Abstract
We explored how the perception of stiffness can be distorted in Minimally Invasive Surgery. We combined a mechanical simulator with a haptic device, and implemented linear springs at the tip of the simulated laparoscopic device. To explore the influence of mechanical advantage on perception, we set different values of the ratio between internal and external length of the tool. We found that a nonsymmetrical ratio causes bias in the perceived stiffness when novice tangential probing is compared to radial probing. In contrast, haptic experts did not show similar perceptual bias.
Keywords: Perception, Stiffness, Fulcrum Effect, Minimally Invasive Surgery, Simulation, Haptic
Introduction
In laparoscopy, a form of Minimally Invasive Surgery (MIS), the surgeon operates with elongated instruments through a small incision in the abdominal wall of the patient. Reduced blood loss, pain, complications, and hospitalization time, and improved cosmesis are just examples of the vast advantages of MIS over traditional open surgery. However, when surgeons perform surgical maneuvers through the laparoscope, their motor control system faces various challenges due to the “fulcrum effect” of the mechanical constraint at the incision point. These challenges include inversion and scaling of movements, altered sensation of forces due to mechanical advantage and friction at the incision point [1]. While the fulcrum effect was studied extensively in the context of laparoscopic performance [2–4], haptic perception through the laparoscopic device has not received as much attention.
In recent studies, investigators have studied the importance of haptic perception in laparoscopy [5, 6]. For example, addition of force feedback reduces excessive forces and errors in blunt dissection [7]. Furthermore, it has been suggested that the increased level of bile duct injuries in laparoscopy [8, 9] might be due to distorted haptic feedback, as the errors leading to laparoscopic bile duct injuries stem principally from misperception, and not errors of skill [10]. This is probably the reason that for complicated laparoscopic procedures, a hand assisted technique is used to allow more efficient palpation [11, 12].
Laparoscopic surgery is a skill requiring extensive training [13]. Differences in both performance and strategies were found between expert surgeons and novices [7, 13, 14]. Extensive research has been conducted to assess and improve laparoscopic skills acquisition, including development of a large variety of mechanical simulators [15], and in the recent years, virtual reality based simulators [13, 16].
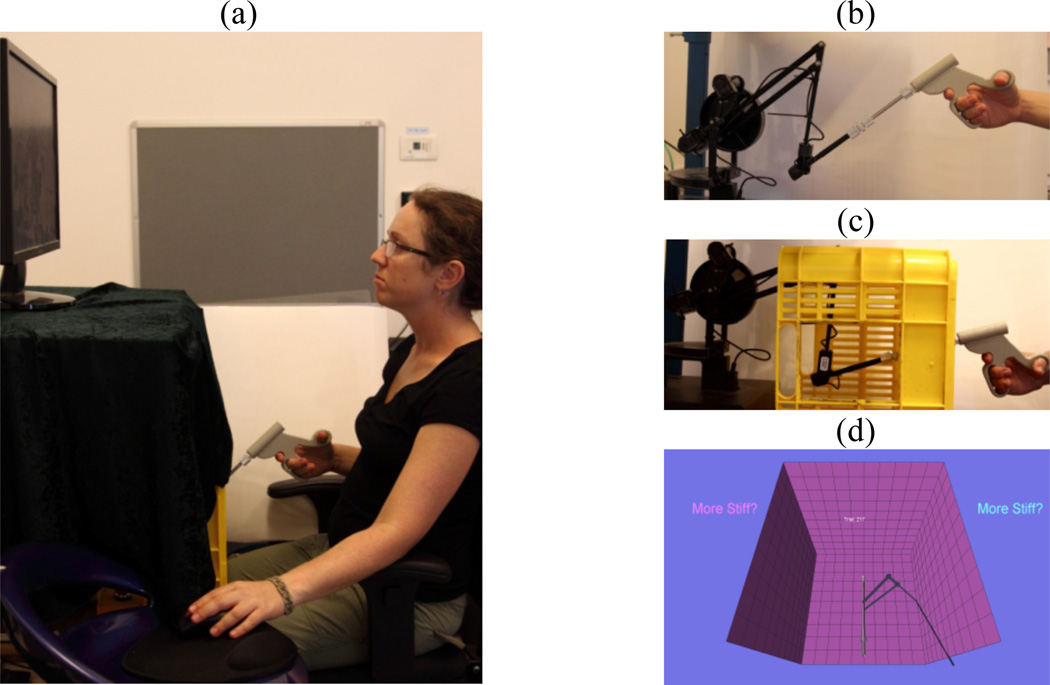
In the current study, we wished to understand basic underlying challenges to performance in laparoscopy. We designed an experimental setup for exploring the effect of the fulcrum on perception of mechanical properties in MIS. We combined a mechanical simulator with a haptic device (Figure 1a–c), and designed a system that applies computer generated forces at the tip of a long tool which is manipulated through a small incision. The forces applied by the system can in principle be any function of the position of the tip of the tool and its derivatives.
Figure 1.
Experimental setup: (a) Seated participant holds the custom made handle of mechanical device. (b)The handle is connected to the haptic device through an aluminum rod that is inserted into a box (c) through small opening. The participant is presented with a 2D version of the environment.
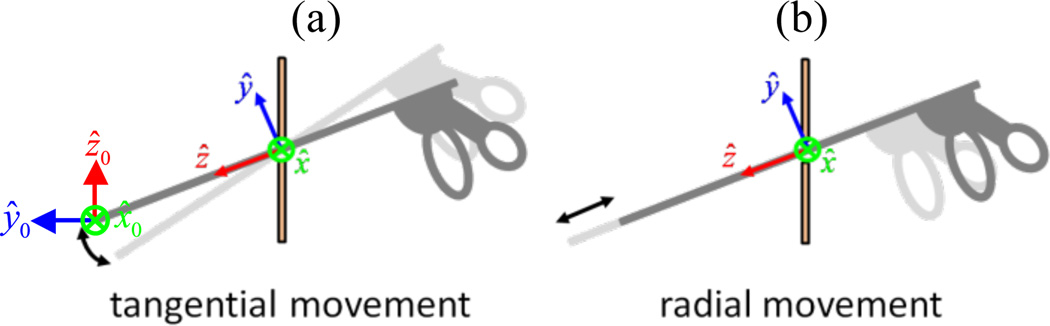
While practical conditions feature complex surgical procedures and a variety of tissue properties, we devised a simplified task as a basic test of our ideas. Hence, we focused on perception of stiffness, and as a prototype of the simulated surgical environment we implemented linear elastic force fields. We considered two fundamental types of movements that are commonly executed in laparoscopy. When moving tools through a small incision, the surgeon can push the tool through the incision (translation along the tool longitudinal axis – ẑ in Figure. 2) – we call it radial movement – or rotate the tool about the incision (rotation about any axis that is perpendicular to the tool longitudinal axis – e.g. x̂ in Figure 2) – we call it tangential movement. Note, that these two movements are strikingly different: the latter is affected by the fulcrum effects, and therefore there is inversion and scaling of motion and reciprocal inversion and scaling of forces. The former movement does not suffer from these effects.
Figure 2.
Two movement types: radial movement (R probing) and tangential movement (T probing)
1. Methods
Thirty-two novice volunteers and three haptic experts (graduate students at the Computational Motor Control Lab) participated in the experiment after signing the informed consent form as stipulated by the local Helsinki Committee. Due to technical calibration reasons, the results of five novice volunteers were not analyzed.
Seated participants held the handle of a long tool that was connected to a PHANTOM® Premium 1.5/6DOF haptic device, and looked at a screen which displayed a 2D representation of the tool inside the patient (Figure 1). We used a plastic box to simulate the abdomen of the patient. The region of the incision was covered with a 10×10×0.3cm rubber sheath such that the mechanical properties of the incision point would be less rigid and more similar to the rubber seal of the trocar in MIS. To minimize the effect of friction, the incision was slightly larger than the tool. The haptic device exerted forces on the tip of the tool at 1KHz and acquired its trajectory at 100Hz.
To explore the perception of stiffness with radial (R) and tangential (T) movements, we used a forced choice paradigm, similar to the one that is described elsewhere in detail [17, 18]. In each trial, participants were presented with a pair of virtual springs with different levels of stiffness: one, reference, was always K=0.07N/mm, and second, stimulus, was one of eight stiffness levels K={0.025, 0.038, 0.051, 0.064, 0.076, 0.089, 0.102, 0.115}N/mm.
Each of the springs within a trial was either an R or a T compression spring; namely, the force that was applied by the haptic device was calculated according to:
| (1) |
where x⃗ is the sampled position of the haptic device, and x⃗h is the home position, and all vectors are written relative to the zero reference frame (x̂0, ŷ0, ẑ0) in figure 2. The home position was chosen such that the R probing is indeed translation along ẑ in Figure 2, and T probing is rotation about x̂.
In each probing, participants positioned the tool at home position, and were instructed to probe a spring using either R or T movements. They were free to switch between the springs in the pair until they were confident about their answer. In the current study, we focused on the haptic modality, and therefore, the visual scene froze during interaction with the springs. Such lack of visual information is relevant in clinical situations when the target tissue is obscured from view by other anatomical structures.
Each subject performed a protocol where all stimulus stiffness levels were repeated 9 times each, in all three conditions – RR (reference and stimulus movements are R), TT (reference and stimulus movements are T), and RT (reference movements are R and stimulus are T). To explore the influence of mechanical advantage of the laparoscopic tool, in each experiment, we set one of three different values of the ratio between internal (li) and external (lo) lengths of the tool: Short, Symmetric, and Long, as specified in Figure 3. Each novice participant performed one of such experiments (nShort=9, nSymmetric=8, and nLong=10), and each expert participated first in the Long and then in the Short experiment.
Figure 3.
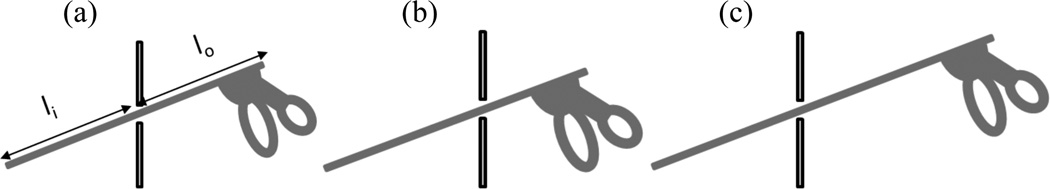
Three experimental conditions – length ratios: (a) Symmetric: li=lo=17cm, (b) Short: li=17cm, lo=14cm, (c) Long: li=17cm, lo=20cm
After positioning their tool in the home position, some of the participants changed their actual li/lo by either pushing or pulling the tool. Thus, for each of the participants we derived the actual length ratio li/lo by calculating the median shift across all tangential movements.
We used a procedure that is described elsewhere in detail [17, 18] to fit psychometric functions to the probability of answering that stimulus spring was stiffer as a function of the difference between stimulus and reference springs [19]. For each participant three such curves were fitted – for the RR, TT, and RT conditions. From each of these curves we extracted the point of subjective equality (PSE) – the difference in stiffness levels that was perceived to be zero, namely, the bias in perception. Positive PSE means underestimation of stimulus stiffness, and negative PSE means overestimation. Therefore, the PSERR and PSETT are expected to be zero, and PSERT is expected to reveal the bias in perception due to tangential probing. We used PSERT to calculate the ratio between the perceived (Kot) and actual (Ki) stiffness levels in tangential probing, according to:
| (2) |
2. Predictions
When tangential movements are used for interaction with the spring there is a scaling in positions and forces. In the following paragraph, we use i subscript to denote “inside” the abdominal box, and o subscript to denote “outside” the abdominal box. The scaling in position and force is thus Δxi = (li/lo)Δxo and Δfo = (li/lo)Δfi respectively, and the stiffness of a spring Ki = Δfi/Δxi is scaled as Kot = (li/lo)2 Ki. However, in the radial case, no such scaling occurs at all, and therefore, Kor = Ki. Therefore, if no compensation for tool length ratio occurs in the perceptuomotor system of the participants, we expect to observe a positive shift in PSERT in the Long experiments, and a negative shift in the Short experiments. Taking together the data of all subjects (novices and experts separately) we expect to find:
| (3) |
However, if perfect compensation occurs, we expect no shift in perceived stiffness, namely:
| (4) |
3. Results
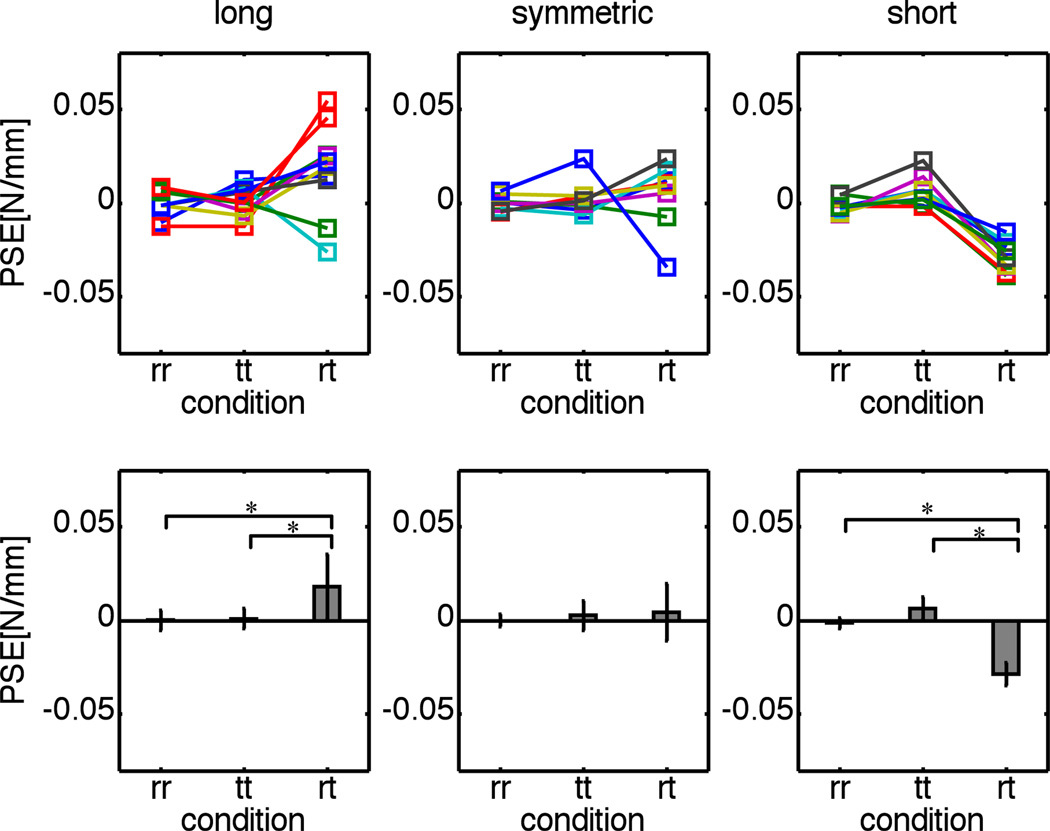
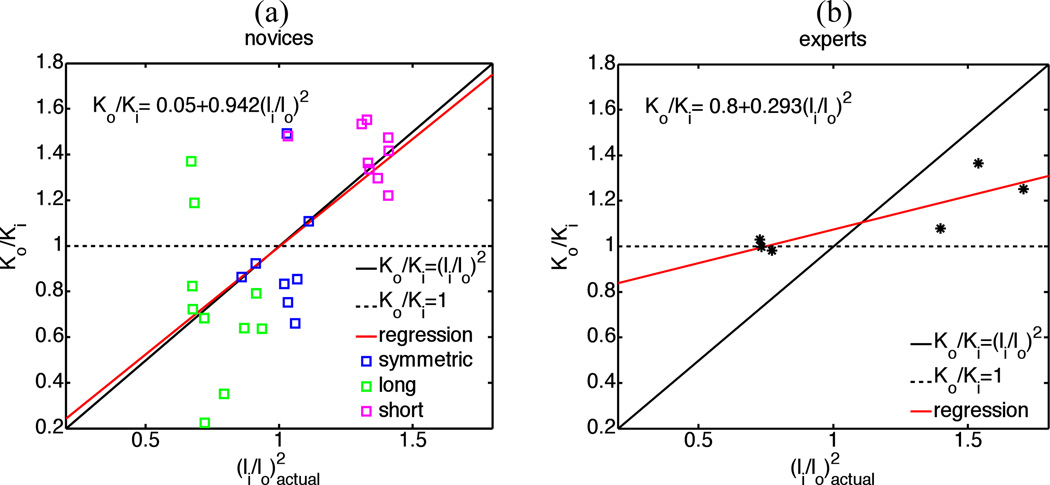
The individual PSE of all novices and averaged PSE are depicted in Figure 4. As expected, the PSERR and PSETT are not statistically significantly different from zero, and PSERT are shifted in the nonsymmetrical conditions: PSERT>0 in Long, PSERT=0 in Symmetrical, and PSERT<0 in Short experimental conditions. We performed 2-way ANOVA with repeated measures on one factor, and found statistically significant effect of length ratio (F2,72=10.55, p<0.001) and interaction between length ratio and probing direction (F4,72=13.82, p<0.001). The statistically significant (p<0.05) contrasts from post-hoc analysis with Bonferroni correction for multiple comparisons are specified in Figure 4. In addition, we calculated a regression between Kot/Ki and of all novice participants. The results of this analysis are depicted in Figure 5a, and they are consistent with Eq. (3). The parameters of the fitted regression line (estimation [lower CI limit, upper CI limit]) are 0.95 [0.5, 1.4] slope and 0.05 [−0.4, 0.5] interception. Taken together, these results suggest that novices were not able to compensate for the bias in perception of stiffness due to fulcrum effect.
Figure 4.
PSE of individual subjects (upper row) and estimation of mean PSE and 95% confidence intervals (bars and error bars respectively, lower row). * denotes statistically significant (p<0.05) difference between the estimated means in post-hoc analysis with Bonferroni correction.
Figure 5.
The ratio between the stiffness perceived in tangential movement and the actual stiffness as a function of actual squared ratio between internal and external lengths of the tool of novices (a) and haptic experts (b).The solid and dashed black lines represent the expected line of means according to the no compensation and full compensation hypotheses respectively. The symbols are data that was calculated according to Eq. (2) from the PSE that was extracted from the answers of subjects. The red line is the line of means that was fitted to the data using linear regression. The equation of this line appears on the panel, left upper corner.
The results of similar analysis of experts are presented in Figure 5b. The parameters of the fitted regression line are 0.29 [0, 0.5] slope and 0.8 [0.5, 1.1] interception. Thus, the results of haptic experts are much closer to be consistent with Eq. (4) than with Eq. (3). These results suggest that haptic experts were far more successful in compensating for the bias in perception.
4. Conclusions and Discussion
We explored perception of stiffness in laparoscopy, and focused on the perceptual consequences of the fulcrum effect. We compared perception of the stiffness of linear compression springs when probed using radial and tangential movements, and found that the fulcrum effect biases perception of stiffness in novices. The perceptual bias is consistent with a mechanical model for scaling of stiffness due to scaling of position and forces when moving about the pivot at the incision point.
Interestingly, the bias in the perception of haptic experts was observed to a much smaller degree, and only in Short condition. In future work, we plan to explore differences in probing strategies of novices and experts, and assess whether the difference is a result of some cognitive strategy. In addition, we plan to repeat the experiment with a group of clinical experts: experienced surgeons.
This study improves our understanding of the perceptual effects and distortions in haptic information during MIS and reveals key differences in perceptual and motor strategies employed by experts. These findings could aid in the development of training techniques for future surgeons and could contribute to improving surgical outcomes.
Acknowledgments
This research was supported by the Binational United States Israel Science Foundation and by NINDS grant 2R01NS035673. IN is supported by the Kreitman and Clore fellowships.
References
- 1.Westebring – van der Putten EP, et al. Haptics in minimally invasive surgery – a review. Minimally Invasive Therapy & Allied Technologies. 2008;17:3–16. doi: 10.1080/13645700701820242. [DOI] [PubMed] [Google Scholar]
- 2.Gallagher AG, et al. An Ergonomic Analysis of the Fulcrum Effect in the Acquisition of Endoscopic Skills. Endoscopy. 1998;30:617–620. doi: 10.1055/s-2007-1001366. [DOI] [PubMed] [Google Scholar]
- 3.Crothers IR, et al. Experienced Laparoscopic Surgeons are Automated to the “Fulcrum Effect”: An Ergonomic Demonstration. Endoscopy. 1999;31:365–369. doi: 10.1055/s-1999-26. [DOI] [PubMed] [Google Scholar]
- 4.Smith CD, et al. Assessing laparoscopic manipulative skills. The American Journal of Surgery. 2001;181:547–550. doi: 10.1016/s0002-9610(01)00639-0. [DOI] [PubMed] [Google Scholar]
- 5.Brydges R, et al. Surface exploration using laparoscopic surgical instruments: The perception of surface roughness. Ergonomics. 2005;48:874–894. doi: 10.1080/00140130500123704. [DOI] [PubMed] [Google Scholar]
- 6.Zhou M, et al. Role of Haptic Feedback and Cognitive Load in Surgical Skill Acquisition. Human Factors and Ergonomics Society Annual Meeting Proceedings. 2007;51:631–635. [Google Scholar]
- 7.Wagner CR, et al. The benefit of force feedback in surgery: examination of blunt dissection. Presence: Teleoperators and Virtual Environments. 2007;16:252–262. [Google Scholar]
- 8.Archer SB, et al. Bile Duct Injury During Laparoscopic Cholecystectomy: Results of a National Survey. Annals of Surgery. 2001;234:549–559. doi: 10.1097/00000658-200110000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deziel DJ, et al. Complications of laparoscopic cholecystectomy: A national survey of 4,292 hospitals and an analysis of 77,604 cases. The American Journal of Surgery. 1993;165:9–14. doi: 10.1016/s0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- 10.Way LW, et al. Causes and Prevention of Laparoscopic Bile Duct Injuries: Analysis of 252 Cases From a Human Factors and Cognitive Psychology Perspective. Annals of Surgery. 2003;237:460–469. doi: 10.1097/01.SLA.0000060680.92690.E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolf JJS, et al. Hand assisted laparoscopic nephrectomy: comparison to standard laparoscopic nephrectomy. The Journal of Urology. 1998;160:22–27. [PubMed] [Google Scholar]
- 12.Miller N, Theodorescu D. Status of robotic cystectomy in 2005. World Journal of Urology. 2006;24:180–187. doi: 10.1007/s00345-006-0066-2. [DOI] [PubMed] [Google Scholar]
- 13.Gallagher AG, Satava RM. Virtual reality as a metric for the assessment of laparoscopic psychomotor skills. Surgical Endoscopy. 2002;16:1746–1752. doi: 10.1007/s00464-001-8215-6. [DOI] [PubMed] [Google Scholar]
- 14.Zhou M, et al. Force perception threshold varies with experience in minimally invasive surgery. in ISIC 2007, IEEE International Conference on.Systems, Man and Cybernetics. 2007:2228–2232. [Google Scholar]
- 15.Rassweiler J, et al. Mechanical Simulators for Training for Laparoscopic Surgery in Urology. Journal of Endourology. 2007;21:252–262. doi: 10.1089/end.2007.9983. [DOI] [PubMed] [Google Scholar]
- 16.Källström R, et al. Impact of virtual reality-simulated training on urology residents' performance of transurethral resection of the prostate. Journal of Endourology. 2010;24:1521–1528. doi: 10.1089/end.2009.0667. [DOI] [PubMed] [Google Scholar]
- 17.Nisky I, et al. A Regression and Boundary-Crossing-Based Model for the Perception of Delayed Stiffness. IEEE Transactions on Haptics. 2008;1:73–82. doi: 10.1109/TOH.2008.17. [DOI] [PubMed] [Google Scholar]
- 18.Nisky I, et al. Proximodistal gradient in the perception of delayed stiffness. Journal of Neurophysiology. 2010;103:3017–3026. doi: 10.1152/jn.00939.2009. [DOI] [PubMed] [Google Scholar]
- 19.Wichmann FA, Hill NJ. The psychometric function: I. Fitting, sampling, and goodness of fit. Perception & Psychophysics. 2001;63:1293–1313. doi: 10.3758/bf03194544. [DOI] [PubMed] [Google Scholar]