Abstract
A telephone survey of 1166 community resident seniors (658 male, 508 female, age between 65 and 97 years, mean 74.8 years) was undertaken, which included among other components telephone versions of the Pittsburgh Sleep Quality Index (PSQI), the Epworth Sleepiness Scale (ESS), and the Sleep Timing Questionnaire (STQ). The median PSQI score was 5 and the median ESS score 6, suggesting that neither sleep problems, nor daytime sleepiness problems, were particularly prevalent in this sample of seniors. The STQ indicated that the habitual timing of the sleep episode appeared to be within the usual 11 pm to 7:30 am range, with about 7.5 hours of actual sleep within that interval being reported. There was, however, a sizable minority who broke this pattern, with 25% of the sample reporting less than 6.7 hours of sleep, and problems with nocturnal sleep and daytime sleepiness.
Keywords: sleep, sleepiness, bedtime, rise-time, old, aging, Epworth, PSQI
Introduction
Many reports about the sleep of seniors—those aged older than 65 years—start with a sentence or two about how much seniors suffer from sleep disruption.1–3 There are often several assumptions made regarding the timing and quality of sleep in older adults. Sleep is presumed to be shorter and less refreshing, bedtime and rise-time are presumed to be very early, and unwanted daytime sleepiness is presumed to be pervasive. Not all of these presumptions are supported by strong empirical data and some might instead be characterized as more anecdotal, perhaps reflecting stereotypical beliefs about older adults or a concentration on the pathologies of aging, rather than aging effects per se.4 The present paper sought to provide empirical data on the timing, quality, and duration of sleep, as well as levels of daytime sleepiness, in a large sample of community-dwelling seniors. A group of 1166 retired seniors from Western Pennsylvania, USA were given an extensive telephone interview, which included detailed questions about sleep and sleepiness.
With regard to sleep quality, the conventional wisdom in the field, as described in several authoritative reviews,5–7 is that older adults experience much greater fragility in their sleep than do younger adults. Thus, in older adults, the deeper levels of sleep are less evident, there are more bouts of unwanted wakefulness during the night, and there is a tendency to wake earlier than desired. Among other possible etiologies, a weaker circadian system has been blamed for at least some of this sleep disruption.8,9 However, as we have noted in a 2005 review,10 at least in the case of healthy older women, circadian rhythms can be as robust as those observed in young adult men. Similarly, having conducted a meta-analysis of the sleep of 3577 subjects covering the whole lifespan, Ohayon and colleagues4 have suggested that age-related effects in seniors may be best regarded as subtle and, to a great extent, dependent upon the level of health of the individual. There also remains the paradox that older women are more likely than older men to report sleep problems, despite showing better sleep consolidation and more of the deeper levels of sleep, as measured by polysomnography in the laboratory.11 In terms of sleep duration, older adults are reported to sleep less than younger adults; a debate has raged about whether this is due to lower sleep need or instead to an impaired ability to maintain sleep.12
With regard to sleep timing, there is evidence from both circadian rhythms and diary measures8,10,13 that older adults do indeed have earlier phasing circadian rhythms (usually by 1–2 hours) and have reliably earlier bedtimes than younger adults. Evidence regarding the latter is not, however, particularly strong.14 Seniors do score reliably higher (more morning-type) than younger adults in questionnaires assessing chronotype.8,15
With regard to unwanted daytime sleepiness, the evidence can be confusing for two major reasons. First, many retired seniors are able—and indeed sometimes find it pleasant—to take a daytime nap, often in the early afternoon. The complication is that the nap may not always reflect the need for daytime sleep (ie, the presence of any pathology). In our 2001 study,16 which conducted a within-participants comparison of healthy older seniors (75 years or older) with and without afternoon naps in a 17 day protocol, there was strong evidence both that participants who did not habitually nap could indeed do so and that in doing so nocturnal sleep was not adversely affected. The second reason that the area of daytime sleepiness in the elderly can be confusing is that seniors are often victims of influences such as medications, illness, and poor nocturnal sleep, which can themselves lead to daytime sleepiness. The influence of illnesses and medications may relate to poorer health in some of the seniors for whom napping occurs. In turn, such influences may be why the presence of daytime napping in the elderly has been found by some to be associated with worsening of morbidity and mortality.17
As part of a 5-year telephone interview study of retired shift workers and day workers, we had the opportunity to investigate the issues of sleep quality, sleep timing, and daytime sleepiness in a group of 1166 retired older adults. Other aspects of this study have been and will be reported elsewhere.18,19 Among other variables, the interview included telephone versions of the Pittsburgh Sleep Quality Index (PSQI),20 the Epworth Sleepiness Scale (ESS)21 and the Sleep Timing Questionnaire (STQ).22 The aim of this analysis was to provide normative empirical data regarding these variables in a sample of Western Pennsylvanian retirees.
Methodology
Telephone survey methodology
The telephone survey lasted approximately 20–30 minutes and comprised a detailed work history as well as telephone-modified versions of various questionnaires. It was conducted by the Survey Research Program of the University Center for Social and Urban Research (UCSUR), which maintains a highly experienced staff of survey professionals as well as a pool of experienced interviewers. Commercially available lists of telephone numbers were purchased which had a high likelihood of having older persons in the household. Postal codes in the Greater Pittsburgh area that were more likely to have retired shift workers were over-sampled and emphasis placed on particular shift work exposure categories,19 leading to an increased representation of retired shift workers in the current sample. Thus, 66% of the sample had done at least one year of shift work at some time in their working life. This may not be typical for seniors in general, although there are undoubtedly geographical influences. The present study took place in a region in which steel making and health care (which both involve considerable shift work) were the major industries during the working lives of our participants. Issues regarding differences in sleep and chronotype between retired shift workers and retired day workers within this sample have been discussed in detail elsewhere.19 To summarize, retired shift workers went to bed an average of only 13 minutes later than retired day workers; the groups did not differ on a questionnaire assessing morningness-eveningness,23 but retired shift workers reported worse sleep than retired day workers by about one PSQI unit.19
As a consequence of the above mentioned sampling strategies, the survey was not a true random sample of older people, but participants were not totally self-selected, as would be the case were the survey to rely upon other methods such as responses to advertisements. It was not a probability sample, rather an age-targeted list-based sample. Thus, we cannot make claims that the results are from a representative population-based sample. As noted below, there are also issues related to the 33% response rate.
The survey instrument was programmed into UCSUR's Computer-Assisted Telephone Interviewing (CATI) system. CATI surveys involve programming the survey, with the interviews conducted at personal computers that displayed the questions in proper order. This technology eliminated the need for paper call records and manual data entry and instead allowed the interviewers to concentrate on conducting high quality interviews. In order to maximize response rates, at least 8 calls were made on varying days of the week at different times to maximize the probability of contacting respondents, and attempts were made to convert initial refusals into completed interviews.
The first section of the interview screened the household for retired residents 65 or older, asking if they would then come to the phone. Then, following permission being given to proceed, questions were asked regarding former employment. This involved the taking of a detailed work history, including questions about shift work schedules. The questionnaires relating to daytime sleepiness and nocturnal sleep quality and timing, as well as other questionnaires regarding circadian rhythms, mood, and health, then followed. We developed telephone versions of the Pittsburgh Sleep Quality Index (PSQI),20 the Epworth Sleepiness Scale (ESS),21,24 and the Sleep Timing Questionnaire (STQ).22,24 The PSQI has become a gold-standard instrument for measuring subjective sleep quality.25 It comprises 18 questions which yield a whole number total score ranging from 0 to 21, with higher scores representing more sleep problems. A score above 5 is considered indicative of poor sleep quality. The ESS has become the gold- standard instrument for measuring unwanted daytime sleepiness.25 It comprises 8 questions which yield a score between 0 and 24, with higher scores indicating more unwanted daytime sleepiness. A score below 8 is considered normal, 8–81 mild, 12–25 moderate, and 16–24 severe. The STQ22 is a questionnaire designed to obtain similar information from that obtained from a week-long sleep diary, but instead in a one-off questionnaire. It yields estimates of habitual bedtime, rise-time, sleep latency, and minutes of wakefulness after sleep onset. Because all participants were retired, no distinction was made between work-days and weekends in the STQ. PSQI questions concerning snoring as reported by a bed-partner, which do not contribute to the overall PSQI score, were not included in the telephone interview. There were also a few simple questions to glean information regarding physical health and demographic information.19 The interview was anonymous and had been ruled as exempt (not requiring signed informed consent) by the University of Pittsburgh Institutional Review Board (IRB). The study conformed to the Declaration of Helsinki.
Participants
All participants were required to be 65 years or older, to have been in the workforce in the past, to have not done any shift work in the past 12 months, and to be retired, meaning not working for pay for more than 10 hours per week outside the home. Both men and women were eligible, and race was not a factor in participant recruitment. All participants lived in the Greater Pittsburgh Area of Western Pennsylvania, USA. All participants were required to speak and understand English and to be cognitively able to understand and answer the questions asked of them.
We contacted 3545 eligible possible interviewees. Of these, 1207 eligible respondents refused to participate, 292 could not be re-contacted to complete the interview, and 315 eligible respondents were unable to participate due to health, physical, or cognitive problems. A total of 1731 interviews were started, but 565 of these represented individuals whose work history responses seemed to the interviewer to be dubious and/or confused. This left a total of 1166 participants who were included in the present analysis (658 men, 508 women); ages ranged from 65 years to 97 years (mean: 74.8 years, standard deviation: 6.4 years). For some variables, sample sizes were reduced due to incomplete answers being given (see final row of Table 1). The loss of 1207 eligible participants to refusal indicates a refusal rate of 34%, a further 17% were lost to health, cognitive, or availability issues, and a further 16% because of a dubious or confused work history. Thus, the sample size of 1166 represents 33% of the eligible participants we initially contacted. As noted in the discussion, this does limit the generality of the present findings.
Table 1.
Summary statistics (n = 1166).
| PSQI | ESS | Bed-time | Rise-time | Time in bed | Total sleep time | |
|---|---|---|---|---|---|---|
| Mean | 5.70 | 6.26 | 23:15 | 07:32 | 08:16 | 07:30 |
| s.d. | 3.65 | 3.75 | 75m | 85m | 78m | 84m |
| 25%ile | 3 | 4 | 22:30 | 06:30 | 07:30 | 06:40 |
| Median | 5 | 6 | 23:00 | 07:30 | 08:15 | 07:35 |
| 75%ile | 8 | 9 | 00:00 | 08:30 | 09:00 | 08:20 |
| % loss | 7.3 | 3.3 | 0.6 | 0.1 | 0.7 | 4.0 |
Notes: Pittsburgh Sleep Quality index (PSQI) and Epworth Sleepiness Scale (ESS) scores are in their respective units; times are given in military time, m denotes minutes, %ile denotes percentile, s.d. denotes standard deviation. The final row of the table reports the % data loss (due to incomplete answers) for each variable.
Data analysis
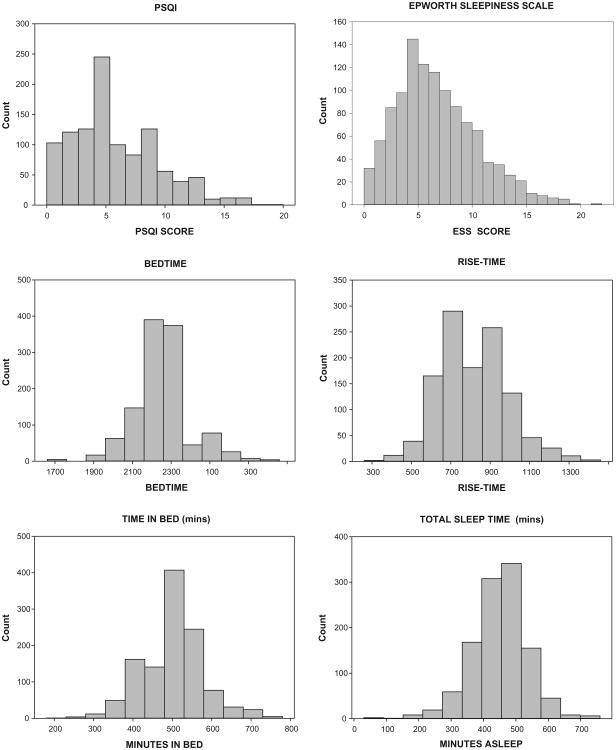
The following major outcome variables were considered in this analysis: (1) Overall sleep quality as measured by the PSQI total score; (2) Level of daytime sleepiness as measured by the ESS score; Two measures of sleep timing from the STQ; (3) Habitual bedtime; and (4) Habitual rise-time. Additionally, the following measures were derived from the STQ; (5) Habitual Time in Bed (TIB) [TIB = minutes between bedtime and rise-time]; and (6) Habitual Total Sleep Time (TST) [TST = TIB minus (sleep latency plus wake after sleep onset)]. For all variables, frequency histograms were plotted and various summary statistics reported (mean, standard deviation, 25th percentile, median, 75th percentile).
Findings
Figure 1 illustrates the frequency histograms for the six variables. The summary statistics are given in Table 1. The median PSQI score was 5 and the ESS score 6. The sample habitually spent a little over 8 hours in bed (TIB), with a mean bedtime of 23:15, and rise-time of 07:32; 7.5 hours of the in-bed episode was reported to be time spent asleep (TST).
Figure 1.
Frequency histograms for each of the six variables.
Notes: Pittsburgh Sleep Quality index (PSQI) and Epworth Sleepiness Scale (ESS) scores are in their respective units; clock times are given in military time, time durations are given in minutes.
Discussion
The present results suggest that caution is needed in interpreting the conventional wisdom regarding the prevalence of troubled sleep and unwanted sleepiness in retired seniors. With a median PSQI score of 5, fully half of our sample was at or below (ie, slept better than) the criterion score of 5 which is considered indicative of sleep problems. In a similar vein, the median ESS score was 6, indicating that more than half of our sample was below (ie, less sleepy than) the criterion of less than 8 considered to be normal in terms of daytime sleepiness level, for any age group. Thus, in this sample at least, neither disrupted sleep nor excessive daytime sleepiness was particularly pervasive. As noted in the section describing the participants, only 33% of eligible participants who were initially contacted remained in the present sample of 1166. Although typical for cold calling within this age group, this does limit the generality of the present findings. This study did not intend to be a true random sample and the findings must therefore be viewed with caution.
The median PSQI score of 5 is very close to the mean score of 4.8 reported for a much smaller (n = 44) sample of seniors,26 and slightly lower than a median score of 6 found in a 2008 Pittsburgh study of 187 participants with a mean age of 59, in which minorities were over-sampled and retirement not required.25 The difference between the two studies in median PSQI score may be at least partially a consequence of our retirement requirement, since retirement per se has been shown to improve sleep.27 In the 2008 Pittsburgh study, the median ESS score was found to be 8,25 again slightly worse than that found in the present sample.
Of course, having made the above conclusions about PSQI and ESS scores being relatively good, the important corollary is that half of our sample did report a PSQI score indicative of sleep problems and that the 75th percentile score of 8 indicated that a sizeable minority had significant sleep issues. Likewise, the 75th percentile ESS score was 9, which is within the mild sleepiness range of ESS scores. Thus, there were some seniors within this sample for whom nocturnal sleep and daytime sleepiness were significant issues.
The present PSQI estimate may actually be an overly high (ie, worse) estimate because the present study deliberately oversampled retired shift workers—as noted above, 66% of the present sample had experienced at least one year of shift work during their working lives. As we discuss elsewhere,19 retired shift workers have PSQI scores that are about one unit higher (ie, worse) than retired day workers. It should be noted, though, that this makes our present conclusions about good sleep in seniors more, rather than less, conservative.
With regard to the timing of the sleep episode, the advantage of this sample is that all participants were retired, allowing them to avoid the constraints of the work week. Thus, their bedtimes and rise-times were of their own choosing. As was the case with the PSQI and the ESS, conventional wisdom regarding the purported extremely early bedtimes and rise-times of seniors was not supported by the data. With a median bedtime of 23:00, fully half of our sample was going to bed at or after 11 pm. Indeed, one quarter of our sample was going to bed at or after midnight. The same was true with regard to rise-times. Half of our sample was rising at or after 7:30 am and one quarter was rising at or after 8:30 am. In both cases, though, there was a standard deviation of more than one hour around the mean times, allowing for a sizable minority of participants to be going to bed and/or awakening extremely early. The value for bedtime in this sample may also have been slightly influenced by the over-representation of retired shift workers, since we have shown elsewhere19 that they have slightly (13 minutes) later bedtimes than retired day workers.
In a similar vein, both TIB and TST were in line with earlier diary findings from middle aged and younger adults (20 years–50 years) in the same geographical area.28 Taking the weekend data from that study (n = 266), mean TIB was 7.9 hours and TST was 7.6 hours, which are comparable to the figures of 8.3 hours (TIB) and 7.5 hours (TST) found in our current seniors. Again, it should be remembered that there was a standard deviation of more than 75 minutes around these means; the lowest 25th percentile was reporting TST values of less than 6.7 hours. Thus as with the other variables, although the majority of our sample of seniors reported very similar values to those of young and middle-aged adults, there appeared to be a sizeable minority with very different values. Unfortunately, we did not assess napping behavior in the telephone interview, so it was possible that the 24 hour TST figure might be even greater were daytime naps to be included.
Conclusions
In a large sample of Western Pennsylvania seniors with an over-representation of retired shift workers, sleep quality and daytime sleepiness levels were within normal limits, although a sizable minority did report problems. The habitual timing of the sleep episode for this sample appeared to be mostly within the usual 11 pm to 7:30 am range, with about 7.5 hours of actual sleep within that interval being reported. There was, however, a sizable minority who broke this pattern, with 25% of the sample reporting less than 6.7 hours of sleep, and problems with nocturnal sleep and daytime sleepiness.
Recommendations
It is recommended that care should be exercised in making assumptions about the quality and timing of nocturnal sleep and the level of daytime sleepiness experienced by most seniors—those 65 years of age or older—which may all be very similar to those of younger adults. It should be recognized that a sizeable minority of seniors do, however, experience problems with nocturnal sleep and daytime sleepiness.
Limitations of the study
There were a couple of key limitations in this study. The study was specific to a particular geographical area (Western Pennsylvania, USA) and there was an over-sampling of retired shift workers. Additionally, daytime napping was not assessed.
Acknowledgments
Special thanks are owed to Jean Miewald and Mary Fletcher for help with data analysis, to Kathy Kennedy and Mary Gasiorowski for administrative help, to Melissa Clark for pilot work, to the UCSUR team of interviewers for their hard work, and to our participants for their time.
Funding: Support for this work was provided by U.S. National Institute on Aging Grants AG-13396 and AG-20677, and by RR-024153. Neither the University of Pittsburgh, nor the funding agencies, necessarily hold the views reported in this paper.
Footnotes
Competing Interests: DJB has received consulting fees from Eisai, Merck, Philips Respironics and Purdue Pharma and payment for lecturing from Servier and Astellas. Other authors disclose no competing interests.
Author Contributions: Originally conceived, designed and supervised the execution of the study and the analysis of the results: THM. Collaborated in the design and execution of the study: DJB, SRB, JES. Wrote the first draft of the manuscript: THM. Edited and contributed text to the manuscript: DJB, SRB, JES.
Disclosures and Ethics: As a requirement of publication author(s) have provided to the publisher signed confirmation of compliance with legal and ethical obligations including but not limited to the following: authorship and contributorship, conflicts of interest, privacy and confidentiality and (where applicable) protection of human and animal research subjects. The authors have read and confirmed their agreement with the ICMJE authorship and conflict of interest criteria. The authors have also confirmed that this article is unique and not under consideration or published in any other publication, and that they have permission from rights holders to reproduce any copyrighted material. Any disclosures are made in this section. The external blind peer reviewers report no conflicts of interest.
This article is available from http://www.la-press.com.
References
- 1.Tozawa T, Mishima K, Satoh K, Echizenya M, Shimizu T, Hishikawa Y. Stability of sleep timing against the melatonin secretion rhythm with advancing age: clinical implications. J Clin Endocrinol Metab. 2003 Oct;88(10):4689–95. doi: 10.1210/jc.2003-030147. [DOI] [PubMed] [Google Scholar]
- 2.Cole C, Richards K. Sleep disruption in older adults. Harmful and by no means inevitable, it should be assessed for and treated. Am J Nurs. 2007 May;107(5):40–9. doi: 10.1097/01.NAJ.0000268167.48606.74. [DOI] [PubMed] [Google Scholar]
- 3.Spira AP, Stone K, Beaudreau SA, Ancoli-Israel S, Yaffe K. Anxiety symptoms and objectively measured sleep quality in older women. Am J Geriatr Psychiatry. 2009 Feb;17(2):136–43. doi: 10.1097/JGP.0b013e3181871345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004 Nov 1;27(7):1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 5.Ancoli-Israel S. Sleep and aging: prevalence of disturbed sleep and treatment considerations in older adults. J Clin Psychiatry. 2005;66(9):24–30. [PubMed] [Google Scholar]
- 6.Bliwise DL. Normal Aging. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th. Philadelphia, PA: Elsevier Saunders; 2005. pp. 24–38. [Google Scholar]
- 7.Vitiello MV. Sleep disorders and aging: understanding the causes. J Gerontol A Biol Sci Med Sci. 1997 Jul;52(4):M189–91. doi: 10.1093/gerona/52a.4.m189. [DOI] [PubMed] [Google Scholar]
- 8.Czeisler CA, Dumont M, Duffy JF, et al. Association of sleep-wake habits in older people with changes in output of circadian pacemaker. Lancet. 1992;340:933–6. doi: 10.1016/0140-6736(92)92817-y. [DOI] [PubMed] [Google Scholar]
- 9.Duffy JF, Willson HJ, Wang W, Czeisler CA. Healthy older adults better tolerate sleep deprivation than young adults. J Am Geriatr Soc. 2009 Jul;57(7):1245–51. doi: 10.1111/j.1532-5415.2009.02303.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monk TH. Aging human circadian rhythms: Conventional wisdom may not always be right. J Biol Rhythms. 2005;20(4):366–74. doi: 10.1177/0748730405277378. [DOI] [PubMed] [Google Scholar]
- 11.Reynolds CF, Kupfer DJ, Taska LS, et al. EEG sleep in elderly depressed, demented, and healthy subjects. Biol Res. 1985;20:431. doi: 10.1016/0006-3223(85)90045-9. [DOI] [PubMed] [Google Scholar]
- 12.Ancoli-Israel S, Alessi C. Sleep and aging. Am J Geriatr Psychiatry. 2005 May;13(5):341–3. doi: 10.1176/appi.ajgp.13.5.341. [DOI] [PubMed] [Google Scholar]
- 13.Monk TH, Thompson WK, Buysse DJ, Hall M, Nofzinger EA, Reynolds CF. Sleep in healthy seniors: a diary study of the relation between bedtime and the amount of sleep obtained. J Sleep Res. 2006;13(3):256–60. doi: 10.1111/j.1365-2869.2006.00534.x. [DOI] [PubMed] [Google Scholar]
- 14.Bliwise DL, Ansari FP, Straight LB, Parker KP. Age changes in timing and 24-hour distribution of self-reported sleep. Am J Geriatr Psychiatry. 2005 Dec;13(12):1077–82. doi: 10.1176/appi.ajgp.13.12.1077. [DOI] [PubMed] [Google Scholar]
- 15.Monk TH, Reynolds CF, Buysse DJ, et al. Circadian characteristics of healthy 80 year olds and their relationship to objectively recorded sleep. J Geront Med Sci. 1991;46(5):M171–5. doi: 10.1093/geronj/46.5.m171. [DOI] [PubMed] [Google Scholar]
- 16.Monk TH, Buysse DJ, Carrier J, Billy BD, Rose LR. Effects of afternoon “Siesta” naps on sleep, alertness, performance, and circadian rhythms in the elderly. Sleep. 2001;24(6):680–7. doi: 10.1093/sleep/24.6.680. [DOI] [PubMed] [Google Scholar]
- 17.Foley DJ, Vitiello MV, Bliwise DL, Ancoli-Israel S, Monjan AA, Walsh JK. Frequent napping is associated with excessive daytime sleepiness, depression, pain, and nocturia in older adults: findings from the National Sleep Foundation ‘2003 Sleep in America’ Poll. Am J Geriatr Psychiatry. 2007 Apr;15(4):344–50. doi: 10.1097/01.JGP.0000249385.50101.67. [DOI] [PubMed] [Google Scholar]
- 18.Monk TH, Buysse DJ, Billy BD, et al. Circadian type and bed-timing regularity in 654 retired seniors: correlations with subjective sleep measures. Sleep. 2011 Feb;34(2):235–9. doi: 10.1093/sleep/34.2.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Monk TH, Buysse DJ, Billy BD, et al. Shiftworkers report worse sleep than day workers, even in retirement. J Sleep Res. 2012 doi: 10.1111/jsr.12003. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 21.Johns MW. Sleepiness in different situations measured by the Epworth Sleepiness Scale. Sleep. 1994 Dec;17(8):703–10. doi: 10.1093/sleep/17.8.703. [DOI] [PubMed] [Google Scholar]
- 22.Monk TH, Buysse DJ, Kennedy KS, Potts JM, DeGrazia JM, Miewald JM. Measuring sleep habits without using a diary: The sleep timing questionnaire (STQ) Sleep. 2003;26(2):208–12. doi: 10.1093/sleep/26.2.208. [DOI] [PubMed] [Google Scholar]
- 23.Smith CS, Reilly C, Midkiff K. Evaluations of three circadian rhythm questionnaires with suggestions for an improved measure of morningess. J Appl Psychol. 1989;74(5):728–38. doi: 10.1037/0021-9010.74.5.728. [DOI] [PubMed] [Google Scholar]
- 24.Johns MW. A new method for measuring daytime sleepiness: the epworth sleepiness scale. Sleep. 1991;14(6):540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 25.Buysse DJ, Hall ML, Strollo PJ, et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008 Dec 15;4(6):563–71. [PMC free article] [PubMed] [Google Scholar]
- 26.Buysse DJ, Reynolds CF, Monk TH, Hoch CC, Yeager AL, Kupfer DJ. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI) Sleep. 1991;14(4):331–8. [PubMed] [Google Scholar]
- 27.Vahtera J, Westerlund H, Hall M, et al. Effect of retirement on sleep disturbances: the GAZEL prospective cohort study. Sleep. 2009 Nov;32(11):1459–66. doi: 10.1093/sleep/32.11.1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Monk TH, Buysse DJ, Rose LR, Hall JA, Kupfer DJ. The sleep of healthy people—A diary study. Chronobiol Int. 2000;17(1):49–60. doi: 10.1081/cbi-100101031. [DOI] [PubMed] [Google Scholar]