Abstract
Background
Most of the harm from marijuana use is experienced by daily users. Despite this, there has not been a detailed prospective description of daily marijuana use.
Methods
We recruited daily marijuana users (n=142) by internet ads, Craigslist, flyers, etc. Participants were mostly women (58%) with a mean age of 33 and 47% were minorities. Participants called an Interactive Voice Response phone system to report marijuana and other drug use daily for 3 months.
Results
Participants averaged using marijuana 3.2 times per day. Almost all participants used multiple modes of delivery during the study. Bongs/vaporizers/pipes was the most common mode of use (45% of uses). Day-to-day variability in amount of use was relatively small. The median rating of intoxication was 3.8 on a 0-6 scale with no intoxication reported on 1% of days and severe intoxication on 24% of days. The large majority binge drank (71%) or used tobacco (73%). Fifteen during-study variables were associated with the frequency of marijuana use; running out of marijuana and social setting were the strongest correlates. Retrospective reports of “usual” use at study entry were often significantly different than daily reports of use during the study.
Conclusions
This is the first detailed prospective description of daily marijuana use. Most users used multiple times/day, used multiple modes to administer marijuana, were often intoxicated, and under-reported high rates of using alcohol and tobacco. The frequency of marijuana use was especially influenced by social factors. These results will help future studies better describe daily marijuana use.
Keywords: cannabis, drug substitution, intoxication, marijuana, natural history
1. Introduction
Marijuana is the most widely used illicit drug (www.samhsa.gov/data/NSDUH). Most of the physical and behavioral harm, dependence, and treatment seeking associated with marijuana use comes from daily users (Gordon A.J., Conley J.W, & Gordon J.M, ). The most recent US national survey estimates there are 5 million daily marijuana users (www.samhsa.gov/nsduh). Among yearly users of marijuana, 14% were daily or near-daily users (SAMHSA, 2008). The number of daily users in the US appears to be increasing as indicated by reports that the prevalence of dependence on marijuana (Stinson, Ruan, Pickering, & Grant, 2006; Compton, Grant, Colliver, Glantz, & Stinson, 2004) and the number seeking treatment for marijuana dependence (Office of Applied Statistics, 2007) have increased dramatically. In addition, the increased availability of marijuana due to legalization is likely to result in more daily users.
Typically, the first step in studying a behavior is to obtain a detailed description of the behavior; however, descriptions of daily marijuana use are limited (Temple, Brown, & Hine, 2010). There have been several large prospective studies that have revealed important information on how marijuana use changes over a lifetime (Kandel & Raveis, 1989; Chen & Kandel, 1998; Chen, Kandel, & Davies, 1997; Halikas, Weller, Morse, & Hoffmann, 1984; Swift, Hall, & Copeland, 2000; VonSydow et al., 2001; Aitken, DeSantis, Harford, & FeCaces, 2000; Hammer & Vaglum, 1990). These were studies of infrequent young adult users who were surveyed at 3-6 month intervals and focused on change occurring over intervals of several years. These studies only reported on “usual use” during the last several months. None provided a detailed description of day-byday use and none reported on use by daily marijuana users.
Surprisingly, we could only locate one study that quantified day-to-day use of marijuana among heavy users. This study examined 49 college students that used marijuana 5-6 times/week over a 2 week period (Buckner, Crosby, Silgado, Wonderlich, & Schmidt, 2012). It found marijuana use was greatest in the evening and when others were using marijuana, but was not greater on the weekends. Marijuana use was also associated with high craving and anxiety ratings.
We recently completed a study of changes in marijuana use among daily users who were contemplating reducing or quitting sometime in the next 3 months. On the large majority of days of the study, these users were not trying to change their marijuana use; thus, we thought that, before describing the changes in marijuana use, it would be helpful to provide a detailed description of marijuana use on such days for several reasons. For example, because of the multiple modes of administration of marijuana (e.g. blunts, bongs, joints, vaporizers, waterpipes) and the multiple topographies of marijuana use (e.g. depth of inhalation, sharing with others), it is difficult to know how to best measure marijuana use (Mariani, Brooks, Haney, & Levin, 2011; Cooper & Haney, 2009; Gray, Watson, & Christie, 2009). A detailed prospective description of real-world marijuana use that examined issues such as how often users used different modes of administration and how often they changed modes would be helpful both to understanding the consequences of marijuana use but also in designing treatments (Temple et al., 2010). Also, assessing whether daily users are likely to be more intoxicated and use other drugs would be of use. Finally, discovering the events that are associated with heavier use would be useful in designing treatment interventions. Although some of the above information has been described in retrospective reports of daily users in research studies, a prospective study of real-world use could provide a more valid and accurate measure of outcomes among daily users. To accomplish this, the current analyses focused on 1) the frequency,, modality (e.g., joints vs. bongs) and variability of marijuana use, 2) possible causes of variability in use, 3) degree of intoxication and 4) concordance of retrospective reports of “usual” use compared to prospective daily reports of marijuana use. We focused on different modalities because recent reports suggest a growing variety of modes of use, and that different modes may differ in marijuana intake; e.g. blunts appear to deliver more delta(9)-tetrahydrocannabinol than joints (Cooper & Haney, 2009). We focused on causes of variability in use and intoxication levels because we could not locate prior studies of either among ongoing marijuana smokers. We also focused on the validity of recall of drug use because studies among tobacco users suggest such recall is poor(Shiffman et al., 1997).
2. Methods
2.1. Study Design
This a secondary analysis of a study whose primary aim was to describe attempts to change marijuana use among daily users and the study was designed to optimize that aim (the main analysis about changes has not been published). This secondary analysis was a natural history description and like most such analyses(Klingemann et al., 2001) did not have firm a priori hypotheses. We recruited daily marijuana users to a 3-month prospective, non-treatment study. Because the major aim of the study was to describe changes in marijuana use, participants had to state they probably or definitely intended to reduce or stop use at some point in the next 3 months. However, we found that, on the large majority of days (74%) during the study, participants were not trying to reduce or quit providing an opportunity to describe routine daily use among daily users.
Participants initially completed a survey on their “usual” use pattern and then called an Interactive Voice Response (IVR) system each morning to report the prior day's marijuana use, intentional and non-intentional reduction or abstinence, intoxication level, circumstances that might be related to amount of use, mood, craving, and alcohol, tobacco, and illegal drug use. No in-person visits were required and no treatment was provided. All participants provided verbal consent. The University of Vermont Committees on the Use of Human Participants approved the study and the study was registered at www.clinicaltrials.com (NCT01039415).
2.2. Recruitment
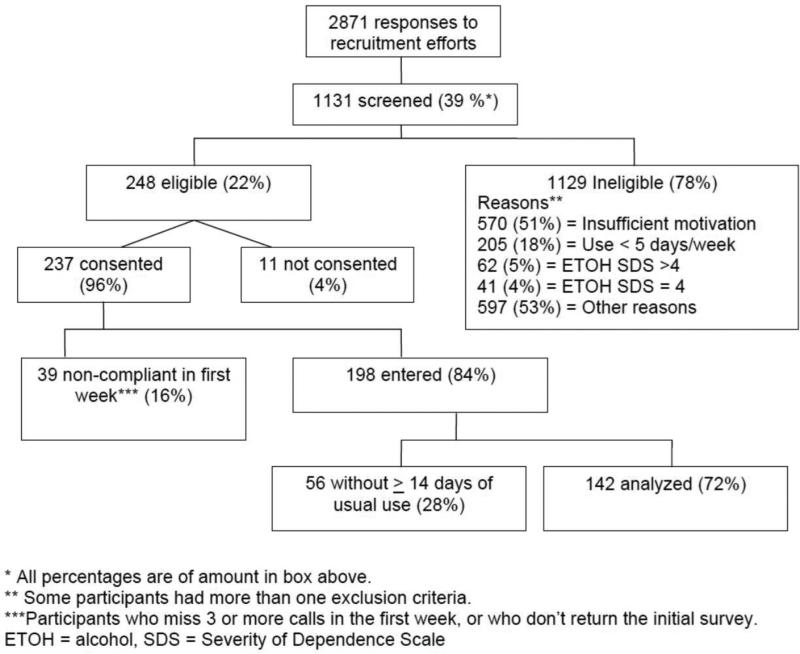
Major inclusion criteria were a) ≥ 18 years old, b) using marijuana at least 5 of 7 days/week, c) scored < 3 on the Severity of Dependence Scales (SDS) (Lawrinson, Copeland, Gerber, & Gilmour, 2007) for dependence on alcohol and non-marijuana illicit drugs, d) stated probably or definitely will try to reduce or stop marijuana use at some point in the next 3 months, and e) had no pending legal actions. The most common reason for exclusion was not stating they either probably or definitely would try to reduce or quit in the next 3 months (Figure 1). Almost all of those eligible consented.
Figure 1.
Participant Flow
Participants were recruited from throughout the US between 1/1/10 and 3/27/12. We recruited participants by notices the on-line bulletin board www.craigslist.com (30% of those enrolled), internet ads (23%), participant referrals (16%), flyers (8%), bus ads (3%) and newspaper ads (2%). A typical ad statement was “Thinking of reducing or quitting marijuana use? You are wanted for a research study. Marijuana users needed for multiple phone interviews. Compensation is available. No treatment is provided. This is a NIH funded research study.” Our target sample size of 200 was based on the ability to accurately estimate incidence rates of various events. A sample of 200 would produce a 95% confidence interval of ± 7% or less, depending on the incidence rate (Fleiss, 2003).
Of the 237 who were eligible and consented, 39 were dropped from the study because they were initially noncompliant (i.e., missed ≥ 3 calls in the first week). To obtain a sufficient sample of both weekdays and weekend days we required ≥ 14 days in which participants were not trying to change. This excluded another 56 participants (e.g. those who were abstinent most of the study); thus, 142 (60% of those consented) provided data for the current analysis. Those excluded were more likely to be men (62% vs. 42%, p < .05), White (73% vs. 53%, p < .05) and had less intention to quit (59% vs. 32% endorsed probably rather than definitely planning to quit, p < .05). None of these differences were associated with frequency of marijuana use (see below).
2.3 Sample Characteristics
Participants completed baseline information via a website or paper questionnaires. Participants were evenly distributed between men and women, minorities and Whites, and employed and unemployed (Table 1). Few were married and most had post-high school education. At study entry, participants stated they usually used marijuana 6 days/wk (median), and on the days they used, averaged 4 (median) times used/day. Few reported using marijuana for medical reasons (11%), or having been in treatment for marijuana problems (11%). Half stated they “usually” used joints (53%), blunts (51%), or pipes (55%) weekly, and fewer reported using bongs (32%), vaporizers (6%) or marijuana substitutes (3%) weekly.
Table 1.
Participant Characteristics in the Current Study Compared to Other Populations of Daily Marijuana Users
| Current study | Ambivalent users | Population-based users | Real world treatment seekers | Treatment research volunteers | ||
|---|---|---|---|---|---|---|
| (n = 142) | MJ Check-Up, 2007 (n=587) | 2010 NSDUH (n= 1323) | 2010 TED clients (n = 10,698) | MJ Tx Project, 1997 (n = 360) | Kadden, 2007 (n = 240) | |
| Mean age | 33 | 30 | - | 36 | 33 | |
| % Women | 58 | 25 | 30 | 49 | 32 | 29 |
| % ≤ HS education | 29 | 51 | 85 | - | - | |
| % Married | 14 | 24 | 12 | 40 | 55 | |
| % Minority | 47 | 16 | 32 | 62 | 30 | 40 |
| % Employed | 48 | 68 | 17 | 83 | 73 | |
| Age of onset of mj use | 15 | 15 | 15 | - | - | |
| Times used/day | 4 | 3 | - | - | 4.5 | 4.5 |
| % Mj abuse or | 80 | 22 | 91 | 100 | 100 | |
| dependence* | ||||||
HS = high school, MJ = marijuana, Tx = treatment, NSDUH = National Survey on Drug Use and Health, TED = Treatment Episode Data Set
Samples varied on criterion for abuse/dependence
Most (63%) met criteria for DSM-IV cannabis dependence using a self-report version of the DSM checklist (Hudziak et al., 1993) and a few more (11%) met criteria for cannabis abuse only (American Psychiatric Association, 2000). Most (80%) scored ≥ 3 (i.e., above recommended cut off) on the SDS (Swift, Copeland, & Hall, 1998) when applied to marijuana. The mean rating of addiction to marijuana was 6.7 (sd = 2.5) on a 0-10 scale (0 = not at all addicted, 10 = very addicted) similar to a scale validated for use in tobacco smokers (Hughes, Keely, Fagerstrom, & Callas, 2005). The mean number of problems on the Cannabis Problems Scale (CPS) (Stephens, Roffman, & Curtin, 2000) was 6.4 (4.5) out of a possible 18 problems.
Upon study entry, 9% stated they had five or more alcoholic drinks on one occasion (i.e., binge drank) at least monthly. Half of participants reported they were current cigarette smokers (55%; 42% daily and 13% nondaily smokers). A quarter (23%) were former smokers, and a quarter (23%) were never-smokers. Few (15%) stated they had used a non-marijuana illegal drug in the last 3 months.
To interpret the generalizability of our sample, we obtained descriptions of daily marijuana users in a) a study of users who were considering changing their marijuana use (Stephens, Roffman, Fearer, Williams, & Burke, 2007), b) daily marijuana users from National Survey of Drug Use and Health (www.nsduhweb.rti.org), c) treatment seekers from the Treatment Episodes Data Set (www.dasis.samhsa.gov), and d) research volunteers from the two largest prior randomized controlled trials on marijuana treatment of users committed to quitting (Marijuana Treatment Project Research Group, 2003; Kadden, Litt, Kabela-Cormier, & Petry, 2007) (Table 1). Our sample appeared to have a similar age, minority prevalence, age of onset, frequency of marijuana use, and prevalence of marijuana dependence to most comparisons samples. However, our sample appeared to have fewer men, fewer with a high school education or less, fewer married, and fewer employed than most comparison samples.
3. Measures
3.1. Interactive Voice Response (IVR)
Participants called an IVR system by phone each morning to report marijuana and other drug use for the prior day. The IVR is a system in which participants respond to phone questions by entering data using the phone keypad (Corkrey & Parkinson, 2002). IVR has many of the assets of computer-assisted telephone interviewing; e.g., automatic skips, branching options, prohibition of illogical responses and outliers, standardized questioning, and direct data entry. Drug use outcomes are more validly reported in IVR compared to phone interviews, computer assessments, written questionnaires or in-person interviews (Aquilino, 1992; Kobak et al., 1997). Daily reporting via IVR appears to produce little reactivity (Hufford, Shields, Shiffman, Paty, & Balabanis, 2002);(Hughes et al., 2013; Helzer, Badger, Rose, Mongeon, & Searles, 2002).
How best to quantify marijuana use is unclear (Zeisser et al., 2012; Gray et al., 2009). On every day of the first week, the IVR initially stated, “Every day we will ask you about your marijuana use. We will ask you both about your times of use and about the total number of joints. A time of use can be long or short but has to be separated from the previous time of use by at least one hour. The number of joints is the total number you smoked all day no matter how many times of use you had. If you use marijuana substitutes like K2, Spice, or Mr. Nice Guy, please count this as marijuana use and include it when you report the number of times you used marijuana and when you report the total number of joints, pipes, or bowls” We chose “times” of use because the largest studies of daily users (e.g., the Marijuana Treatment Project); (Stephens, Babor, Kadden, & Miller, 2002) suggest this is a valid measure. Participants were asked about blunts, bongs/pipes /vaporizers/waterpipes (any of these), and foods containing marijuana they used. Participants were also asked about nine events (e.g., seeing someone use – yes/no) and six internal states (e.g., anxiety – some or a lot vs. none or little) that might predict use of marijuana, as well as the number of alcoholic beverages and cigarettes they used each day. The events and internal states were chosen based on our review of the literature (Lee, Neighbors C., Hendershot, & Grossbard, 2009) and our own experience in interviewing daily marijuana users and are listed in Table 2. An example of an event question is “Yesterday, did you see someone else use marijuana?” with a yes/no response. An example of an internal state question is “How sad or depressed were you yesterday?” with ratings of not all, a little, some, a lot. Endorsement of the last three options was classified as a yes.
Table 2.
Significant Correlates of Greater Number of Times Used Marijuana
| Predictor | Median percent of days | Times used MJ on day of occurrence | Times used MJ on day of non-occurrencea | t statistic from multilevel linear regression |
|---|---|---|---|---|
| Events | ||||
| At a party | 6 (2, 16) | 3.5 (2.6, 4.6) | 3.1 (2.3, 3.9) | 11.91 ** |
| Binge drinking (n=86) | 6 (2, 13) | 3.2 (2.6, 4.8) | 3.1 (2.4, 3.7) | 10.20 ** |
| Concerns about cost of MJ | 5 (1, 22) | 3.0 (2.4, 4.0) | 3.1 (2.4, 4.1) | −2.41 * |
| Offered marijuana | 30 (12, 57) | 3.3 (2.5, 4.2) | 2.9 (2.1, 3.6) | 14.91 ** |
| Ran out of MJ | 6 (1, 13) | 2.6 (1.9, 3.2) | 3.2 (2.4, 4.1) | −15.34 ** |
| Seeing someone using | 66 (28, 92) | 3.2 (2.5, 4.1) | 2.6 (1.8, 3.5) | 15.02 ** |
| Used alcohol (n=129) | 21 (8, 46) | 3.3 (2.3, 4.3) | 3.0 (2.2, 3.8) | 10.58 ** |
| Using with someone | 61 (25, 91) | 3.2 (2.6, 4.2) | 2.6 (1.8, 3.3) | 15.25 ** |
| Weekend | 43 (41, 45) | 3.1 (2.4, 4.1) | 3.0 (2.2, 3.8) | 7.57 ** |
| Internal States (none vs any) | ||||
| Anger | 21 (8, 44) | 3.0 (2.2, 3.9) | 3.1 (2.4, 4.0) | −3.94 * |
| Anxiety | 21 (5, 55) | 3.0 (2.2, 3.9) | 3.1 (2.3, 4.1) | −2.05 * |
| Craving | 96 (85, 100) | 3.1 (2.4, 4.1) | 2.8 (2.0, 4.0) | 4.96 ** |
| Sadness | 21 (6, 53) | 3.0 (2.2, 3.7) | 3.1 (2.4, 4.0) | −3.86 ** |
| Hunger | 83 (58, 95) | 3.1 (2.4, 4.0) | 2.9 (2.0, 4.0) | 6.15 ** |
| Sleep problems | 27 (9, 48) | 3.0 (2.3, 3.8) | 3.1 (2.3, 4.0) | −2.39 * |
Medians (25th and 75th percentiles). Retained subsets of participants for drinking and binging.
p values for difference in marijuana use on days of occurrence vs. non-occurrence ofevent
p < .05
p < .001
p < .001
MJ = marijuana
Participants were reimbursed $2 for daily IVR completion plus a $10 bonus if they completed all IVR calls in a week. They also received $75 for completion of questionnaires. The total maximum amount available was $363.
4. Data Analysis
All descriptive summary statistics (e.g. percents) were calculated by first averaging within participants, and then averaging across participants, so that each participant provided the same amount of data. Multilevel models were used to account for the difference in within- vs. between-participant variability. Missing data was not imputed. Most of the outcomes had skewed distributions; thus, we report medians and non-parametric statistical tests. The analyses used SAS version 9 (SAS Institute, Cary, NC).
5. Results
5.1. Compliance
Among the 142 participants in the current analysis, the incidence of missing data was 8%, and the incidence of dropouts (i.e. did not provide data in the last week of the study) was 5%. Comparable rates among the 198 who entered the study were 16% and 13%.
5.2. Reactivity
Self-monitoring can cause “reactivity;” i.e., a decrease in reports of a behavior (Korotitsch & Nelson-Gray, 1999). The median number of times marijuana was used in the first week of the study on days participants were not trying to change was lower than the number of times of use in a “usual” week reported on the baseline survey (3.4 vs. 4.1 times used/day, Wilcoxon signed rank test, p = 003). We do not know if this reduction represents reactivity, inaccurate reporting of “usual” number of times used, or unreported attempts to reduce.
5.3. Patterns of Marijuana Use
Participants reported use without an attempt to change on 62% of days, and of non-intentional reduction (e.g. due to non-availability of marijuana) on 12% of days; thus, a total of 74% of days (i.e., a median of 73.5 days) were included in the current analysis. The remaining days were excluded due to intentional reduction (13%), intentional abstinence (9%), and non-intentional abstinence (3%).
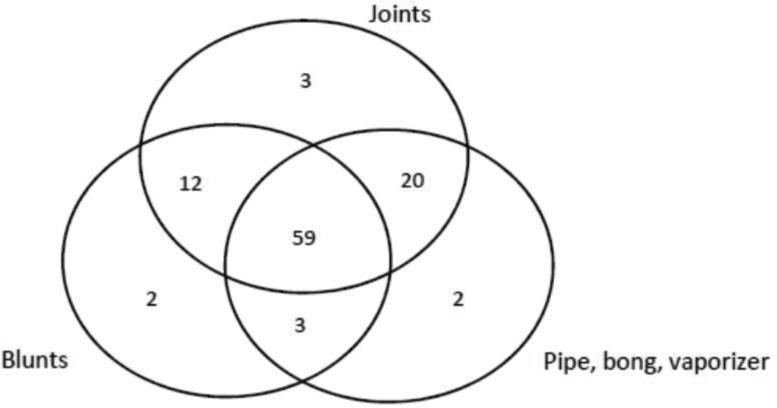
The median number of times used/day was 3.0 (2.2-3.8) and 83% users averaged ≥ 2 times used/day. The number of times used/day declined slightly over the 84 days of the study from 3.4 during the first week to 3.0 during the last week (multilevel regression p < .0001). Marijuana use was slightly greater on weekend than weekdays (Table 2). Almost all participants used different modes of marijuana administration during the study and joints were not the most common mode of administration. For example, 59% used all three modes during the study while less than 3% used only joints or only blunts (Figure 2) . Overall 7% used only one mode during the study, 25% used two modes, and 59% used three modes or more. Participants used pipes/bongs on a median of 49% of days, blunts on 33% of days, and joints on 16% of days. African Americans were more likely to use blunts than Whites (72% vs. 20% of days; ANOVA, F= 11.0, p < .0001). The median number of times used/day of bongs/pipes was 2.5 day (1.7-3.7), of joints was 2.0/day (1.3-3.1), of blunts was 2.2/day (1.5-3.3). The daily sum of the number of times used of bongs/pipes, blunts, joints and food on a usual use day was equal to 74% of the number of “times” used, indicating some “times of use” included multiple modes of administration. The median within-participant standard deviation in the number of times used was 1.1; thus, on 68% of the days, the number of times used differed from the mean by ≤ 1.1 times used.
Figure 2.
Percent of participants who used a single mode of marijuana administration or used different modes during the study. The subsets are mutually exclusive.
5.4. Intoxication/High Scores
On days when marijuana was used, the median high score was 3.8 (3.2, 4.6) on a 0-6 scale with 0 = “did not get high” and 6 = “got very high”; i.e., on 50% of days, users reported a score of ≥ 3.8. The median incidence of days of little intoxication (rating = 0 or 1) was 1% and of days of severe intoxication (ratings = 5 or 6) was 24%. Higher intoxication scores were associated with greater times of use/day (multilevel regression p < .0001, median within-participant correlation = .40) and greater number of modes of administration used/day (median correlation = .41, p< .0001), suggesting equal validity of these two measures. Average intoxication scores were greater in those with higher SDS for marijuana scores (univariate regression, r = .20, p = .03), higher self-reported addiction scale scores (r= .26, p = .006), and higher baseline marijuana intake (r = .19, p=.05). Intoxication scores were higher on days participants used blunts than on days they used joints or pipes (4.3 vs. 3.7, multilevel regression p < .0001) and on days they used any alcohol (4.1 vs 3.7, multilevel regression, p < .0001) or binge drank (4.4 vs 3.9, multilevel regression, p < .0001). Among daily tobacco smokers, intoxication scores were higher on smoking than non-smoking days (3.9 vs 3.5, multilevel regression, p < .0001) and increased with increased cigs/day (+0.05/cigarette; multilevel regression, p < .0001).
5.5. Use of Other Drugs
Almost all (91%) of participants consumed alcohol during the study and those who did, drank alcohol on 21% of days with a median number of 2.7 drinks (2.0-3.8) on a day of drinking. Most (72%) alcohol users binge drank (≥ 5 drinks for men and ≥ 4 drinks for women) at least once during the study and 30% binged monthly. Most participants (73%) smoked tobacco during the study. Among those who smoked, 42% were non-daily smokers. Among daily smokers, the median cigs/day was 9.6 (5.9, 16.9). Smoking was more common among primary blunt/joint users (chi-square = 7.7, p <.02). One-third (33%) of participants reported use of ≥ 1 non-marijuana illicit drug during the 3 months of the study, but only 9% used illicit drugs ≥ 5 times during the study
5.6. Prediction of Number of Times of Use
None of the baseline demographic variables (see Table 1) predicted the number of times used. Among the other baseline variables, age of onset, number of marijuana problems, number of friends using, partner use, social use, use for medical reasons, and support for legalization of marijuana did not predict frequency. Self-rated and DSM-defined dependence, and ease of obtaining marijuana predicted greater times of use (all p's < .05). None of the alcohol use nor mood variables predicted frequency, but tobacco smokers used marijuana less frequently (2.9 vs. 3.2 times used/day; F= 4.9, p < .05).
In contrast, all 15 variables collected daily during the study were associated with times used (multilevel univariate regressions; all p's < .05) (Table 2). Running out of marijuana and seeing someone using marijuana appeared to be the strongest correlates, followed by using with someone, being at a party, and being offered marijuana. In a multilevel multivariate regression testing which variables were associated with times used independent of other variables, eight variables; (i.e., the above five variables plus drinking alcohol, anxiety, and craving) remained as significant correlates.
6. Discussion
Most daily marijuana users used marijuana multiple times/day and half used more than 3 times/day. The large majority of marijuana natural history, epidemiological and treatment studies report only the number of joints being used; however, the large majority of daily users in our study used multiple modes of administration and joints, in fact, were not the most commonly used mode of administration. In addition, social factors and availability were the two most powerful predictors of marijuana which is consistent with the one prior detailed prospective study(Buckner et al., 2012) Marijuana use was slightly greater on weekends than weekdays in the current study, which is inconsistent with the prior study.
To our knowledge, this is the first study to assess daily levels of intoxication from marijuana. Most of our daily users were chronically intoxicated; i.e., they do not appear to have developed substantial tolerance to intoxication effects. This suggests many, if not most, daily users are likely to have impaired cognitive function and decision making on a daily basis (Crean, Crane, & Mason, 2011). Consistent with retrospective studies(Timberlake, 2009) Use of blunts was associated with greater intoxication that use of joints. Although this appears to contradict a laboratory study that found with similar weights of marijuana, intoxication was greater with joints that blunts (Cooper & Haney, 2009). However, blunts typically contain more marijuana than joints (Mariani et al., 2011), and this may be the reason for their association with greater intoxication.
Almost all participants used alcohol, and users averaged 4-5 alcoholic drinks/week, which is identical to recent national survey data for alcohol users (Saad, 2012). During the study about 30% of participants binge drank monthly which does not appear to be higher than the national average for adults in this same age range (28%) (Kanny, Liu, Brewer, Lu, & Centers for Disease Control and Prevention (CDC), 2013). Non-marijuana illicit drug use was uncommon, probably due to our inclusion criteria.
About 3/4ths of our daily users smoked tobacco during the study, which is similar to that seen with heavy users of other illicit drugs(Peters, Budney, & Carroll, 2012). However, among those who smoked, only 60% were daily smokers and these daily smokers averaged 10 cigs/day, both of which are less than among US adult smokers (King, Dube, & Tynan, 2012). There are several plausible hypotheses about why the prevalence of tobacco smoking is so high among dailymarijuana users (e.g. similar routes of administration, and offsetting of sedating effects of marijuana); however, empirical tests of these are lacking (Peters et al., 2012). Since, tobacco smoking is likely a major cause of morbidity among marijuana users and is associated with decreased cessation of marijuana(Peters et al., 2012), further research into the overlap of tobacco and marijuana use is indicated.
The use of alcohol and cigarettes during the study was much greater than the “usual” use reported at study entry. For example, at study entry, only 9% reported monthly binge drinking, but 72% binged during the 3-month study; 55% stated they were current tobacco smokers, but 73% smoked during the study; and also at study entry; 15% stated they used an illegal drug in the last 3 months, but 33% used during the 3 month study. These results suggest retrospective report of “usual” use of drugs can be quite inaccurate. Similar results have been found for tobacco use (Shiffman, 2009).
Several during-study variables predicted increased marijuana use; however, the magnitude of most of these effects was small (difference of ≤ 0.4 times used/day). The stronger correlates were running out of marijuana, seeing someone use marijuana, and using with someone. This result confirms prior retrospective reports that social influences are prominent in determining the amount of marijuana use (Buckner et al., 2012).
One possible liability of our study is that the daily monitoring appeared to suppress marijuana use. We believe this may not be the case because the effect occurred immediately (i.e., within the first week) which is different from most reactivity effects (Korotitsch & Nelson-Gray, 1999). Also, the difference in baseline vs, during study use may be due to overestimating usual use at baseline rather than reactivity per se or intentional reductions during study.. Another liability of the current study was its use of a convenience sample. Although the sample was similar to national samples of daily users on many demographic and use characteristics, it did have substantially fewer men and fewer less-educated participants than most comparison samples of daily users. Also, our participants were daily marijuana users who were planning to reduce or quit at some point in the next 3 months and who were not currently dependent on alcohol or non-marijuana illicit drugs. Clearly our sample was not representative. Unfortunately, we a priori lumped bongs, pipes, vaporizers and waterpipes together because at study onset we were not aware each was so prevalent. We also did not collect data on co-administration of marijuana with other drugs. Our results are based on prospective prediction and although such associations are more likely to be causal than cross-sectional or retrospective associations, they still may not represent a causal relationship. For example, the variables in Table 2 could be consequences rather than causes of increased marijuana use. Non-substance use psychiatric comorbidity is common among heavy marijuana users (Satyanaravana, 2009); however, we did not measure this in our sample. Finally, we did not collect biological samples to verify levels of use. The major assets of our study were the use of non-treatment seeking sample, the prospective design, the small amount of missing data, and the multiple data points for each participant
Our study has several possible implications. First, since daily marijuana users are quite heavy users and are often intoxicated, they are a group that should be targeted for interventions. Second, since almost all daily users used multiple modes of administration, future clinical and epidemiological descriptions need to include measures of multiple modes to adequately describe use patterns and outcomes. Third, since “times used” was as correlated with intoxication levels as number of different modes of administration used, it may be thought of as a simpler, more easily operationalized quantity measure than asking about the six different modes of administration. On the other hand, since blunts were associated with greater intoxication levels, future studies of the relative speed of onset and maximum level of THC across the modes of administration is needed to determine if exposure to marijuana constituents differs across modes. Fourth, since the use of alcohol and tobacco during the study was significantly greater than that reported as “usual,” future studies may want to use prospective or retrospective Time-Line Follow-Back procedures(Sobell, Brown, Leo, & Sobell, 1996) to obtain a more accurate measure of their use. Fifth, our finding that social factors were the most important factors in determining marijuana use replicates earlier work with less-heavy users(Chen & Kandel, 1998) and suggests that, even with the progression to daily marijuana use, much use continues to be occurring in social settings. Finally, since we had little missing data and since there appeared to be little reactivity with daily monitoring, this suggests the feasibility of further prospective natural history studies of subsets of marijuana users.
In summary, our major findings are that daily marijuana users a) use multiple times each day, b) use multiple modes of administration (not just joints), c) are often intoxicated, d) have high rates of tobacco use, e) are often influenced by social cues to use and f) underreport alcohol and tobacco use. Since this is one of the first intensive studies of daily marijuana use, replications are needed, including replications in a more generalizable sample and among less heavy marijuana users and users not contemplating changing.
Highlights.
Most daily marijuana users use multiple methods of delivery
Most report significant daily intoxication
Most binge drank and were tobacco smokers
Replication in a more generalizable sample is needed
Acknowledgment
Xxx assisted in the conduct of the study.
Role of funding sources
Funding for this study was provided by grant DA024591 from the US National Institute on Drug Abuse. The sponsor had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
JRH, AJB, designed the study and wrote the protocol. JRF collected the data and JRF, PC conducted data analysis. JRH wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Conflict of interest: None
Contributor Information
John R. Hughes, Departments of Psychiatry, Psychology and Family Practice, University of Vermont, Burlington; VT 05405.
James R. Fingar, Department of Psychiatry, University of Vermont, Burlington, VT 05405.
Alan J. Budney, Department of Psychiatry, Geisel School of Medicine at Dartmouth, Lebanon, NH 03766
Shelly Naud, Department of Medical Biostatistics, University of Vermont, Burlington, VT 05405.
John E. Helzer, Department of Psychiatry, University of Vermont, Burlington, VT 05405; Peter W. Callas, Department of Biostatistics, University of Vermont, Burlington, VT 05405.
Reference List
- Aitken SS, DeSantis J, Harford TC, FeCaces M. Marijuana use among adults. A longitudinal study of current and former users. Journal of Substance Abuse. 2000;12:213–226. doi: 10.1016/s0899-3289(00)00051-1. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition, Text Revision American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Aquilino WS. Telephone versus face-to-face interviewing for household drug use surveys. International Journal of Addiction. 1992;27:71–91. doi: 10.3109/10826089109063463. [DOI] [PubMed] [Google Scholar]
- Buckner J, Crosby R, Silgado J, Wonderlich S, Schmidt N. Immediate antecedents of marijuana use: An analysis from ecological momentary assessment. Journal of Behavior Therapy and Experimental Psychiatry. 2012;43:647–655. doi: 10.1016/j.jbtep.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K, Kandel DB. Predictors of cessation of marijuana use: An event history analysis. Drug and Alcohol Dependence. 1998;50:109–121. doi: 10.1016/s0376-8716(98)00021-0. [DOI] [PubMed] [Google Scholar]
- Chen K, Kandel DB, Davies M. Relationships between frequency and quantity of marijuana use and last year proxy dependence among adolescents and adults in the United States. Drug and Alcohol Dependence. 1997;46:53–67. doi: 10.1016/s0376-8716(97)00047-1. [DOI] [PubMed] [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States. 1991-1992 and 2001-2002. Journal of the American Medical Association. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- Cooper Z, Haney M. Comparison of subjective, pharmacokinetic, and physiological effects of marijuana smoked as joints and blunts. Drug and Alcohol Dependence. 2009;103:107–113. doi: 10.1016/j.drugalcdep.2009.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corkrey R, Parkinson L. nteractive voice response: Review of studies 1989-2000. Behavior Research Methods, Instruments & Computers. 2002;34:342–353. doi: 10.3758/bf03195462. [DOI] [PubMed] [Google Scholar]
- Crean R, Crane N, Mason B. An evidence based review of acute and long-term effects of cannabis use on executive cognitive functions. Journal of Addiction Medicine. 2011;5:1–8. doi: 10.1097/ADM.0b013e31820c23fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleiss J. Statistical Methods for Rates and Proportions. 3rd ed. Wiley-Interscience; Hoboken, NJ: 2003. [Google Scholar]
- Gordon AJ, Conley JW, Gordon JM. Medical consequences of marijuana use: A review of current literature. Current Psychiatry Reports 15. doi: 10.1007/s11920-013-0419-7. [DOI] [PubMed] [Google Scholar]
- Gray K, Watson N, Christie D. Challenges in quantifying marijuana use. American Journal of Addiction. 2009;18:178–179. doi: 10.1080/10550490902772579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halikas JA, Weller RA, Morse CL, Hoffmann RG. Use of marijuana and other drugs among adult marijuana users: A longitudinal study. Compr Psychiatr. 1984;25:63–70. doi: 10.1016/0010-440x(84)90023-3. [DOI] [PubMed] [Google Scholar]
- Hammer T, Vaglum P. Initiation, continuation or discontinuation of cannabis use in the general population. British Journal of Addiction. 1990;85:899–909. doi: 10.1111/j.1360-0443.1990.tb03720.x. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Badger GJ, Rose GL, Mongeon JA, Searles JS. Decline in alcohol consumption during two years of daily reporting. Journal of Studies on Alcohol. 2002;63:551–558. doi: 10.15288/jsa.2002.63.551. [DOI] [PubMed] [Google Scholar]
- Hudziak JJ, Helzer JE, Wetzel MW, Kessel KB, McGee B, Janca A, et al. The use of the DSM-III-R checklist for initial diagnostic assessments. Compr Psychiatry. 1993;34:375–383. doi: 10.1016/0010-440x(93)90061-8. [DOI] [PubMed] [Google Scholar]
- Hufford MR, Shields AL, Shiffman S, Paty J, Balabanis M. Reactivity to ecological momentary assessment: An example using undergraduate problem drinkers. Psychology of Addictive Behaviors. 2002;16:205–211. [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Fagerstrom K-O, Callas PW. Intentions to quit smoking change over short periods of time. Addictive Behaviors. 2005;30:653–662. doi: 10.1016/j.addbeh.2004.08.011. [DOI] [PubMed] [Google Scholar]
- Hughes J, Solomon L, Fingar J, Naud S, Helzer J, Callas P. The natural history of efforts to stop smoking: A prospective cohort study. Drug and Alcohol Dependence. 2013;128:171–174. doi: 10.1016/j.drugalcdep.2012.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadden RM, Litt MD, Kabela-Cormier E, Petry NM. Abstinence rates following behavioral treatments for marijuana dependence. Addictive Behaviors. 2007;32:1220–1236. doi: 10.1016/j.addbeh.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel DB, Raveis VH. Cessation of illicit drug use in young adulthood. Archives of General Psychiatry. 1989;46:109–116. doi: 10.1001/archpsyc.1989.01810020011003. [DOI] [PubMed] [Google Scholar]
- Kanny D, Liu Y, Brewer BD, Lu H, Centers for Disease Control and Prevention (CDC) Binge drinking - United States, 2011. Morbidity and Mortality Weekly Report Surveillance Summary. 62(Suppl. 3):77–80. (11-22-2013) [PubMed] [Google Scholar]
- King B, Dube S, Tynan M. Current tobacco use among adults in the United States: Findings from the National Adult Tobacco Survey. American Journal of Public Health. 2012;102:e93–e100. doi: 10.2105/AJPH.2012.301002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klingemann H, Sobell L, Barker J, Blomqvist J, Cloud W, Ellinstad T, et al. Promoting Self-Change from Problem Substance Use: Practical Implications for Policy, Prevention and Treatment. Kluwer Academic Publications; Dordrecht, Netherlands: 2001. [Google Scholar]
- Kobak KA, Taylor L. vH., Dottl SL, Greist JH, Jefferson JW, Burroughs D, et al. A computer-administered telephone interview to identify mental disorders. Journal of the American Medical Association. 1997;278:905–910. [PubMed] [Google Scholar]
- Korotitsch WJ, Nelson-Gray RO. An overview of self-monitoring research in assessment and treatment. Psychological Assessment. 1999;11:415–425. [Google Scholar]
- Lawrinson P, Copeland J, Gerber S, Gilmour S. Determining a cutoff on the Severity of Dependence Scale (SDS) for alcohol dependence. Addictive Behaviors. 2007;32:1474–1479. doi: 10.1016/j.addbeh.2006.09.005. [DOI] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, Hendershot CS, Grossbard JR. Development and preliminary validation of a comprehensive marijuana motives questionnaire. Journal of Studies on Alcohol and Drugs. 2009;70(2):279–287. doi: 10.15288/jsad.2009.70.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariani J, Brooks D, Haney M, Levin F. Quantification and comparison of marijuana smoking practices: Blunts, joints, and pipes. Drug and Alcohol Dependence. 2011;113:249–251. doi: 10.1016/j.drugalcdep.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marijuana Treatment Project Research Group Brief treatments for cannabis dependence: Findings from a randomized multi-site trial. Journal of Consulting and Clinical Psychology. 2003;72:455–466. doi: 10.1037/0022-006X.72.3.455. [DOI] [PubMed] [Google Scholar]
- Office of Applied Statistics Treatment Episode Data Set (TEDS) 2007 www.oas.samhsa.gov/teds [On-line]
- Peters E, Budney A, Carroll K. Clinical correlates of co-occurring cannabis and tobacco use: A systematic review. Addiction. 2012;107:1404–1417. doi: 10.1111/j.1360-0443.2012.03843.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saad L. Majority in U.S. drink alcohol, averaging four drinks a week. 2012 http://www.gallup.com/poll/156770/majority-drink-alcohol-averaging-four-drinks-week.aspx [On-line]
- SAMHSA Results from the 2007 national survey on drug use and health; national findings. Substance Abuse and Mental Health Service Administration H-34 No. SMA 08-4343. 2008.
- Satyanaravana V. Mental health consequences of cannabis use. Acta Psychiatrica Scandinavica. 2-8-2009;119:411–412. doi: 10.1111/j.1600-0447.2009.01354.x. [DOI] [PubMed] [Google Scholar]
- Shiffman S. How many cigarettes did you smoke? Assessing cigarette consumption by global report, time-line follow-back, and ecological momentary assessment. Health Psychology. 2009;28:519–526. doi: 10.1037/a0015197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Hufford M, Hickcox M, Paty JA, Gnys M, Kassel JD. Remember that? A comparison of real-time versus retrospective recall of smoking lapses. Journal of Consulting and Clinical Psychology. 1997;65:292–300. doi: 10.1037/0022-006x.65.2.292.a. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Brown J, Leo GI, Sobell MB. Reliability of the alcohol timeline followback when administered by telephone and by computer. Drug and Alcohol Dependence. 1996;42:49–54. doi: 10.1016/0376-8716(96)01263-x. [DOI] [PubMed] [Google Scholar]
- Stephens RS, Babor TF, Kadden R, Miller M. The Marijuana Treatment Project: Rationale, design and participant characteristics. Addiction. 2002;97:109–124. doi: 10.1046/j.1360-0443.97.s01.6.x. [DOI] [PubMed] [Google Scholar]
- Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68:898–908. [PubMed] [Google Scholar]
- Stephens RS, Roffman RA, Fearer SA, Williams C, Burke RS. The Marijuana Check-up: promoting change in ambivalent marijuana users. Addiction. 2007;102:947–957. doi: 10.1111/j.1360-0443.2007.01821.x. [DOI] [PubMed] [Google Scholar]
- Stinson FS, Ruan WJ, Pickering R, Grant BF. Cannabis use disorders in the USA: prevalence, correlates and co-morbidity. Psychological Medicine. 2006;36:1447–1460. doi: 10.1017/S0033291706008361. [DOI] [PubMed] [Google Scholar]
- Swift W, Copeland J, Hall W. Choosing a diagnostic cut-off for cannabis dependence. Addiction. 1998;93:1681–1692. doi: 10.1046/j.1360-0443.1998.931116816.x. [DOI] [PubMed] [Google Scholar]
- Swift W, Hall W, Copeland J. One year follow-up of cannabis dependence among long-term users in Syndey, Australia. Drug and Alcohol Dependence. 2000;59:309–318. doi: 10.1016/s0376-8716(99)00131-3. [DOI] [PubMed] [Google Scholar]
- Temple EC, Brown RF, Hine DW. The ‘grass ceiling’: limitations in the literature hinder our understanding of cannabis use and its consequences. Addiction. 11-11-2010;106:238–244. doi: 10.1111/j.1360-0443.2010.03139.x. [DOI] [PubMed] [Google Scholar]
- Timberlake D. Marijuana a comparison of drug use and dependence between blunt smokers and other cannabis users. Substance Use and Misuse. 2009;44:401–415. doi: 10.1080/10826080802347651. [DOI] [PubMed] [Google Scholar]
- VonSydow K, Lieb R, Pfister H, Hofler M, Sonntag H, Wittchen HU. The natural course of cannabis use, abuse and dependence over four years: A longitudinal community study of adolescents and young adults. Drug and Alcohol Dependence. 2001;64:347–361. doi: 10.1016/s0376-8716(01)00137-5. [DOI] [PubMed] [Google Scholar]
- Zeisser C, Thompson K, Stockwell T, Duff C, Chow C, Vallance K, et al. A ‘standard joint’? The role of quantity in predicting cannabis-related problems. Addiction Research and Theory. 2012;20:82–92. [Google Scholar]