Abstract
Background/Aims
Recently, many cases of vitamin K-dependent coagulopathy of unknown origin have been reported. Such patients lack any relevant family history and have no systemic disease, raising suspicion of superwarfarin intoxication. We evaluated individual risk factors causing coagulopathy and hemorrhagic symptoms in patients with suspected superwarfarin intoxication. In addition, we determined how to effectively treat vitamin K-dependent coagulopathy caused by suspected superwarfarin intoxication.
Methods
Seven patients with suspected superwarfarin intoxication who lacked any definitive history of rodenticide ingestion were included. Thirty-one patients initially diagnosed with rodenticide poisoning were also included. We performed a retrospective chart review of all subjects and examined clinical data including patient demographics and medical histories.
Results
Patients initially diagnosed with rodenticide poisoning were divided into two groups, one of which had a laboratory abnormality (prothrombin time [PT] > 13 seconds) and another group with PTs in the normal range. There was no significant difference between the two groups in any of age, gender, the extent of chronic alcohol consumption, the causative rodenticide, psychiatric problems, ingestion of drugs interacting with warfarin, the extent of intoxication, or the type of ingestion attempt. The albumin level of the former group was significantly lower than that of the latter group (p = 0.014). Furthermore, a significant difference between the two groups was evident in terms of simultaneous ingestion of rodenticide and alcohol (p = 0.023).
Conclusions
Most patients with superwarfarin poisoning did not exhibit any complication. When such complications were evident, they were associated with serum albumin level and coingestion of rodenticide and alcohol.
Keywords: Vitamin K deficiency bleeding, Brodifacoum, Poisoning
INTRODUCTION
Recently, many cases of vitamin K-dependent coagulopathy of unknown origin have been reported. Relevant family history is lacking and systemic disease absent [1,2]. Such cases are suggestive of superwarfarin intoxication. However, most patients have no definitive history of rodenticide poisoning. Many case reports suggest that patients manifested Munchausen syndrome, or had developed rodenticide intoxication via a nonoral route, such as inhalation or absorption through the skin [1,3,4]. However, such theories do not explain individual variations in the symptoms of, or coagulopathies among, the various cases, and no report has yet addressed individual risk factors for superwarfarin intoxication.
In the present study, we sought to evaluate individual risk factors causing coagulopathy and hemorrhagic symptoms in patients suspected of superwarfarin intoxication. In addition, in the absence of any consensus, we sought to describe an effective treatment for vitamin K-dependent coagulopathy in patients lacking evidence of definitive rodenticide poisoning who presented to a single center.
METHODS
Subjects
Between October 2009 and April 2012, we treated seven patients with suspected superwarfarin intoxication who lacked definitive histories of rodenticide ingestion. All were admitted to our hospital with complaints of various hemorrhagic events and were diagnosed with vitamin K-dependent coagulopathies after measurement of coagulation factor levels. Six were evaluated in terms of serum brodifacoum levels, which confirmed superwarfarin intoxication despite the lack of any definitive history of such intoxication.
In addition, 31 patients were diagnosed with rodenticide poisoning in Chosun University Hospital from January 2006 to March 2013. All had definitive clinical histories of ingestion of superwarfarin-type rodenticides. We analyzed the incidence of coagulopathy in these patients, and evaluated associated factor(s), via statistical analysis.
Methods
We performed a retrospective chart review of all seven subjects mentioned above, and examined clinical data, patient information, and medical histories; comparing these with those of the 31 patients with definitive rodenticide intoxication.
Diagnosis of brodifacoum intoxication was confirmed by high-performance liquid chromatography (HPLC) featuring brodifacoum detection via ultraviolet light absorption. We also noted comedications (principally warfarin-interacting drugs), alcohol consumption habits, histories of psychiatric illness and consultation, and the presence of genetic factors (the cytochrome P450 2C9 [CYP2C9] and the vitamin K epoxide reductase complex subunit 1 [VKORC1] alleles), to detect risk factors.
Statistical analysis
A probability p value < 0.05 was considered to indicate a significant difference. All statistical analyses were performed using SPSS version 21.0 (IBM Co., Armonk, NY, USA). Differences between continuous variables were analyzed using Student t test and those between categorical variables employing the chi-square test.
RESULTS
Baseline characteristics of patients with definitive rodenticide intoxication
We studied a total of 31 patients (19 males and 12 females) of median age 48 years (range, 2 to 88). The poisoning agents were brodifacoum (n = 21), flocumafen (n = 5), bromodiolone (n = 2), coumatetralyl (n = 1), and unknown (n = 2). Thirteen patients had psychiatric conditions including depressive disorders (n = 5), intellectual disabilities (n = 5), a cognitive impairment (n = 1), an adjustment disorder (n = 1), or another condition (n = 1). Eleven patients (35.5%) had histories of ingestion of agents that probably interact with warfarin, including antidepressants (selective serotonin reuptake inhibitors [SSRIs], tricyclic antidepressants [TCAs]; n = 6); nonsteroidal anti-inflammatory drugs (NSAIDs) (n = 3); antiplatelet agents (n = 3); and antacids (cimetidine, ranitidine; n = 2). Two patients abused herbal treatment(s). No patient had a history of hepatitis or liver cirrhosis. Ten patients were accidentally exposed to rodenticide, whereas 21 ingested rodenticide to attempt suicide.
The mean amount of ingested rodenticide was 0.79 mg (range, 0.2 to 2), with one tablet containing 0.2 mg. However, those who ingested over 10 tablets could not accurately report how much rodenticide they had ingested, because of their psychological conditions. Notably, rodenticide and alcohol were simultaneously ingested by 11 patients (35.5%).
Only one patient (3.2%) had hemorrhagic symptoms (hematuria and hematoma). However, 11 of the 31 patients (35.5%) had a laboratory abnormality (prothrombin time [PT] > 13 seconds) attributable to rodenticide intoxication. Laboratory data (international normality ratio > 1.5) revealed that only four patients had coagulopathies (12.9%). Upon chart review, the basal PT (pre-ingestion or post-follow-up) in all cases of rodenticide intoxication was within the normal range (under 13 seconds). PT prolongation (to over 13 seconds) may be caused by such intoxication.
Therefore, to evaluate individual risk factors causing coagulopathy, patients were divided into two groups: those with a laboratory abnormality (PT > 13 seconds), and the others.
The general characteristics of the 31 study subjects, all of whom had acute rodenticide poisoning symptoms at presentation, are summarized in Table 1.
Table 1.
General characteristics of the 31 study subjects presenting with acute rodenticide poisoning
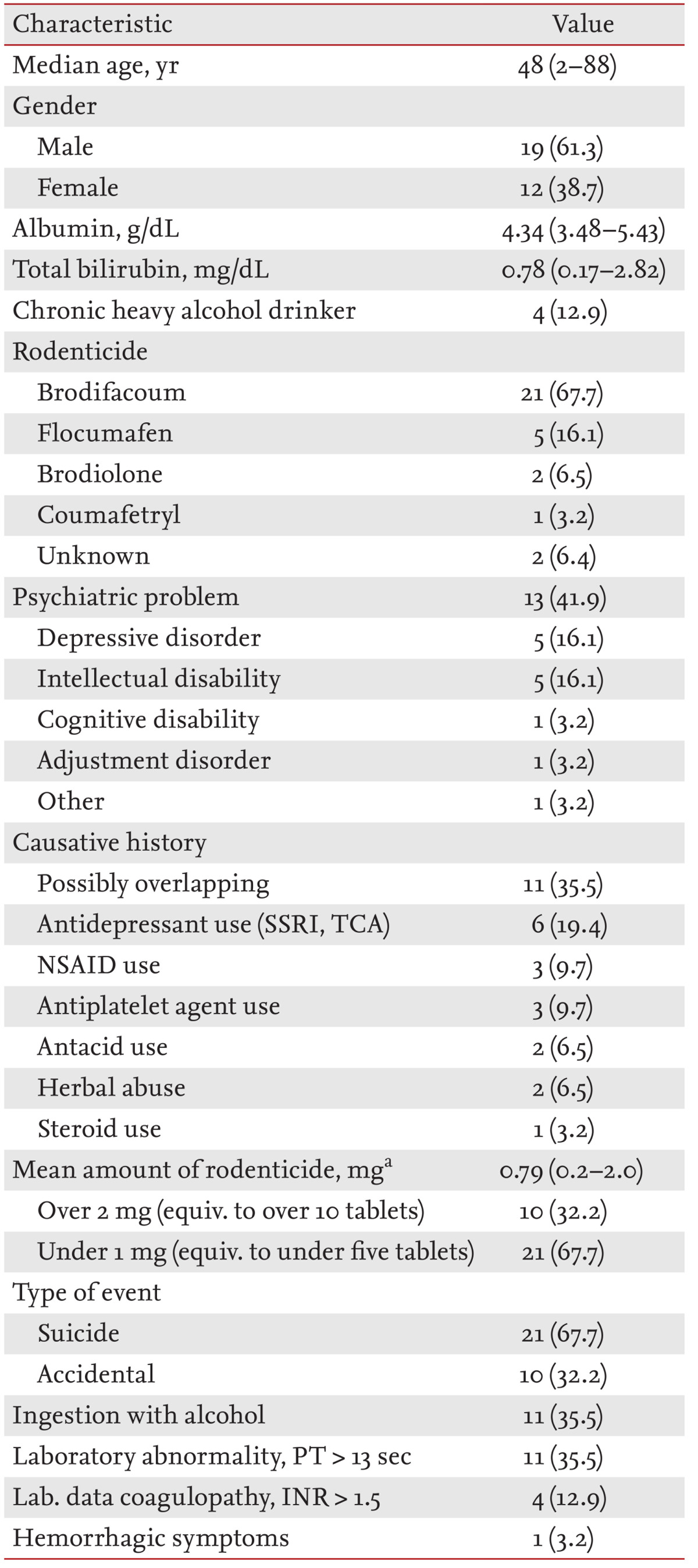
Values are presented as median (range) or number (%).
SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant; NSAID, nonsteroidal anti-inflammatory drug; equiv., equivalent; PT, prothrombin time; INR, international normality ratio.
aEach tablet has 0.2 mg at 0.005% (w/w).
Comparison of clinical characteristics between the two groups
There was no significant difference between the two groups in terms of age, gender, the extent of chronic alcohol consumption, the rodenticide agent present, psychiatric problems, the taking of warfarin-interacting drugs, the extent of intoxication, or the type of poisoning. However, in the PT > 13 seconds group, the albumin level (4.06 g/dL) was significantly lower than that of the other group (4.53 g/dL; p = 0.014). Furthermore, a significant between-group difference was evident in terms of simultaneous rodenticide ingestion and alcohol consumption (p = 0.023). This may be a significant risk factor for coagulopathy and development of hemorrhagic symptoms in patients suspected of superwarfarin intoxication.
In summary, the two groups differed significantly in serum albumin level and a history of rodenticide ingestion with alcohol (Table 2).
Table 2.
Comparison of clinical characteristics between the group with a laboratory abnormality (prothrombin time > 13 sec) and the other group
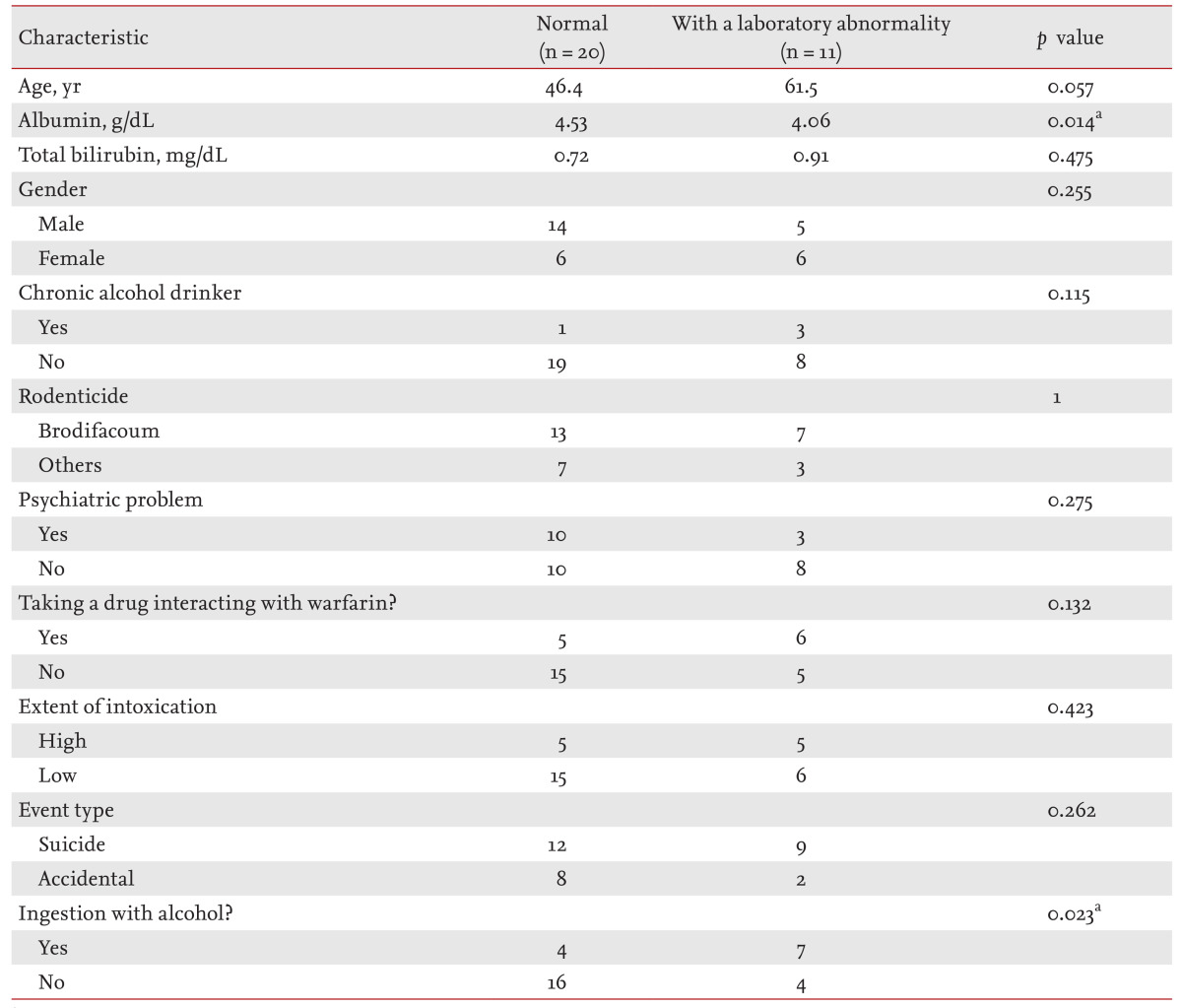
ap < 0.05.
Baseline characteristics of patients suspected of superwarfarin intoxication but lacking definitive histories of rodenticide ingestion
All seven patients were admitted to our hospital with various hemorrhagic symptoms and were diagnosed with vitamin K-dependent coagulopathies based on evaluation of the levels of coagulation factors. The seven patients (four males and three females) ranged from 38 to 81 years of age, with a median age of 64 years. The principal hemorrhagic events were bleeding gums (four patients), epistaxis (three patients), hematuria (one patient), hematoma formation (one patient), and hematochezia (one patient). All patients had prolonged PTs and activated partial thromboplastin times (aPTTs). The plasma-mixing test was performed for all patients and the activities of coagulation factors measured. All patients were similar; the PTs and aPTTs were abnormal and the levels of factors II, VII, IX, and X reduced. Serum brodifacoum tests were run on six of the seven patients (all except patient 1), and the results were positive. Two patients (patients 1 and 7) lived in the city and the others in nonurban areas. Three patients (patients 2, 4, and 5) were farmers; two were housekeepers (patients 3 and 7); one was a salesman (patient 1); and one was a demolition worker (patient 6). However, the two housekeepers also worked on farms on a daily basis (patients 3 and 7). No patient had a history of hepatitis or liver cirrhosis. One patient had schizophrenia, but none had Munchausen syndrome based on a review of psychiatric history and consultations (however, patient 1 was not assessed). One patient had well-controlled depression that developed after a cerebral stroke (patient 2: treated with a TCA, valproic acid, ranitidine, and aspirin); one well-controlled schizophrenia (patient 3: treated with a SSRI); one severe asthma (patient 4: treated with oral and inhaled steroid); and one Parkinson disease (patient 5: treated with an SSRI).
Three patients (patients 1, 2, and 3) had taken various herbal medications of unknown origin. In particular, patient 3 experienced two episodes of coagulopathy after taking the same herbal preparation, suggesting that the medication may have contained warfarin or a warf arin-interacting component. However, we were unable to obtain a sample of the material to explore this suggestion further. Three patients (patients 1, 4, and 6) were chronic heavy drinkers, especially patient 6, who had been diagnosed with chronic alcoholic hepatitis.
Four patients were subjected to CYP2C9 and VKORC1 1173C/T genotyping, but all were wild-type at the CYP2C9 locus. Interestingly, two patients had the VKORC1 1173C/T allele (which is well-known to reduce warfarin activity), but no patient had the CYP2C9*2, CYP2C9*3, or VKORC1 1639 G/A allele, which are well known to enhance warfarin activity and trigger hemorrhagic complications.
Finally, environmental exposure was a possible cause of intoxication in five patients who were full-time (patients 2, 4, and 5) or part-time farmers (patients 3 and 7). The poison may have been absorbed through the skin. Patient 7, who was a demolition worker, may have been exposed to various superwarfarins via inhalation. Environmental exposure and herbal medication were other possible sources of exposure to superwarfarins. Chronic alcohol ingestion, the taking of various drugs interacting with warfarin, and the use of herbal medications, may have induced coagulopathies.
All patients were initially given fresh frozen plasma (FFP), followed by various (high) intravenous doses of vitamin K (10 to 40 mg). Two patients (patients 1 and 6) were transferred to another hospital and became lost to follow-up. Treatment of the other patients (except for patient 7) was later changed to oral vitamin K. Patient 7 was given intravenous vitamin K until discontinuation of vitamin therapy because the oral route was difficult to access. Total treatment duration varied but, for most patients, was over 6 months.
Information on patients' characteristics, symptoms, and treatments is summarized in Tables 3 and 4.
Table 3.
Patients with vitamin K-dependent coagulopathy presumed to be caused by exposure to brodifacoum
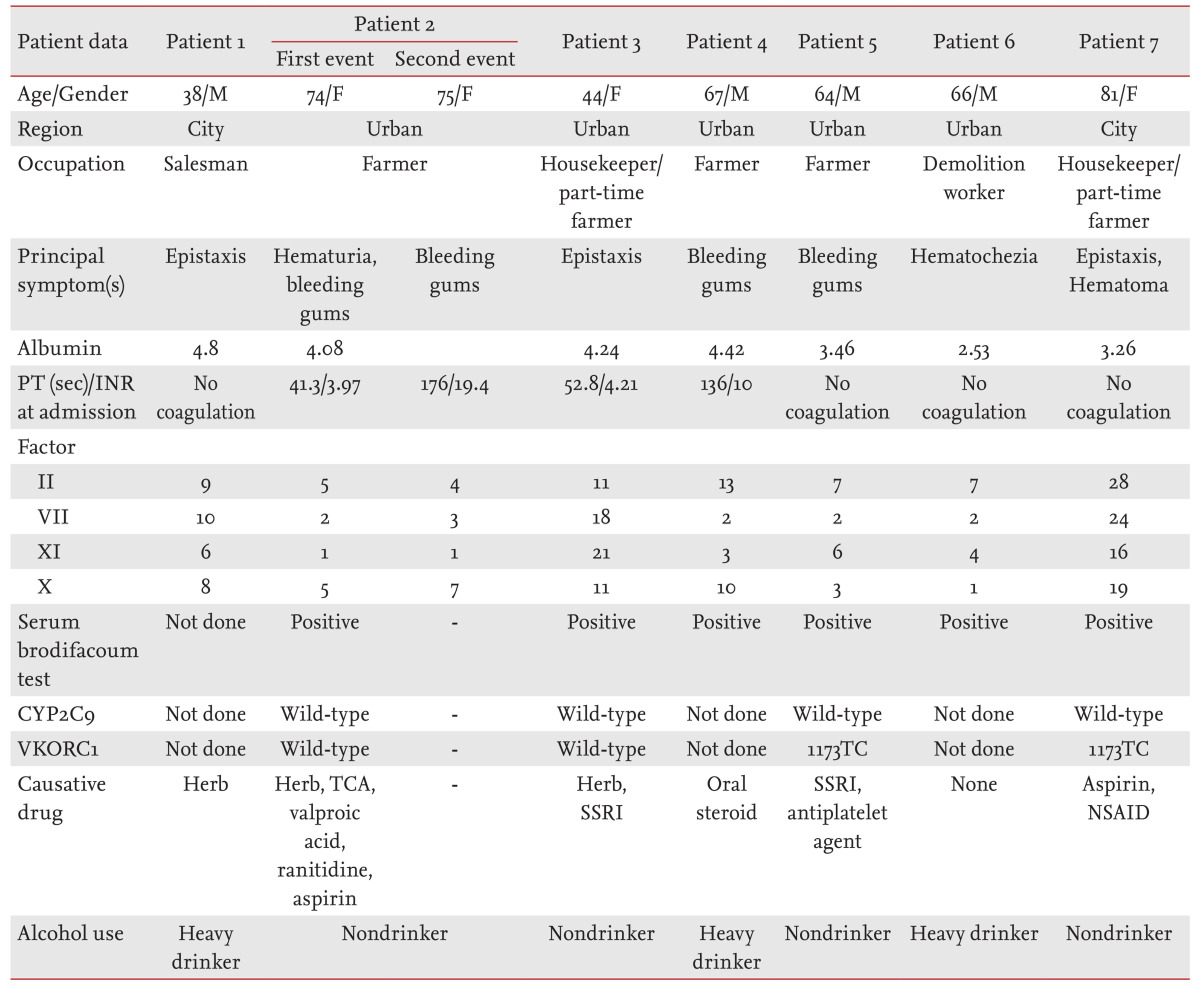
M, male; F, female; PT, prothrombin time; INR, international normality ratio; CYP2C9, cytochrome P450 2C9; VKORC1, vitamin K epoxide reductase complex subunit 1; TCA, tricyclic antidepressant; SSRI, selective serotonin reuptake inhibitor; NSAID, nonsteroidal anti-inflammatory drug.
Table 4.
Patients with vitamin K-dependent coagulopathy presumed to be associated with exposure to brodifacoum
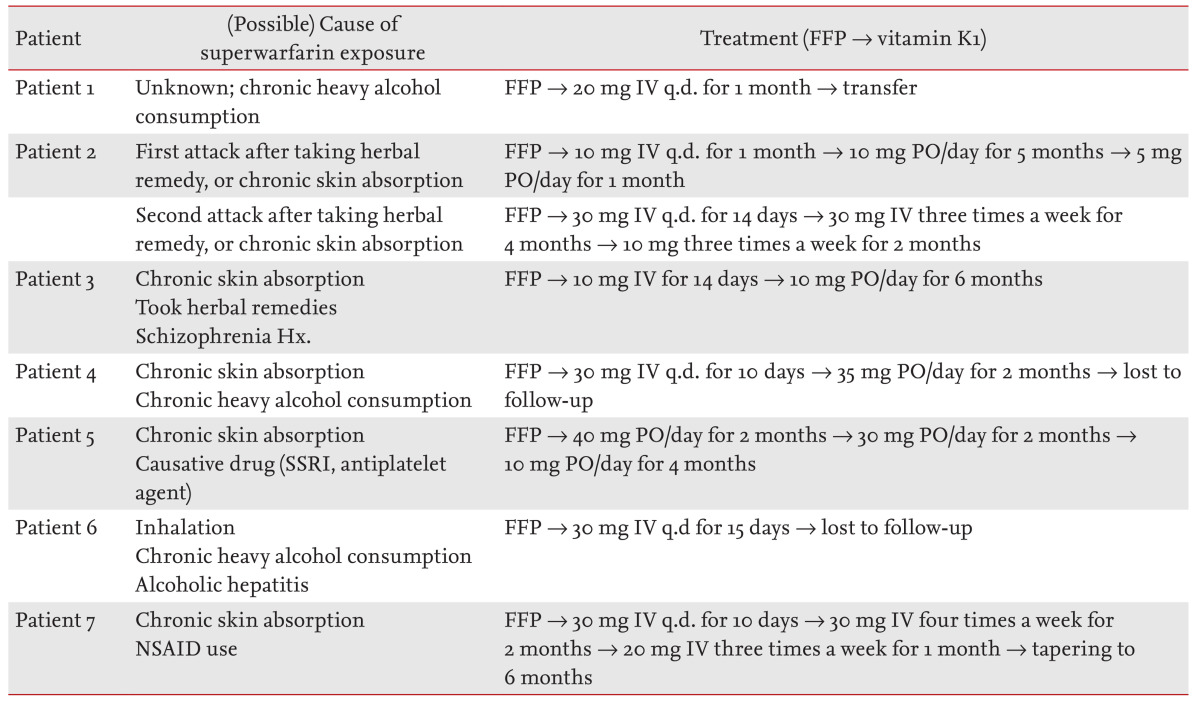
FFP, fresh frozen plasma; IV, intravenous; q.d., queque die (every day); PO, per os (by mouth); SSRI, selective serotonin reuptake inhibitor; NSAID, nonsteroidal anti-inflammatory drug.
DISCUSSION
Rodenticides are a heterogeneous group of compounds, the toxicities of which differ markedly in humans and rodents. Many rodenticides have been used throughout history. Before the mid-20th century, heavy metals (arsenic, thallium) were most frequently employed. Since that time, second-generation anticoagulant rodenticides including brodifacoum, diffnacoum, bromdialone, counatetralyl, and the latest (Food and Drug Administration-approved) agent flocumafen, have been the mainstays of rodenticide products. These agents are long-acting warfarin derivatives termed superwarfarins, are tasteless and colorless, are used as poisons, and are still marketed as pesticides to kill rats and mice [1,2,5,6].
Superwarfarins are popular and readily available, but may cause intoxication upon overexposure, triggering coagulopathy, or abnormal bleeding. This is an important public health problem. Most ingestions are accidental, and many patients are children. However, attempted suicide, ingestion associated with psychiatric disorders, and deliberate self-poisoning with denial (Munchausen syndrome), have been reported [7,8,9]. Superwarfarin intoxication via the oral route is well known, but it remains unclear how warfarin enters the sera of patients without any history of oral ingestion. However, some cases of poisoning caused by inhalation or direct skin contact have been reported [3,4].
Superwarfarin-type rodenticides act like warfarin, reducing γ-carboxylation of vitamin K-dependent clotting factors by inhibiting vitamin K 2, 3-epoxide reductase. Such inhibition triggers coagulopathy manifesting as increases in the PT and aPTT, and reductions in the levels of vitamin K-dependent clotting factors (factor II, VII, IX, and X; protein C; protein S; and antithrombin III). Most superwarfarin-type rodenticides have a considerably longer half-life than warfarin (at least 16 to 69 days), are 100-fold more potent, and have a more rapid onset of action, because phenyl groups replace the terminal methyl group in the warfarin structure. The increased efficacy of superwarfarins as rodenticides is attributable to high-level lipid solubility, a high affinity for hepatic tissue, and extremely slow elimination from the body [10,11,12].
The most common clinical feature of superwarfarin intoxication is bleeding from any mucosal site or organ. Epistaxis and gingival bleeding, gastrointestinal and pulmonary hemorrhage, hematoma, and/or hematuria, may be evident [13].
In a patient with a definitive history of superwarfarin ingestion, PT and aPTT are the optimal screening tests. However, in those presenting with a vitamin K-dependent coagulation factor deficiency of unknown cause, diagnosis of superwarfarin-induced coagulopathy can be difficult. A definitive diagnosis requires a blood test featuring the use of HPLC. This accurately measures superwarfarin levels, but the technology is not yet widely available. However, if superwarfarin intoxication is suspected, and the test is not readily available, high-dose vitamin K may be administered empirically [14,15].
Most patients presenting with superwarfarin exposure or poisoning do not exhibit or develop major complications. The 2009 Annual Report of the American Association of Poison Control Centers' National Poison Data System stated that 11,091 instances of long-acting anticoagulant rodenticide exposure had been reported to United State Poison Control Centers in that year. However, the outcomes were generally benign. One death, and 36 and 12 instances of moderate and major clinical effects, respectively, were described (0.4%) [5]. Only 35.5% of cases were associated with coagulopathy as measured in the laboratory, and symptomatic complications were rare (3.2%).
However, the LD50 (i.e., the dose causing 50% of a group to die) of warfarin in humans is unknown; only animal data are available. Also, the human ED50 level (the dose effective in 50% of a group) is unknown [4,11,12,13]. In fact, the toxic dose of brodifacoum varies widely among individuals, as reflected by variations in the half-life. Thus, brodifacoum metabolism may differ individually, but this remains unclear. The mechanism of action of the superwarfarins is the same as that of warfarin [10,11,16,17].
Usually, warfarin therapy is associated with a significant risk of bleeding complications because the warfarin therapeutic index is narrow. It is well known that certain factors increase the risk of over-anticoagulation. Such factors are 1) impaired liver function and hypoalbuminemia; 2) alcohol consumption; 3) drug-drug interactions; and 4) genetic polymorphisms (CYP2c9 and VKORC1) affecting the levels or activities of enzymes metabolizing warfarin [18,19].
First, anticoagulants accumulate principally in the liver. Superwarfarins exhibit high liver to serum concentration ratios (ca. 20:1 in rats) because the rodenticides are very lipid-soluble and exhibit an affinity for hepatic tissue. Thus, impaired liver function may trigger symptoms of superwarfarin poisoning [11,17,20].
Warfarin is extensively protein-bound (97% to 99%, when albumin levels are > 3.2 mg/100 mL), and only the free drug exerts any biological effects. When albumin levels are low, the amount of free warfarin thus increases. Hence, such patients generally require less warfarin. As the albumin level rises, the warfarin maintenance dose also rises. Thus, hypoalbuminemia may trigger increased warfarin activity and symptoms of coagulopathy [18,21].
The anticoagulant effect of warfarin is dramatically altered by ingestion of even small amounts of alcohol. In those taking warfarin and ingesting a few alcoholic drinks in a single sitting, the anticlotting effects may become greater than medically required, placing the patient at risk of increased bleeding. Such excessive warfarin action is the result of alcohol-related inhibition of warfarin metabolism by liver cytochrome P450. Conversely, in those who chronically consume alcohol, long-term cytochrome P450 is constitutively activated and warfarin metabolism thus permanently affected. Warfarin is metabolized more rapidly than normal in such subjects, and higher warfarin doses are generally required to achieve the desired anticoagulant effects [22,23].
Drug-drug interactions are of major concern, triggering adverse drug reactions in patients under warfarin treatment. Comedications may inhibit the hepatic P450 system, triggering hemorrhagic symptoms. Such medications include SSRIs, NSAIDs, metronidazole, and cimetidine [24,25,26,27,28,29,30].
Finally, genetic screens have identified two genes responsible for most of the genetic effect; these are the CYP2C9 allele (encoding CYP2C9 that metabolizes S-warfarin) and VKORC1 (encoding the target of warfarin; vitamin K epoxide reductase). Certain loss-of-function CYP2C9 and VKORC1 polymorphisms are known to be associated with reductions in enzymatic activity and, thus, an increased risk of hemorrhage. These alleles are CYP2C9*2 (Cysl44/Ile359), CYP2C9*3 (Argl44/Leu359), and VKORC1 (.1639 G>A) [31,32]. Furthermore, certain patients have CYP2C9 poor metabolizer alleles and experience rates of major bleeding 3.68-fold higher than those of patients with the wild-type gene. Therefore, in known carriers of variant CYP2C9 alleles, the initial loading dose of warfarin should be reduced to as little as 10% of the standard recommendation. The VKORC 1639 G>A allele is associated with increased warfarin activity. On the other hand, the VKORC1 1173 C>T variant causes partial resistance to warfarin, and very high doses are thus required to obtain therapeutic effects [31,32,33,34,35,36,37,38,39,40].
Treatment options for superwarfarin intoxication include administration of vitamin K1, FFP, and/or a prothrombin complex concentrate. If a patient has active bleeding, or is at a high risk of bleeding, FFP transfusions are given. Administration of recombinant factor VIIa also controls acute bleeding. However, the effect of either treatment is short-lived. After controlling bleeding, patients with prolonged PTs and aPTTs should be given high doses of vitamin K to normalize the coagulopathy. The optimal dose and duration of vitamin K1 therapy have yet to be established. However, early tapering or discontinuation will cause repeat prolongation of PT and aPTT even after normal values have been attained [11,41,42,43]. Our experience supports the use of multiple treatments (daily oral or intermittent intravenous vitamin K); prolonged treatment (for a minimum of 6 months if hemorrhagic symptoms are evident); and high-dose (10 to 60 mg) vitamin K1 supplementation.
To date, no report has identified risk factors for superwarfarin intoxication or discussed suspected superwarfarin intoxication in patients without definitive histories of rodenticide ingestion. This is the first report to detail individual risk factors, to investigate routes of poisoning other than the oral, and to explore treatments for superwarfarin intoxication especially in those without definitive histories of ingestion.
We found that albumin levels and simultaneous ingestion of rodenticide and alcohol may be associated with coagulopathy. Superwarfarin may be ingested with alcohol in a single sitting, or rodenticide may be chronically absorbed through the skin or via inhalation.
To our knowledge, no previous report has identified individual risk factors for development of coagulopathy or hemorrhagic symptoms, or has sought to identify the source of exposure, in patients suspected of superwarfarin intoxication.
Further studies are required to ascertain whether albumin level, acute or chronic alcohol consumption, and use of herbal medications, are important in the context of superwarfarin poisoning.
KEY MESSAGE
Most patients with superwarfarin poisoning do not exhibit any complications.
Complications of superwarfarin poisoning may be associated with serum albumin level and simultaneous ingestion of rodenticide and alcohol.
The serum brodifacoum test should be performed to identify vitamin K-dependent coagulopathy in adult patients even in the absence of a definitive history of rodenticide poisoning.
The source of exposure in patients exhibiting superwarfarin toxicity of unknown origin may be long-term transdermal absorption or inhalation.
The CYP2C9 and VKORC1 genotypes were not noted among our 31 subjects, despite the fact that these mutations are well-known sensitizers to warfarin poisoning.
Chronic heavy alcohol drinkers may be at risk of hemorrhagic complications because of chronic rodenticide absorption from the skin, or via respiration.
In cases with hemorrhagic complications, the optimal route of vitamin K administration is initially intravenous, followed by a later change to the oral route. However, if oral vitamin K cannot be easily obtained (in Korea, oral vitamin K is no longer on sale), intravenous vitamin K can be given every other day. Regardless of modality, treatment should be continued for at least 6 months.
Acknowledgments
This work was supported by a grant from the Clinical Medicine Research Institute of the Chosun University Hospital (2013).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Hong J, Yhim HY, Bang SM, et al. Korean patients with superwarfarin intoxication and their outcome. J Korean Med Sci. 2010;25:1754–1758. doi: 10.3346/jkms.2010.25.12.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rauch AE, Weininger R, Pasquale D, et al. Superwarfarin poisoning: a significant public health problem. J Community Health. 1994;19:55–65. doi: 10.1007/BF02260521. [DOI] [PubMed] [Google Scholar]
- 3.Abell TL, Merigian KS, Lee JM, Holbert JM, McCall JW., 3rd Cutaneous exposure to warfarin-like anticoagulant causing an intracerebral hemorrhage: a case report. J Toxicol Clin Toxicol. 1994;32:69–73. doi: 10.3109/15563659409000432. [DOI] [PubMed] [Google Scholar]
- 4.Kim HY, Jeon HJ, Ko BS, Lee KH, Kim ST. Two cases of brodifacoum poisoning from inhalation route. Korean J Hematol. 1996;31:473–479. [Google Scholar]
- 5.Hadler MR, Shadbolt RS. Novel 4-hydroxycoumarin anticoagulants active against resistant rats. Nature. 1975;253:275–277. doi: 10.1038/253275a0. [DOI] [PubMed] [Google Scholar]
- 6.Chua JD, Friedenberg WR. Superwarfarin poisoning. Arch Intern Med. 1998;158:1929–1932. doi: 10.1001/archinte.158.17.1929. [DOI] [PubMed] [Google Scholar]
- 7.Pavlu J, Harrington DJ, Voong K, Savidge GF, Jan-Mohamed R, Kaczmarski R. Superwarfarin poisoning. Lancet. 2005;365:628. doi: 10.1016/S0140-6736(05)17916-1. [DOI] [PubMed] [Google Scholar]
- 8.Lipton RA, Klass EM. Human ingestion of a 'superwarfarin' rodenticide resulting in a prolonged anticoagulant effect. JAMA. 1984;252:3004–3005. [PubMed] [Google Scholar]
- 9.Bronstein AC, Spyker DA, Cantilena LR, Jr, Green JL, Rumack BH, Giffin SL. 2009 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 27th Annual Report. Clin Toxicol (Phila) 2010;48:979–1178. doi: 10.3109/15563650.2010.543906. [DOI] [PubMed] [Google Scholar]
- 10.Park BK, Leck JB. A comparison of vitamin K antagonism by warfarin, difenacoum and brodifacoum in the rabbit. Biochem Pharmacol. 1982;31:3635–3639. doi: 10.1016/0006-2952(82)90587-1. [DOI] [PubMed] [Google Scholar]
- 11.Bachmann KA, Sullivan TJ. Dispositional and pharmacodynamic characteristics of brodifacoum in warfarin-sensitive rats. Pharmacology. 1983;27:281–288. doi: 10.1159/000137881. [DOI] [PubMed] [Google Scholar]
- 12.Bruno GR, Howland MA, McMeeking A, Hoffman RS. Long-acting anticoagulant overdose: brodifacoum kinetics and optimal vitamin K dosing. Ann Emerg Med. 2000;36:262–267. doi: 10.1067/mem.2000.108317. [DOI] [PubMed] [Google Scholar]
- 13.Hui CH, Lie A, Lam CK, Bourke C. 'Superwarfarin' poisoning leading to prolonged coagulopathy. Forensic Sci Int. 1996;78:13–18. doi: 10.1016/0379-0738(95)01835-2. [DOI] [PubMed] [Google Scholar]
- 14.Wu YF, Chang CS, Chung CY, Lin HY, Wang CC, Shen MC. Superwarfarin intoxication: hematuria is a major clinical manifestation. Int J Hematol. 2009;90:170–173. doi: 10.1007/s12185-009-0374-6. [DOI] [PubMed] [Google Scholar]
- 15.Jin MC, OuYang XK, Chen XH. High-performance liquid chromatography coupled with electrospray ionization tandem mass spectrometry for the determination of flocoumafen and brodifacoum in whole blood. J Appl Toxicol. 2007;27:18–24. doi: 10.1002/jat.1179. [DOI] [PubMed] [Google Scholar]
- 16.Olmos V, Lenzken SC, del Carmen Paz M, et al. Quantification of brodifacoum, bromadiolone and difenacoum in human serum by HPLC with ultraviolet and fluorometric detection. Acta Toxicol Argent. 2004;12:9–14. [Google Scholar]
- 17.Watt BE, Proudfoot AT, Bradberry SM, Vale JA. Anticoagulant rodenticides. Toxicol Rev. 2005;24:259–269. doi: 10.2165/00139709-200524040-00005. [DOI] [PubMed] [Google Scholar]
- 18.Eason CT, Murphy EC, Wright GR, Spurr EB. Assessment of risks of brodifacoum to non-target birds and mammals in New Zealand. Ecotoxicology. 2002;11:35–48. doi: 10.1023/a:1013793029831. [DOI] [PubMed] [Google Scholar]
- 19.Wadelius M, Pirmohamed M. Pharmacogenetics of warfarin: current status and future challenges. Pharmacogenomics J. 2007;7:99–111. doi: 10.1038/sj.tpj.6500417. [DOI] [PubMed] [Google Scholar]
- 20.Makris M, Watson HG. The management of coumarin-induced over-anticoagulation Annotation. Br J Haematol. 2001;114:271–280. doi: 10.1046/j.1365-2141.2001.02908.x. [DOI] [PubMed] [Google Scholar]
- 21.O'Bryan SM, Constable DJ. Quantification of brodifacoum in plasma and liver tissue by HPLC. J Anal Toxicol. 1991;15:144–147. doi: 10.1093/jat/15.3.144. [DOI] [PubMed] [Google Scholar]
- 22.Kaminsky LS, Zhang ZY. Human P450 metabolism of warfarin. Pharmacol Ther. 1997;73:67–74. doi: 10.1016/s0163-7258(96)00140-4. [DOI] [PubMed] [Google Scholar]
- 23.Lieber CS. Alcohol and the liver: 1994 update. Gastroenterology. 1994;106:1085–1105. doi: 10.1016/0016-5085(94)90772-2. [DOI] [PubMed] [Google Scholar]
- 24.Weathermon R, Crabb DW. Alcohol and medication interactions. Alcohol Res Health. 1999;23:40–54. [PMC free article] [PubMed] [Google Scholar]
- 25.Schalekamp T, Klungel OH, Souverein PC, de Boer A. Increased bleeding risk with concurrent use of selective serotonin reuptake inhibitors and coumarins. Arch Intern Med. 2008;168:180–185. doi: 10.1001/archinternmed.2007.32. [DOI] [PubMed] [Google Scholar]
- 26.Dalton SO, Sorensen HT, Johansen C. SSRIs and upper gastrointestinal bleeding: what is known and how should it influence prescribing? CNS Drugs. 2006;20:143–151. doi: 10.2165/00023210-200620020-00005. [DOI] [PubMed] [Google Scholar]
- 27.Greenblatt DJ, von Moltke LL, Harmatz JS, Shader RI. Drug interactions with newer antidepressants: role of human cytochromes P450. J Clin Psychiatry. 1998;59(Suppl 15):19–27. [PubMed] [Google Scholar]
- 28.Choi KH, Kim AJ, Son IJ, et al. Risk factors of drug interaction between warfarin and nonsteroidal anti-inflammatory drugs in practical setting. J Korean Med Sci. 2010;25:337–341. doi: 10.3346/jkms.2010.25.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Reilly RA. Comparative interaction of cimetidine and ranitidine with racemic warfarin in man. Arch Intern Med. 1984;144:989–991. [PubMed] [Google Scholar]
- 30.Hungin AP, Rubin GP, O'Flanagan H. Co-prescription of H2 receptor blockers and proton pump inhibitors with warfarin in general practice. Postgrad Med J. 1999;75:721–722. doi: 10.1136/pgmj.75.890.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rost S, Fregin A, Ivaskevicius V, et al. Mutations in VKORC1 cause warfarin resistance and multiple coagulation factor deficiency type 2. Nature. 2004;427:537–541. doi: 10.1038/nature02214. [DOI] [PubMed] [Google Scholar]
- 32.D'Andrea G, D'Ambrosio RL, Di Perna P, et al. A polymorphism in the VKORC1 gene is associated with an interindividual variability in the dose-anticoagulant effect of warfarin. Blood. 2005;105:645–649. doi: 10.1182/blood-2004-06-2111. [DOI] [PubMed] [Google Scholar]
- 33.Rettie AE, Korzekwa KR, Kunze KL, et al. Hydroxylation of warfarin by human cDNA-expressed cytochrome P-450: a role for P-4502C9 in the etiology of (S)-warfarin-drug interactions. Chem Res Toxicol. 1992;5:54–59. doi: 10.1021/tx00025a009. [DOI] [PubMed] [Google Scholar]
- 34.Higashi MK, Veenstra DL, Kondo LM, et al. Association between CYP2C9 genetic variants and anticoagulation-related outcomes during warfarin therapy. JAMA. 2002;287:1690–1698. doi: 10.1001/jama.287.13.1690. [DOI] [PubMed] [Google Scholar]
- 35.Li T, Chang CY, Jin DY, Lin PJ, Khvorova A, Stafford DW. Identification of the gene for vitamin K epoxide reductase. Nature. 2004;427:541–544. doi: 10.1038/nature02254. [DOI] [PubMed] [Google Scholar]
- 36.Gage BF, Eby C, Johnson JA, et al. Use of pharmacogenetic and clinical factors to predict the therapeutic dose of warfarin. Clin Pharmacol Ther. 2008;84:326–331. doi: 10.1038/clpt.2008.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gage BF, Lesko LJ. Pharmacogenetics of warfarin: regulatory, scientific, and clinical issues. J Thromb Thrombolysis. 2008;25:45–51. doi: 10.1007/s11239-007-0104-y. [DOI] [PubMed] [Google Scholar]
- 38.Visser LE, van Vliet M, van Schaik RH, et al. The risk of overanticoagulation in patients with cytochrome P450 CYP2C9*2 or CYP2C9*3 alleles on acenocoumarol or phenprocoumon. Pharmacogenetics. 2004;14:27–33. doi: 10.1097/00008571-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Steward DJ, Haining RL, Henne KR, et al. Genetic association between sensitivity to warfarin and expression of CYP2C9*3. Pharmacogenetics. 1997;7:361–367. doi: 10.1097/00008571-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 40.Aithal GP, Day CP, Kesteven PJ, Daly AK. Association of polymorphisms in the cytochrome P450 CYP2C9 with warfarin dose requirement and risk of bleeding complications. Lancet. 1999;353:717–719. doi: 10.1016/S0140-6736(98)04474-2. [DOI] [PubMed] [Google Scholar]
- 41.Schalekamp T, Brasse BP, Roijers JF, et al. VKORC1 and CYP2C9 genotypes and phenprocoumon anticoagulation status: interaction between both genotypes affects dose requirement. Clin Pharmacol Ther. 2007;81:185–193. doi: 10.1038/sj.clpt.6100036. [DOI] [PubMed] [Google Scholar]
- 42.Spahr JE, Maul JS, Rodgers GM. Superwarfarin poisoning: a report of two cases and review of the literature. Am J Hematol. 2007;82:656–660. doi: 10.1002/ajh.20784. [DOI] [PubMed] [Google Scholar]
- 43.Zupancic-Salek S, Kovacevic-Metelko J, Radman I. Successful reversal of anticoagulant effect of superwarfarin poisoning with recombinant activated factor VII. Blood Coagul Fibrinolysis. 2005;16:239–244. doi: 10.1097/01.mbc.0000169215.70184.56. [DOI] [PubMed] [Google Scholar]


