Abstract
Background
Embolic events are a major cause of morbidity and mortality in patients with infective endocarditis. We analyzed the database of the prospective cohort study SEI in order to identify factors associated with the occurrence of embolic events and to develop a scoring system for the assessment of the risk of embolism.
Methods
We retrospectively analyzed 1456 episodes of infective endocarditis from the multicenter study SEI. Predictors of embolism were identified. Risk factors identified at multivariate analysis as predictive of embolism in left-sided endocarditis, were used for the development of a risk score: 1 point was assigned to each risk factor (total risk score range: minimum 0 points; maximum 2 points). Three categories were defined by the score: low (0 points), intermediate (1 point), or high risk (2 points); the probability of embolic events per risk category was calculated for each day on treatment (day 0 through day 30).
Results
There were 499 episodes of infective endocarditis (34%) that were complicated by ≥ 1 embolic event. Most embolic events occurred early in the clinical course (first week of therapy: 15.5 episodes per 1000 patient days; second week: 3.7 episodes per 1000 patient days). In the total cohort, the factors associated with the occurrence of embolism at multivariate analysis were prosthetic valve localization (odds ratio, 1.84), right-sided endocarditis (odds ratio, 3.93), Staphylococcus aureus etiology (odds ratio, 2.23) and vegetation size ≥ 13 mm (odds ratio, 1.86). In left-sided endocarditis, Staphylococcus aureus etiology (odds ratio, 2.1) and vegetation size ≥ 13 mm (odds ratio, 2.1) were independently associated with embolic events; the 30-day cumulative incidence of embolism varied with risk score category (low risk, 12%; intermediate risk, 25%; high risk, 38%; p < 0.001).
Conclusions
Staphylococcus aureus etiology and vegetation size are associated with an increased risk of embolism. In left-sided endocarditis, a simple scoring system, which combines etiology and vegetation size with time on antimicrobials, might contribute to a better assessment of the risk of embolism, and to a more individualized analysis of indications and contraindications for early surgery.
Keywords: Infective endocarditis, Embolism, Stroke, Risk score
Background
Embolic events are common complications of infective endocarditis (IE) and are of prognostic importance [1-3]. Neurologic complications, mostly caused by embolic events, are frequent causes of intensive care unit admission, and embolism is a strong predictor of death for patients who have IE [4-8].
Small, clinically inapparent emboli probably occur in most patients who have IE, as demonstrated with positron-emission tomography and magnetic resonance imaging; silent cerebrovascular complications (including ischemia and microhemorrhage) may occur in up to 81% of patients [9-11]. Symptomatic embolism may occur in 13% to 46% of patients [6,12,13]. Many symptomatic emboli involve the central nervous system; clinical evidence of cerebrovascular embolic events is present in 12% to 40% of patients who have IE; the incidence may be higher in patients who are treated in referral centers, critically ill, or admitted to an intensive care unit [5,6,14].
Assessment of the embolic risk in individual patients is difficult, this having a major impact on clinical decisions regarding the indications for diagnostic procedures, antiaggregant and anticoagulant therapy and the timing of cardiac valve surgery [2,3,12,15-20]. Prevention of embolism is an established indication for surgery; in the Euro Heart Survey, vegetation size and previous embolism were reported as factors contributing to the surgical decision in, respectively, 48% and 18% of the patients who had surgery; in the French series recently published by Hubert et al. the presence of large vegetations (with or without previous embolism) was reported as an indication for surgery in 36% of the 493 patients who underwent surgery [3,21,22].
Most previous studies about the embolic complications of IE have been retrospective, with selection bias and limited numbers of patients. In addition, the epidemiology and standard of care of IE have clearly evolved over the years, and less recent observations may no more adequately represent the contemporary clinical profile of the disease [8,12,23-26]. The present study was based on data from a large prospective observational cohort; the retrospective analysis of the database had two main objectives: (1) to identify factors associated with the occurrence of embolic events and (2) to design a scoring system for the assessment of the risk of embolic complications.
Methods
Patients
The Italian Study on Endocarditis (Studio Endocarditi Italiano - SEI) working group was established in October 2003 in order to promote research on IE in Italy. Within this group, a prospective, observational, multicenter, open cohort study was designed. All consecutive episodes of IE diagnosed from January 2004 through December 2011 at 25 secondary and tertiary care institutions were included in the study. The diagnosis of IE was defined as possible or definite, in accordance with the modified Duke criteria [27]. Adult and pediatric patients were identified prospectively using institution-specific procedures, so as to ensure the consecutive enrollment of all the patients with IE observed at each participating institution. Echocardiography, diagnosis of embolic complications and treatment, were in accordance with current clinical practice (the study did not prescribe a standard diagnostic and therapeutic approach).
At the time of clinical observation of each patient, clinical data were recorded in a form that was designed for the study and registered in an electronic data entry system. The SEI database was maintained at the Infectious Diseases Department, Bergamo Hospital; the study was approved by the ethics committee “Comitato di Bioetica dell'Azienda Ospedali Riuniti di Bergamo”, and patients consented to enrollment in the SEI cohort as required by local guidelines and procedures. Details on the SEI study have been previously published [28].
Here we present the results of a retrospective analysis of the SEI database, aimed at investigating factors associated with the occurrence of embolic events; all the episodes of possible and definite IE were included.
Clinical data
Available information included demographic data, predisposing conditions, anatomic site of disease, microbiology, echocardiographic findings (presence, number, location and maximal length of vegetations), antimicrobial and surgical treatment, complications (heart failure, embolic events, intracardiac abscess, persistent positive blood cultures and new cardiac conduction abnormalities) and clinical outcome (survival and New York Hearth Association functional class). Central nervous system embolic events were reported as transient ischemic attack, ischemic stroke or hemorrhagic stroke. Peripheral embolic events were reported with details of anatomic site. Mycotic aneurysms, meningitis, encephalopathy, cerebral abscesses, arthritis, spondylodiscitis and cutaneous complications were excluded.
Infective endocarditis was classified as left-sided IE (LS-IE), left-sided native valve IE (LS-NVE), left-sided prosthetic valve IE (LS-PVE), right-sided IE (RS-IE) or IE associated with a cardiac implantable electronic device (CIED-IE).
Statistical analysis
Data analysis was performed with statistical software (Stata 13, StataCorp LP, College Station, TX). Comparisons were done using χ2 test (chi-square test) for proportions and Mann–Whitney test for ordered or continuous variables. Receiver operating characteristic (ROC) analysis was performed to determine the optimal vegetation size cut-off for the prediction of embolism.
Cumulative incidence analysis was performed from the date of starting treatment to the date of embolism (uncensored) or discharge from the hospital (censored). Cardiac surgery was treated as a competing event. Univariate and multivariate analyses were performed with logistic regression. Variables that were statistically significant in univariate analysis, variables that were clinically meaningful and possible confounders, were selected for prognostic assessment. For LS-IE, a weight was assigned to each factor that was associated with embolism, in order to build a risk score. The Kaplan‒Meier method was used to estimate univariate cumulative incidence of embolism according to the risk score. All tests were 2-sided, and statistical significance was defined by p ≤ 0.05. The probability of the occurrence of embolic events for each risk category was calculated for each day on treatment (from day 1 through day 30).
Results
Clinical characteristics of patients and embolic events
During the study period, 1456 IE episodes were observed at the participating institutions (1297 definite and 159 possible episodes); 10 episodes (0.7%) involved pediatric patients (age <18 y); basic demographic and medical data are summarized in Table 1.
Table 1.
Demographic and clinical characteristics of the cohort*
| Characteristics | All episodes | LS-NVE | LS-PVE | RS-IE | CIED-IE |
|---|---|---|---|---|---|
| Number of IE episodes |
1456 (100) |
967 (66.4) |
339 (23.3) |
89 (6.1) |
61 (4.2) |
| Age (y) |
65 (50 to 64) |
64 (48 to 74) |
70 (61 to 76) |
48 (35 to 67) |
67 (55 to 77) |
| Male |
1018 (70) |
688 (71) |
221 (65) |
61 (69) |
48 (79) |
| Comorbidity and predisposing conditions |
|
||||
| Native valve disease |
372 (26) |
299 (31) |
60 (18) |
7 (8) |
6 (10) |
| Diabetes mellitus |
268 (18) |
164 (17) |
79 (23) |
10 (11) |
15 (25) |
| Chronic liver disease |
262 (18) |
169 (18) |
49 (15) |
38 (43) |
6 (10) |
| Cancer |
175 (12) |
131 (14) |
28 (8) |
10 (11) |
6 (10) |
| Chronic intravenous access |
154 (11) |
102 (11) |
34 (10) |
11 (12) |
7 (12) |
| Current intravenous drug abuse |
131 (9) |
81 (8) |
14 (4) |
34 (38) |
2 (3) |
| Previous IE |
118 (8) |
48 (5) |
59 (17) |
7 (8) |
4 (7) |
| Congenital heart disease |
112 (8) |
85 (9) |
16 (5) |
6 (7) |
5 (8) |
| Immunosuppressive therapy |
86 (6) |
70 (7) |
11 (3) |
2 (2) |
3 (5) |
| HIV infection |
52 (4) |
36 (4) |
4 (1) |
10 (11) |
2 (3) |
| Hemodialysis |
29 (2) |
21 (2) |
4 (1) |
2 (2) |
2 (3) |
| Microbiology |
|
||||
| Staphylococcus aureus |
283 (19) |
181 (19) |
53 (16) |
35 (39) |
14 (23) |
| Viridans group streptococci |
217 (15) |
172 (18) |
29 (9) |
8 (9) |
8 (13) |
| Enterococcus species |
182 (13) |
117 (12) |
53 (16) |
8 (9) |
4 (7) |
| Coagulase-negative staphylococci |
147 (10) |
74 (8) |
55 (16) |
4 (5) |
14 (23) |
| Streptococcus bovis |
142 (10) |
105 (11) |
29 (9) |
7 (8) |
1 (2) |
| Other streptococci |
59 (4) |
46 (5) |
7 (2) |
3 (3) |
3 (5) |
| Other microorganisms |
61 (4) |
36 (4) |
20 (6) |
2 (2) |
3 (5) |
| Polymicrobial |
51 (4) |
34 (4) |
10 (3) |
4 (5) |
3 (5) |
| Fungi |
20 (1) |
12 (1) |
8 (2) |
0 (0) |
0 (0) |
| HACEK |
3 (0.2) |
0 (0) |
2 (0.6) |
1 (1) |
0 (0) |
| Microbiology negative | 291 (20) | 190 (20) | 73 (22) | 17 (19) | 11 (18) |
*Data reported as number, median (interquartile range), or number (% patients).
Abbreviations:CIED-IE infective endocarditis associated with a cardiac implantable electronic device, HACEKHaemophilus species, Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, and Kingella kingae, HIV human immunodeficiency virus, LS-NVE left-sided native valve endocarditis, LS-PVE left-sided prosthetic valve endocarditis, RS-IE right-sided infective endocarditis.
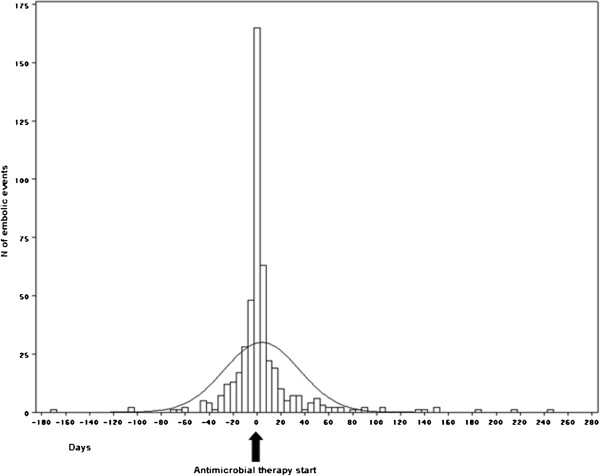
Embolization occurred in 499 IE episodes (34.3%), with more than one embolic event in 135 episodes (9.3%), and a cumulative number of 700 embolic events (Table 2). In 121/499 IE episodes (24.2%) the first embolic event occurred in the days preceding the diagnosis of IE and the start of antimicrobial therapy; in 77 cases (15.4%) on the same day of diagnosis. After the starting of antimicrobial therapy, most embolic events occurred early (15.5 episodes per 1000 patient days during the first week of therapy; 3.7 episodes per 1000 patient days during the second week of therapy) (Figure 1). In 93 IE episodes, the disease was complicated by both CNS and peripheral embolism; in 25 of these episodes CNS embolism was preceded by overt peripheral embolism.
Table 2.
Type and anatomic site of embolic events*
| Characteristics | All IE episodes | LS-NVE | LS-PVE | RS-IE | CIED-IE |
|---|---|---|---|---|---|
| Number of IE episodes |
1456 |
967 |
339 |
89 |
61 |
| Embolic events |
700 |
436 |
166 |
74 |
24 |
| CNS emboli |
249 (36) |
174 (40) |
68 (41) |
3 (4) |
4 (17) |
| Ischemic stroke |
176 (25) |
126 (29) |
45 (27) |
2 (3) |
3 (13) |
| Transient ischemic attack |
42 (6) |
26 (6) |
14 (8) |
1 (1) |
1 (4) |
| Hemorrhagic stroke |
31 (4) |
22 (5) |
9 (6) |
0 (0) |
0 (0) |
| Peripheral emboli |
451 (64) |
262 (60) |
98 (59) |
71 (96) |
20 (83) |
| Pulmonary |
122 (17) |
26 (6) |
25 (15) |
57 (84) |
14 (58) |
| Splenic |
117 (17) |
90 (21) |
23 (14) |
3 (4) |
1 (4) |
| Limbs |
95 (14) |
70 (16) |
15 (9) |
7 (10) |
3 (13) |
| Other | 117 (17) | 76 (17) | 35 (21) | 4 (6) | 2 (8) |
*Data reported as number or number (% of embolic events).
Abbreviations: CIED-IE infective endocarditis associated with a cardiac implantable electronic device, LS-NVE left-sided native valve endocarditis, LS-PVE left-sided prosthetic valve endocarditis, RS-IE right-sided infective endocarditis.
Figure 1.
Timing of embolic events. Negative values represent days before the beginning of the antibiotic therapy; zero represents the day of the beginning of antibiotic therapy; positive values represent the days after the beginning of the antibiotic therapy.
IE episodes complicated by embolic events had a higher in-hospital mortality (OR 1.84; 95% CI 1.36 – 2.49, p ≤ 0.0001); no significant difference was observed in the rate of cardiac surgical procedures when comparing IE episodes complicated by embolism with uncomplicated IE episodes (OR 0.98; 95% CI 0.79 – 1.23, p ns) (Additional file 1: Appendix 1 and Additional file 2: Appendix 2).
Factors associated with embolic events
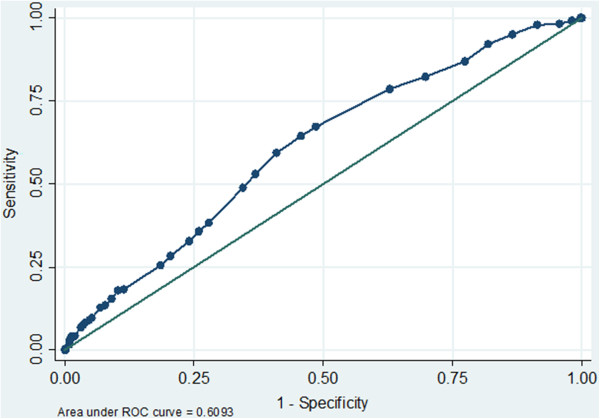
In the total cohort (including LS-IE, RS-IE, and CIED-IE), univariate analysis showed that embolism was associated with younger patient age, HIV infection, absence of cancer, presence of chronic liver disease, current intravenous drug abuse, RS-IE, larger vegetation size, S. aureus and Enterococcus species etiology (Table 3). The ROC curve analysis showed that a vegetation size ≥ 13 mm was significantly associated with the occurrence of emboli (Figure 2). Anticoagulant therapy at the onset of the IE episode was not associated with a significant difference in the frequency of embolic events; the same was true for antiaggregant therapy (Table 3). Multivariate analysis showed that the only independent predictors of embolism were prosthetic valve involvement, right-side localization, vegetation size (13 mm cut-off value) and S. aureus etiology (Table 4).
Table 3.
Total cohort: univariate analysis of factors associated with embolism*
|
Characteristics |
IE episodes |
IE episodes |
p
≤ † |
|---|---|---|---|
| |
with embolic |
without embolic |
|
| events | events | ||
| Number of episodes of IE |
499 |
957 |
|
|
Age (y) |
62 (28 to 81) |
67 (31 to 84) |
0.0002 |
| Male |
361 (72) |
657 (69) |
NS |
| Hemodialysis |
10 (2) |
19 (2) |
NS |
| Diabetes mellitus |
86 (17) |
182 (19) |
NS |
|
HIV infection |
29 (6) |
23 (2) |
0.004 |
|
Cancer |
46 (9) |
129 (13) |
0.03 |
|
Chronic liver disease |
115 (23) |
147 (15) |
0.0005 |
|
Current intravenous drug abuse |
74 (15) |
57 (6) |
0.0001 |
| Previous IE |
38 (8) |
80 (8) |
NS |
| Chronic intravenous access |
59 (12) |
95 (10) |
NS |
| Congenital heart disease |
38 (8) |
74 (8) |
NS |
| Native valve predisposition |
132 (26) |
270 (28) |
NS |
| Nosocomial IE |
29 (6) |
50 (5) |
NS |
| Health care associated IE |
107 (21) |
227 (24) |
NS |
| Community-acquired IE |
363 (73) |
680 (71) |
NS |
| Native vs prosthetic valve |
385 vs 114 |
732 vs 225 |
NS |
| Site of IE (n = 1282) |
|
||
| Mitral vs aortic valve |
166 vs 161 |
329 vs 359 |
NS |
| Bivalvular involvement (mitral and aortic) |
39 (8) |
78 (8) |
NS |
|
Right-sided IE |
60 (12) |
29 (3) |
0.0001 |
| CIED-IE |
21 (4) |
40 (4) |
NS |
| Vegetations (n = 710)‡ |
|
||
| Size of all vegetations (mm) |
14 (6 to 30) |
10 (4 to 26) |
0.0001 |
| ≥ 10 mm |
228 (79) |
264 (63) |
0.0001 |
| ≥ 15 mm |
142 (49) |
145 (35) |
0.0001 |
| ≥ 20 mm |
74 (26) |
78 (19) |
0.03 |
| Concomitant therapy at onset of IE |
|
||
| Anticoagulants |
102 (20) |
228 (24) |
NS |
| Antiaggregants |
68 (14) |
103 (11) |
NS |
| Microbiology |
|
|
|
|
Staphylococcus aureus
|
141 (28) |
142 (15) |
0.0001 |
| Viridans group streptococci |
66 (13) |
151 (16) |
NS |
| Coagulase-negative staphylococci |
52 (10) |
95 (10) |
NS |
|
Enterococcus
species |
45 (9) |
137 (1) |
0.004 |
| Streptococcus bovis |
44 (9) |
98 (10) |
NS |
| Polymicrobial |
19 (4) |
32 (3) |
NS |
| Other microorganisms |
16 (3) |
45 (6) |
NS |
| Other streptococci |
16 (3) |
43 (5) |
NS |
| Fungi/yeasts |
7 (1) |
13 (1) |
NS |
| HACEK |
1 (0.2) |
2 (0.2) |
NS |
| Microbiology negative | 92 (18) | 199 (21) | NS |
*Total cohort, N = 1456 episodes of infective endocarditis. Data reported as number, median (range, 5th to 95th percentile), or number (%). Abbreviations:CIED-IE infective endocarditis associated with a cardiac implantable electronic device, HACEKHaemophilus species, Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, and Kingella kingae, HIV human immunodeficiency virus, IE infective endocarditis.
†NS, not significant (p > 0.05).
‡ IE episodes with vegetations of known size: 710 episodes (290 episodes with embolism and 420 episodes without embolism).
Bold numbers represent statistically significant differences.
Figure 2.
Total cohort: size of vegetation. Receiver operating characteristic analysis for the prediction of embolic events, based on vegetation size.
Table 4.
Total cohort: multivariate analysis of factors associated with embolism*
| Odds ratio | 95% CI | p ≤ † | |
|---|---|---|---|
| Age |
1.0 |
1.0 – 1.0 |
NS |
| HIV infection |
0.8 |
0.3 – 2.0 |
NS |
| Cancer |
1.10 |
0.7 – 1.9 |
NS |
| Chronic liver disease |
1.4 |
0.9 – 2.2 |
NS |
| Mitral vs aortic valve |
1.0 |
0.7 – 1.3 |
NS |
|
Prosthetic vs native valve |
1.8 |
1.2 – 2.9 |
0.011 |
|
Righ-sided IE |
3.9 |
2.0 – 7.7 |
<0.0001 |
|
Size of vegetation ≥ 13 mm |
1.9 |
1.3 – 2.6 |
<0.0001 |
|
Staphylococcus aureus
|
2.2 |
1.5 – 3.4 |
<0.0001 |
|
Coagulase-negative staphylococci |
1.6 |
1.0 – 2.6 |
NS |
|
Enterococcus spp. |
0.8 |
0.4 – 1.4 |
NS |
| Anticoagulant therapy | 0.8 | 0.5 – 1.3 | NS |
*N = 1456 IE episodes. Abbreviation:HIV human immunodeficiency virus.
†NS, not significant (p > 0.05).
Bold numbers represent statistically significant differences.
In LS-IE, univariate analysis showed that embolism was associated with younger patient age, current intravenous drug abuse, larger vegetation size, S. aureus and Enterococcus species etiology (Additional file 3: Table S1). The ROC curve analysis showed that a vegetation size ≥ 13 mm was significantly associated with the occurrence of emboli (Additional file 4: Figure S1). Multivariate analysis showed that in LS-IE the only independent predictors of embolism were vegetation size (13 mm cut-off value; OR 2.1; 95% CI 1.5 – 2.8, p = 0.0001) and S. aureus etiology (OR 2.1; 95% CI 1.5 – 3.1, p = 0.0001) There were no significant differences in the frequency of embolism between mitral and aortic valves or between native and prosthetic valves. (Additional file 5: Table S2).
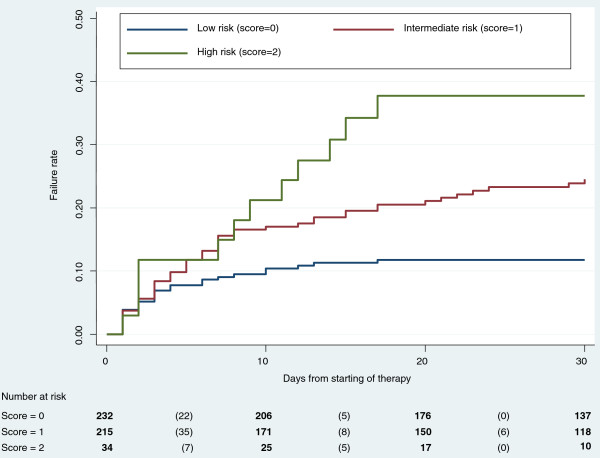
Risk score
The two risk factors for LS-IE embolism that were identified with multivariate analysis (vegetation size ≥ 13 mm and Staphylococcus aureus etiology) were combined for designing the risk score. Because there was no marked difference in the odds ratios of the 2 prognostic variables, 1 point was assigned for the presence of each factor (total risk score range: minimum 0 points; maximum 2 points), this resulting in a three-tiered score:
•low risk category (no poor prognostic factor: etiology other than S. aureus, and vegetations size <13 mm);
•intermediate risk category (1 poor prognostic factor: S. aureus etiology or vegetations size ≥ 13 mm);
•high risk category (2 poor prognostic factors: S. aureus etiology and vegetations size ≥ 13 mm).
•The 30-day cumulative incidence of embolism varied significantly across the different risk categories: 11.8% (95% CI 7.2 – 19.2) in the low risk category, 24.5% (95% CI 20.3 – 37.0) in the intermediate risk category, 37.7 (95% CI 22.1 – 64.9) in the high risk category. Kaplan-Meier plots showed that the 3 risk categories differed significantly from each other by log-rank test and test for trend (p ≤ 0.001) (Figure 3, Table 5).
Figure 3.
Left-sided IE: Kaplan-Meier plots of failure rates (embolic events) for different risk categories. Bold numbers: number of patients at risk at any given time. Numbers in parentheses: number of embolic events that occurred in each time interval.
Table 5.
Left-sided IE: 30-day probability (%) of embolic events per risk category
| Time from start of therapy (d) | Low (0) | Intermediate (1) | High (2) |
|---|---|---|---|
| 0 |
11.78 |
24.54 |
37.73 |
| 1 |
7.90 |
20.82 |
34.79 |
| 2 |
6.61 |
18.95 |
25.97 |
| 3 |
4.88 |
16.13 |
25.97 |
| 4 |
4.01 |
14.70 |
25.97 |
| 5 |
4.01 |
12.78 |
25.97 |
| 6 |
3.14 |
11.34 |
25.97 |
| 7 |
2.71 |
8.95 |
22.81 |
| 15 |
0.48 |
5.02 |
3.46 |
| 30 | 0.00 | 0.00 | 0.00 |
Note: numbers represent the probability (%) of embolism at the end of a given time interval. Time 0 values include embolic events occurred on the first calendar day of therapy; day 1 values represent the risk at the end of the first calendar day of therapy.
Discussion
Embolism is a common complication of infective endocarditis. The cumulative incidence of clinically overt embolic events in our series (34.3%) is within the range observed in most published series, notwithstanding differences in definitions and enrollment criteria between studies [6,7,12,13,22,26,29,30]. More in detail, the incidence of embolization observed in our study in LS-NVE (31.4%), LS-PVE (33.6%), RS-IE (67%), CIED-IE (34.4%) is similar to what has been reported from most contemporary studies: a high incidence of embolic events in RS-IE, and an incidence in the range 20-33% for CIED-associated IE; it has to be noted that in our study, in contrast with other published series, we did not observe significant differences in the frequency of embolic events between mitral and aortic valve localization, and between LS-NVE and LS-PVE [8,15].
It is well known that embolic episodes occur early in the course of the disease, often before the diagnosis of IE is established and antimicrobial therapy is started; our findings confirm this, with a large part of the embolic events (39.6%) occurring in the days preceding the diagnosis or on the day of diagnosis [3,8,15]. The present study confirms that the risk of embolism decreases markedly after the first week of antimicrobial therapy; this seems to support previous recommendations against stroke prevention as the only indication for valvular surgery after 1 week of therapy [15].
An embolic event may predict the risk of further embolic events and neurologic complications, and this may have an effect on decision making [3,14]. In our series, central nervous system embolism was preceded by symptomatic peripheral embolism in just 25 patients, this apparently limiting the utility of peripheral embolism as a predictor for CNS embolic complications. These 25 patients might point to a missed opportunity for surgical prevention of embolism, but it has to be noted that in the SEI study data regarding the possible presence of major contraindications for surgery were not systematically collected.
Many papers have reported on the characteristics of vegetations which are predictive of the risk of embolism [1,3,7,12,25,26,31]; lacking a standardized echocardiographic study of our patients, the analysis was restricted to the size of the vegetations, which is a major determinant of the embolic risk, as underlined by two meta-analyses [32,33]. The cut-off value of 13 mm derived by our cumulative analysis (and confirmed by an analysis restricted to the LS-IE episodes) is within the range commonly discussed in the literature (10 mm or 15 mm for LS-IE, and 20 mm for RS-IE) [3,7,12,25,26,31].
S. aureus has been associated with an increased risk of embolic events; our data clearly confirm this, with an OR for S. aureus versus all other microbial agents of 2.2 [3,7,8,15,34]. A few papers have also reported on a higher incidence of embolic complications in Streptococcus bovis IE: our analysis of 142 S. bovis IE episodes did not confirm these findings; it has to be noted that in the report by Pergola et al. (40 S. bovis episodes), a significant difference was observed when comparing S. bovis with other streptococci, but not when comparing S. bovis with other pathogens; and Tripodi et al. found a significant difference when comparing S. bovis IE (30 episodes) with IE due to other etiological agents (p = 0.002 at univariate analysis); however, patients with S. bovis IE were older and had a higher rate of bivalvular involvement [7,35,36]. High rates of embolic events have been described in fungal endocarditis (43% in 21 cases of PVE-IE reported by Boland); in our series (20 fungal episodes) we did not observe a significant difference when comparing fungal IE episodes with episodes due to other pathogens [37-39].
In our series age, sex and a number of predisposing and comorbidity conditions were not found to be associated with the occurrence of embolic events, and were not included in the score; this is in contrast with what has recently been proposed by Hubert et al., which included in their risk calculator not only vegetation size (10 mm cut-off) and S. aureus etiology, but also age, diabetes, previous embolism and atrial fibrillation [3].
Despite the large sample size in the present study, only 2 factors were significantly associated with the occurrence of embolic events in LS-IE: vegetation size ≥ 13 mm and S. aureus etiology. These variables were incorporated into a 3-tiered risk score; the 3 categories of the scoring system were associated with clinically relevant differences in the risk of developing embolic events. Combining the risk category with the number of days on antimicrobials could be used to assess the probability of embolism (as shown in Table 5), in order to compare the embolic risk with the risks associated with surgery, making it possible to individualize a patient’s evaluation, especially during the crucial first days of the clinical course. However, differences in patient populations, clinical settings, and models of care may affect the predictive value of the score. Therefore, the clinical use of the scoring system will be possible only following successful external validation.
Our study has inherent limitations: firstly, the participant centers were secondary and tertiary care units, where a major interest in the field of IE had developed; yet, patients with IE are admitted all over the country to Infectious Diseases, Internal Medicine, Cardiology, Cardiac Surgery wards and to intensive care units, and a referral bias has to be taken in account; in fact, our data do not represent the wide range of clinical conditions and patterns of treatment which are observed across Italy, and there is clearly the need for large, population-based studies, which could better describe the full spectrum of the disease, as currently observed and treated in our country. Secondly, echocardiographic evaluation was left to local expertise, without a centralized standardization or supervision: this may have limited our ability to identify characteristics of the vegetations that may be associated with the occurrence of embolic events. Finally, embolization was diagnosed at the different institutions in accordance with current clinical practice, and therefore differences in the diagnostic approach may have reduced the discriminatory power of our analysis.
Conclusions
Embolism occurs early in the course of IE; the steep decline of the risk of embolization immediately after antibiotics initiation allows only a narrow time window for the surgical prophylaxis of embolic complications. In this challenging clinical context, the simple score system described in the present study, if externally validated, might contribute to a timely and individualized assessment of the embolic risk.
Competing interests
No financial support was obtained for this work.
The authors declare that they have no competing interests.
Authors’ contributions
MR designed the study; VR managed the database; AC performed all statistical analyses; MR prepared the initial draft of the manuscript; MBP, EDM, and AP, revised the manuscript and made important content contributions; all authors were involved in manuscript review and editing; all authors, with the exception of AC, contributed to pts’ enrolment, and to the implementation of the SEI study. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
Embolic events and in-hospital mortality.
Embolic events and surgery.
Left-sided IE: univariate analysis of factors associated with embolism.
Left-sided IE: size of vegetation. Receiver operating characteristic analysis for the prediction of embolic events, based on vegetation size.
Left-sided IE: multivariate analysis of factors associated with embolism.
Contributor Information
Marco Rizzi, Email: mrizzi@hpg23.it.
Veronica Ravasio, Email: vravasio@hpg23.it.
Alessandra Carobbio, Email: acarobbio@hpg23.it.
Irene Mattucci, Email: irene82m@hotmail.it.
Massimo Crapis, Email: crapis.massimo@aoud.sanita.fvg.it.
Roberto Stellini, Email: roberto.stellini@hotmail.it.
Maria Bruna Pasticci, Email: mariabruna.pasticci@unipg.it.
Pierangelo Chinello, Email: pierangelo.chinello@inmi.it.
Marco Falcone, Email: marcofalc@libero.it.
Paolo Grossi, Email: paolo.grossi@uninsubria.it.
Francesco Barbaro, Email: francesco.barbaro@libero.it.
Angelo Pan, Email: ange.pan@tiscali.it.
Pierluigi Viale, Email: pierluigi.viale@unibo.it.
Emanuele Durante-Mangoni, Email: emanuele.durante@unina2.it.
Acknowledgments
SEI investigators: Alberto Biglino, Maria Teresa Brusa, Paolo Crivelli, and Roberta Moglia (Asti); Sebastiano Leone, Veronica Ravasio, Marco Rizzi and Fredy Suter (Bergamo); Pierluigi Viale (Bologna); Peter Mian and Greta Spoladore (Bolzano); Francesco Castelli, Silvia Magri and Roberto Stellini (Brescia); Domenico Di Caprio (Caserta); Evelyn Van Hauwermeiren, Angelo Pan and Fabio Zacchi (Cremona); Nicoletta Barzaghi (Cuneo); Marco Libanore and Mario Pantaleoni (Ferrara); Valerio Del Bono and Claudio Viscoli (Genova); Gianni Gattuso and Alfredo Scalzini (Mantova); Maria Riccarda Villa (Milano); Mariano Bernardo, Roberta Casillo, Susanna Cuccurullo, Giovanni Dialetto, Emanuele Durante-Mangoni, Irene Mattucci, Enrico Ragone, Marie-Françoise Tripodi and Riccardo Utili (Napoli); Francesco Barbaro and Elke Erne (Padova); Lorenzo Minoli and Elena Maria Seminari (Pavia); Laura Martinelli, Carlo Pallotto and Maria Bruna Pasticci (Perugia); Benedetta Canovari and Laura Stoppini (Pesaro); Pierangelo Chinello, Marco Falcone, Nicola Petrosillo and Mario Venditti (Roma); Palma Delle Foglie (Trento); Mario Giobbia, Walter Inoiosa, Pier Giorgio Scotton and Alberto Vaglia (Treviso); Matteo Bassetti, Massimo Crapis and Sergio Venturini (Udine); Daniela Dalla Gasperina, Paolo Grossi and Alessandro Tebini (Varese); Ercole Concia, Paola Del Bravo and Andrea Tedesco (Verona); Roberto Nicolin and Giampietro Pellizzer (Vicenza).
References
- Cabell CH, Pond KK, Peterson GE, Durack DT, Corey GR, Anderson DJ, Ryan T, Lukes AS, Sexton DJ. The risk of stroke and death in patients with aortic and mitral valve endocarditis. Am Heart J. 2001;14:75–80. doi: 10.1067/mhj.2001.115790. [DOI] [PubMed] [Google Scholar]
- Thuny F, Avierinos J-F, Tribouilloy C, Giorgi R, Casalta J-P, Milandre L, Brahim A, Nadji G, Riberi A, Collart F, Renard S, Raoult D, Habib G. Impact of cerebrovascular complications on mortality and neurologic outcome during infective endocarditis: a prospective multicentre study. Eur Heart J. 2007;14:1155–1161. doi: 10.1093/eurheartj/ehm005. [DOI] [PubMed] [Google Scholar]
- Hubert S, Thuny F, Resseguier N, Giorgi R, Tribouilloy C, Le Dolley Y, Casalta J-P, Riberi A, Chevalier F, Rusinaru D, Malaquin D, Remadi JP, Ben Ammar A, Avierinos J-F, Collart F, Raoult D, Habib G. Prediction of symptomatic embolism in infective endocarditis: construction and validation of a risk calculator in a multicenter cohort. J Am Coll Cardiol. 2013;14:1384–1392. doi: 10.1016/j.jacc.2013.07.029. [DOI] [PubMed] [Google Scholar]
- Sonneville R, Mourvillier B, Bouadma L, Wolff M. Management of neurological complications of infective endocarditis in ICU patients. Ann Intensive Care. 2011;14:10. doi: 10.1186/2110-5820-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SJ, Oh SS, Lim DS, Na CY, Kim JH. Clinical significance of cerebrovascular complications in patients with acute infective endocarditis: a retrospective analysis of a 12-year single-center experience. BMC Neurol. 2014;14:30. doi: 10.1186/1471-2377-14-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu VH, Cabell CH, Benjamin DK Jr, Kuniholm EF, Fowler VG Jr, Engemann J, Sexton DJ, Corey R, Wang A. Early predictors of in-hospital death in infective endocarditis. Circulation. 2004;14:1745–1749. doi: 10.1161/01.CIR.0000124719.61827.7F. [DOI] [PubMed] [Google Scholar]
- Thuny F, Di Salvo G, Belliard O, Avierinos J-F, Pergola V, Rosenberg V, Casalta J-P, Gouvernet J, Derumeaux G, Iarussi D, Ambrosi P, Calabro R, Riberi A, Colart F, Metras D, Lepidi H, Raoult D, Harle J-R, Weiller P-J, Cohen A, Habib G. Risk of embolism and death in infective endocarditis: prognostic value of echocardiography. A prospective multicenter study. Circulation. 2005;14:69–75. doi: 10.1161/CIRCULATIONAHA.104.493155. [DOI] [PubMed] [Google Scholar]
- Fabri J Jr, Issa VS, Pomerantzeff PM, Grinberg M, Barretto AC, Mansur AJ. Time-related distribution, risk factors and prognostic influence of embolism in patients with left-sided infective endocarditis. Int J Cardiol. 2006;14:334–339. doi: 10.1016/j.ijcard.2005.07.016. [DOI] [PubMed] [Google Scholar]
- Van Riet J, Hill EE, Gheysens O, Dymarkowski S, Herregods M-C, Herijgers P, Peetermans WE, Mortelmans L. (18)F-FDG PET/CT for early detection of embolism and metastatic infection in patients with infective endocarditis. Eur J Nucl Med Mol Imaging. 2010;14:1189–1197. doi: 10.1007/s00259-010-1380-x. [DOI] [PubMed] [Google Scholar]
- Snygg-Martin U, Gustafsson L, Rosengren L, Alsiö Å, Ackerholm P, Andersson R, Olaison L. Cerebrovascular complications in patients with left-sided infective endocarditis are common: a prospective study using magnetic resonance imaging and neurochemical brain damage markers. Clin Infect Dis. 2008;14:23–30. doi: 10.1086/588663. [DOI] [PubMed] [Google Scholar]
- Duval X, Iung B, Klein I, Brochet E, Thabut G, Arnoult F, Lepage L, Laissy J-P, Wolff M, Leport C. for the IMAGE (Resonance Magnetic Imaging at the Acute Phase of Endocarditis) Study Group. Effect of early cerebral magnetic resonance imaging on clinical decisions in infective endocarditis: a prospective study. Ann Intern Med. 2010;14:497–504. doi: 10.7326/0003-4819-152-8-201004200-00006. [DOI] [PubMed] [Google Scholar]
- Di Salvo G, Habib G, Pergola V, Avierinos J-F, Philip E, Casalta J-P, Vailloud J-M, Derumeaux G, Gouvernet J, Ambrosi P, Lambert M, Ferracci A, Raoult D, Luccioni R. Echocardiography predicts embolic events in infective endocarditis. J Am Coll Cardiol. 2001;14:1069–1076. doi: 10.1016/S0735-1097(00)01206-7. [DOI] [PubMed] [Google Scholar]
- Hill EE, Herijgers P, Claus P, Vanderschueren S, Herregods MC, Peetermans WE. Infective endocarditis: changing epidemiology and predictors of 6-month mortality: a prospective cohort study. Eur Heart J. 2007;14:196–203. doi: 10.1093/eurheartj/ehl427. [DOI] [PubMed] [Google Scholar]
- Sonneville R, Mirabel M, Hajage D, Tubach F, Vignon P, Perez P, Lavoué S, Kouatchet A, Pajot O, Dessap AM, Tonnelier J-M, Bollaert P-E, Frat J-P, Navellou J-C, Hyvernat H, Hssain AA, Tabah A, Trouillet J-L, Wolff M. for the ENDOcardite en REAnimation Study Group. Neurologic complications and outcomes of infective endocarditis in critically-ill patients: the ENDOcardite en REAnimation prospective multicenter study. Crit Care Med. 2011;14:1474–1481. doi: 10.1097/CCM.0b013e3182120b41. 28. [DOI] [PubMed] [Google Scholar]
- Dickerman SA, Abrutyn E, Barsic B, Bouza E, Cecchi E, Moreno A, Doco-Lecompte T, Eisen DP, Fortes CQ, Fowler VG jr, Lerakis S, Mirò JM, Pappas P, Peterson GE, Rubinstein E, Sexton DJ, Suter F, Tornos P, Verhagen DW, Cabell CH. for the ICE Investigators. The relationship between the initiation of antimicrobial therapy and the incidence of stroke in infective endocarditis: an analysis from the ICE Prospective Cohort Study (ICE-PCS) Am Heart J. 2007;14:1086–1094. doi: 10.1016/j.ahj.2007.07.023. [DOI] [PubMed] [Google Scholar]
- Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Bolger AF, Levison ME, Ferrieri P, Gerber MA, Tani LY, Gewitz MH, Tong DC, Steckelberg JM, Baltimore RS, Shulman ST, Burns JC, Falace DA, Newburger JW, Pallasch TJ, Takahashi M, Taubert KA. Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation. 2005;14:e394–e434. doi: 10.1161/CIRCULATIONAHA.105.165564. [DOI] [PubMed] [Google Scholar]
- Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I, Moreillon P, Antunes MJ, Thilen U, Lekakis J, Lengyel M, Müller L, Naber CK, Nihoyannopoulos P, Moritz A, Zamorano JL. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur Hearth J. 2009;14:2369–2413. doi: 10.1093/eurheartj/ehp285. [DOI] [PubMed] [Google Scholar]
- Gould FK, Denning DW, Elliott TS, Foweraker J, Perry JD, Prendergast BD, Sandoe JAT, Spry MJ, Watkin RW. Guidelines for the diagnosis and antibiotic treatment of endocarditis in adults: a report of the working party of the British society for antimicrobial chemotherapy. J Antimicrob Chemother. 2012;14:269–289. doi: 10.1093/jac/dkr450. [DOI] [PubMed] [Google Scholar]
- Derex L, Bonnefoy E, Delahaye F. Impact of stroke on therapeutic decision making in infective endocarditis. J Neurol. 2010;14:315–321. doi: 10.1007/s00415-009-5364-3. [DOI] [PubMed] [Google Scholar]
- Kang DH, Kim YJ, Kim SH, Sun BJ, Kim D-H, Yun S-C, Song J-M, Choo SJ, Chung C-H, Song J-K, Lee J-W, Sohn D-W. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;14:2466–2473. doi: 10.1056/NEJMoa1112843. [DOI] [PubMed] [Google Scholar]
- Prendergast BD, Tornos P. Surgery for infective endocarditis: who and when? Circulation. 2010;14:1141–1152. doi: 10.1161/CIRCULATIONAHA.108.773598. [DOI] [PubMed] [Google Scholar]
- Tornos P, Iung B, Permanyer-Miralda G, Baron G, Delahaye F, Gohlke-Bärwolf C, Butchart EG, Ravaud P, Vahanian A. Infective endocarditis in Europe: lessons from the Euro heart survey. Heart. 2005;14:571–575. doi: 10.1136/hrt.2003.032128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang A, Athan E, Pappas PA, Fowler VG Jr, Olaison L, Paré C, Almirante B, Muñoz P, Rizzi, Naber C, Logar M, Tattevin P, Iarussi DL, Selton-Suty C, Braun Jones S, Casabé J, Morris A, Corey GR, Cabell CH. Contemporary clinical profile and outcome of prosthetic valve endocarditis. JAMA. 2007;14:1354–1361. doi: 10.1001/jama.297.12.1354. [DOI] [PubMed] [Google Scholar]
- Vilacosta I, Graupner C, San Román JA, Sarriá C, Ronderos R, Fernández C, Mancini L, Sanz O, Sanmartìn JV, Stoermann W. Risk of embolization after institution of antibiotic therapy for infective endocarditis. J Am Coll Cardiol. 2002;14:1489–1495. doi: 10.1016/S0735-1097(02)01790-4. [DOI] [PubMed] [Google Scholar]
- Durante-Mangoni E, Adinolfi LF, Tripodi MF, Andreana A, Gambardella M, Ragone E, Precone DF, Utili R. Risk factors for “major” embolic events in hospitalized patients with infective endocarditis. Am Heart J. 2003;14:311–316. doi: 10.1016/S0002-8703(02)94802-7. [DOI] [PubMed] [Google Scholar]
- Deprèle C, Berthelot P, Lemetayer F, Comtet C, Fresard A, Cazorla C, Fascia P, Cathébras P, Chaumentin G, Convert G, Isaaz K, Barral X, Lucht F. Risk factors for systemic emboli in infective endocarditis. Clin Microbiol Infect. 2004;14:46–53. doi: 10.1111/j.1469-0691.2004.00735.x. [DOI] [PubMed] [Google Scholar]
- Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, Bashore T, Corey R. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;14:633–638. doi: 10.1086/313753. [DOI] [PubMed] [Google Scholar]
- Leone S, Ravasio V, Durante-Mangoni E, Crapis M, Carosi G, Scotton PG, Barzaghi N, Falcone M, Chinello P, Pasticci MB, Grossi P, Utili R, Viale P, Rizzi M, Suter F. Epidemiology, characteristics, and outcome of infective endocarditis in Italy: the Italian Study on Endocarditis. Infection. 2012;14:527–535. doi: 10.1007/s15010-012-0285-y. [DOI] [PubMed] [Google Scholar]
- Murdoch DR, Corey GR, Hoen B, Miró JM, Fowler VG Jr, Bayer AS, Karchmer AW, Olaison L, Pappas PA, Moreillon P, Chambers ST, Chu VH, Falcò V, Holland DJ, Jones P, Klein JL, Raymond NJ, Read KM, Tripodi M-F, Utili R, Wang A, Woods CW, Cabell CH. for the International Collaboration on Endocarditits-Prospective Cohort Study (ICE-PCS) Investigators. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Infective Endocarditis - Prospective Cohort Study. Arch Intern Med. 2009;14:463–473. doi: 10.1001/archinternmed.2008.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athan E, Chu VH, Tattevin P, Selton-Suty C, Jones P, Naber C, Mirò JM, Ninot S, Fernàndez-Hidalgo N, Durante-Mangoni E, Spelman D, Hoen B, Lejko-Zupane T, Cecchi E, Thuny F, Hannan MM, Pappas P, Henry M, Fowler VG Jr, Crowley AL, Wang A. for the ICE-PCS Investigators. Clinical characteristics and outcome of infective endocarditis involving implantable cardiac devices. JAMA. 2012;14:1727–1735. doi: 10.1001/jama.2012.497. [DOI] [PubMed] [Google Scholar]
- Martin-Dávila P, Navas E, Fortún J, Moya JL, Cobo J, Pintado V, Quereda C, Jiménez-Mena M, Moreno S. Analysis of mortality and risk factors associated with native valve endocarditis in drug users: the importance of vegetation size. Am Heart J. 2005;14:1099–1106. doi: 10.1016/j.ahj.2005.02.009. [DOI] [PubMed] [Google Scholar]
- Tischler MD, Vaitkus PT. The ability of vegetation size on echocardiography to predict clinical complications: a meta-analysis. J Am Soc Echocardiogr. 1997;14:562–568. doi: 10.1016/S0894-7317(97)70011-7. [DOI] [PubMed] [Google Scholar]
- Salehian O, Chan KL. In: Endocarditis. Diagnosis and Management. Chan KL, Embil JM, editor. London: Springer-Verlag; 2006. Systemic embolism in endocarditis: incidence, risk factors, clinical significance, and treatment strategies; pp. 229–240. [Google Scholar]
- Fowler VG Jr, Miró JM, Hoen B, Cabell CH, Abrutyn E, Rubinstein E, Corey RG, Spelman D, Bradley SF, Barsic B, Pappas PA, Anstrom KJ, Wray D, Fortes CQ, Anguera I, Athan E, Jones P, van der Meer JTM, Elliott TSJ, Levine DP, Bayer AS. for the ICE Investigators. Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA. 2005;14:3012–3021. doi: 10.1001/jama.293.24.3012. [DOI] [PubMed] [Google Scholar]
- Pergola V, Di Salvo G, Habib G, Avierinos J-F, Philip E, Vailloud J-M, Thuny F, Casalta J-P, Ambrosi P, Lambert M, Riberi A, Ferracci A, Mesana T, Metras D, Harle J-R, Weiller P-J, Raoult D, Luccioni R. Comparison of clinical and echocardiographic characteristics of Streptococcus bovis endocarditis with that caused by other pathogens. Am J Cardiol. 2001;14:871–875. doi: 10.1016/S0002-9149(01)01914-2. [DOI] [PubMed] [Google Scholar]
- Tripodi MF, Adinolfi LE, Ragone E, Durante-Mangoni E, Fortunato R, Iarussi D, Ruggiero G, Utili R. Streptococcus bovis endocarditis and its association with chronic liver disease: an underestimated risk factor. Clin Infect Dis. 2004;14:1394–1400. doi: 10.1086/392503. [DOI] [PubMed] [Google Scholar]
- Ellis ME, Al-Abdely H, Sandridge A, Greer W, Ventura W. Fungal endocarditis: evidence in the world literature, 1965–1995. Clin Infect Dis. 2001;14:50–62. doi: 10.1086/317550. [DOI] [PubMed] [Google Scholar]
- Baddley JW, Benjamin DK Jr, Patel M, Miró J, Athan E, Barsic B, Bouza E, Clara L, Elliott T, Kanafani Z, Klein J, Lerakis S, Levine D, Spelman D, Rubinstein E, Tornos P, Morris AJ, Papa P, Fowler VG Jr, Chu VH, Cabell C. The International Collaboration on Endocarditis-Prospective Cohort Study Group (ICE-PCS) Candida infective endocarditis. Eur J Clin Microbiol Infect Dis. 2008;14:519–529. doi: 10.1007/s10096-008-0466-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boland JM, Chung HH, Robberts FJL, Wilson WR, Steckelberg JM, Baddour LM, Miller DV. Fungal prosthetic valve endocarditis: Mayo Clinic experience with a clinicopathological analysis. Mycoses. 2011;14:354–360. doi: 10.1111/j.1439-0507.2010.01884.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Embolic events and in-hospital mortality.
Embolic events and surgery.
Left-sided IE: univariate analysis of factors associated with embolism.
Left-sided IE: size of vegetation. Receiver operating characteristic analysis for the prediction of embolic events, based on vegetation size.
Left-sided IE: multivariate analysis of factors associated with embolism.