Abstract
Background:
Prevalence of passive smoke exposure is relatively unknown in chronic rhinosinusitis (CRS). Previous studies have attempted to establish this relationship using subjective, questionnaire-based methodologies to assess smoke exposure, thus introducing the potential for error bias. The purpose of this study was to accurately determine the prevalence of passive smoke exposure in CRS and control patients using hair nicotine levels as a quantitative measure of cigarette smoke exposure.
Methods:
Hair samples were obtained at time of surgery from 569 patients: 404 undergoing surgery for CRS and 165 controls undergoing surgery for repair of cerebrospinal fluid leak, removal of pituitary tumors, or adenoidectomy from 2007 to 2013. Patient charts were reviewed for reported smoking status. Hair nicotine was quantified using reversed-phase high-performance liquid chromatography. Nonsmoking patients were classified as passive smoke exposed or smoke naïve according to the hair nicotine results. Statistical analysis was performed to test for differences in demographic information and smoke exposure prevalence between CRS, CRS subtypes, and controls.
Results:
The prevalence of passive smoke exposure in CRS as documented by hair nicotine was lower than previously reported subjective estimates. Passive smoke exposure rates were equivalent between those with CRS versus controls and significantly higher in children. Severity of passive smoke exposure was also equivalent between CRS subsets and controls. Annual passive smoke exposure prevalence did not change over time.
Conclusion:
There is no clear evidence of avoidance of passive smoke exposure in the CRS population compared with controls. Passive smoke exposure also remained stable over time despite recent regional implementation of smoking bans. Given the constancy of exposure, it is critical that the impact of passive smoke on CRS exacerbation, outcomes, and pathophysiology be evaluated in large-scale clinical studies.
Keywords: Chronic rhinosinusitis, hair nicotine, passive smoke, prevalence, quantitative
Chronic rhinosinusitis (CRS) is a disease with significant health, quality of life, and economic consequences. The daily health and quality of life impact of CRS has been shown to be comparable or worse than other chronic conditions such as angina, chronic obstructive pulmonary disease, and chronic back pain.1 CRS is also relatively common, with an estimated incidence in the United States of ∼1130 per 100,000 people/year.2 The etiology of CRS is multifactorial and incompletely understood, but environmental factors, including active and passive smoking, are thought to have a role in disease incidence or severity.3–5
Passive smoke exposure has been evaluated by the U.S. Surgeon General as a cause or exacerbating factor in cardiac, pulmonary, and oncologic diseases for >40 years. It is estimated that 60% of children aged 3–11 years and 40% of nonsmoking adults are exposed to passive smoke, which is known to cause symptoms of nasal irritation.6 Passive smoke exposure has been shown to inhibit upper airway mucociliary clearance,7,8 increase the incidence of sinonasal biofilms,9 promote the sinonasal tissue allergic response,10 and negatively impact sinus surgery clinical outcomes.11,12 Exposure to passive smoke has also been linked to increased incidence and severity of acute and allergic rhinosinusitis.13,14
Prospective, case–control evidence found an independent, dose–response association between self-reported passive smoke exposure and a diagnosis of CRS.15 A large cohort analysis supported this finding and related passive smoke exposure to significantly more severe symptoms of nasal obstruction/blockage, rhinorrhea, headache, and cough and an increased use of nasal decongestants for acute exacerbations.16 It is unclear if patients with CRS made any attempts to avoid passive smoke due to exacerbation of CRS symptoms, or if the severity of disease made them more conscious of the exposure. Also, the prevalence of recent passive smoke exposure in CRS varied widely from 39 to 68.3%. Both studies determined passive smoke exposure through a subjective questionnaire that pools information regarding perceived home, work, and social exposure. This method of evaluating smoke exposure introduces the potential for inaccurate assessment and recall bias that could be resolved with quantitative measurements of smoke exposure.17
Several objective biological markers have been validated as effective measurements of smoke exposure.18 Hair nicotine measurements reliably and reproducibly correlate with subjective accounts, as well as biological and environmental assessments of smoke exposure in nonsmoking subjects, with 1 cm of hair collected nearest the scalp representing 1 month of exposure.19,20,21 The aim of this study was to perform quantitative measurements of hair nicotine to assess the prevalence and severity of passive smoke exposure in CRS compared with controls.
METHODS
Study Design
The Institutional Review Board of the Medical University of South Carolina approved these studies (HR 14124, 18105, 20077, and 19548), and written informed consent was obtained for all patients. Hair samples ∼1–2 cm in length were cut from the postauricular scalp at the time of surgery in patients with CRS and controls. All patients with CRS met diagnostic criteria as defined by the European Position Paper on Rhinosinusitis and Nasal Polyps 20125 and underwent endoscopic sinus surgery at the Medical University of South Carolina between 2007 and 2013. CRS was divided into subgroups: CRS with nasal polyps (CRSwNP) and CRS without nasal polyps (CRSsNP), with allergic fungal rhinosinusitis (AFRS) examined separately. Control patients were undergoing surgery for cerebrospinal fluid leak repair, nonhormone-secreting pituitary tumors, or adenoidectomy. Patients who were known to use nicotine patches were excluded.
Hair samples were analyzed for nicotine at the Wellington Hospital Laboratory in Newton, New Zealand, using reversed-phase high-performance liquid chromatography as previously described.22 Smoking status, active smoker versus nonsmoker, at time of surgery was obtained through the preoperative medical records. Smoke naive patients were defined according to previously published guidelines21 as nonsmoking patients with a hair nicotine measurement of <2.0 ng/mg, and nonsmoking patients with hair nicotine of >2.0 ng/mg were classified as passive smoke exposed. The hair nicotine of active smokers was measured and recorded but was not used to classify exposure because of historic data that details its relative inaccuracy in assessment of active smokers.21
Statistical Analysis
Statistical analysis was conducted using GraphPad Prism 6.0 software (GraphPad Software, La Jolla, CA) and IBM SPSS Statistics for Windows, Version 21.0 (IBM, Armonk, NY). Dichotomous variables were analyzed using χ2. Binary and multinomial logistic regression analyses were used to control for confounding factors in the relationship between smoke exposure and CRS status, including age, sex, and race. Analysis of more than two nonnormally distributed continuous variables was performed using a Kruskal-Wallis one-way ANOVA with Dunn's multiple comparison test. Linear regression was used to obtain 95% confidence interval bands on data presented over time, and analysis for statistical significance of these data was performed using the χ2-test for trend.
RESULTS
Population Characteristics
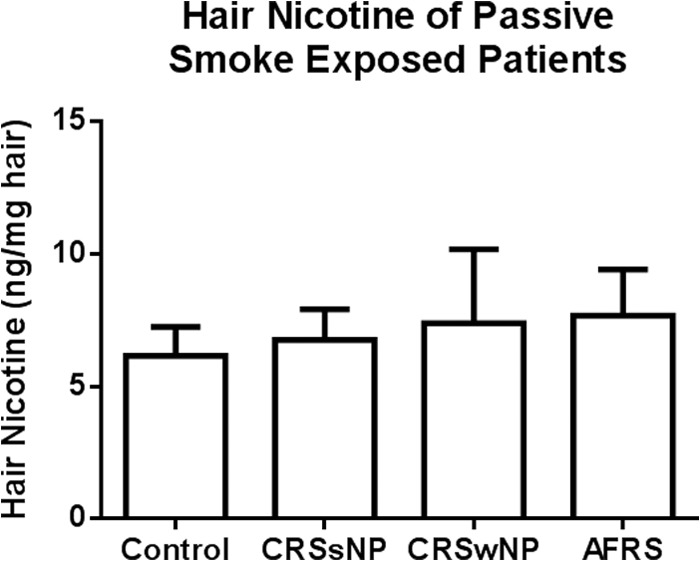
A total of 569 participants were enrolled in the study, including 165 controls, 248 with CRSsNPs, 87 with CRSwNPs, and 69 fulfilling criteria for AFRS. The mean age of all study participants was 41 ± 23 years with 127 of the patients <18 years. CRSsNP and CRSwNP patients tended to be older, control patients younger, and AFRS were the youngest. Control and CRSsNP patients were more likely to be female subjects, and CRSwNP and AFRS patients were mostly male subjects. Control patients were 61% Caucasian, CRSsNP and CRSwNP patients were more likely to be Caucasian, and AFRS patients were more likely to be African American. These differences were statistically significant as described in Table 1 and consistent with the literature.3,23–25
Table 1.
Demographics of patient populations
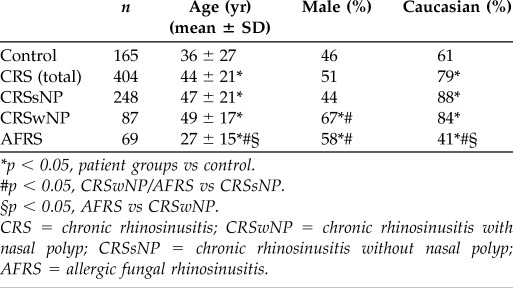
*p < 0.05, patient groups vs control.
#p < 0.05, CRSwNP/AFRS vs CRSsNP.
§p < 0.05, AFRS vs CRSwNP.
CRS = chronic rhinosinusitis; CRSwNP = chronic rhinosinusitis with nasal polyp; CRSsNP = chronic rhinosinusitis without nasal polyp; AFRS = allergic fungal rhinosinusitis.
Passive Smoke Exposure Prevalence and Severity
Analysis of passive smoke exposure in the CRS populations showed a significantly decreased (p < 0.05) prevalence in CRSsNPs and CRSwNPs when compared with controls and AFRS (Fig. 1). Exposure to passive smoke was found to be statistically more likely in a younger, non-Caucasian, male population (p = 0.001, 0.000, and 0.024, respectively). After correcting for demographic variables with binary logistic regression, passive smoke exposure prevalence was equivalent to controls in CRSsNPs (p = 0.629), CRSwNPs (p = 0.275), and AFRS (p = 0.511). The prevalence of passive smoke exposure is detailed in Table 2.
Figure 1.
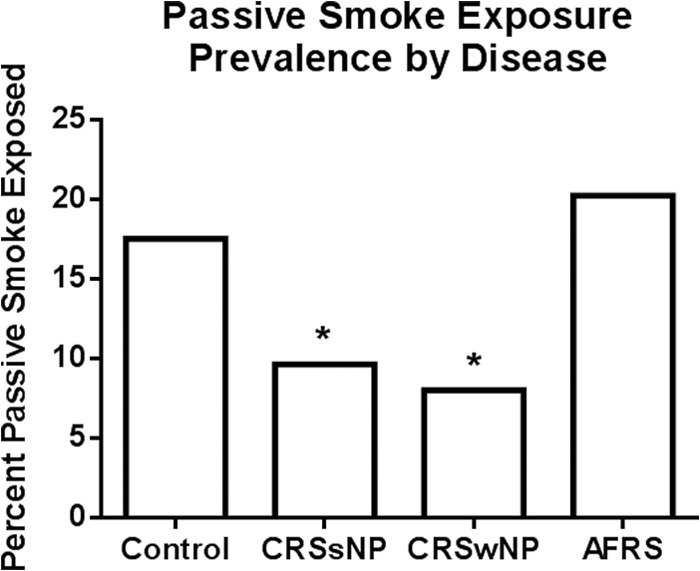
Passive smoke exposure prevalence by disease. Percentage of passive smoke-exposed patients as defined by nonsmokers with hair nicotine >2 ng/mg in chronic rhinosinusitis (CRS) subsets and control populations (*p < 0.05 compared with control).
Table 2.
Prevalence of passive smoke exposure in patient populations
The p value is calculated through binary logistic regression analysis with covariates of age, sex, and race with the control population as the reference variable.
CRS = chronic rhinosinusitis; CRSwNP = chronic rhinosinusitis with nasal polyp; CRSsNP = chronic rhinosinusitis without nasal polyp; AFRS = allergic fungal rhinosinusitis.
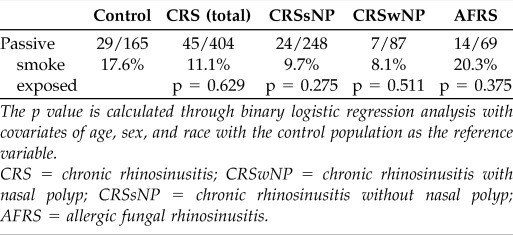
The average hair nicotine measurements of patients classified as passive smoke exposed were compared and found equivalent between all patient groups (p = 0.9312; Fig. 2).
Figure 2.
Severity of passive smoke exposure by disease. Severity of passive smoke exposure as estimated by average hair nicotine of passive smoke-exposed control, chronic rhinosinusitis without nasal polyp (CRSsNP), CRS with nasal polyp (CRSwNP), and allergic fungal rhinosinusitis (AFRS) patients. Values are mean ± SEM; p = 0.9312.
Pediatric Passive Smoke Exposure Prevalence
Prevalence of passive smoke exposure was significantly greater in children than adults for both control (26.2% versus 12.5%; p = 0.0338) and CRS (18.2% versus 9.8%; p = 0.0468) populations as depicted in Fig. 3. Among the CRS subsets, CRSwNP children were more likely to be exposed to passive smoke than adults (42.9% versus 5.0%; p = 0.01), and no appreciable difference was observed between age groups in CRSsNP (13.3% versus 2%; p = 0.5068) or AFRS (17.2% versus 22.5%; p = 0.7637).
Figure 3.
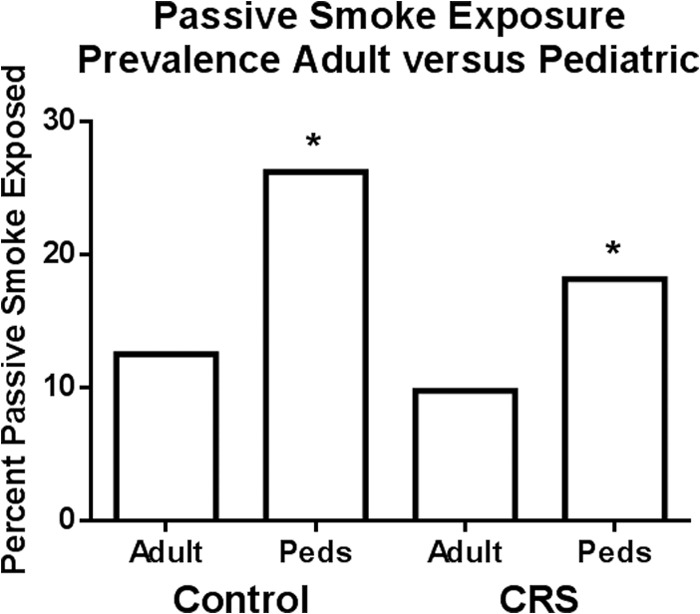
Passive smoke exposure prevalence adult versus pediatric. Percentage of passive smoke-exposed pediatric and adult patients as defined by nonsmokers with hair nicotine >2 ng/mg in chronic rhinosinusitis (CRS) and control populations (*p < 0.05).
Prevalence of Passive Smoke Exposure over Time
The prevalence of passive smoke exposure was evaluated in the patient population for each year of study from 2007 through 2013. Each patient received a hair nicotine measurement at the time of surgery, the results of which were compared with the other patients who had surgery in that same year to establish an annual passive smoke exposure prevalence. There was no significant trend or change in prevalence (p = 0.8365) over this 6-year time course, during which time several public smoking bans had been instituted in the studied region (Fig. 4).
Figure 4.
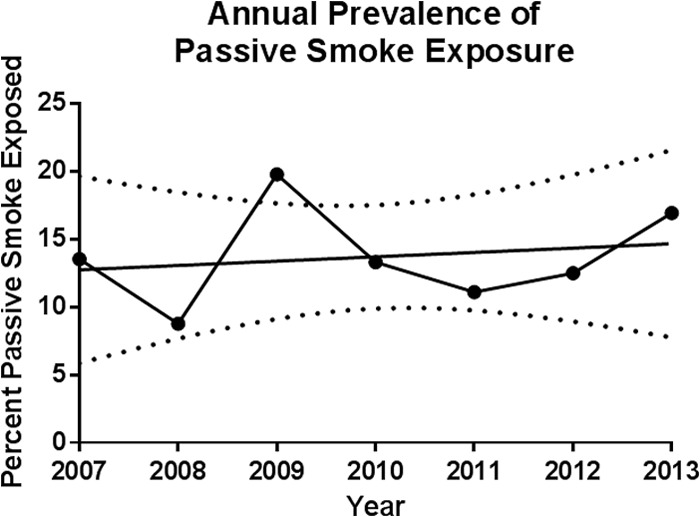
Passive smoke exposure prevalence over time. Annual percentage of passive smoke exposure as derived from year of surgery. The trend line was approximated using linear regression along with 95% confidence interval bands (dashed lines). The χ2-test for trend analysis for prevalence yielded a value of p = 0.67.
Prevalence of Active Smoking and CRS
A thorough chart review identified 58 active smokers at time of surgery, of which 19 were control patients, 29 were CRSsNP patients, 7 were CRSwNP patients, and 3 were AFRS patients (Fig. 5). The average hair nicotine of these patients was 24.58 ± 33.77 ng/mg with a range of 0.045–202.5 ng/mg and did not correlate with the reported number of cigarettes smoked per day (R2 = 0.003883). Despite a seemingly downward trend in active smoking prevalence with polypoid disease, particularly AFRS, the difference was not statistically significant before (p = 0.138) or after (p = 0.127) controlling for demographic differences in the groups (Table 3).
Figure 5.
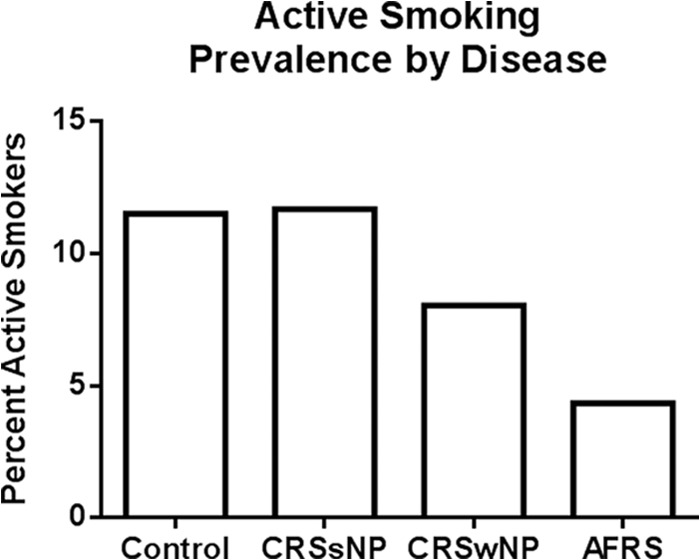
Active smoking prevalence by disease. Percentage of active smokers as defined by preoperative medical records in chronic rhinosinusitis (CRS) subsets and control populations.
Table 3.
Prevalence of active smoking in patient populations
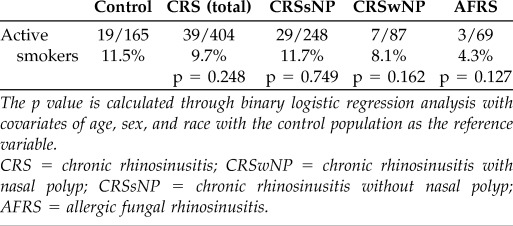
The p value is calculated through binary logistic regression analysis with covariates of age, sex, and race with the control population as the reference variable.
CRS = chronic rhinosinusitis; CRSwNP = chronic rhinosinusitis with nasal polyp; CRSsNP = chronic rhinosinusitis without nasal polyp; AFRS = allergic fungal rhinosinusitis.
DISCUSSION
This study uses quantitative measures of hair nicotine to determine the prevalence of passive cigarette smoke exposure in the CRS patient population compared with controls. We observed that although passive smoke exposure initially appears to be less common in the CRS population compared with controls, these differences are attributable to the unique demographic characteristics of the study populations. Thus, a randomly selected patient with CRS is equally likely to be passive smoke exposed as a randomly selected control. The severity of this exposure as determined by average hair nicotine of the passive smoke–exposed patients was also equivalent between control, CRSsNP, CRSwNP, and AFRS groups. Furthermore, the annual prevalence of passive smoke exposure in the patient population over the 6 years of data collection indicated no reductions in passive smoke exposure rates, despite the implementation of regional public smoking bans during this time frame. Through binary regression model analysis of this specific, regional patient population it was determined that passive smoke exposure was significantly more common in younger, non-Caucasian, male subjects (p = 0.001, 0.000, and 0.024, respectively), which is consistent with recent epidemiological reports.26 There were no significant associations between age (p = 0.070), sex (p = 0.146), or race (p = 0.577) on active smoking status. Active smoking prevalence appeared to be decreased in polypoid disease compared with controls; however, an informal power analysis estimated an additional 117 AFRS and 280 control patients were needed to achieve significance at this ratio.
Using the definition of passive smoke exposure as a nonsmoker with a hair nicotine level >2 ng/mg yielded a much lower passive smoke exposure rate than previous studies that have relied on subjective assessments of exposure. In the study by Reh et al., 39% of the 100 CRS patients enrolled in the study admitted to some amount of recent passive smoke exposure. This was comparable with the 35% of matched controls.16 Tammemagi et al. found 68% of the 306 CRS patients studied had reported passive smoke exposure in at least one environmental setting, either work, home, or public areas.15 However, patients with substantial symptoms of CRS may simply be more aware of nasal irritation from smoke exposure, leading to potential overreporting of passive smoke exposure in CRS or underreporting in healthy controls. Using hair nicotine as a quantifiable method to measure passive smoke exposure, we found a dramatically lower percentage of patients with measurable passive smoke exposure, and prevalence was comparable between CRS and controls (17.6% versus 11.1%). Hair nicotine from 1 cm of hair measures exposure over the previous month, therefore it is also possible that subjective recall was of distant or sporadic exposures not reflected in hair nicotine. The longer half-life of hair nicotine measurement renders it a more reliable measure of long-term passive smoke exposure than serum or urine cotinine, which has a half-life of 10–27 hours. However, by limiting the hair nicotine measurement to the last month of exposure, long-term exposure of several months to years is not distinguished from newly introduced exposure. The potential likelihood of a new and sustained exposure was weighed against the potential skewing of the data toward those with longer hair, predominantly women, and a length of 1 cm, or 1 month, was deemed a sufficient time frame for establishing passive smoke exposure in a wide population. In lieu of matched controls we corrected for demographic disparities between groups with binary logistic regression and confirmed no significant differences in prevalence between CRS, CRS subsets, and controls. This highlights the potential disparity between subjective recall instruments and objective measures of exposure.
Childhood exposure to passive smoke is more common than recent exposure in adults. Reh et al. estimated that ∼72% of their entire patient cohort experienced some exposure to passive smoke as children compared with the 28% that had no reported lifetime exposure or exposure limited to adulthood.16 In our study, 28 of the 127 children (22%) were passive smoke exposed by hair nicotine, compared with 46 of 442 adults (10.4%). Interestingly, although these estimated prevalences using hair nicotine as a quantifiable measure are lower than that obtained via survey, the ratio is approximately equal with passive smoke exposure being over twice as likely in children compared with adults. This exposure is most likely attained in the home and is reduced in homes where the parents do not permit smoking indoors.27–30 Given the potential impact of childhood cigarette smoke exposure on future health, limiting exposure to passive smoke in children is of the utmost importance.
Despite heavily advertised public health concerns and the direct link between cigarette smoke exposure and nasal irritation,6 this study indicates that there was no clear pattern of passive smoke avoidance in CRS. Passive smoke exposure prevalence and severity in CRS was comparable with controls, and any difference was found to be statistically insignificant after controlling for known differences in age, sex, and race via binary logistic regression. Starting in 2007 and continuing through 2013, several large cities and counties in South Carolina began instituting both indoor and outdoor smoking bans in public areas. Although public smoking bans have been shown to decrease cigarette smoke exposure in the general population over time,17 annual passive smoke exposure prevalence remained consistent over the 6-year course of this study. Smoke exposure in this specific population appears to be resilient against such measures and may require additional smoking education or cessation programs before a definitive decrease in exposure rates can be reached. In addition, it is possible that the majority of passive smoke exposure occurs in environments not impacted by smoking bans, such as private households.
With the apparent constancy of smoke exposure in CRS compared with controls, further studies are required to address the ramifications of exposure on disease pathology. Cigarette smoke exposure is known to contribute to the respiratory disease processes through numerous mechanisms including inhibiting mucociliary clearance,31 disrupting respiratory epithelium,32 inducing allergic mechanisms,10,14 increasing proinflammatory cytokine production,33 and increasing epithelial permeability.34 Although the specific mechanisms involved in the pathogenesis of CRS are still being elucidated, disruption of the protective barrier of the nasal and sinus mucosa is currently thought to play a key role.35–37 This disruption could theoretically be potentiated or exacerbated by cigarette smoke exposure through active smoking or passive smoke exposure.
Although attempts could be made to retrospectively establish a clinical correlation of smoke exposure to CRS severity through review of available 22-item Sino-Nasal Outcome Test scores, Lund-Mackay computed tomography scores, and comorbid asthma or allergic rhinitis diagnoses, etc, analysis of disease severity metrics was not the goal in the design of this study, and thus these data are of limited usefulness and ultimately not available in a comprehensive and validated fashion. A prospective collection of clinical outcome data would be required for a true assessment of the effects of passive smoke exposure on CRS severity and quality of life, and future studies at our institution are currently aimed at acquiring and examining these data. Additionally, the patient population studied is skewed because all patients involved were those who had failed medical management and required surgical intervention, representing only the most severe forms of CRS, making it unsuitable for assessment of clinical measures. Additionally, the analysis of this small, regional patient population would be insufficient because large-scale clinical studies, such as National Health and Nutrition Examination Survey and Surveillance, Epidemiology, and End Results Program collect information from tens of thousands of patients from a variety of large geographical regions over several years to establish strong correlations relating to disease incidence or severity. Future studies are needed to investigate the relationship between passive smoke exposure and CRS, including the correlation between passive smoke and clinical parameters of disease severity (computed tomography scores, 22-item Sino-Nasal Outcome Test, etc.) in a large-scale, prospective, multicenter survey of a broad clinical range of CRS patients.
CONCLUSION
Passive exposure to cigarette smoke is a considerable health hazard that is not avoided in patients with CRS. Quantifiable measures of hair nicotine allow an objective assessment of passive smoke exposure prevalence that is dramatically less than previous survey-based estimates but equivalent between CRS patients and controls. Passive smoke exposure prevalence is higher in children and the overall annual prevalence remains constant over time despite the institution of wide-spread public smoking bans in this region. Additional studies are therefore necessary to examine the clinical and physiological impact of passive cigarette smoke exposure on CRS.
ACKNOWLEDGMENTS
The authors thank Ryan Mulligan and Whitney Nagel for their technical support. These studies were made possible by the technical efforts and expertise of the Wellington Hospital Laboratory in Newton, New Zealand.
Footnotes
Funded by grants from the Flight Attendant Medical Research Institute to JK Mulligan (092401), Z Solar (113042), and RJ Schlosser (113039), as well as a Merit-Review Award from the Clinical Sciences Research and Development Program of the Department of Veterans Affairs (1 I01 CX000377).
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Gliklich RE, Metson R. The health impact of chronic sinusitis in patients seeking otolaryngologic care. Otolaryngol Head Neck Surg 113:104–109, 1995. [DOI] [PubMed] [Google Scholar]
- 2. Tan BK, Chandra RK, Pollak J, et al. Incidence and associated premorbid diagnoses of patients with chronic rhinosinusitis. J Allergy Clin Immunol 131:1350–1360, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen Y, Dales R, Lin M. The epidemiology of chronic rhinosinusitis in Canadians. Laryngoscope 113:1199–1205, 2003. [DOI] [PubMed] [Google Scholar]
- 4. Hastan D, Fokkens WJ, Bachert C, et al. Chronic rhinosinusitis in Europe—An underestimated disease. A GA2LEN study. Allergy 66:1216–1223, 2011. [DOI] [PubMed] [Google Scholar]
- 5. Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 50:1–12, 2012. [DOI] [PubMed] [Google Scholar]
- 6. Public Health Service. The health consequences of involuntary exposure to tobacco smoke: A report of the Surgeon General. Office of the Surgeon General, Office on Smoking and Health, Washington, D.C.: U.S. Department of Health and Human Services, Public Health Service, 2006. [Google Scholar]
- 7. Tamashiro E, Xiong G, Anselmo-Lima WT, et al. Cigarette smoke exposure impairs respiratory epithelial ciliogenesis. Am J Rhinol Allergy 23:117–122, 2009. [DOI] [PubMed] [Google Scholar]
- 8. Elwany SI, Ibrahim AA, Mandour Z, Talaat I. Effect of passive smoking on the ultrastructure of the nasal mucosa in children. Laryngoscope 112:965–969, 2012. [DOI] [PubMed] [Google Scholar]
- 9. Goldstein-Daruech N, Cope EK, Zhao KQ, et al. Tobacco smoke mediated induction of sinonasal biofilms. PLoS One 6 :e15700, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. De S, Leong SC, Fenton JE, et al. The effect of passive smoking on the levels of matrix metalloproteinase 9 in nasal secretions of children. Am J Rhinol Allergy 25:226–230, 2011. [DOI] [PubMed] [Google Scholar]
- 11. Siedek V, Stelter K, Betz CS, et al. Functional endoscopic sinus surgery—A retrospective analysis of 115 children and adolescents with chronic rhinosinusitis. Int J Pediatr Otorhinolaryngol 73:741–745, 2009. [DOI] [PubMed] [Google Scholar]
- 12. Smith TL, Mendolia-Loffredo S, Loehrl TA, et al. Predictive factors and outcomes in endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope 115:2199–2205, 2005. [DOI] [PubMed] [Google Scholar]
- 13. Eyigör H, Başal S. Evaluation of predisposing factors and bacteriologic agents in pediatric rhinosinusitis. Kulak Burun Bogaz Ihtis Derg 15:49–55, 2005. [PubMed] [Google Scholar]
- 14. Lin SY, Reh DD, Clipp S, et al. Allergic rhinitis and secondhand tobacco smoke: A population-based study. Am J Rhinol Allergy 25:e66–e71, 2011. [DOI] [PubMed] [Google Scholar]
- 15. Tammemagi C, Davis RM, Benninger MS, et al. Secondhand smoke as a potential cause of chronic rhinosinusitis. Arch Otolaryngol Head Neck Surg 135:327–334, 2010. [DOI] [PubMed] [Google Scholar]
- 16. Reh DD, Lin SY, Clipp SL, et al. Secondhand tobacco smoke exposure and chronic rhinosinusitis: A population-based case-control. Am J Rhinol Allergy 23:562–567, 2009. [DOI] [PubMed] [Google Scholar]
- 17. Rajkumar S, Huynh CK, Bauer GF, et al. Impact of a smoking ban in hospitality venues on second hand smoke exposure: A comparison of exposure assessment methods. BMC Public Health 13:536, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Avila-Tang E, Al-Delaimy WK, Ashley DL, et al. Assessing secondhand smoke using biological markers. Tob Control 22:164–171, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Eisner MD, Klein J, Hammond SK, et al. Directly measured second hand smoke exposure and asthma health outcomes. Thorax 60:814–821, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kim S, Wipfli H, Navas-Acien A, et al. Determinants of hair nicotine concentrations in nonsmoking women and children: A multicountry study of secondhand smoke exposure in homes. Cancer Epidemiol Biomarkers Prev 18:3407–3414, 2009. [DOI] [PubMed] [Google Scholar]
- 21. Al-Delaimy WK. Hair as a biomarker for exposure to tobacco smoke. Tob Control 11:176–182, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mahoney GN, Al-Delaimy W. Measurement of nicotine in hair by reversed-phase high-performance liquid chromatography with electrochemical detection. J Chromatogr B Biomed Sci Appl 753:179–187, 2001. [DOI] [PubMed] [Google Scholar]
- 23. Collins JG. Prevalence of selected chronic conditions: United States, 1990–1992. Vital Health Stat 10 194:1–89, 1997. [PubMed] [Google Scholar]
- 24. Johansson L, Akerlund A, Holmberg K, et al. Prevalence of nasal polyps in adults: The Skövde population-based study. Ann Otol Rhinol Laryngol 112:625–629, 2002. [DOI] [PubMed] [Google Scholar]
- 25. Laury A, Wise SK. Chapter 7: Allergic fungal rhinosinusitis. Am J Rhinol Allergy Suppl 1:S26–S27, 2013. [DOI] [PubMed] [Google Scholar]
- 26. Wichmann MA, Cruickshanks KJ, Nondahl DM, et al. Changes in environmental tobacco smoke exposure: The Beaver Dam experience. WMJ 112:53–57, 2013. [PMC free article] [PubMed] [Google Scholar]
- 27. Gonçalves-Silva RM, Valente JG, Lemos-Santos MG, Sichieri R. Smoking in households in Brazil with children younger than 5 years of age [in Portuguese]. Rev Panam Salud Publica 17:163–169, 2005. [DOI] [PubMed] [Google Scholar]
- 28. Winkelstein ML, Tarzian A, Wood RA. Parental smoking behavior and passive smoke exposure in children with asthma. Ann Allergy Asthma Immunol 78:419–423, 1997. [DOI] [PubMed] [Google Scholar]
- 29. Ayers JW, Hofstetter CR, Hughes SC, et al. Smoking on both sides of the pacific: Home smoking restriction and secondhand smoke exposure among Korean adults and children in Seoul and California. Nicotine Tob Res 12:1142–1150, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gonzales M, Malcoe LH, Kegler MC, Espinoza J. Prevalence and predictors of home and automobile smoking bans and child environmental tobacco smoke exposure: A cross-sectional study of U.S.- and Mexico-born Hispanic women with young children. BMC Public Health 6:265, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wang LF, White DR, Andreoli SM, et al. Cigarette smoke inhibits dynamic ciliary beat frequency in pediatric adenoid explants. Otolaryngol Head Neck Surg 146:659–663, 2012. [DOI] [PubMed] [Google Scholar]
- 32. Dye JA, Adler KB. Effects of cigarette smoke on epithelial cells of the respiratory tract. Thorax 49:825–834, 1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mulligan JK, Mulligan RM, Atkinson C, Schlosser RJ. Human sinonasal epithelial cells direct dendritic function and T-cell T helper 1/T helper 2 skewing following Aspergillus exposure. Int Forum Allergy Rhinol 1:268–274, 2011. [DOI] [PubMed] [Google Scholar]
- 34. Forteza RM, Casalino-Matsuda SM, Falcon NS, et al. Glycobiology and extracellular matrices: Hyaluronan and layilin mediate loss of airway epithelial barrier function induced by cigarette smoke by decreasing E-cadherin. J Biol Chem 287:42288–42298, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zuckerman JD, Lee WY, DelGaudio JM, et al. Pathophysiology of nasal polyposis: The role of desmosomal junctions. Am J Rhinol 22:589–597, 2008. [DOI] [PubMed] [Google Scholar]
- 36. Rogers GA, Den Beste K, Parkos CA, et al. Epithelial tight junction alterations in nasal polyposis. Int Forum Allergy Rhinol 1:50–54, 2011. [DOI] [PubMed] [Google Scholar]
- 37. Richer S, Truong-Tran AQ, Conley DB, et al. Epithelial genes in chronic rhinosinusitis with and without nasal polyps. Am J Rhinol 22:228–234, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]


