Abstract
Multi-parametric MRI (MP-MRI) provides an accurate anatomical assessment of the tumor and its local staging. Herein we report a case of intermediate risk prostatic adenocarcinoma, initially followed on active surveillance, which upgraded from Gleason 7 (3+4) to Gleason 8 (4+4) on transrectal ultrasound/MRI (TRUS/MRI) fusion biopsy after progression of MR spectroscopic findings and review the role of MP-MRI in the follow-up of prostate cancer patients undergoing active surveillance.
Keywords: prostate carcinoma, MRI, active surveillance, MR spectroscopy
Introduction
Prostate cancer is the most common noncutaneous malignancy in American men. The slow-growing nature and long latency time of many tumors highlight the urgent need to predict which tumors will grow and spread beyond the prostate as compared to which tumors will never cause problems of clinical significance. MP-MRI is a noninvasive method of identifying tumor location as well as functional characteristics to predict tumor behavior and is an important component in the follow-up of patients with prostate cancer on active surveillance. Functional MR sequences such as MR spectroscopy are particularly important in predicting tumor aggressiveness, although further validation studies should be performed.
Case
A 62-year-old man with a serum prostate specific antigen (PSA) of 3.15 ng/dl on active surveillance presented for a prostate MP-MRI following a positive outside biopsy of Gleason 3+4 in one out of eight cores. MP-MRI revealed a 1cm lesion in the right apical-mid peripheral zone, which was positive on T2W MRI, DW MRI, and DCE MRI but negative on MR spectroscopy (Fig. 1) [1]. The lesion was targeted by MR-transrectal ultrasound (TRUS/MRI) fusion guided biopsy, which showed two out of eighteen cores of Gleason 7 (3+4) with 40% and 55% involvement. The patient was offered definitive treatment; however he preferred to remain on active surveillance and underwent MP-MRI eighteen months after his baseline MRI. His PSA remained stable at 3.28 ng/dl, however the right apical-mid peripheral zone lesion grew to 1.3 cm and was now also positive on MR spectroscopy (Fig. 2) [1]. A second TRUS/MRI fusion guided biopsy was performed, which showed Gleason 8 (4+4) in three out of twenty cores with up to 80% involvement. At this time, treatment was recommended again and the patient underwent a radical prostatectomy, which demonstrated consistent pathological grading (Gleason 4+4) at the right apical-mid peripheral zone location.
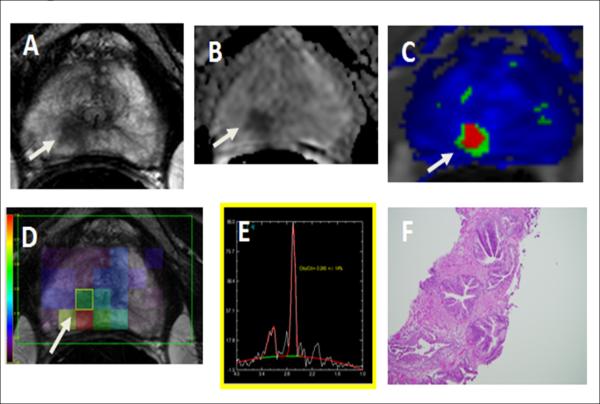
Figure 1.
A 62-year-old man with serum PSA of 3.15 ng/mL. (A) Axial T2W MRI, (B) ADC map of DW image, and (C) ktrans map derived from DCE MRI demonstrate a 1cm right apical mid-peripheral zone lesion (arrow). (D, E) MR spectroscopy was diagnostic and negative with a choline/citrate ratio of 0.243 +/− 14% (arrow). (F) Subsequent transrectal ultrasonography/MRI fusion-guided biopsy revealed Gleason 3+4 cancer in the lesion (up to 55% core involvement).
Figure 2.
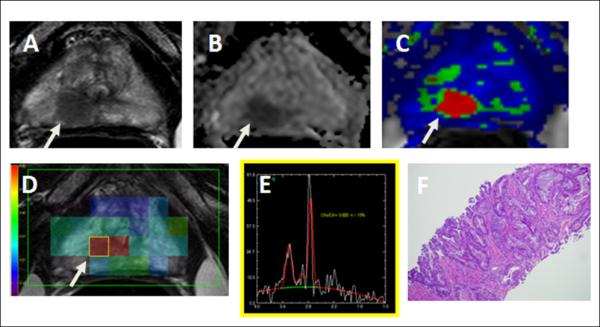
A 63-year-old man with serum PSA of 3.28 ng/mL. (A) Axial T2W MRI, (B) ADC map of DW image, and (C) ktrans map derived from DCE MRI demonstrate a 1.3cm right apical mid-peripheral zone lesion (arrow). (D, E) MR spectroscopy was diagnostic and positive with a choline/citrate ratio of 0.623 +/− 13% (arrow). (F) Subsequent transrectal ultrasonography/MRI fusion-guided biopsy revealed Gleason 4+4 cancer in the lesion (up to 80% core involvement).
Discussion
With more than 238,590 new cases and 29,720 deaths predicted for 2013 in the United States, prostate cancer is the most common cancer in adult males, excluding skin cancer, and is the second most common cause of cancer deaths in men [2]. Largely as a result of increased PSA screening tests which increases early stage diagnosis, about one in six men are now diagnosed with prostate cancer in their lifetime, but only one in thirty-three will die [3]. Unfortunately there is rarely a clear treatment recommendation for patients diagnosed with localized, low-risk prostate cancer, who face an array of treatment options ranging from active surveillance to whole-gland radical therapy. Predicting the clinical course of a tumor is not straightforward, and the risks of treatment (incontinence, impotence, bowel changes) must be weighed against the uncertainty of long-term cancer control without treatment.
Active surveillance is usually reserved for low- or intermediate risk disease, while patients with intermediate- or high-risk disease are often counseled to undergo surgery or radiation therapy. The goal of active surveillance is to avoid radical treatment and its side effects in men who have truly low risk prostate cancer, while offering radical treatment to those men who are at higher risk of local progression or metastatic disease. The traditional tools used to attribute these risk categories are prostate specific antigen, digital rectal examination, transrectal biopsy and their repeated application over time.
Increasingly, multiparametric MRI (MP-MRI) is emerging as a tool which may be able to more accurately determine the risk of significant disease at diagnosis and its progression over time, making MP-MRI a useful method in the follow-up of active surveillance patients with prostate cancer [4]. MP-MRI provides an anatomical assessment which can determine the location of the tumor and whether the tumor is localized to the prostate or it has spread beyond [5]. Lesions are typically hypointense on T2-weighted images, however this has low specificity for prostate cancer since many benign conditions such as hemorrhage, prostatitis, benign prostatic hyperplasia, radiation therapy, and hormonal therapy can all cause low signal in the peripheral zone [6]. Additional MR sequences such as MR spectroscopic imaging, dynamic contrast-enhanced (DCE)-MR imaging, and diffusion-weighted imaging sequences offer more functional information about the biochemical changes, vascularity, permeability and free water length path, respectively and provide greater insight into tumor aggressiveness [7]. Initial data suggest that the negative predictive value of a normal MP-MRI for clinically significant prostate cancer is 95%, making MP-MRI a useful tool in determining whether a patient is a candidate for active surveillance [8].
In this case, a patient with intermediate risk disease who chose active surveillance based on personal preference underwent serial MR imaging, which detected advancing disease after positive MR spectroscopy findings. MR spectroscopy is a functional method of measuring the intracellular concentrations of choline and citrate. Metabolic spectra from volumes of interest (voxels) encompassing cancerous tissue show increased levels of choline and decreased levels of citrate due to the increased cell membrane turnover associated with proliferation of tumor cells. Our patient made the unusual decision to remain on active surveillance even after MP-MRI and TRUS/MRI fusion guided biopsy demonstrated Gleason 3+4 disease. Eighteen months later, MP-MRI demonstrated a lesion which was now positive on MR spectroscopy, upgrading the lesion from moderately to highly suspicious for prostate cancer. Subsequent TRUS/MRI fusion guided biopsy and prostatectomy revealed Gleason 4+4 disease, highlighting the ability of MR spectroscopy to predict tumor progression and aggressiveness, even with no increase in PSA. This report demonstrates that MP-MRI in combination with MR spectroscopy may help monitor disease progression over time in patients on active surveillance.
Abbreviations
- MP-MRI
Multi-parametric MRI
- TRUS/MRI
MR-transrectal ultrasound
- PSA
Prostate-specific antigen
- MR
Magnetic resonance
- DCE
Dynamic contrast-enhanced
References
- 1.Rais-Bahrami S, et al. Utility of multiparametric magnetic resonance imaging suspicion levels for detecting prostate cancer. J Urol. 2013;190(5):1721–7. doi: 10.1016/j.juro.2013.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cancer facts and figures. American Cancer Society; 2013. [Google Scholar]
- 3.Weissbach L, Altwein J. Active surveillance or active treatment in localized prostate cancer? Dtsch Arztebl Int. 2009;106(22):371–6. doi: 10.3238/arztebl.2009.0371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turkbey B, et al. Prostate cancer: can multiparametric MR imaging help identify patients who are candidates for active surveillance? Radiology. 2013;268(1):144–52. doi: 10.1148/radiol.13121325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turkbey B, Pinto PA, Choyke PL. Imaging techniques for prostate cancer: implications for focal therapy. Nat Rev Urol. 2009;6(4):191–203. doi: 10.1038/nrurol.2009.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verma S, Rajesh A. A clinically relevant approach to imaging prostate cancer: review. AJR Am J Roentgenol. 2011;196(3 Suppl):S1–10. doi: 10.2214/AJR.09.7196. Quiz S11-4. [DOI] [PubMed] [Google Scholar]
- 7.Daar D, et al. Prostate Multiparameter MR Imaging. Radiologic Technology. 2011;82(6):563MR–568MR. [PMC free article] [PubMed] [Google Scholar]
- 8.Moore CM, et al. Image-Guided Prostate Biopsy Using Magnetic Resonance Imaging– Derived Targets: A Systematic Review. European Urology. 2013;63(1):125–140. doi: 10.1016/j.eururo.2012.06.004. [DOI] [PubMed] [Google Scholar]