intestinal malrotation is a complex gastrointestinal anomaly, which could easily lead to midgut volvulus and gastrointestinal obstruction. It occurs predominantly in the infants and rarely in adults [1,2]. Over 90% of patients with this condition were reported to present at by their first birthday [3]. So far, large studies on this condition only focus on infants, while its characteristics and diagnosis in adults are rarely investigated. Ladd’s procedure has been indicated in adults, although it is the standard procedure in children with congenital midgut malrotation [4]. In elderly patients with acute symptoms, earlier diagnosis and surgical procedure could save their lives [5]. This widely regarded pediatric pathology was reported as initially presented as acute bowel obstruction in adults [6]. The current study aimed to explore the clinical profile and diagnostic modalities of congenital midgut malrotation in Chinese adult patients. Clinical and radiological data of eight adult patients with congenital intestinal malrotation were retrospectively analyzed and related literatures were simultaneously reviewed.
Materials and methods
Patients
This retrospective study involved eight Chinese adult patients with congenital midgut malrotation hospitalized at the Department of Gastrointestinal Surgery, Third Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China during 2004 to 2012 Patients included 5 male and 3 female patients with a mean age of 41.25 years old (range 14 to 63 years old). The disease course ranged from 5 days to 18 months. The chief complaints of these patients included epigastric distension, anorexia and fatigue for 10 to 18 months (n=2); epigastric distension, nausea and vomiting from 7 to 20 days (n=4); and recurrent epigastric vague pain for 1 year and sudden sharp colic pain for 2 days (n=1). Notably, a 32-week pregnant women was referred from Obstetrical Department to the Gastrointestinal Surgery with recurrent abdominal pain and vomiting. Of the eight patients, three were accompanied by malnutrition.
Diagnosis of congenital midgut malrotation
Of the eight patients, the diagnosis of congenital midgut malrotation in five patients was confirmed by computerized tomography (CT), displaying positional crossing and whirlpool volvulus of superior mesenteric vein and artery (Figure 1A). The condition in three patients was diagnosed by color ultrasonography, displaying circumferential elicitor mass in the upper abdominal cavity, abundant whirlpool strip flow signals in the mesentery and elicitor rotation of superior mesenteric vein around artery (Figure 1B). For the pregnant woman, the diagnosis was not defined by both colour ultrasonography and magnetic resonance imaging (MRI), but distal duodenal obstruction was confirmed. The patient with sharp abdominal pain presented with physical signs relating to acute peritonitis, only dilation, gas, and effusion in the stomach and duodenum were displayed in the preoperative abdominal radiography. He did not receive further imaging examinations.
Figure 1.
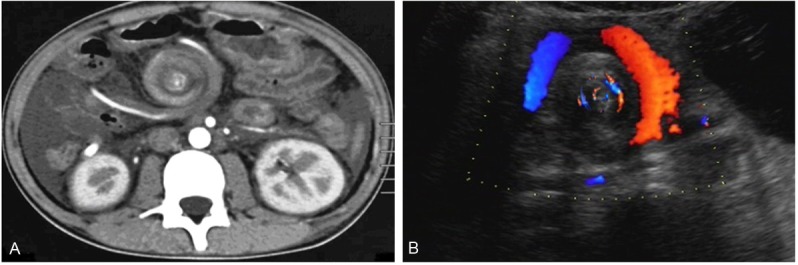
CT: whirlpool volvulus of superior mesenteric vein and artery (A). Color ultrasonography: whirlpool volvulus of superior mesenteric vein and artery (B).
Treatment
Conditions of all patients were surgically treated. Prior to surgery, proper fluids were infused, water-electrolyte disequilibrium was corrected, and antibiotics were given to prevent infections. Surgical approaches varied with pathological types. Gut volvulus reduction, Ladd’s band loosening and stage I appendectomy were performed in all patients. During surgery, the initial jejunum and transverse colon were routinely inspected; if necessary, the initial jejunum was fixed and the transverse colon was loosened. Post surgery, gastrointestinal decompression, fluid infusion and venous nutritional support were persisted until she could orally take the whole fluid food.
Results
Operative findings
The ligament of Treitz was absent in all cases. The horizontal duodenum, jejunum, ileum and right colon left to the superior mesenteric artery twist in the root of mesentery. Bowels rotate and wrap around the superior mesenteric vessels for 1.5 to 3 cycles (Figure 2A). Obstruction occurs in the horizontal duodenum and initial jejunum 2 patients. In most cases, proximal duodenum and stomach have different degrees of dilation and hypertrophy and the ascending colon is separated (Figure 2B).
Figure 2.
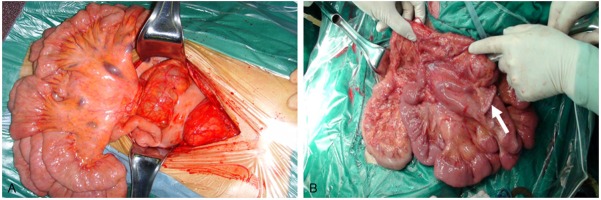
Bowels rotate and wrap around the superior mesenteric vessels (A). The ascending colon is separated and the appendix is visible Arrow showed (B).
Mesenteric lymphadenectasis and tortuosity and dilation of the superior mesenteric vein are common 5 patients. Three patients had different degrees of intestinal canal adhesion and received additional adhesion release. The patient with peritonitis was found ischemia and necrosis of 50 cm in small intestine which had to be removed. For the pregnant women, the uterus was enlarged and entered into the abdominal cavity; to avoid any difficulty in surgery, the right colon was fixed in a higher position.
Treatment outcomes
Of the 8 patients, 7 showed good prognosis and normal healing, with no surgical complications and incision infection. The pregnant woman was referred to the Obstetrical Department for further treatment, but her fetal development arrested 7 days after surgery. Induction delivery was performed. Eventually, the patient healed and discharged.
Safety follow-up
During the follow-up of 3 months to 5 years, midgut volvulus did not recur and no significantly abnormal gastrointestinal symptoms were reported. Three patients with malnutrition prior to surgery gained significant weight. The patient with partial small bowel resection showed good nutritional condition. Two patients received barium-meal radiography at 6 months after surgery; however, no other abnormalities were observed.
Discussion
The present work involved the retrospective analysis of clinical profile and diagnostic modalities of congenital midgut malrotation in eight Chinese adult patients. Outcomes to surgical treatment were promising during the follow-up till five years. Intestinal malrotation [7] is characterized with abnormal intestinal position, isolated mesentery and intestinal obstruction owing to absent or incomplete rotation of embryonic gut. The exact cause remains unclear. In pathology, it is mainly presented with abnormal termination of normal intestinal rotation and attachment of mesentery, which causes compression of duodenal and upper jejuna bands, ectopic appendix and midgut volvulus. Malrotation rarely happens in adulthood; hence, it is hard to diagnose in an initial stage [8]. Most patients visit the hospital only when acute or chronic volvulus occurs. Recurrent abdominal pain, distension, nausea, vomiting and anal insufflations and defecate close are predominant manifestations. Some patients can be accompanied with malnutrition and a few patients experience peritonitis from bowel strangulation and ischemia. In the current study, three patients had malnutrition prior to surgery. Two patients were only presented with abdominal distension and anorexia, while other six developed intestinal obstruction one with partial intestinal necrosis. Of the six patients with intestinal obstruction, five complained abdominal distension and nausea, while another had no significant gastrointestinal symptoms. These findings suggest that symptoms of adult congenital intestinal malrotation are not always acute or specific and often present as the intestinal obstruction.
Imaging examinations such CT and colour ultrasonography play an important role in the diagnosis of adult congenital intestinal malrotation. Of the eight patients, condition of five was confirmed by CT, displaying positional crossing and whirlpool volvulus of superior mesenteric vein and artery. Condition of three patients was confirmed by color ultrasonography, displaying circumferential elicitor mass in the upper abdominal cavity, abundant whirlpool strip flow signals in the mesentery and elicitor rotation of superior mesenteric vein around artery. This suggested the availability and accuracy of the two imaging modalities in the diagnosis. The pregnant woman was not confirmed either by colour ultrasonography or MRI, possibly due to the forward and upward position of bowels pushed by enlarged uterus and unsafe use of contrast agents. Positional crossing and whirlpool sign of superior mesenteric vein and artery are characteristic for intestinal malrotation and volvulus. In CT images of five patients, the normal position of superior mesenteric vein and artery disappeared, and dilated veins and mesentery arranged around the axis of the superior mesenteric arterywhirlpool sign, indicating a pathological change which was validated during surgery. It was reported that CT could assist in definitive diagnosis even after the disappearance of symptoms [9,10]. Although midgut volvulus could resolve by changing the posture, the mesentery and related arteries could remain in abnormal arrangement, which could result in serious consequences such as intestinal necrosis. CT allows early diagnosis and treatment. Abdominal colour ultrasonography also can display the positional crossing and whirlpool rotation [11,12] and is more practical.
There was a pregnant case in the current study who presented recurrent vomiting. Color ultrasonography and MRI only displayed distal duodenal obstruction; however, they could not definite the diagnosis, suggesting the limitation of imaging examinations. This series of cases is extremely rare and should be paid more attention to [13-16].
The majority of adults with congenital intestinal malrotation and volvulus have acute abdomen symptoms and even intestinal strangulation and necrosis. In the current study, six patients were found with intestinal obstruction in diagnosis; of which, one was accompanied by intestinal necrosis in surgery. Currently, an emergent surgery is recommended once the diagnosis is made [17]. However, few patients did not have intestinal obstruction. In one patient, bowels turned around the axis of superior mesenteric vessels for 2.5 cycles and fibers adhered extensively among bowels, with no intestinal obstruction. Surgery is still definitively indicated for such patients, because preoperative imaging examinations are incapable of identifying adhesion among bowels and reducing the incidences of intestinal obstruction, strangulation, and necrosis.
The success of surgical treatment lies in judging the rotation form and degree and the correct knowledge of rotation form is the premise of successful lysis and reduction. Other critical aspect is complete lysis of the Ladd’s band, which removes the membranaceous adhesion of peritoneal bands and upper jejunum pressing the duodenum. All surgical procedures should be carefully performed. During lysis, the superior mesenteric vein and artery should be paid special attention to prevent any damage. In some patients, rotation leads to compression and deformation of the superior mesentery vein, which is often erroneously identified as adhered bands. The vein damage induces the intestine resection will result in short bowel syndrome. The appendix is also resected together during surgery to avoid delayed diagnosis due to positional variation of cecum.
The majority of adult congenital midgut volvulus has favorable prognosis. Only those with extensive bowel necrosis have to receive surgical resection. In the current study, all eight patients received gut volvulus reduction, Ladd’s band loosening and stage I appendectomy; of which, three received additional extensive intestinal adhesion lysis and one received 50-cm bowel resection. All the patients recovered well after surgery. In the follow-up, no recurrence of gut volvulus or adhesional intestinal obstruction was found. Three patients with preoperative malnutrition had different degrees of weight gain. Unfortunately, the fetal development arrested in the pregnant woman 7 days after surgery, likely due to the lack of nutrition intake during intestinal obstruction, surgical stress and consumption of various drugs.
In conclusion, adult congenital midgut volvulus is often manifested with symptoms with regard to intestinal obstruction. Some patients are accompanied with malnutrition and intestinal necrosis; if require, surgery should be conducted in an early stage, including gut volvulus reduction, Ladd’s band loosening and stage I appendectomy. The outcomes of these surgical procedures are favorable. Color ultrasonography and CT are helpful for preoperative diagnosis and positional crossing and whirlpool volvulus of superior mesenteric vein and artery are the characteristic manifestations of congenital midgut malrotation.
Disclosure of conflict of interest
None.
References
- 1.Hsu SD, Yu JC, Chou SJ, Hsieh HF, Chang TH, Liu YC. Midgut volvulus in an adult with congenital malrotation. Am J Surg. 2008;195:705–7. doi: 10.1016/j.amjsurg.2007.01.044. [DOI] [PubMed] [Google Scholar]
- 2.Applegate KE, Anderson JM, Klatte EC. Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics. 2006;26:1485–500. doi: 10.1148/rg.265055167. [DOI] [PubMed] [Google Scholar]
- 3.von Flüe M, Herzog U, Ackermann C, Tondelli P, Harder F. Acute and chronic presentation of intestinal nonrotation in adults. Dis Colon Rectum. 1994;37:192–8. doi: 10.1007/BF02047549. [DOI] [PubMed] [Google Scholar]
- 4.Seymour NE, Andersen DK. Laparoscopic treatment of intestinal malrotation in adults. JSLS. 2005;9:298–301. [PMC free article] [PubMed] [Google Scholar]
- 5.Pickhardt PJ, Bhalla S. Intestinal malrotation in adolescents and adults: spectrum of clinical and imaging features. AJR Am J Roentgenol. 2002;179:1429–35. doi: 10.2214/ajr.179.6.1791429. [DOI] [PubMed] [Google Scholar]
- 6.Emanuwa OF, Ayantunde AA, Davies TW. Midgut malrotation first presenting as acute bowel obstruction in adulthood: a case report and literature review. World J Emerg Surg. 2011;6:22. doi: 10.1186/1749-7922-6-22. doi: 10.1186/1749-7922-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aslanabadi S, Ghalehgolab-Behbahan A, Jamshidi M, Veisi P, Zarrintan S. Intestinal malrotations: a review and report of thirty cases. Folia Morphol (Warsz) 2007;66:277–82. [PubMed] [Google Scholar]
- 8.Gamblin TC, Stephens RE Jr, Johnson RK, Rothwell M. Adult malrotation: a case report and review of the literature. Curr Surg. 2003;60:517–20. doi: 10.1016/S0149-7944(03)00030-8. [DOI] [PubMed] [Google Scholar]
- 9.Yama N, Akiba H, Tamakawa M, Oouchi A, Sakata K, Koito K, Hareyama M, Morita K. Spontaneously reduced midgut malrotation: CT diagnosis. Abdom Imaging. 2000;25:132–3. doi: 10.1007/s002619910031. [DOI] [PubMed] [Google Scholar]
- 10.Strouse PJ. Clinics in diagnostic imaging (74). Midgut malrotation with volvulus. Singapore Med J. 2002;43:325–8. [PubMed] [Google Scholar]
- 11.Ojeda CM, Prochazka ZR, Vila GS, Piscoya RA, De Los Ríos SR, Pinto VJL, Huerta-Mercado TJ, Bussalleu RA. Intestinal malrotation in the adult: case report and review of literature. Rev Gastroenterol Peru. 2006;26:395–9. [PubMed] [Google Scholar]
- 12.Kapfer SA, Rappold JF. Intestinal malrotation-not just the pediatric surgeon’s problem. J Am Coll Surg. 2004;199:628–35. doi: 10.1016/j.jamcollsurg.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 13.Hardikar JV. Malrotation of the gut manifested during pregnancy. J Postgrad Med. 2000;46:106–7. [PubMed] [Google Scholar]
- 14.Wang DG, Chen H, Yu J, Yu Q, Zhou HY. Midgut malrotation during pregnancy: a case report. Journal of New Medicine. 2007;17:237–239. [Google Scholar]
- 15.Scheuermeyer F. Precipitous decline of gravid patient with congenital small bowel malrotation. Am J Emerg Med. 2009;27:629, e5–6. doi: 10.1016/j.ajem.2008.08.034. [DOI] [PubMed] [Google Scholar]
- 16.Rothstein RD, Rombeau JL. Intestinal malrotation during pregnancy. Obstet Gynecol. 1993;81:817–9. [PubMed] [Google Scholar]
- 17.Sodhi KS, Khandelwal N. Upper gastrointestinal studies in malrotation. Pediatr Radiol. 2008;38:1034. doi: 10.1007/s00247-008-0926-6. [DOI] [PubMed] [Google Scholar]


