Abstract
Stigma, discrimination and violence contribute to health disparities among sexual minorities. Lesbian, bisexual and queer (LBQ) women experience sexual violence at similar or higher rates than heterosexual women. Most research with LBQ women, however, has focused on measuring prevalence of sexual violence rather than its association with health outcomes, individual, social and structural factors. We conducted a cross-sectional online survey with LBQ women in Toronto, Canada. Multivariate logistic regression analyses were conducted to assess correlates of lifetime sexual assault (LSA). Almost half (42%) of participants (n = 415) reported experiences of LSA. Participants identifying as queer were more likely to have experienced LSA than those identifying as lesbian. When controlling for socio-demographic characteristics, experiencing LSA was associated with higher rates of depression, sexually transmitted infections (STIs), receiving an STI test, belief that healthcare providers were not comfortable with their LBQ sexual orientation, and sexual stigma (overall, perceived and enacted). A history of sexual violence was associated with lower: self-rated health, overall social support, family social support and self-esteem. This research highlights the salience of a social ecological framework to inform interventions for health promotion among LBQ women and to challenge sexual stigma and sexual violence.
Introduction
Sexual minorities experience pervasive health disparities associated with stigma, discrimination and violence [1–4]. Chronic stress stemming from these social contexts of stigma, discrimination and violence contributes to health inequities [3, 5]. For example, a national US study (n = 34 653) reported that lesbian, gay and bisexual (LGB) persons had higher risk for the onset of post-traumatic stress disorder (PTSD) than heterosexuals, in part due to LGB person’s elevated exposure to interpersonal violence [6]. Lesbian, bisexual and queer (LBQ) women experience sexual violence at similar [e.g. adult sexual assault (ASA)] or higher (e.g. childhood sexual abuse) rates than heterosexual women [7–14]. There is an urgent need to better understand the interplay between sexual violence, health outcomes, individual, social and structural factors among LBQ women.
Sexual violence among sexual minority women
Although study findings highlight that LBQ women experience health disparities and are particularly vulnerable to certain types of violence (e.g. hate crime, childhood sexual abuse) there is a dearth of LBQ population-specific information about types and correlates of sexual assault (in line with previous studies [10, 11, 14] we use the term ‘sexual assault’ to include the scope of sexual assault, sexual violence, forced sex, sexual abuse and rape; we use ‘sexual assault’ and ‘sexual violence’ interchangeably. We acknowledge there are varying conceptual definitions of sexual assault and sexual violence [14]) [6, 8]. A recent systematic review by Rothman et al. [14] explored prevalence rates for various types of sexual assault victimization, including lifetime sexual assault (LSA), childhood sexual assault (CSA), ASA, intimate partner sexual assault (IPSA) and hate crime-related assault, and concluded that these types of violence were elevated for LGB populations. For example, although estimates from the United States indicate 11–17% of women have experienced LSA [15, 16], systematic review results reported lesbian and bisexual (LB) women had prevalence rates of LSA from 16% to 85% [14]. The wide variance was in part attributed to study design, with population-based studies reporting lower rates of sexual violence in comparison with convenience samples, as well as widely varying sampling methods and definitions of sexual assault and sexual orientation [14].
Friedman et al.’s [9] meta-analysis indicated that female sexual minorities were 1.5 times more likely to have experienced CSA than female heterosexuals. Although LB women were more likely than gay/bisexual men to report CSA, ASA, LSA and IPSA, LB women remain greatly underrepresented in sexual violence research in comparison with GB men [14]. Few studies assess the gender or sexual orientation of perpetrators of sexual violence among LB women, and this is also true for IPSA studies where there is a knowledge gap regarding whether perpetrators were same or opposite-sex partners [14].
Social and structural contexts of health among sexual minority women
Systematic reviews and population-based studies highlight elevated risks for mental health issues among sexual minority women. Social ecological approaches explore the complex associations between health disparities and social and structural environments [17, 18]. Health outcomes are shaped by individual (e.g. knowledge, attitudes, behavior), social (e.g. social support, sexual networks) and structural (e.g. stigma and discrimination, access to health care) level factors [18]. For example, numerous studies indicate higher rates of depression among sexual minority women in comparison with heterosexual women [1, 3, 19–21]. Sexual stigma—a structural factor—has been associated with these higher rates of depression [3] and psychological distress [22].
Sexual stigma refers to social and institutional processes of devaluation of sexual minority identities, communities and same-sex relationships [23]. Forms of stigma include perceived, or felt-normative stigma that refers to awareness of negative societal attitudes and fear of discrimination; and enacted stigma such as overt acts of discrimination and violence [23, 24]. Internalized homophobia refers to individuals’ acceptance of negative beliefs, views and feelings toward the stigmatized group and oneself [23, 24].
Experiences of sexual violence may also be correlated with depression [13] and PTSD [6, 25] among lesbians. Internalized homophobia was associated with PTSD among gay male [26] and lesbian [27] sexual assault survivors. Among heterosexual women sexual violence appears to be consistently correlated with alcohol abuse, yet the pattern with LBQ women appears to be different. For instance, one study found that among LBQ women, CSA—but not ASA—was positively associated with alcohol abuse [10].
Limited research has examined physical and sexual health correlates of LSA among sexual minority women. Childhood sexual abuse was associated with functional pain in a US based cohort study of sexual minority youth [28]. Functional pain refers to pain without a diagnosed pathology, such as headaches, abdominal and pelvic pain [28]. Another study reported that a history of CSA was associated with the likelihood to engage in sexual risk behaviors in adolescence and adulthood, thus contributing to HIV and sexually transmitted infections (STIs) risk among ‘mostly heterosexual’ young women [29]. Sexual abuse was also correlated with HIV risk behaviors among LB students in a US and Canadian cohort study [30].
Response strategies to sexual violence among sexual minority women
Sexual minority and heterosexual women tend to have passive response strategies following incidences of sexual violence: they either do nothing or only tell someone they trust, as opposed to authorities that can intervene [8, 31]. However, some researchers argue that sexual minority women are better at coping with violence as a result of managing the stigma of being a sexual minority and subsequently developing stronger support networks [7]. Although the literature indicates that LBQ women do access certain support services, there are barriers to access for LBQ women. Concerns regarding stigma and discrimination may result in LBQ women choosing not to disclose their sexual orientation to healthcare providers (HCP) [32, 33]. The experiences of LBQ women accessing care may also differ based on sexual identity. For instance, bisexual and ‘mostly heterosexual’ women may feel uncomfortable accessing services for lesbians [30]; similarly, lesbians may feel uncomfortable accessing services that are perceived to be for heterosexual women (e.g. rape crisis centers, shelters) [7, 31].
Study goals and objectives
We aimed to address two important gaps in the literature in this study. First, scant research has explored the impact of LSA among sexual minority women [14]. Sexual violence research with LBQ women has predominately focused on prevalence, rather than the impact of such violence on various dimensions of women’s lives, including sexual and mental health outcomes [7]. Second, most studies among sexual minority women have not explicitly measured the associations between LSA and structural factors, such as sexual stigma and barriers to health care. The social ecological approach of understanding individual, social and structural factors associated with LSA among sexual minority women therefore warrants further exploration.
Our study was informed by the social ecological framework. The objective of this study was to contribute to understanding regarding associations between experiences of LSA and: health outcomes (depression, STI, self-rated health), individual factors (self-esteem, resilient coping, substance use), social factors (safer sex practices, social support) and structural factors (utilization of HIV and STI testing services, barriers to healthcare access, sexual stigma) among sexual minority women in Toronto, Canada.
Methods
Study design and population
We conducted a structured cross-sectional internet-based survey with sexual minority women in Toronto, Canada in December 2011. Inclusion criteria for survey participants were adults aged 18 and over, capable of providing online informed consent, who self-identified as (i) a women, (ii) a sexual minority and/or a women who has sex with women, including lesbian, gay, bisexual, queer, ‘other’ and (iii) residing in the Greater Toronto Area. We hired 10 peer research assistants (PRAs), defined as someone who identifies as a sexual minority women to facilitate participant recruitment; PRAs represented diverse ages, ethnicities and sexualities.
Data collection
We used modified peer-driven recruitment, where each PRA recruited a pre-specified number of participants (n = 25) as well as convenience sampling, whereby participants could invite additional participants. Recruitment was primarily undertaken by PRAs through word of mouth and emails to social networks, LGBTQ agencies and ethno-cultural agencies. There was an email that briefly outlined the study purpose and inclusion criteria that included a direct link to the survey; this email was distributed by PRAs and agencies. We used a self-administered survey that participants completed online in a location of their choosing; the survey took ∼60 min to complete. We aimed to recruit 425 participants. The recommended sample size for logistic regression (odds ratio: 1.3, P < 0.05, power: 0.80) is 406 as calculated using G*Power 3.1. Research Ethics Board approval was obtained from Women’s College Hospital at the University of Toronto.
We designed a survey to collect information on socio-demographic variables, health outcomes, individual, social and structural factors. We pilot-tested the survey with a focus group of sexual minority community representatives (n = 12) (e.g. LGBT event promoters, artists, community organizers) to acquire feedback to enhance clarity and content validity. No identifying information was collected; participants had the option to choose to include their email address to receive a $20 gift card as honorarium for survey completion. Email addresses were erased after the gift card was sent. At the end of the survey, participants were provided with a list of community and online resources for sexual minority women and health and supportive services.
Measures
We report measures used and Cronbach’s alpha coefficients from the current analyses. The survey included 105 items. Measures were chosen based on (i) conceptual relevance for the social ecological framework, (ii) established reliability and validity in the North American context, and where possible among LGBQ persons and (iii) shortened scales where possible to reduce participant burden (e.g. with depression symptoms, resilient coping). We summed scale items to calculate total scores for: sexual stigma, depression, safer sex practices, resilient coping; sub-scale and total scores were calculated for social support. The intervals for the measures were one unit (e.g. 1 year of age, one scale unit).
Lifetime sexual assault
We used a single dichotomous item: ‘In your life have you ever experienced forced sex (for example rape or sexual assault)?’ to assess if participants had a history of LSA.
Health outcomes
Participants self-reported if they had ever been diagnosed with an STI. Self-reporting of HIV/STI history was effective in a previous study with LBQ women in the United States [34]. The two-item Patient Health Questionnaire-2 was used to assess depression symptoms [35], Cronbach’s α = 0.89 (scale range: 0–6). Participants rated their health using single global self-rated health response recommended by the World Health Organization (score range: 1–5) [36].
Socio-demographic variables
We collected the following socio-demographic information: age (years), annual personal income (Canadian dollars), sexual orientation (queer, lesbian, bisexual, gay, other, with options to specify), ethno-racial identity (self-identified) and highest level of education (less than primary, primary, some secondary, secondary, some post-secondary, post-secondary, graduate and post-graduate).
Individual factors
Resilient coping was measured using the Brief Resilient Coping Scale [37], Cronbach’s α = 0.69 (scale range: 4–20). Self-esteem was measured using the Single-Item Self-Esteem Scale that has participants respond the statement: ‘I have high self-esteem’ on a five-point Likert scale (score range: 1–5) [38]. Substance use was assessed using an eight-point Likert scale single-item measure regarding frequency of drug and alcohol use in the past 3 months (score range: 1–8).
Social factors
Safer sex practices were measured using the ‘Safer Sexual Behaviors Among Lesbian Women Scale’ [39], Cronbach’s α = 0.70 (scale range: 9–36). The social support measure was based on the Multi-dimensional Scale of Perceived Social Support [40] (Cronbach’s α = 0.91) (scale range: 12–60) that includes sub-scales to assess support from family (Cronbach’s α = 0.93) (sub-scale range: 4–20), friends (Cronbach’s α = 0.92) (sub-scale range: 4–20) and a significant other (Cronbach’s α = 0.95) (sub-scale range: 4–20).
Structural factors
The sexual stigma measure was based on the Homophobia Scale [5] (Cronbach’s α = 0.78) (scale range: 12–48), that includes sub-scales to examine both perceived (Cronbach’s α = 0.70) (sub-scale range: 4–16) and enacted (Cronbach’s α = 0.72) (sub-scale range: 8–32) stigma. Participants responded to questions asking if they had ever received (i) an HIV test and (ii) an STI test (not including HIV). Participants also responded to questions asking if they had ever experienced the following barriers to accessing health care: (i) cost travel, (ii) cost medications and (iii) belief that their HCP was not comfortable with their sexual orientation.
Data analysis
We conducted descriptive analyses to calculate frequencies, means and standard deviations for each variable. Data analyses were conducted using IBM SPSS 20. Cronbach’s alpha was conducted to assess scale reliability for each scale. We conducted logistic regression analyses based on the social ecological framework to examine sexual violence and its association with health outcomes, individual, social and structural factors. Multivariate logistic regression analyses were conducted to determine correlates of having experienced sexual assault in one’s lifetime. We first conducted unadjusted logistic regression analyses, followed by analyses that controlled for socio-demographic variables (age, education, income, ethnicity, sexual orientation). We also present relative risks (RRs) for significant variables to illustrate the probability of the outcome for those who have a history of LSA in comparison with those with no LSA.
Results
Study population
There were 439 women who participated in the survey; 415 completed the item on LSA and were included in the analyses. Socio-demographic and health characteristics of participants (n = 415) are described in Table I. The mean participant age (n = 396) was 31.44 (SD: 8.13), and the median annual income was $29 000.00 (range: 18–70). Most participants identified as queer (45.5%) followed by lesbian (29.2%), bisexual (16.1%), gay (4.6%) and other (4.1%). Almost half (41.7%) of participants reported having experienced sexual assault. One-fifth (20.5%) of participants reported ever being diagnosed with an STI.
Table I.
Demographic and health information among survey participants (n = 415)
| Variables | Mean (SD) | ||
|---|---|---|---|
| Age (n = 396) | 31.44 (8.13) | ||
| Annual income (n = 400) | 31 651.32 (28 144.14) | Range: 18–70, median: 29 000.00 | |
| % | n | ||
| Sexual orientation (n = 415) | Queer | 45.5 | 189 |
| Lesbian | 29.2 | 121 | |
| Bisexual | 16.1 | 67 | |
| Gay | 4.6 | 19 | |
| Other | 4.1 | 17 | |
| Ethno-racial identity (n = 389) | White/Caucasian | 67.1 | 261 |
| Black, African Caribbean | 18.7 | 73 | |
| Asian | 4.2 | 16 | |
| South Asian | 4.2 | 16 | |
| Indigenous/Aboriginal | 3.8 | 15 | |
| Multiple ethnicities | 2.0 | 8 | |
| Education (n = 415) | Less than high school | 0.7 | 3 |
| High school or equivalent | 7.0 | 29 | |
| Some college/university | 14.7 | 61 | |
| College diploma | 13.0 | 54 | |
| Bachelor degree | 36.9 | 153 | |
| Graduate degree | 27.7 | 115 | |
| Self-rated health (n = 415) | Excellent | 14.2 | 59 |
| Very good | 46.0 | 191 | |
| Good | 30.8 | 128 | |
| Fair | 7.0 | 29 | |
| Poor | 1.9 | 8 | |
| HIV serostatus (n = 415) | HIV negative | 90.1 | 374 |
| Don’t know | 8.4 | 35 | |
| HIV positive | 1.2 | 5 | |
| Don’t want to share | 0.2 | 1 | |
| History of an STI (n = 415) | Yes | 20.5 | 85 |
| No | 79.5 | 330 | |
| History of LSA (n = 415) | Yes | 41.7 | 173 |
| No | 58.3 | 242 | |
Correlates of having experienced sexual violence
Logistic regression results are presented in Table II. Participants with a lesbian identity were significantly less likely to report a history of sexual violence than those with a queer identity [OR: 0.56 (CI: 0.35, 0.89), P < 0.05]. The RR of LSA among queer woman in comparison with lesbians was 2.16. No other socio-demographic characteristics were associated with a history of sexual violence. In multivariate analyses, when controlling for socio-demographic characteristics, having experienced sexual violence was associated with significantly higher reported mean frequencies of depressive symptoms [OR: 1.21 (CI: 1.06, 1.39), P < 0.01; RR: 1.17], prevalence of STI [OR: 1.83 (CI: 1.05, 3.18), P < 0.05; RR: 1.86], belief that their HCP was not comfortable with their sexual orientation [OR: 2.45 (CI: 1.29, 4.66), P < 0.01; RR: 2.45] and having ever received an STI test [OR: 2.92 (CI: 1.42, 6.01), P < 0.01; RR: 3.00]. Those with a history of sexual violence also reported higher mean frequencies of sexual stigma (overall) [OR: 1.13 (CI: 1.07, 1.18), P < 0.001; RR: 1.13], enacted sexual stigma [OR: 3.87 (CI: 2.20, 6.84), P < 0.001; RR: 3.79] and perceived sexual stigma [OR: 1.81 (CI: 1.30, 2.51), P < 0.001; RR: 1.78]. A history of forced sex was associated with lower reported mean frequencies of: self-rated health [OR: 0.70 (CI: 0.54, 0.92), P < 0.05; RR: 0.69], overall social support [OR: 0.97 (CI: 0.95, 0.99), P < 0.05; RR: 0.96], social support from family [OR: 0.93 (CI: 0.88, 0.98), P < 0.01; RR: 0.92] and self-esteem [OR: 0.61 (CI: 0.48, 0.77), P < 0.001; RR: 0.61]. Participants with a history of LSA were 1.63 times more likely to report low self-esteem, 1.44 times more likely to report lower self-rated health, 1.08 more likely to report low family social support and 1.04 times more likely to report low overall social support than those with no history of LSA.
Table II.
Multivariate logistic regression of factors correlated with LSA among LBQ women in Toronto, Canada (n = 415)
| Variablesa | Unadjusted logistic regression analyses, OR (95% CI) | P-value | Adjusted logistic regression analysesb, OR (95% CI) (n = 341) | P-value |
|---|---|---|---|---|
| Socio-demographics | ||||
| Age (n = 396) | 0.99 (0.97, 1.03) | 0.959 | ||
| Education | 1.03 (0.92, 1.16) | 0.636 | ||
| Income (n = 400) | 0.87 (0.70, 1.09) | 0.233 | ||
| Ethnicity (person of color versus white) (n = 389) | 0.79 (0.52, 1.23) | 0.305 | ||
| Sexual orientation | ||||
| Queer (ref) | 1 | |||
| Other | 0.45 (0.15, 1.32) | 0.146 | ||
| Bisexual | 0.77 (0.44, 1.36) | 0.371 | ||
| Lesbian | 0.56 (0.35, 0.89) | 0.016* | ||
| Gay | 0.49 (0.18, 1.36) | 0.174 | ||
| Health outcomes | ||||
| Depression | 1.23 (1.09, 1.38) | 0.001* | 1.21 (1.06, 1.39) | 0.006* |
| Self-rated health | 0.66 (0.53, 0.83) | 0.000* | 0.70 (0.54, 0.92) | 0.010* |
| History of STI | 2.18 (1.35, 3.53) | 0.002* | 1.83 (1.05, 3.18) | 0.033* |
| Individual factors | ||||
| Resilient coping | 1.07 (1.00, 1.16) | 0.059 | 1.08 (0.99, 1.18) | 0.105 |
| Self-esteem | 0.64 (0.53, 0.79) | 0.000 | 0.61 (0.48, 0.77) | 0.000* |
| Substance use-past 3 months | 0.89 (0.79, 1.01) | 0.069 | 0.89 (0.77, 1.02) | 0.101 |
| Social factors | ||||
| Safer sex practices | 0.93 (0.88, 0.98) | 0.006* | 0.95 (0.90, 1.01) | 0.220 |
| Social support (overall) | 0.97 (0.95, 0.99) | 0.016* | 0.97 (0.95, 0.99) | 0.043* |
| Social support: family | 0.92 (0.88, 0.97) | 0.001* | 0.93 (0.88, 0.98) | 0.005* |
| Social support: friends | 0.98 (0.92, 1.05) | 0.576 | 0.97 (0.90, 1.04) | 0.422 |
| Social support: sig other | 0.97 (0.92, 1.01) | 0.196 | 0.97 (0.91, 1.03) | 0.376 |
| Structural factors: stigma | ||||
| Sexual stigma (overall) | 1.13 (1.08, 1.18) | 0.000* | 1.13 (1.07, 1.18) | 0.000* |
| Sexual stigma (perceived) | 1.68 (1.27, 2.23) | 0.000* | 1.81 (1.30, 2.51) | 0.000* |
| Sexual stigma (enacted) | 4.18 (2.56, 6.81) | 0.000* | 3.87 (2.20, 6.84) | 0.000* |
| Structural factors: health services access and barriers to health care | ||||
| Ever had an HIV test (n = 370) | 2.21 (1.33, 3.67) | 0.002* | 1.66 (0.93, 2.96) | 0.088 |
| Ever had an STI test (n = 370) | 3.64 (1.87, 7.08) | 0.000* | 2.92 (1.42, 6.01) | 0.004* |
| Barrier: belief HCP not comfortable with sexual orientation | 2.47 (1.43, 4.28) | 0.001* | 2.45 (1.29, 4.66) | 0.006* |
| Barrier: travel | 2.07 (0.99, 4.34) | 0.055 | 2.01 (0.86, 4.71) | 0.110 |
| Barrier: medication cost | 1.93 (1.16, 3.21) | 0.012* | 2.35 (1.26, 4.35) | 0.007* |
an = 415 unless otherwise specified.
bAnalyses include individual variables with adjustment for socio-demographic variables.
*P < 0.05.
Discussion
This study’s examination of correlates of experiences of LSA among LBQ women revealed deleterious health outcomes associated with LSA, including exacerbated risk for depression, STI and lower self-rated health. Our findings that individual (self-esteem), social (social support) and structural (barriers to care, access to STI testing, sexual stigma) factors were associated with LSA support the utility of the social ecological framework to understanding LBQ women’s experiences of sexual violence.
A social ecological conceptual framework that incorporates these multi-level domains associated with LSA among LBQ women is illustrated in Fig. 1. We categorized multi-level—structural, social, individual—factors and health outcomes correlated with LSA that can guide the development of health promotion (e.g. mental, sexual) interventions. This framework may inform future research focused on sexual violence and connections with health outcomes (e.g. depression, STI) and resilience (e.g. social support) among sexually diverse women.
Fig. 1.
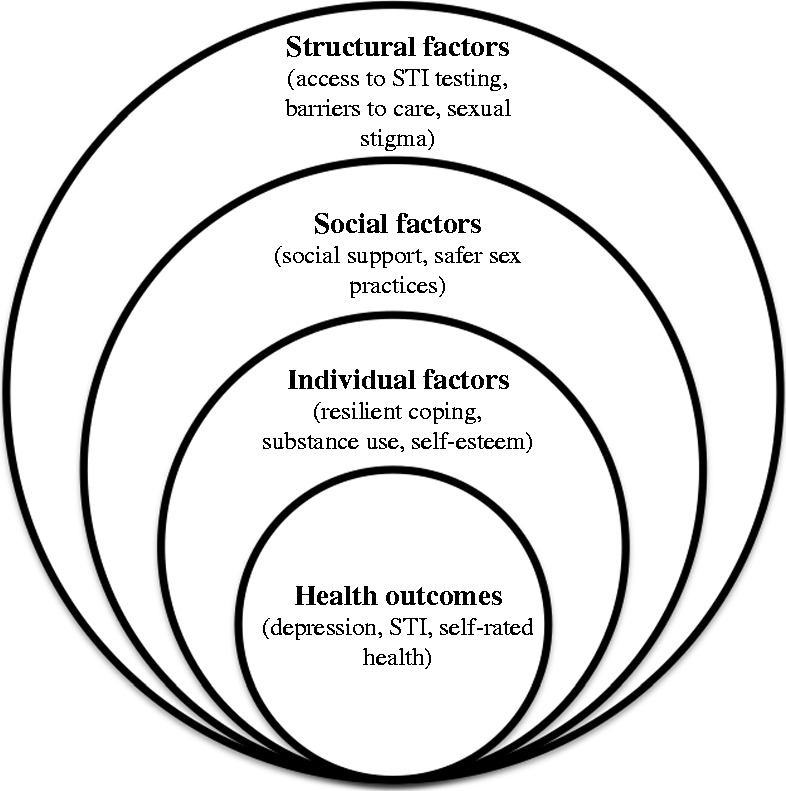
Social ecological approach to understanding correlates of LSA experienced by sexual minority women in Toronto, Canada (n = 415).
Approximately 40% of our sample reported LSA, corroborating median rates of LSA reported among LB women in systematic review results in the United States [14]. Our findings that LSA was associated with reported higher mean frequencies of depressive symptoms and prevalence of STI, and lower mean frequencies of self-rated health and self-esteem, corroborate previous research. The negative effects of sexual assault are well documented and include PTSD in up to 50% of sexual assault survivors, and concurrent depression [6, 13, 21, 41]. Our findings that LSA was correlated with lower self-rated health align with Roberts et al. [28] US based cohort study findings with sexual minority youth that reported associations between functional pain and CSA [28]. Indeed our study found associations between LSA and higher STI rates, supported by previous research with samples of predominately heterosexual [42, 43] and sexual minority [29] women. We found lower self-esteem was associated with LSA, self-esteem has been associated with CSA [44]. Similar to another study with lesbians, we found no significant association between substance use and sexual violence [10].
Despite the disproportionate rates of sexual violence experienced by sexual minority women in comparison with heterosexual women, we found no other studies that explicitly measured associations between LSA and perceived or enacted sexual stigma. Our findings that LSA was correlated with higher reported mean frequencies of overall, perceived and enacted sexual stigma suggests that sexual violence may be associated with experiences, perceptions and subsequent expectations of homophobia and discrimination. The belief that one’s HCP was uncomfortable with their sexual orientation is another example of a structural barrier experienced by LBQ women with a history of LSA. This finding is corroborated by research that highlights heterosexism in women’s sexual health care [45, 46], fear of discrimination from disclosing sexual orientation to HCP [32, 33] and discomfort utilizing services not tailored for their sexual orientation [7, 29, 31]. Other barriers emerged for participants who experienced LSA—medication costs—even when controlling for income and education. This suggests that factors such as sexual stigma and fear of discrimination may enhance perception of other barriers to healthcare access.
Despite these barriers, those with a history of LSA did in fact access STI testing more frequently than those without a history of LSA. We are not aware of research that has explored this phenomenon. Other research, however, suggests that coping with stigma and discrimination has resulted in utilization of services by LBQ women. For example, some authors have suggested that as a result of having had to cope with sexual stigma, LBQ women tend to access therapy at a higher rate than heterosexual women [7, 10, 13]. LBQ women who have experienced LSA may, therefore, be more accustomed to accessing healthcare services, and this may also be viewed as a strategy of resilience.
Those with a history of LSA reported lower mean frequencies of overall social support and social support from family. This could be associated with sexual stigma from family members due to their sexual minority identity [47, 48]. Lower levels of family social support could also be associated with a history of CSA, especially if the perpetrator was a family member or close to the family. Family support is often compromised with divided loyalties or outright disbelief when the accused perpetrator is a family relation or friend [49].
Participants with a history of LSA were more likely to identify as queer than lesbian. There is very little understanding of the interplay between LSA and sexual orientation. Previous studies with young women reported higher rates of CSA [29] and LSA [30] among women who identified as ‘mostly heterosexual’ or bisexual [9, 38] in comparison with those identifying as heterosexual. Austin et al.’s [29] thoughtful discussion regarding possible reasons for sexual orientation differences in rates of sexual assault include (i) response bias, (ii) sexual identity formation and (iii) different risk factors. First, a woman identifying as queer—a fluid sexual orientation that moves beyond the dichotomies of lesbian/heterosexual [50]—may be more willing to report sexual violence than other women as they may feel less stigma about having forced sex with men. Second, depending on when sexual assault occurred, it could influence sexual identity formation [29]; for example, adopting a queer identity, rather than a lesbian one, could be more congruent with a history of LSA. Third, persons identifying as lesbian may have more positive group identity and social support than those with other sexual minority identities such as ‘mostly heterosexual’ [28], and this strong group identity and support may reduce vulnerability to abuse by parents, adults and youth [51, 52]. The interplay between sexual orientation and LSA warrants further attention.
The study design has several limitations. First, the non-probability sample limits the generalizability of findings. The sample was recruited by diverse PRAs but oversampled white LBQ women; our sample included approximately one-third visible minorities while almost one-half—47%—of persons in the City of Toronto are visible minorities [53]. Our sample also had higher education levels—with almost 65% holding a bachelor’s degree or higher—than the general population of Toronto where 33% hold a bachelor degree [54]. The online survey method may have contributed to oversampling LBQ women with access to internet and computer/written literacy; Meyer and Wilson [55] discussed a digital divide in the United States where persons with internet access were more likely to be white. The online survey method and sampling strategy may therefore have introduced selection bias. Second, because of the cross-sectional survey design we could not assess causation. Therefore, a longitudinal design could be more conducive to understanding the relationships between sexual violence, mental and sexual health outcomes, and sexual stigma. As we did not measure PTSD, it is possible that higher rates of depression were associated with PTSD stemming from sexual assault. In addition, we did not measure internalized homophobia—this could have enhanced our understanding of sexual stigma correlates of LSA. Third, we only had one sexual violence occurrence question, limiting understanding of age and frequency for which sexual violence occurred, gender of perpetrator and the number of perpetrators. We did not explore whether sexual violence occurred within a relationship or differentiate between the types of sexual violence. Fourth, our measure of resilient coping may not have adequately captured the complexity of resilience (e.g. coping with trauma, adapting to one’s socio-cultural environment), the ability to cope with multiple risks (e.g. stigma, sexual assault) or access to multiple resources [56, 57]. Fifth, we used a single item question regarding substance use that did not differentiate between alcohol and other substances, precluding an in-depth understanding of this phenomenon among participants. Given these limitations, further research could engage more diverse samples of LBQ women—perhaps using both on/offline methods, explore additional resilience and substance use measures and include more detailed questions regarding types and perpetrators of sexual violence.
Despite these limitations our study has several strengths. First, this study contributes to theoretical development by exploring health outcomes and individual, social and structural factors associated with LSA among LBQ women. Our findings support the utilization of a social ecological approach to better contextualize sexual violence and its impacts among LBQ women. Second, to our knowledge this is the first study to demonstrate associations between enacted and perceived sexual stigma with LSA among LBQ women. Third, this study highlighted the importance of understanding barriers to accessing health care and the need for training HCP to demonstrate trauma-informed, LGBTQ affirmative practice.
Enhanced understanding of correlates of LSA among LBQ women can inform the development of multi-level interventions to promote health and reduce stigma and violence. Our findings suggest that LBQ women who have experienced LSA have unique health needs, as they may be particularly vulnerable to sexual stigma, depression, STI and report lower self-esteem and self-rated health. These myriad health challenges require a syndemics approach that targets the interaction between these risk factors to allay the health impacts of LSA [9]. On a micro-level, interventions could focus on counseling to build strategies to cope with experiences of sexual violence as well as address self-esteem, internalized sexual stigma, depression and STI prevention [9, 29]. Meso-level interventions could foster peer support and solidarity, and address family issues. To illustrate, support groups for survivors of LSA could address the particular needs of LBQ women who may have less social support from family due to sexual stigma.
On a macro-level, interventions could focus on enhanced competence among providers across a range of systems—educational, mental and sexual health, social services—to better support sexual minorities and provide referrals to LGBTQ community resources [9, 30]. Clinicians should practice from a trauma-informed approach that screens all patients for a history of sexual assault [14, 30]. For example, as LBQ women who have experienced LSA may be more likely to offer STI testing, sexual health clinics could screen patients for a history of sexual violence and provide resources for support and counseling. Practice competence must involve an understanding of the fluidity and multiplicity of sexual identities, such as queer, that are not captured in standard categorizations of lesbian, bisexual, gay or heterosexual identities [28, 29]. Programming should also promote empowerment and engage youth and others in advocacy [9]. Community-based approaches and interventions to challenge sexual stigma—and sexual violence—are urgently needed [14]. Putting into practice strategies that concomitantly build coping, address depression and STI risk, challenge sexual stigma within community norms and healthcare practice and reduce violence can promote health and wellbeing among sexual minority women.
Acknowledgements
We acknowledge all the women who participated and shared their time and experiences as PRAs and participants in the survey and focus group. We are also thankful for the E.D. and staff at Women’s Health in Women’s Hands Community Health Centre and Women’s College Research Institute. We thank the anonymous reviewers and Editor for constructive and thoughtful feedback.
Funding
Canadian Institutes of Health Research (CIHR) Social Research Centre (SRC) in HIV Prevention.
Conflict of interest statement
None declared.
References
- 1.King M, Semlyen J, Tai S, et al. A systematic review of mental disorder, suicide and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry. 2008;8:70. doi: 10.1186/1471-244X-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Logie C. The case for the World Health Organization’s Commission on the Social Determinants of Health to address sexual orientation. Am J Public Health. 2012;102:1243–6. doi: 10.2105/AJPH.2011.300599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129:674–97. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57:13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 5.Díaz RM, Ayala G, Bein E, et al. The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: findings from 3 US cities. Am J Public Health. 2001;91:927–32. doi: 10.2105/ajph.91.6.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts AL, Austin SB, Corliss HL, et al. Pervasive trauma exposure among US sexual orientation minority adults and risk of posttraumatic stress disorder. Am J Public Health. 2010;100:2433–41. doi: 10.2105/AJPH.2009.168971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balsam KF. Traumatic victimization in the lives of lesbian and bisexual women: a contextual approach. J Lesbian Stud. 2003;7:1–14. doi: 10.1300/J155v07n01_01. [DOI] [PubMed] [Google Scholar]
- 8.Bernhard LA. Physical and sexual violence experienced by lesbian and heterosexual women. Violence Against Women. 2000;6:69–78. [Google Scholar]
- 9.Friedman MS, Marshal MP, Guadamuz TE, et al. A meta-analysis of disparities in childhood sexual abuse, parental physical abuse, and peer victimization among sexual minority and sexual nonminority individuals. Am J Public Health. 2011;101:1481–4. doi: 10.2105/AJPH.2009.190009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hughes TL, Johnson T, Wilsnack SC. Sexual assault and alcohol abuse: a comparison of lesbians and heterosexual women. J Substance Abuse. 2011;13:515–32. doi: 10.1016/s0899-3289(01)00095-5. [DOI] [PubMed] [Google Scholar]
- 11.Lehavot K, Molina Y, Simoni JM. Childhood trauma, adult sexual assault, and adult gender expression among lesbian and bisexual women. Sex Roles. 2012;67:272–84. doi: 10.1007/s11199-012-0171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martin SL, Fisher BS, Warner TD, et al. Women’s sexual orientations and their experiences of sexual assault before and during university. Women's Health Issues. 2011;21:199–205. doi: 10.1016/j.whi.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Matthews AK, Hughes TL, Johnson T, et al. Prediction of depressive distress in a community sample of women: the role of sexual orientation. Am J Public Health. 2002;92:1131–9. doi: 10.2105/ajph.92.7.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rothman EF, Exner D, Baughman AL. The prevalence of sexual assault against people who identify as gay, lesbian, or bisexual in the Unites States: a systematic review. Trauma Violence Abuse. 2011;12:55–66. doi: 10.1177/1524838010390707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Basile K, Chen J, Lynberg M, et al. Prevalence and characteristics of sexual violence victimization. Violence Vict. 2007;22:437–48. doi: 10.1891/088667007781553955. [DOI] [PubMed] [Google Scholar]
- 16.Tjaden P, Thoennes N. Extent, Nature, and Consequences of Intimate Partner Violence: Findings from the National Violence Against Women Survey (No. NCJ 181867) Washington, DC: U.S. Department of Justice; 2000. [Google Scholar]
- 17.Krieger N. The ostrich, the albatross, and public health: an ecosocial perspective-or why an explicit focus on health consequences of discrimination and deprivation is vital for good science and public health practice. Public Health Rep. 2001;116:419–23. doi: 10.1093/phr/116.5.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poundstone KE, Strathdee SA, Celentano DD. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol Rev. 2004;26:22–35. doi: 10.1093/epirev/mxh005. [DOI] [PubMed] [Google Scholar]
- 19.Cochran SD, Mays VM. Burden of psychiatric morbidity among lesbian, gay and bisexual individuals in the California Quality of Life Survey. J Abnorm Psychol. 2009;118:647–58. doi: 10.1037/a0016501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frisell T, Lichenstein P, Rahman Q, et al. Psychiatric morbidity associated with same-sex sexual behaviour: influence of minority stress and familial factors. Psychol Med. 2010;40:315–24. doi: 10.1017/S0033291709005996. [DOI] [PubMed] [Google Scholar]
- 21.Lewis NM. Mental health in sexual minorities: recent indicators, trends and their relationship to place in North America and Europe. Health Place. 2009;15:1029–45. doi: 10.1016/j.healthplace.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 22.Bontempo DE, D’Augelli AR. Effects of at-school victimization and sexual orientation on lesbian, gay, or bisexual youths’ health risk behaviour. J Adolesc Health. 2002;30:364–74. doi: 10.1016/s1054-139x(01)00415-3. [DOI] [PubMed] [Google Scholar]
- 23.Herek GM. Confronting sexual stigma and prejudice: theory and practice. J Soc Issues. 2007;63:905–25. [Google Scholar]
- 24.Deacon H. Towards a sustainable theory of health-related stigma: lessons from the HIV/AIDS literature. J Community Appl Soc Psychol. 2006;16:418–25. [Google Scholar]
- 25.Roberts AL, Rosario M, Corliss HL, et al. Elevated risk of posttraumatic stress in sexual minority youths: mediation by childhood abuse and gender nonconformity. Am J Public Health. 2012;102:1587–93. doi: 10.2105/AJPH.2011.300530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gold SD, Marx BP, Lexington JM. Gay male sexual assault survivors: the relations among internalized homophobia, experiential avoidance, and psychological symptom severity. Behav Res Therapy. 2007;45:549–62. doi: 10.1016/j.brat.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 27.Gold S, Dickstein B, Marx B, et al. Psychological outcomes among lesbian sexual assault survivors: an examination of the roles of internalized homophobia and experiential avoidance. Psychol Women Q. 2009;33:54–66. [Google Scholar]
- 28.Roberts AL, Rosario M, Corliss HL, et al. Sexual orientation and functional pain in U.S. young adults: the mediating role of childhood abuse. PLoS ONE. 2013;8:e54702. doi: 10.1371/journal.pone.0054702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Austin SB, Roberts AL, Corliss H, et al. Sexual violence victimization history and sexual risk indicators in a community-based urban cohort of “mostly heterosexual” and heterosexual young women. Am J Public Health. 2008;98:1015–20. doi: 10.2105/AJPH.2006.099473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saewyc E, Skay C, Richens K, et al. Sexual orientation, sexual abuse, and HIV-risk behaviors among adolescents in the Pacific Northwest. Am J Public Health. 2006;96:1104–10. doi: 10.2105/AJPH.2005.065870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Girshick LB. No sugar, no spice: reflections on research on woman-to-woman sexual violence. Violence Against Women. 2002;8:1500–20. [Google Scholar]
- 32.Clark ME, Landers S, Linde R, et al. The GLBT health access project: a state-funded effort to improve access to care. Am J Public Health. 2001;91:895–6. doi: 10.2105/ajph.91.6.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wohl AR, Galvan FH, Myers HF, et al. Do social support, stress, disclosure and stigma influence retention in HIV care for Latino and African American men who have sex with men and women? AIDS Behav. 2011;15:1098–110. doi: 10.1007/s10461-010-9833-6. [DOI] [PubMed] [Google Scholar]
- 34.Bauer GR, Welles SL. Beyond assumptions of negligible risk: sexually transmitted diseases and women who have sex with women. Am J Public Health. 2001;91:1282–6. doi: 10.2105/ajph.91.8.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organisation, Statistics Netherland. Health Interview Surveys: Towards International Harmonization of Methods and Instruments. Copenhagen: WHO Regional Office for Europe; 1996. (WHO Regional Publications, European Series, no 58) [PubMed] [Google Scholar]
- 37.Sinclair VG, Wallston KA. The development and psychometric evaluation of the brief resilient coping scale. Assessment. 2004;11:94–101. doi: 10.1177/1073191103258144. [DOI] [PubMed] [Google Scholar]
- 38.Robins RW, Hendin HM, Trzesniewski KH. Measuring global self-esteem: construct validation of a single-item measure and the Rosenberg self-esteem scale. Pers Soc Psychol Bull. 2001;27:151–61. [Google Scholar]
- 39.Fishman SJ, Anderson EH. Perception of HIV and safer sexual behaviors among lesbians. J Assoc Nurses AIDS Care. 2003;14:48–55. doi: 10.1177/1055329003255591. [DOI] [PubMed] [Google Scholar]
- 40.Zimet GD, Dahlem NW, Zimet SG, et al. The multi-dimensional scale of perceived social support. J Pers Assess. 1998;52:30–41. [Google Scholar]
- 41.Kimerling R, Ouimette P, Wolf J. Gender and PTSD. New York: Guilford; 2002. [Google Scholar]
- 42.Allsworth JE, Anand MA, Redding CA, et al. Physical and sexual violence and incident sexually transmitted infections. J Womens Health. 2009;18:529–34. doi: 10.1089/jwh.2007.0757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Noell J, Rohde P, Seeley J, et al. Childhood sexual abuse, adolescent sexual coercion and sexually transmitted infection acquisition among homeless female adolescents. Child Abuse Negl. 2001;25:137–48. doi: 10.1016/s0145-2134(00)00223-4. [DOI] [PubMed] [Google Scholar]
- 44.Putnam FW. Ten-year research update review: child sexual abuse. J Am Acad Child Adolesc Psychiatry. 2003;42:269–78. doi: 10.1097/00004583-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 45.Logie CH, James L, Tharao W, et al. ‘We Don’t Exist’: a qualitative study of marginalization experienced by HIV-positive lesbian, bisexual, queer and transgender women in Toronto, Canada. J Int AIDS Soc. 2012;15:17392–403. doi: 10.7448/IAS.15.2.17392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marrazzo JM. Dangerous assumptions: Lesbians and sexual death. Sex Transm Dis. 2005;32:570–1. doi: 10.1097/01.olq.0000175368.82940.61. [DOI] [PubMed] [Google Scholar]
- 47.Goldfriend MR, Goldfried AP. The importance of parental support in the lives of gay, lesbian, and bisexual individuals. J Clin Psychol. 2001;57:681–93. doi: 10.1002/jclp.1037. [DOI] [PubMed] [Google Scholar]
- 48.Ryan C, Huebner D, Diaz RM, et al. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123:346–52. doi: 10.1542/peds.2007-3524. [DOI] [PubMed] [Google Scholar]
- 49.Elliot AN, Carnes CN. Reactions of nonoffending parents to the sexual abuse of their child: a review of the literature. Child Maltreat. 2011;6:314–31. doi: 10.1177/1077559501006004005. [DOI] [PubMed] [Google Scholar]
- 50.Logie CH, Gibson M. A mark that is no mark? Queer women and violence in HIV discourse. Cult Health Sex. 2013;15:29–43. doi: 10.1080/13691058.2012.738430. [DOI] [PubMed] [Google Scholar]
- 51.Garofalo R, Wolf RC, Kessel S, et al. The association between health risk behaviors and sexual orientation among a school-based sample of adolescents. Pediatrics. 1998;101:895–902. doi: 10.1542/peds.101.5.895. [DOI] [PubMed] [Google Scholar]
- 52.Russell ST, Driscoll AK, Truong N. Adolescent same-sex romantic attractions and relationships: implications for substance use and abuse. Am J Public Health. 2002;92:198–202. doi: 10.2105/ajph.92.2.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.City of Toronto. Toronto’s Racial Diversity. Available at: http://www.toronto.ca/toronto_facts/diversity.htm. Accessed: 1 September 2013. [Google Scholar]
- 54.City of Toronto. 2011 National Household Survey: Labour Force, Education, Place of Work, Commuting and Mobility. Available at: www.toronto.ca/demographics/pdf/nhs_backgrounder.pdf. Accessed: 1 September 2013. [Google Scholar]
- 55.Meyer IH, Wilson PA. Sampling lesbian, gay and bisexual populations. J Couns Psychol. 2009;56:23–31. [Google Scholar]
- 56.Cohn TJ, Hastings SL. Resilience among rural lesbian youth. J Lesbian Stud. 2010;14:71–9. doi: 10.1080/10894160903060325. [DOI] [PubMed] [Google Scholar]
- 57.Fergus S, Zimmerman MA. Adolescent resilience: a framework for understanding healthy development in the face of risk. Annu Rev Public Health. 2005;26:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]


