Abstract
Sparganosis is a parasitic infestation of human by plerocercoid larvae. Sparganum is usually reported to be found in the subcutaneous tissues as well as other organs, including scrotum. However, testicular sparganosis is extremely rare, because of strong capsule of tunica albuginea. An urban-living 54-yr-old Korean man presented with left scrotal pain for 6 yr. Both testes look normal physically. Ultrasonography revealed poorly defined, heterogeneous mass with increased echogenicity in the left testis. This case was misdiagnosed as testicular tumor and underwent orchiectomy, but was diagnosed as testicular sparganosis by histopathology. Sparganosis should be included for differential diagnosis of testis tumor in countries where sparganosis is prevalent.
Graphical Abstract
Keywords: Sparganosis, Testis
INTRODUCTION
Sparganosis is a rare zoonotic disease of humans in Asia and South America, resulting from infection of plerocercoid larvae, sparganum, of the genus Spirometra. Humans are infected as aberrant hosts by ingesting raw or undercooked birds, chickens, rodents, wild pigs and other wild mammals or by drinking water containing infected copepods. Once spargana enter the human body, they readily migrate to various parts of the body, increasing in size and possibly undergoing multiplication. The most common sites of infection are beneath the skin of the abdomen and in the eyes. The brain, oral cavity, pleura, breast, skeletal muscle of the lower extremities, and scrotum were also rarely reported as sites of infection (1). The site of infection was known to be relatively soft or loose tissue. It is very rare in the testis parenchyma. There have been only 3 case reports of sparganosis in the testis worldwide (2, 3, 4). Our case was mistakenly considered as testicular tumor and received orchiectomy.
CASE DESCRIPTION
A 54-yr-old Korean man, who was a salaried office worker in Incheon, Korea, presented left scrotal pain for 6 yr in February 2009. The size and the general shape of the scrotum were within normal range, but intermittent pain has been the main symptom. The patient had no history of trauma or any scrotal operation. There was no history of hereditary disease or any other chronic disease except hypertension. No habit of ingesting raw reptiles such as snakes or frogs was reported. However, occasional drinking of not purified water from a spring during mountain climbing was revealed in the interview with the patient. The patient did not complain of fever or chilling sensation on the day of outpatient visit. There were no measurable weight loss, abdominal pain, and significant voiding difficulty. Only intermittent sharp and squeezing pain was present at the left testis. On the manual examination of testes, palpable mass, tenderness or redness, and wall thickening of the scrotum were not found. Laboratory tests were all within normal range, including complete blood count, blood chemistry, urinalysis, and testis-specific tumor markers. Ultrasonography of testis revealed a 0.4 × 0.5 × 0.4 cm sized poorly defined, heterogeneous mass with increased echogenicity in the left testis (Fig. 1A). No posterior acoustic shadowing was observed. Instead, another hypoechoic ring was identified around the mass (Fig. 1B) forming a "tubule-in-a-tubule" appearance. On the color Doppler examination, moderately increased flow was noted in the periphery of the mass. At the time testicular teratoma was strongly suspected by our radiologist. Radical orchiectomy was performed under the impression of left testis tumor. Under the spinal anesthesia, about 7 cm long left inguinal incision was made. A 15-mL sized round firm testis was identified. En bloc resection of the left testis was done after thorough exploration verifying no other structural abnormalities were present. On the second day after the operation, patient was discharged with oral antibiotic medication without complication. Pathological examination of the resected tissue showed the sparganum was present in the testicular parenchyma within tunica albuginea and surrounded by abscess and necrotic materials (Fig. 2A). And at close up view, tortuous recess of the bothrium, tegument, longitudinal layer of the smooth muscle, and loose internal stroma were seen and multiple calcarous bodies were present in the loose internal stroma (Fig. 2B). This finding was consistent with the diagnosis of sparganosis in the tesitis. Further treatment was not given to the patient.
Fig. 1.
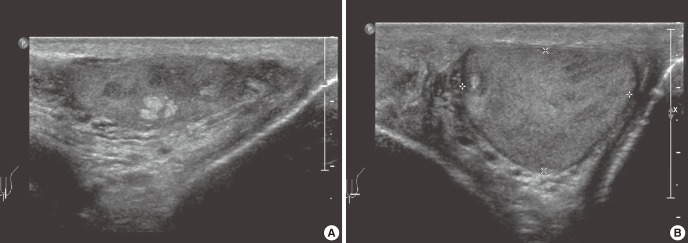
Ultrasonography of the left testis. (A) A 0.4 × 0.5 × 0.4 cm sized poorly defined, heterogeneous mass with increased echogenicity. (B) Hypoechoic ring identified around the mass forming a "tubule-in-a-tubule" appearance.
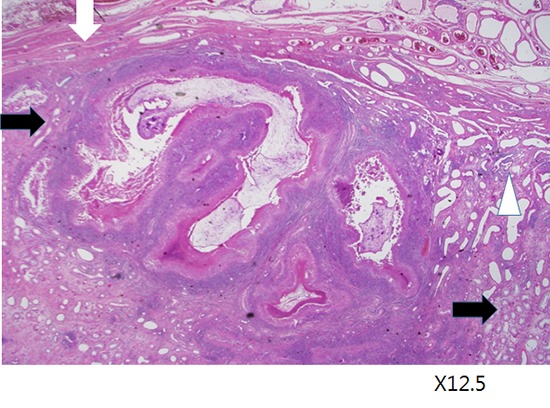
Fig. 2.
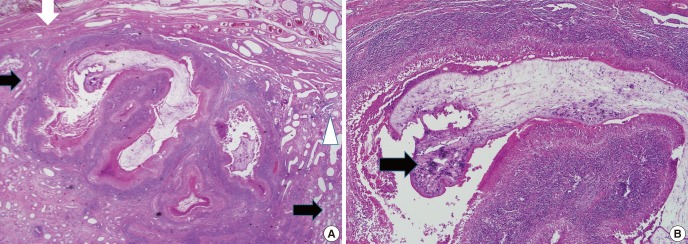
Histopathological findings of the left testis. (A) A sparganum surrounded by abscess and necrotic materials is present within the testicular parenchyma. White arrows indicate seminiferous tubules, a black arrow indicates tunica albuginea, and a white triangle rete testis (×12.5). (B) The sparganum shows tortous recess of the bothrium, tegument, longitudinal layer of the smooth muscle, and loose internal stroma and multiple calcarous bodies are present in the loose internal stroma (×40).
DISCUSSION
The present patient was a definite case of testicular sparganosis. The left scrotum was grossly normal before surgery and the testis showed no abnormal findings externally by surgery. Ultrasound image of the scrotum recognized a foreign body in the left testis. Furthermore, the histopathology of the left testis confirmed a sparganum which was embedded in the seminiferous tubule within the tunica albuginea. The sparganum demonstrated well-preserved typical structure of the tegument and parenchyma. One blunt end was compatible with the scolex of a sparganum. These gross views, ultrasound images, and the hisopathological findings indicated that the diagnosis of testicular sparganosis was correct.
Usually the patients with sparganosis come to the clinic with the painless, sometimes migratory mass. However, testicular pain was the chief complaint in our case and it was unusual. The pain was thought to be caused by surrounding abscess and necrotic materials within the testicular parencyhma which could elevate the pressure toward hard capsule, tunica albuginea.
The infection route of the sparganosis in this case was not clearly identified. In Korea there was a custom of eating live snake, especially during the military discipline period. Our patient does not have any experience of eating raw snake. The patient's hobby was mountain climbing. He had several experiences of drinking not purified water in the mountain. Possible route may be penetration through the abdominal wall after drinking of water contaminated with infected copepods. The plerocercoid is thought to invade the testis along the spermatic cord from the peritoneal cavity or abdominal wall.
In the aspect of treatment, surgical removal may remain the first choice (5). Oral antiparasitic drugs such as praziquantel, and gamma ray radiation might be partly effective (6). In this patient radical orchiectomy must have been excessive. At the time of diagnosis, sparganosis was not suspected to be a cause of the lesion. Percutaneous testicular biopsy is prohibited in case of testicular malignancy because it can hurt normal lymphatic pathway. Sometimes when other benign disease was suspected, surgical biopsy can be done after temporary clamping of spermatic cord in the operation field. Following the result of frozen biopsy surgical method, total or partial orchiectomy can be selected. If a surgeon has strong suspicion of testis tumor, surgical removal of the testis is a urological common practice.
Individual positive rate of ELISA in Korea was from 2.6% (1993) to 1.6% (2006) for sparganum (7). The sparganosis could be diagnosed with ELISA test and "tubule-in-a-tubule" appearance in ultrasonic finding. However, we did not perform ELIZA test for sparganum because sparganosis was not suspected and eosinophilia was absent. We could have had a chance to spare the testis by simply removing the worm if sparganosis had been diagnosed before the surgery. However, the testicular sparganosis is extremely rare and clinical presentation was unusual in this case. The lesson from this report is that we should include the sparganosis for differential diagnosis of testis tumor in countries where sparganosis was prevalent.
Footnotes
Funding: This study was supported by Inha University Research Grant.
References
- 1.Nithiuthai S, Anantaphruti MT, Waikagul J, Gajadhar A. Waterborne zoonotic helminthiases. Vet Parasitol. 2004;126:167–193. doi: 10.1016/j.vetpar.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 2.Kim DS, Park HJ, Kim SY, Kim SI, Lee TY, Park MH. Sparganosis in the testis. Korean J Urol. 2001;42:883–885. [Google Scholar]
- 3.Lee SY, Bae IH, Han GS, Cha SH, Kim SJ, Park KS, Song HK. A case of testis sparganosis. J Korean Soc Med Ultrasound. 2004;23:147–150. [Google Scholar]
- 4.Sakamoto T, Gutierrez C, Rodriguez A, Sauto S. Testicular sparganosis in a child from Uruguay. Acta Trop. 2003;88:83–86. doi: 10.1016/s0001-706x(03)00171-2. [DOI] [PubMed] [Google Scholar]
- 5.Lho YS, Kim HS, Yang SK. A case of sparganosis of the scrotum. Korean J Urol. 2001;42:263–264. [Google Scholar]
- 6.Sohn WM, Hong ST, Chai JY, Lee SH. Infectivity of the sparganum treated by praziquantel, gamma-irradiation and mechanical cutting. Korean J Parasitol. 1993;31:135–139. doi: 10.3347/kjp.1993.31.2.135. [DOI] [PubMed] [Google Scholar]
- 7.Lee MK, Hong SJ, Kim HR. Seroprevalence of tissue invading parasitic infections diagnosed by ELISA in Korea. J Korean Med Sci. 2010;25:1272–1276. doi: 10.3346/jkms.2010.25.9.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]


