Abstract
This study aimed to develop and validate a method to measure bolus flow time (BFT) through the esophagogastric junction (EGJ) using a high-resolution impedance-manometry (HRIM) sleeve. Ten healthy subjects were studied with concurrent HRIM and videofluoroscopy; another 15 controls were studied with HRIM alone. HRIM studies were performed using a 4.2-mm-outer diameter assembly with 36 pressure sensors at 1-cm intervals and 18 impedance segments at 2-cm intervals (Given Imaging, Los Angeles, CA). HRIM and fluoroscopic data from four barium swallows, two in the supine and two in the upright position, were analyzed to create a customized MATLAB program to calculate BFT using a HRIM sleeve comprising three sensors positioned at the crural diaphragm. Bolus transit through the EGJ measured during blinded review of fluoroscopy was almost identical to BFT calculated with the HRIM sleeve, with the nadir impedance deflection point used as the signature of bolus presence. Good correlation existed between videofluoroscopy for measurement of upper sphincter relaxation to beginning of flow [R = 0.97, P < 0.001 (supine) and R = 0.77, P < 0.01 (upright)] and time to end of flow [R = 0.95, P < 0.001 (supine) and R = 0.82, P < 0.01 (upright)]. The medians and interquartile ranges (IQR) of flow time though the EGJ in 15 healthy subjects calculated using the virtual sleeve were 3.5 s (IQR 2.3–3.9 s) in the supine position and 3.2 s (IQR 2.3–3.6 s) in the upright position. BFT is a new metric that provides important information about bolus transit through the EGJ. An assessment of BFT will determine when the EGJ is open and will also provide a useful method to accurately assess trans-EGJ pressure gradients during flow.
Keywords: manometry, impedance, bolus transit
the primary role of the esophagus is transport of food from the mouth into the stomach; perturbations in this function can lead to dysphagia, regurgitation, or aspiration. Thus the evaluation of bolus transit is crucial to the management and understanding of esophageal diseases. Until recently, bolus transit was primarily evaluated using fluoroscopy to visualize esophageal transit of various radiopaque materials. Radiographic observations assessing esophageal physiology were critical in developing an understanding of esophageal disorders, and this tool remains an important component of esophageal function testing (1).
In 1994, Fass et al. (2) described a technique utilizing an application of Ohm's law to study bolus transit by assessing electrical impedance along a catheter placed within the esophagus. This technique was shown to provide a reasonably accurate assessment of bolus transit of various liquid and viscous boluses through the esophagus and was later combined with manometry to obtain a comprehensive assessment of motor function and bolus transit without radiation exposure (2, 6, 14). Studies utilizing impedance-manometry added insight into the disconnect between peristaltic function and bolus transit and also highlighted the delicate balance between esophagogastric junction (EGJ) dysfunction and peristaltic integrity and vigor in determining bolus transit (16).
Although impedance-manometry provided a measure of bolus transit time, it did not provide an accurate assessment of bolus transit through the EGJ, as the sensors did not have the requisite spatial resolution. In 2005, our research group applied a methodology incorporating high-resolution impedance along a 6-cm sleeve sensor to investigate EGJ opening during deglutitive relaxation and reflux events (12). Using concepts of bolus transit adapted from esophageal studies (13), we were able to distinguish EGJ opening from EGJ relaxation and also to detect periods of bolus transit through the EGJ. However, the technique was not validated against simultaneous fluoroscopy, and the use of water perfusion in the region of the impedance recording sites could obscure the distinction between the mucosa and liquid transit.
Given recent advances in high-resolution manometry and impedance technology, we sought to determine whether our previous paradigms could be adapted to better assess EGJ opening and determine the time periods of trans-EGJ flow. This information could be helpful in refining measurements of intrabolus pressure (IBP) and EGJ opening dynamics in EGJ dysfunction. Thus our goal was to develop a new high-resolution impedance-manometry (HRIM) sleeve measurement of trans-EGJ flow and to test this measurement against simultaneous fluoroscopy.
METHODS
Subjects
The ability of HRIM to quantify bolus flow time (BFT) through the EGJ was tested by comparison with concurrent fluoroscopic imaging using a 50% barium-50% saline mixture in 10 healthy subjects [4 men, mean age 28 yr (range 21–47 yr)]. HRIM studies without fluoroscopy were performed in an additional 15 healthy subjects [7 men, mean age 33 yr (range 20–50 yr)] to define normative values for trans-EGJ BFT using swallowed saline. Volunteers, who were recruited by advertisement or word of mouth, had no history of gastrointestinal symptoms or surgery. The study protocol was approved by the Northwestern University Institutional Review Board, and informed consent was obtained from each subject.
Study Protocol
Concurrent HRIM and videofluoroscopy studies were done during two barium swallows (5 ml of thin barium with 50% saline) in supine and upright positions after a ≥6-h fast. The HRIM catheter was a 4.2-mm-outer diameter solid-state assembly with 36 circumferential pressure sensors at 1-cm intervals and 18 impedance segments at 2-cm intervals (Given Imaging, Los Angeles, CA). The transducers were calibrated at 0 and 300 mmHg using externally applied pressure. The assembly was placed transnasally and positioned to record from the hypopharynx to the stomach with about three intragastric pressure sensors. Fluoroscopic imaging and HRIM data were acquired simultaneously using the HRIM video system (V. model A400, Given Imaging), which synchronizes the fluoroscopic image with manometric data during acquisition. Fluoroscopy was performed with a multipurpose X-ray system (Siemens, Artis MP). This information was displayed on a computer screen in real time and stored on a hard drive for further analysis. The HRIM protocol without fluoroscopy included a 5-min baseline recording and ten 5-ml swallows in the supine position and five 5-ml swallows in the upright position using 50% saline for test swallows at 20- to 30-s intervals.
Data Analysis
Impedance changes through the EGJ during bolus transit.
Video images from the barium swallows were reviewed by two investigators (J.E.P. and F.N.) using ManoView software (ESO 3.0, Given Imaging) for synchronous display of the images with cursor-defined time points on the HRIM color topography plots and impedance line traces. For each swallow, the fluoroscopically defined times of barium movement through the EGJ were examined and analyzed independently. The following time measures were recorded (Fig. 1): time from the onset of upper esophageal sphincter relaxation to the beginning of trans-EGJ flow (i), time from the onset of upper esophageal sphincter relaxation to the end of trans-EGJ flow (ii), and intervals during which trans-EGJ flow was occurring between points i and ii (iii; Fig. 1B, pink horizontal bars). These time points were superimposed on impedance traces spaced 1 cm apart, with the distal sensor localized within the EGJ at the hiatus (Fig. 1A). Although the impedance sensors were 2 cm apart, this spacing length allowed correlation with the manometry sensors. This sensor configuration also optimized the assessment of bolus flow through the hiatus during swallowing by ensuring that at least one sensor would be colocalized with the lower esophageal sphincter during swallow-induced esophageal shortening. The impedance characteristics that correlated with fluoroscopic evidence of trans-EGJ flow were analyzed to develop a measurement of bolus presence through the EGJ. Although a 50% drop in impedance is associated with bolus contact through the esophageal body, the mucosal contact with the catheter through the EGJ is more extensive. Thus we sought to determine whether the same criteria were consistent with bolus presence through the EGJ. We manually assessed the impedance measurement associated with onset of bolus transit through the EGJ and compared this measurement with the baseline impedance before the swallow and the nadir impedance value during the deglutitive window. We also assessed the timing of the drop in impedance through the EGJ, so that we could determine that these changes were consistent with antegrade movement. This was accomplished by analyzing the progression through the HRIM sleeve. The same process was performed for the offset of bolus transit.
Fig. 1.
Methodology for analyzing impedance and manometric correlates of bolus transit through the esophagogastric junction (EGJ). A: esophageal pressure topography (EPT) of a single swallow with overlaid impedance traces through the EGJ from sensors 31–33 [high-resolution impedance manometry (HRIM) sleeve], with the corresponding impedance values (kΩ) shown as white numerals. B: pressure traces through the HRIM sleeve at sensors 31–33. Simultaneous fluoroscopic images are from the times shown as white circles on the impedance trace in A, positioned at the crural diaphragm on the EPT plot, and the lines extending from the circles onto the manometric panel. Time points of interest (i, ii, and iii) are documented at the top of the EPT plot (A), and areas of flow are shown as horizontal pink bars (B). This layout provides an opportunity to visualize impedance and manometry correlates of bolus presence and transit during a single swallow. At baseline, resting EGJ pressure is 25 mmHg and impedance is 2.2 kΩ. Impedance does not change dramatically after upper esophageal sphincter relaxation (i), and flow does not occur until the point shown by the black circle, when impedance reaches its nadir deflection (0.26 kΩ) and a preferential pressure gradient is noted through the EGJ into the stomach. There is no evidence of flow during the impedance drop at the 50% mark (1.1 kΩ), and this correlates with EGJ relaxation. Flow stops during the crural contraction (blue pressure trace), where peak contractions are 27 and 26 mmHg. This shift of the crural diaphragm signal among the sensors is consistent with typical axial sensor changes during swallowing. Flow continues after the crural contraction returns to baseline pressure.
Flow permissive pressure through the EGJ during bolus transit.
The same approach used to assess impedance characteristics indicative of bolus transit was utilized to assess pressure measurements during bolus transit (Fig. 1B). A short virtual EGJ sleeve was created using three sensors spaced 1 cm apart, with the distal sensor within the EGJ at the hiatus. Pressure characteristics concordant with bolus transit were analyzed to determine the pressure relationships associated with bolus transit. Specifically, we focused on the time at which flow was interrupted by inspiratory crural contractions, as this would potentially close the EGJ and also alter the flow gradient by increasing intragastric pressure. This was quantified by determining the pressure increase associated with flow interruption and return of flow.
Virtual HRIM sleeve for calculating BFT through the EGJ.
An automated HRIM virtual sleeve was created to simultaneously measure impedance and pressure and calculate BFT using the criteria developed for bolus presence in the EGJ and flow permissive pressure. This allowed an assessment of direction of bolus flow, as impedance drops from the top sensor to the bottom sensor would define direction. Additionally, a preferential flow gradient could be measured with the virtual sleeve by comparing the esophagogastric pressure gradient using the proximal sensor and a gastric pressure reference. The automated HRIM virtual sleeve was created by export of each subject's HRIM data from ManoView (Given Imaging) to MATLAB (MathWorks, Natick, MA) for further analysis using a MATLAB program. Three functional analytic steps were performed in this analysis.
OPTIMIZING RESOLUTION OF IMPEDANCE AND MANOMETRY.
For each test swallow, original pressure and impedance data were plotted in color contours and enhanced in the spatial dimension by interpolation using a cubic Hermite polynomial function to increase the spatial data by a factor of 10 for pressure data and 20 for impedance data, giving the impedance data the same resolution in the temporal and spatial domains as the pressure data.
DEFINING AN EGJ REGION OF INTEREST AND DOMAIN OF BOLUS PRESENCE.
From the superimposed pressure and impedance color contour plots, an EGJ region of interest (ROI), from 3 cm above to 2 cm below the crural diaphragm (CD) line and from 2 s prior to onset of swallowing to 12 s later, was defined. At all loci within the ROI, the mean baseline impedance was calculated to define domains where a 50% drop to zero occurred, indicative of bolus presence. These areas are highlighted and outlined by the solid white line in Fig. 2A and the dashed black box in Fig. 2B.
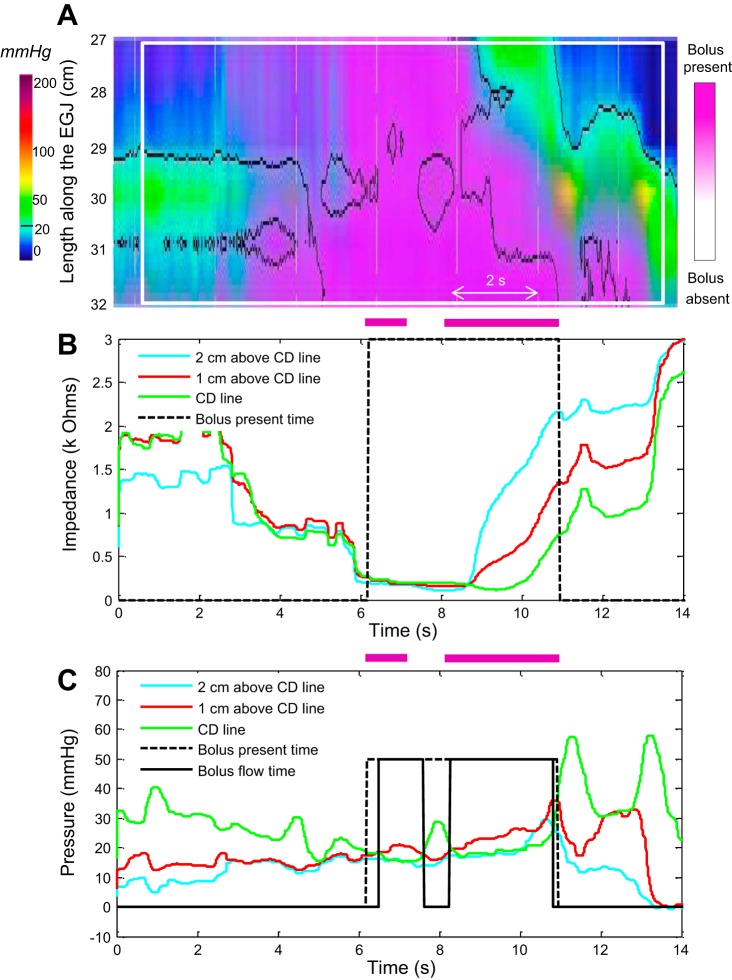
Fig. 2.
Methodology for derivation of trans-EGJ bolus flow time (BFT) from HRIM data. A: EGJ region of interest on an EPT plot centered on the EGJ. B and C: 3 impedance traces (B) and 3 pressure traces (C) from HRIM data beginning 2 s before upper esophageal sphincter relaxation used to identify bolus presence in the distal esophagus (black dashed lines) and BFT (black solid lines). Horizontal pink bars represent times of flow visualized on fluoroscopy. These times are closely synchronized with BFT domains. CD, crural diaphragm.
DERIVING BFT USING THE HRIM SLEEVE.
The criteria for defining BFT are based on our analysis of impedance and pressure changes through the ROI that were associated with bolus flow during simultaneous fluoroscopy. Hence, BFT was calculated by summing EGJ bolus presence time based on impedance and subtracting time periods during which flow was halted as determined by pressure recordings of crural activity (Fig. 2C).
Statistical Analysis
Values are medians and interquartile ranges (IQR). Nonparametric Wilcoxon's rank-sum test was used for comparison of BFT parameters between groups. Statistical significance was accepted when P < 0.05. Pearson's linear correlation was used for correlation analysis between actual BFT on fluoroscopy and BFT calculated with the automated HRIM sleeve algorithm.
RESULTS
Impedance Trace Changes Associated With Bolus Transit
Visual analysis suggested that a 50% reduction in the impedance trace from baseline through the EGJ was not associated with bolus transit and that trans-EGJ bolus flow was not confirmed until the impedance value dropped median 91% (IQR 89–94%) from baseline to nadir impedance. There was no significant difference in the median drop from baseline to nadir impedance when the upright swallows were compared with supine: 93% in the upright position vs. 89% in the supine position (P = 0.27). In addition, the 50% reduction in impedance appeared to be associated with EGJ relaxation and changes associated with loss of contact of the catheter with the mucosa during the initial phases of relaxation. The termination of bolus transit or offset of bolus transit was associated with a median 49% (IQR 31–120%) return to baseline through the CD. A significant difference in the median impedance percent return to baseline was associated with the end or offset of bolus transit when the upright swallows were compared with supine: 33% in the upright position vs. 62% in the supine position (P = 0.01). These criteria were incorporated into the algorithm for automated analysis of BFT.
Pressure Measurements Through the EGJ Associated With Bolus Transit
Visual analysis of bolus transit through the EGJ suggested that bolus transit required a preferential gradient where the pressure in the body of the esophagus below the contracting wave front is higher than or equal to the pressure at the CD. Thus crural contractions would interrupt flow once the pressure through the crura exceeded the esophageal body pressure. Flow was disrupted by a median rise of 10.2 mmHg (IQR 7.7–26.0 mmHg) above baseline pressure recorded at the CD location referenced to atmospheric pressure. This was a ∼50% rise toward the maximal crural contraction amplitude during inspiration. Flow restarted after a crural contraction when pressure returned to within −0.5 mmHg (IQR −2.5 to 2.4 mmHg) of baseline pressure, or a 50% decline from the maximal contraction to zero. These findings were incorporated into the algorithm for automated analysis of BFT.
Validation of the BFT Algorithm Against Fluoroscopy
A MATLAB BFT algorithm was created from the data validating appropriate impedance and pressure measures through the EGJ that correlated with bolus flow. The nadir deflection (90% drop in impedance) was used as the starting point of bolus presence at the EGJ, and a 50% return to baseline was used to signify the end of bolus presence at the EGJ. BFT was presumed to stop at a 50% increase in pressure above baseline to the maximal crural contraction as long as the absolute increase was ≥10 mmHg above baseline referenced to atmospheric pressure. Flow was deemed to restart once the crural contraction decreased to 50% of the maximal peak pressure.
A total of 40 swallows (4 per subject, 2 in the supine and 2 in the upright position) were analyzed from the 10 healthy subjects with concurrent fluoroscopic imaging and HRIM data. Bolus flow start and finish through the EGJ measured during blinded review of videofluoroscopy was almost identical to the start and finish of BFT calculated with the MATLAB algorithm (Table 1). Good correlation existed between videofluoroscopy for measurement of upper sphincter relaxation to beginning of flow [R = 0.97, P < 0.001 (supine); R = 0.77, P < 0.01 (upright)] and time to end of flow [R = 0.95, P < 0.001 (supine); R = 0.82, P < 0.01 (upright)]. In addition, the BFT in the supine position was, on average, only 0.27 s different from measured fluoroscopic flow time, and there was excellent correlation between the two (R = 0.87, P < 0.05). The overall average difference in flow time in the upright position was 0.33 s; however, the correlation was less linear (R = 0.67, P < 0.05).
Table 1.
Trans-EGJ BFT measured from videofluoroscopy and the virtual HRIM sleeve
| Supine |
Upright |
|||||
|---|---|---|---|---|---|---|
| Fluoroscopy | HRIM | R | Fluoroscopy | HRIM | R | |
| Flow onset, s | 5.49 (4.85–6.23) | 5.6 (4.84–6.32) | 0.97 | 4.25 (3.75–4.8) | 4.3 (3.67–4.6) | 0.77 |
| Flow offset, s | 10.4 (9.35–11.1) | 9.68 (8.8–10.7) | 0.95 | 8.10 (7.3–9.2) | 8.18 (7.53–8.72) | 0.82 |
| BFT, s | 4.35 (3.25–4.8) | 3.90 (3.0–4.64) | 0.87 | 3.6 (2.95–4.1) | 3.22 (2.74–3.73) | 0.67 |
Values are medians and interquartile ranges (IQR) from 10 subjects (20 supine and 20 upright swallows). Times are relative to upper sphincter relaxation. Bolus flow time (BFT) is equal to flow offset minus flow onset and time intervals excluded on pressure criteria. EGJ, esophagogastric junction; HRIM, high-resolution impedance-manometry; R, Pearson's correlation coefficient.
Normal Values of BFT Through EGJ in Asymptomatic Controls
The median BFT in 15 healthy subjects was 3.5 s (IQR 2.3–3.9 s) in the supine position and 3.2 s (IQR 2.3–3.6 s) in the upright position. These results were similar to those of the 10 healthy controls from concurrent HRIM and fluoroscopy studies. Of the 15 asymptomatic controls, 11 had normal peristalsis, 2 had weak peristalsis, and 2 had frequent failed peristalsis categorized by the Chicago Classification of Esophageal Motility. Subjects with normal peristalsis had significantly greater median BFT through the EGJ than subjects with peristaltic abnormalities in supine (3.7 vs. 2.3 s, P < 0.05) and upright (3.5 vs. 2.1 s, P < 0.05) positions.
On the basis of conventional line-tracing mode and the impedance color contour view analysis of HRIM data, 24 of 150 swallows in the supine position had incomplete bolus transit (IBT) and 14 of 75 swallows in the upright position had IBT. The mean BFT through the EGJ were significantly shorter for swallows with IBT in the supine and upright positions than for swallows with complete bolus transit (CBT): 3.78 vs. 1.73 s (P < 0.001) in the supine position and 3.40 vs. 1.39 s (P < 0.0001) in the upright position (Table 2). This finding was also associated with a significant correlation between BFT and distal contractile integral in the supine position (R = 0.66, P = 0.0017) and nearly significant correlation in the upright position (R = 0.44, P = 0.0535).
Table 2.
BFT for swallows with CBT and IBT
Values are medians and IQR of 150 swallows in the supine position [126 complete bolus transit (CBT) and 24 incomplete bolus transit (IBT)] and 75 swallows in the upright position (61 CBT and 14 IBT).
P < 0.001 vs. CBT.
DISCUSSION
This study developed and tested an interpretative algorithm for HRIM data to measure BFT through the EGJ. The algorithm utilized a virtual HRIM sleeve stipulating specific impedance and pressure characteristics as compatible with bolus flow and then compared the computation to trans-EGJ BFT measured from concomitant fluoroscopic recordings. Summary criteria used in the algorithm were as follows: 1) the nadir impedance deflection was taken as the initiation of trans-EGJ flow; 2) a 50% increase in impedance relative to baseline was taken as the termination of trans-EGJ flow; and 3) BFT was interrupted during periods characterized by a 50% pressure increase at the hiatus relative to the maximum increase, providing that the absolute increase was ≥10 mmHg. For the major findings of the study, correlation between BFT and fluoroscopic trans-EGJ flow time was excellent in the supine posture and good in the upright posture. BFT was then calculated in a set of 15 control subjects to establish normative median values: 3.5 s (IQR 2.3–3.9 s) in the supine position and 3.2 s (IQR 2.3–3.6 s) in the upright position.
Previous investigations from our laboratory first described HRIM as a technology to distinguish EGJ relaxation, defined manometrically, from EGJ opening, defined by impedance criteria of fluid or gas within the relaxed segment (12). However, those findings were not validated against fluoroscopy. Hence, we devised the current protocol, also in part driven by substantial technological advancements. Our previous recording assembly was a custom-built water-perfused device. The new protocol and analysis paradigm were adapted to a solid-state recording system utilizing a new generation of high-resolution manometry and impedance catheter. Applying this technology and verifying bolus presence by concurrent fluoroscopy, we found that bolus presence within the EGJ did not conform to the convention used in the esophageal body of a 50% reduction from baseline impedance. Rather, the impedance minimum, or nadir, was more accurate. This is consistent with other recent observations that the nadir impedance value correlated most strongly with barium area and bolus pressure dynamics in the esophageal body and upper sphincter (5, 8–10, 15). We now extend this observation to pertain to the EGJ as well.
Using the BFT calculation, we were also able to confirm our previous findings assessing pressure criteria for flow permissive time using high-resolution manometry with simultaneous fluoroscopy (3, 11). Our results confirm that a flow permissive pressure gradient is present when flow is occurring through the EGJ and that this is interrupted by crural contractions that are associated with pressures greater than the IBP in the distal esophagus. These findings are also consistent with previous studies of the influence of breathing pattern on healthy controls reporting that deep inspirations during swallowing cause transient interruptions of flow (7).
The BFT calculation facilitates an accurate measurement of the duration of EGJ opening and trans-EGJ bolus flow without the requirement of radiation. We propose that this new metric will be complementary to current methodologies for assessing EGJ function, as it is the first to incorporate the criteria of flow. BFT has direct implications with regard to the efficacy of a given esophagogastric pressure gradient in emptying the esophagus, as evidenced by shorter flow times associated with swallows associated with IBT. This association in asymptomatic controls may be due to the fact that the IBP generated by these weak swallows was not sufficient to generate flow through the EGJ, despite normal relaxation. This fact was supported by the correlation between distal contractile integral values and BFT. Alternatively, a short flow time could be a cause for IBT in patients with achalasia or an EGJ outflow obstruction. Hong et al. (4) utilized a similar concept to study the emptying mechanism in achalasia and found that flow across the EGJ was related to longitudinal muscle contraction with associated pressurization of the esophagus. Although their methodology did not quantify the duration of flow, the evidence provided in the study of Hong et al. confirmed that flow through the EGJ could be ascertained with HRIM.
Limitations to the technique described here could have an impact on our findings. 1) The impedance sensors were 2 cm apart; thus the impedance sleeve was an interpolated estimate of the impedance signal through the EGJ. Despite this limitation, we found excellent correlation between calculated and observed (fluoroscopy) bolus presence within the EGJ, suggesting that a higher-resolution device may not be required. 2) Our study population was healthy controls, and it is unclear whether the technique can be applied to study disease states, such as achalasia and nonobstructive dysphagia. Further study is required, and Hong et al. (4) provide encouraging data that it will be feasible. 3) A mild reduction in accuracy was observed in the upright position; however, this difference overall was small in terms of absolute time (0.33 s) and was probably related to the effect of gravity hastening bolus transit and a variable mixing of swallowed air with liquid at the EGJ. In the supine position, the phrenic ampulla tends to pool the liquid for longer periods of time, creating less opportunity for mixing.
In summary, BFT represents a unique measure of deglutitive EGJ function that may prove useful in the assessment of dysphagia. Development of this metric was the natural extension of work optimizing the interpretation of high-resolution impedance (12) and high-resolution manometry (3, 11) independently to assess bolus transit dynamics through the EGJ. We hypothesize that BFT may complement our existing strategy of assessing deglutitive EGJ function that focuses predominantly on relaxation pressure completeness and persistence, instead of opening. Future research to assess how the BFT measurement performs as an outcome measure is required, and intervention trials in achalasia, nonobstructive dysphagia, and large hiatal hernia would be optimal protocols for that evaluation.
GRANTS
This work was supported by National Institute of Diabetes and Digestive and Kidney Diseases Grants R01 DK-56033 (to P. J. Kahrilas) and R01 DK-079902 (to J. E. Pandolfino).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
AUTHOR CONTRIBUTIONS
Z.L., H.I., F.N., D.A.C., B.Y., and J.E.P. analyzed the data; Z.L., F.N., D.A.C., P.J.K., and J.E.P. interpreted the results of the experiments; Z.L. and J.E.P. prepared the figures; Z.L. and J.E.P. drafted the manuscript; Z.L., P.J.K., and J.E.P. edited and revised the manuscript; Z.L., H.I., F.N., D.A.C., C.-Y.L., B.Y., P.J.K., and J.E.P. approved the final version of the manuscript; C.-Y.L. performed the experiments; P.J.K. and J.E.P. are responsible for conception and design of the research.
REFERENCES
- 1. Dodds WJ. 1976 Walter B. Cannon Lecture: current concepts of esophageal motor function: clinical implications for radiology. Am J Roentgenol 128: 549–561, 1977 [DOI] [PubMed] [Google Scholar]
- 2. Fass J, Silny J, Braun J, Heindrichs U, Dreuw B, Schumpelick V, Rau G. Measuring esophageal motility with a new intraluminal impedance device. First clinical results in reflux patients. Scand J Gastroenterol 29: 693–702, 1994 [DOI] [PubMed] [Google Scholar]
- 3. Ghosh SK, Kahrilas PJ, Lodhia N, Pandolfino JE. Utilizing intraluminal pressure differences to predict esophageal bolus flow dynamics. Am J Physiol Gastrointest Liver Physiol 293: G1023–G1028, 2007 [DOI] [PubMed] [Google Scholar]
- 4. Hong SJ, Bhargave V, Jiang Y, Denboer D, Mittal RK. A unique esophageal motor pattern that involves longitudinal muscles is responsible for emptying in achalasia esophagus. Gastroenterology 139: 102–111, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Imam H, Marrero F, Shay S. Impedance nadir values correlate with barium bolus amount. Dis Esophagus 25: 600–607, 2012 [DOI] [PubMed] [Google Scholar]
- 6. Imam H, Shay S, Ali A, Baker M. Bolus transit patterns in healthy subjects: a study using simultaneous impedance monitoring, videoesophagram, and esophageal manometry. Am J Physiol Gastrointest Liver Physiol 288: G1000–G1006, 2005 [DOI] [PubMed] [Google Scholar]
- 7. Mittal RK, Shaffer HA, Parollisi S, Baggett L. Influence of breathing pattern on the esophagogastric junction pressure and esophageal transit. Am J Physiol Gastrointest Liver Physiol 269: G577–G583, 1995 [DOI] [PubMed] [Google Scholar]
- 8. Myers JC, Nguyen NQ, Jamieson GG, Van Hek JE'T, Ching K, Holloway RH, Dent J, Omari TI. Susceptibility to dysphagia after fundoplication revealed by novel automated impedance manometry analysis. Neurogastroenterol Motil 24: 812-e393, 2012 [DOI] [PubMed] [Google Scholar]
- 9. Nguyen NQ, Holloway RH, Smout AJ, Omari TI. Automated impedance-manometry analysis detects esophageal motor dysfunction in patients who have non-obstructive dysphagia with normal manometry. Neurogastroenterol Motil 25: 238-e164, 2013 [DOI] [PubMed] [Google Scholar]
- 10. Omari TI, Rommel N, Szczesniak MM, Fuentealba SE, Dinning PG, Davidson GP, Cook IJ. Assessment of intraluminal impedance for the detection of pharyngeal bolus flow during swallowing in healthy adults. Am J Physiol Gastrointest Liver Physiol 290: G183–G188, 2006 [DOI] [PubMed] [Google Scholar]
- 11. Pandolfino JE, Ghosh SK, Lodhia N, Kahrilas PJ. Utilizing intraluminal pressure gradients to predict esophageal clearance: a validation study. Am J Gastroenterol 103: 1898–1905, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pandolfino JE, Shi G, Zhang Q, Ghosh S, Brasseur JG, Kahrilas PJ. Measuring EGJ opening patterns using high resolution intraluminal impedance. Neurogastroenterol Motil 17: 200–206, 2005 [DOI] [PubMed] [Google Scholar]
- 13. Sifrim D, Castell DO, Dent J, Kahrilas PJ. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut 53: 1024–1031, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Srinivasan R, Vela MF, Katz PO, Tatuian R, Castell JA. Esophageal function testing using multichannel intraluminal impedance. Am J Physiol Gastrointest Liver Physiol 280: G457–G462, 2001 [DOI] [PubMed] [Google Scholar]
- 15. Szczesniak MM, Rommel N, Dinning PG, Fuentealba SE, Cook IJ, Omari TI. Optimal criteria for detecting bolus passage across the pharyngo-oesophageal segment during the normal swallow using intraluminal impedance recording. Neurogastroenterol Motil 20: 440–447, 2008 [DOI] [PubMed] [Google Scholar]
- 16. Tutuian R, Castell DO. Combined multichannel intraluminal impedance and manometry clarifies esophageal function abnormalities: study in 350 patients. Am J Gastroenterol 99: 1011–1019, 2004 [DOI] [PubMed] [Google Scholar]