Abstract
A meta-review, or review of systematic reviews, was conducted to explore the risks of all-cause and suicide mortality in major mental disorders. A systematic search generated 407 relevant reviews, of which 20 reported mortality risks in 20 different mental disorders and included over 1.7 million patients and over a quarter of a million deaths. All disorders had an increased risk of all-cause mortality compared with the general population, and many had mortality risks larger than or comparable to heavy smoking. Those with the highest all-cause mortality ratios were substance use disorders and anorexia nervosa. These higher mortality risks translate into substantial (10-20 years) reductions in life expectancy. Borderline personality disorder, anorexia nervosa, depression and bipolar disorder had the highest suicide risks. Notable gaps were identified in the review literature, and the quality of the included reviews was typically low. The excess risks of mortality and suicide in all mental disorders justify a higher priority for the research, prevention, and treatment of the determinants of premature death in psychiatric patients.
Keywords: Mortality, suicide, mental disorders, substance use disorders, anorexia nervosa, meta-review
Higher mortality risks in many mental disorders are well recognized and may be worsening over time 1,2. Data from the Global Burden of Disease (GBD) study suggested that mental and behavioural disorders account for 8.6 million, or 0.5%, of all years of life lost to premature mortality 3. This is equivalent to 232,000 deaths in 2010, an increase from 1990, when there were 138,000 premature deaths secondary to mental disorders 4. More than three-quarters of these deaths were attributed to substance use disorders. However, substance use and mental illness are commonly comorbid and mutually amplify the risk to premature death, often by suicide.
The GBD study also reported that suicide was the 13th leading cause of death globally, and was more prevalent in regions with advanced health care systems 4. Suicide accounted for 5% of female and 6% of male deaths in persons aged 15-49 years old, and 884,000 deaths across all ages.
These stark mortality figures highlight an obvious challenge to preventive medicine, because mental disorders and substance use have evidence-based treatments. Delivering such treatments effectively should reduce the risks of premature death for individual patients, particularly from suicide.
Clarifying the pattern of risks across mental disorders is a necessary step to identify where resources can be most effectively targeted and interventions prioritized. However, syntheses of mortality risks associated with different diagnoses have not been attempted since the 1998 publication of the highly influential meta-analysis by Harris and Barraclough 5. This is despite the exponential growth in the literature over recent decades and contrasting estimates in subsequent studies for mortality in individual conditions. For example, a 2007 systematic review 1 suggested that the standardized mortality ratio (SMR) for patients with schizophrenia is 2.5, while Harris and Barraclough's estimate was 1.6. Another recent review 6 provided an SMR for opioid use of 14.7, more than twice that reported in the Harris and Barraclough review (6.4). In addition, there is now a much greater awareness of the contribution of treatable physical ill health to premature death in psychiatric patients. An understanding of the comparative data for exposure to known physical risk factors, like tobacco smoking, is also currently lacking.
With the increase in evidence over recent decades and contrasting estimates in meta-analyses, an updated review is required. This will enable clinicians to prioritize interventions based on the comparative risks of mortality across disorders, researchers to identify where gaps exist in the literature, and commissioners and policy makers to target resources more effectively. We have therefore conducted a meta-review, or a review of systematic reviews, of all-cause and suicide mortality in all major mental disorders.
METHODS
Using the Google Scholar database, a systematic search was conducted to identify systematic reviews and meta-analyses that reported on risks for all-cause and suicide mortality for unipolar depressive disorders, anxiety disorders, bipolar disorder, schizophrenia spectrum disorders, eating disorders, learning disability and autistic spectrum disorders, childhood behavioural disorders (including conduct disorder and oppositional defiant disorder), personality disorders, dementia, substance use disorders, alcohol use disorder and smoking.
We used the following search terms: ‘allintitle: mortality OR death OR suicide OR suicidal OR suicidality, review OR meta-analysis OR meta-analytic, psychiatry OR psychiatric OR mental OR mood OR affective OR depression OR depressive OR dysthymia OR cyclothymia OR adjustment OR anxiety OR anxious OR “obsessive compulsive” OR OCD OR panic OR “post-traumatic” OR posttraumatic OR PTSD OR neurosis OR neuroses OR bipolar OR manic OR schizophrenia OR psychotic OR psychosis OR psychoses OR dementia OR demented OR Alzheimer OR “learning disability” OR “learning disabilities” OR IQ OR “mental retardation” OR autism OR autistic OR Asperger OR “attention deficit” OR ADHD OR hyperactivity OR hyperkinetic OR conduct OR disruptive OR personality OR personalities OR borderline OR antisocial OR psychopathic OR dissocial OR forensic OR narcissistic OR schizoid OR schizotypal OR paranoid OR dependent OR avoidant OR “emotionally unstable” OR eating OR anorexia OR bulimia OR EDNOS OR heroin OR opioid OR opioids OR cocaine OR cannabis OR marijuana OR alcohol OR alcoholism OR benzodiazepine OR benzodiazepines OR hypnotic OR hypnotics OR amphetamine OR amphetamines OR barbiturate OR barbiturates OR smoking OR smokers OR cigarette OR cigarettes'. We targeted articles published between January 1, 1998 and February 19, 2014.
Papers were excluded if they did not report a pooled all-cause mortality or completed suicide statistic. Gender-specific estimates were reported if available. If a review was superseded by a more recently published review, only the more recent paper was included. For diagnoses where no pooled mortality statistic was found, we identified the most recent large (N>1000) single study providing data on mortality by conducting further database and citation searches.
A second search was carried out to identify systematic reviews and studies on life expectancy in mental disorders. Using the Google Scholar database, the following search terms were used: ‘allintitle: review, life expectancy' and ‘allintitle: life expectancy, mental OR psychiatric OR psychiatry OR mood OR depression OR bipolar OR schizophrenia OR personality OR anxiety OR smoking OR substance OR opioid OR alcohol OR anorexia OR eating'. We targeted articles published between January 1, 1998 and February 19, 2014. Supplementary citation searches were used to identify additional studies.
The majority of reviews reported SMRs. An SMR compares the gender and age standardized mortality of a sample (i.e., people with a mental disorder) to the whole population. Some studies instead reported relative risks (RRs) or odds ratios (ORs). A RR is defined by the incidence in the exposed divided by the incidence in the unexposed. The OR is defined by odds of an event (i.e., death or suicide) in the exposed divided by the odds of such an event in the unexposed 7. The OR and RR tend to report a larger effect than SMR, because the denominator in the SMR includes those with mental illness (whereas these individuals are excluded in the denominator for an OR or RR). Typically, the OR is similar to the RR when events are rare, as is the case for death and suicide 8.
One of the authors (EC) extracted mortality statistics with their 95% confidence intervals. Another researcher re-assessed the data extraction – no discrepancies were identified. If reported, RRs/ORs adjusted by age and gender were included. We chose random effects estimates if reported, as heterogeneity in individual reviews was high.
Each review was rated using the Assessing the Methodological Quality of Systematic Reviews (AMSTAR) 9, an empirically developed scoring system to assess the quality of systematic reviews, made up of the following eleven criteria scored from 0 to 1: Was an “a priori” design provided? Was there duplicate study selection and data extraction? Was a comprehensive literature search performed? Was the status of publication (i.e., grey literature) used as an inclusion criterion? Was a list of studies (included and excluded) provided? Were the characteristics of the included studies provided? Was the scientific quality of the included studies assessed and documented? Was the scientific quality of the included studies used appropriately in formulating conclusions? Were the methods used to combine the findings of studies appropriate? Was the likelihood of publication bias assessed? Was the conflict of interest stated? Scores of 0 to 3 are considered low, 4 to 7 medium, and 8 to 11 high 10.
We excluded a review of mortality in benzodiazepine use 11 as it only provided risk data for prescribed use, not misuse. In addition, a review of suicide in bipolar disorder 12 was excluded as it did not provide a pooled mortality statistic. Finally, a review of suicide in attention-deficit/hyperactivity disorder (ADHD) 13 was excluded as it did not use comparative population data.
RESULTS
The search for reviews on all-cause mortality identified 406 citations, and additional citation searches identified one review. After removing duplicates, and screening titles and abstracts, 96 reviews were identified. After exclusions, a final sample of 20 systematic reviews and meta-analyses 1,6,14–31 were included (Figure 1, Table 1). Excluding the smoking review, these reviews included over 1.7 million individuals with mental disorders and investigated over a quarter of a million deaths. We identified a further 12 mortality estimates from the largest single studies for disorders where there were no systematic reviews 32–42 (Table 2).
Figure 1.
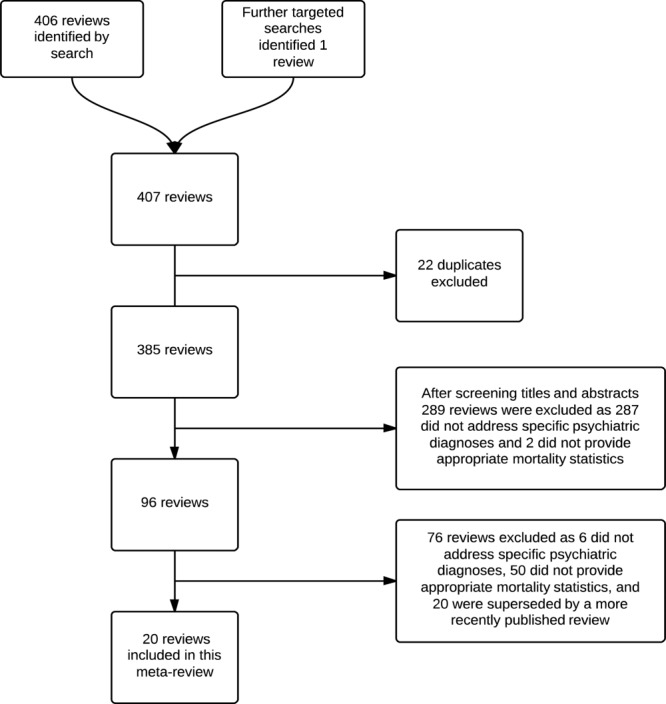
Flow chart of systematic search strategy
Table 1.
All-cause and suicide mortality in mental disorders
| Diagnosis | All-cause mortality risk estimate (95% CI) | Statistic | Men (95% CI) | Women (95% CI) | Suicide risk estimate (95% CI) | Statistic | Men (95% CI) | Women (95% CI) | AMSTAR score |
|---|---|---|---|---|---|---|---|---|---|
| Opioid use 6,14 | 14.7 (12.8-16.5) | SMR | 13.5 (10.5-17.2) | SMR | 7.6 (4.4-12.1) | 3.6 (0.1-19.9) | 7, 1 | ||
| Amphetamine use 15 | 6.2 (4.6-8.3) | SMR* | 5.9 (4.1-8.1) | 7.8 (3.9-14.0) | 8 | ||||
| Cocaine use 16 | 4 to 8 | SMRs | 7 | ||||||
| Anorexia nervosa 17,18 | 5.9 (4.2-8.3) | SMR | SMR* | 31.0 (21.0-44.0) | 2, 3 | ||||
| Alcohol use disorder 19,20 | 4.6 (2.7-7.7) | RR | 3.4 (3.0-3.8) | 4.6 (3.9-5.4) | SMR | 8.8 (6.4-12.1) | 16.4 (10.7-25.2) | 5, 5 | |
| Autism spectrum disorder 21 | 2.8 (1.8-4.2) | SMR | 2.1 (1.7-2.7) | 7.2 (3.0-17.2) | 7 | ||||
| Heavy smoking22 | RR - WA | 2.4 | 2.7 | 2 | |||||
| Schizophrenia 1 | 2.5 (2.2-2.4) | SMR | 3.0 | 2.4 | 12.9 (0.7-174.3)** | SMR* | 6 | ||
| Dementia 23 | 1.5 to 3.0 | RRs | 5 | ||||||
| Moderate smoking 22,24 | RR -WA | 2.0 | 2.0 | 1.8 (1.5-2.2) | RR | 1.7 (1.4-2.1) | 1.8 (1.2-2.7) | 2, 6 | |
| Bulimia nervosa 17,18 | 1.9 (1.4-2.6) | SMR | SMR* | 7.5 (1.6-11.6) | 2, 3 | ||||
| Eating disorder NOS 17 | 1.9 (1.5-2.5) | SMR | 2 | ||||||
| Depression 25,26 | 1.6 (1.6-1.7) | RR | 19.7 (12.2-32.0) | SMR | 7, 3 | ||||
| Depression in the elderly 27 | 1.6 (1.4-1.8) | RR | 4 | ||||||
| Dysthymic disorder 27 | 1.4 (0.9-2.0) | RR | 4 | ||||||
| Cannabis use 28 | RRs | 1.2 to 1.3 | 1.1 (0.8-1.5) | 4 | |||||
| Borderline personality disorder 29 | 45.1 (29.0-61.3) | SMR* | 1 | ||||||
| Bipolar disorder 26 | 17.1 (9.8-29.5) | SMR | 3 | ||||||
| Personality disorders 30 | RR | 4.1 (3.0-5.8) | 1.8 (0.7-5.2) | 3 | |||||
| Anxiety disorder (any type) 31 | 3.3 (2.1-5.3) | OR | 7 | ||||||
| Post-traumatic stress disorder 31 | 2.5 (0.5-13.4) | OR | 7 |
SMR – standardized mortality ratio, OR – odds ratio, RR – relative risk, WA – weighted average, AMSTAR – Assessing the Methodological Quality of Systematic Reviews, NOS – not otherwise specified
Not adjusted for random effects
90% confidence intervals
Table 2.
Single studies providing data on mortality risks in disorders where systematic reviews were not identified
| Diagnosis | Statistic | All-cause mortality risk estimate (95% CI) | Men | Women |
|---|---|---|---|---|
| Early-onset dementia 32 | HR | 43.3 (3.1-600.4) | ||
| Post-partum psychiatric admission (at 1 year) 33 | SMR | 19.5 (11.7-30.4) | ||
| Disruptive behaviour disorder* 34 | SMR | 5.8 (4.1-8.0) | 4.1 (1.3-9.4) | |
| Methamphetamine use 35 | SMR | 4.7 (4.5-4.8) | 4.9 (4.7-5.0) | 4.4 (4.1-4.6) |
| Acute and transient psychotic disorder 36 | SMR | 4.7 (4.1-5.3) | 4.9 (4.2-5.8) | 4.4 (3.6-5.4) |
| Personality disorder 37 | SMR | 4.2 (3.0-5.6) | 3.5 (2.2-5.5) | 5.0 (3.2-7.5) |
| Late-onset dementia 32 | aHR | 3.3 (1.8-6.2) | ||
| Schizophrenia in the elderly 38 | SMR | 2.7 (2.6-2.8) | 3.0 (2.9-3.1) | 2.6 (2.5-2.6) |
| Intellectual disability (moderate to profound) 39 | SMR | 2.8 (2.5-3.0) | 2.3 (2.0-2.6) | 3.2 (2.8-3.7) |
| Bipolar disorder 40 | aHR | 2.0 (1.9-2.2) | 2.3 (2.2-2.5) | |
| Adults with childhood ADHD 41 | SMR | 1.9 (0.8-4.3) | ||
| Comorbid anxiety/depression 42 | OR | 1.4 (1.2-1.7) | 1.4 (1.1-1.8) | 1.5 (1.2-1.8) |
SMR – standardized mortality ratio, HR – hazard ratio, aHR – adjusted hazard ratio, OR – odds ratio, ADHD – attention-deficit/hyperactivity disorder
Mainly consists of conduct disorder and oppositional defiant disorder
The search for reviews on life expectancy yielded 28 papers, none of which was relevant. The second search, for single studies, identified 123 relevant papers, of which 8 were included. Further citation searches, and the results from the above all-cause and suicide mortality search, identified one further systematic review and five relevant primary studies. Therefore, we identified 14 relevant publications 37,40,43–54 (Table 3).
Table 3.
Single studies and reviews reporting life expectancy in mental disorders
| Diagnosis | Years lost | Men (95% CI) | Women (95% CI) | Population |
|---|---|---|---|---|
| Depressive episode/recurrent depressive disorder 43 | 10.6 (9.5-12.8) | 7.2 (6.3-8.1) | UK | |
| Affective disorders 44 | 15.6 to 17.4 | 11.1 to 13.6 | Denmark, Finland and Sweden | |
| Bipolar disorder 43 | 10.1 (8.9-11.3) | 11.2 (10.2-12.1) | UK | |
| Bipolar disorder 45 | 13.6 (13.2-14.0) | 12.1 (11.8-12.4) | Denmark | |
| Bipolar disorder 46 | 9.0 | 9.0 | Israel | |
| Bipolar disorder 40 | 8.5 | 9.0 | Sweden | |
| Bipolar disorder 47 | 12.7 to 19.8 | 11.0 to 16.2 | Denmark, Finland and Sweden | |
| Schizoaffective disorder 43 | 8.0 (6.9-9.1) | 17.5 (14.4-20.7) | UK | |
| Schizophrenia spectrum 44 | 15.5 to 20.1 | 10.9 to 17.3 | Denmark, Finland and Sweden | |
| Schizophrenia 43 | 14.6 (12.3-15.8) | 9.8 (8.9-10.7) | UK | |
| Schizophrenia 45 | 18.7 (18.4-19.0) | 16.3 (16.2-16.8) | Denmark | |
| Schizophrenia 46 | 11.0 | 13.0 | Israel | |
| Schizophrenia 48 | 14.7 | 15.3 | 11.4 | Denmark |
| Schizophrenia 47 | 17.1 to 20.0 | 15.6 to 16.9 | Denmark, Finland and Sweden | |
| Schizophrenia 49 | 15.0 | 12.0 | Sweden | |
| Personality disorders 44 | 13.0 to 21.9 | 14.5 to 20.0 | Denmark, Finland and Sweden | |
| Personality disorders 37 | 17.7 (15.9-19.5) | 18.7 (17.3-20.1) | UK | |
| Younger onset dementia 50 | 9.6 to 19.4 | Review (1985-2010) | ||
| Late onset dementia 50 | 1.3 to 9.2 | Review (1985-2010) | ||
| Alzheimer's dementia 50 | 0.9 to 16.7 | Review (1985-2010) | ||
| Fronto-temporal dementia 50 | 11.5 to 15.4 | Review (1985-2010) | ||
| Dementia 50 | 0.4 to 11.4 | 1.4 to 15.3 | Review (1985-2010) | |
| Alcohol use 51 | 17.1 (15.4-18.8) | 10.8 (9.6-12.1) | UK | |
| Opioid use 51 | 9.0 (7.8-10.2) | 17.3 (15.4-19.2) | UK | |
| Substance use disorders 43 | 13.6 (12.5-14.8) | 14.8 (13.4-16.2) | UK | |
| Substance abuse 44 | 21.3 to 23.6 | 17.6 to 22.6 | Denmark, Finland and Sweden | |
| Heavy smoking 52 | 9.2 | 9.4 | Denmark | |
| Smoking 53 | 8.0 | 10.0 | Japan | |
| Smoking54 | 8.7 (7.6-9.6) | 7.6 (6.3-8.9) | USA |
All mental disorders had higher mortality risks than general population samples, but there was a considerable range from dysthymia, with an RR of 1.4, to opiate use disorders, with an SMR of 14.7. Substance use disorders and anorexia nervosa had the highest mortality risks (Table 1). For schizophrenia and autism, mortality risks were at least as high as heavy smoking (Table 4).
Table 4.
Mortality risk in specific mental disorders compared to heavy smoking
| Diagnosis | All-cause mortality (risk compared with the general population) | Prevalence ratio (risk compared with that for heavy smoking) |
|---|---|---|
| Post-partum psychiatric admission (at 1 year) 33 | 19.5 | 7.7 |
| Opioid use 6 | 14.7 | 5.8 |
| Amphetamine use 15 | 6.2 | 2.4 |
| Cocaine use 16 | 6.0** | 2.4 |
| Anorexia nervosa 17 | 5.9 | 2.3 |
| Disruptive behaviour disorder* 34 | 5.0*** | 1.9 |
| Methamphetamine use 35 | 4.7 | 1.8 |
| Acute and transient psychotic disorder 36 | 4.7 | 1.8 |
| Alcohol use disorder 19 | 4.6 | 1.8 |
| Personality disorder 37 | 4.2 | 1.7 |
| Intellectual disability (moderate to profound) 39 | 2.8 | 1.1 |
| Heavy smoking22 | 2.6*** | 1.0 |
| Schizophrenia 1 | 2.5 | 1.0 |
| Bipolar disorder 40 | 2.2** | 0.8 |
| Bulimia nervosa 17 | 1.9 | 0.8 |
| Eating disorder NOS 17 | 1.9 | 0.8 |
| Adults with childhood ADHD 41 | 1.9 | 0.8 |
| Depression 25 | 1.6 | 0.6 |
| Dysthymic disorder 27 | 1.4 | 0.6 |
| Comorbid anxiety/depression 42 | 1.4 | 0.6 |
| Cannabis use 28 | 1.2**,*** | 0.5 |
ADHD – attention-deficit/hyperactivity disorder, NOS – not otherwise specified
Mainly consists of conduct disorder and oppositional defiant disorder
mid-point of range
mean value of male and female mortality
The pattern of suicide estimates was different from all-cause mortality (Table 1). Borderline personality disorder, depression, bipolar disorder, opioid use and schizophrenia, as well as anorexia nervosa and alcohol use disorder in women, had higher suicide risks than most other disorders. A sample of anorexic patients presenting to specialist care (outpatients and inpatients) was an outlier for suicide (SMR=31.0, 95% CI: 21.0-44.0) 18. As a review on suicide in borderline personality disorder 29 did not provide a pooled mortality statistic, we combined data to provide a median SMR (SMR=45.1, 95% CI: 29.0-61.3). Again, these patients were mostly hospitalized and thus represent the severe end of the diagnostic spectrum.
Two reviews 23,27 reported data on all-cause mortality relevant to older adults. Increases were seen in depression (RR=1.6, 95% CI: 1.4-1.8), and dementia (RRs of 1.5 to 3.0). These are not dissimilar to risks of death for elderly smokers (RR=1.8, 95% CI: 1.7-2.0) 55.
The reduction in life expectancy associated with moderate to heavy smoking ranged from 8 to 10 years. This range is similar to that reported for a single depressive episode or recurrent depressive disorder (7-11 years), but lower than that associated with substance use (9-24 years), personality disorders (13-22 years), schizophrenia (10-20 years), and bipolar disorder (9-20 years) (Table 3).
We did not identify any reviews on all-cause mortality for some major diagnostic classes, including bipolar disorder, anxiety disorders, personality disorders, ADHD, obsessive-compulsive disorder and post-traumatic stress disorder. For suicide, we did not identify systematic reviews for cocaine and amphetamine use, autism, dementia and ADHD. In addition, we identified no reviews of mortality in people with dual diagnosis.
DISCUSSION
To our knowledge, this is the first meta-review of all-cause mortality and suicide risks in mental disorders. We identified 20 systematic reviews and meta-analyses that reported such risks in over 1.7 million individuals with mental disorders and over a quarter of a million deaths. We located a further 14 publications on life expectancy.
We found that all the reported mental disorders had elevated all-cause mortality risks compared with the general population. Several disorders had higher or equal mortality risks compared to heavy smoking. However, there was considerable variation between diagnoses, for both mortality and completed suicide. Substance use disorders and anorexia nervosa had the highest mortality ratios. The mortality data for schizophrenia (SMR=2.5) and bipolar disorder (adjusted hazard ratio=2.0-2.3) were comparable with that for heavy smoking (RR=2.4-2.7). This result was underscored by the data for life expectancy, where all major mental disorder diagnoses had reductions (7-24 years) similar to, or greater than, heavy smoking (8-10 years).
For suicide mortality, borderline personality disorder, depression, bipolar disorder, opioid use and schizophrenia, as well as anorexia nervosa and alcohol use disorder in women, had substantially increased rates (greater then 10 times) compared with the general population. There was also an increased risk for suicide in moderate smokers, but this was lower than the mental disorder diagnoses investigated.
A limitation of this meta-review is the varied quality of the reviews (7 out of 20 had a low AMSTAR quality rating score, a further 12 had a medium score, and only one review could be considered of a high quality). Common omissions in the reviews were lack of testing for publication bias, not searching grey literature, and not having two data extractors. An additional limitation is the underreporting of suicide statistics which is common in some countries 56 and the potential contribution of psychiatric comorbidity to mortality.
Few reviews specified or commented on the samples included in their meta-analyses. The common use of solely inpatient data may overestimate risks for disorders mild enough to be managed in primary care 57. This may not be the case for schizophrenia, in which mortality was compared between inpatient and outpatient populations and no difference was found 1. Furthermore, the review on depression 25 had similar mortality risks for all patients compared with depressed persons identified solely using community based data. The reviews on dysthymia and depression in the elderly 27 and dementia 23 also used community and outpatient clinic data only. On the other hand, the review on amphetamine use only reported one SMR, which was taken from an inpatient sample 15. Furthermore, the two outliers for suicide risk – anorexia nervosa 18 and borderline personality disorder 29 – were taken from samples with high proportions of inpatients, and thus represent the most severe cases of these disorders.
Most of the primary studies making up the reviews made use of large administrative data sets. As recently highlighted by Ioannidis 58, these data sets have their weaknesses, despite the precision associated with their large sample sizes. Analyses using such data are typically overpowered, so that statistically significant results can be obtained despite very small differences in mortality. As a result, it is not only the statistical significance that is important, but the size of the difference in mortality risk needs to be considered and balanced against the relative risk. Further, data were not collected for research purposes and hence diagnoses may be subject to substantial noise. Sensitivity analysis should be undertaken to examine diagnoses that have been made in different ways and also the degree of miscoding. Lack of, and error in the measurement of covariates may lead to inadequate adjustment, as can differences in the coding and treatment between hospitals and other health care settings 23.
Smoking has been an important target for prevention because it is so common and perceived to be so dangerous. Mental disorders are also relatively common when considered together, but the risk to life is not perceived in the same way. From a public health perspective, patients with serious mental illness should be designated as a high risk population for physical illness, given the substantial health disparities compared with the general population. National strategies could and should target improving access to physical health care 59.
In conclusion, the impact on mortality and suicide of mental disorders is substantial, and probably poorly appreciated as a public health problem. The scale of the unmet needs complements the social burden and costs of mental disorders 60. These findings must justify a higher priority for research, prevention and treatment of the determinants of premature death in psychiatric patients.
Acknowledgments
The authors are grateful to L. Hart for being the second data extractor. S. Fazel is funded by the Wellcome Trust [095806].
References
- 1.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64:1123–31. doi: 10.1001/archpsyc.64.10.1123. [DOI] [PubMed] [Google Scholar]
- 2.Hoang U, Stewart R, Goldacre MJ. Mortality after hospital discharge for people with schizophrenia or bipolar disorder: retrospective study of linked English hospital episode statistics, 1999-2006. BMJ. 2011;343:d5422. doi: 10.1136/bmj.d5422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–86. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 4.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry. 1998;173:11–53. doi: 10.1192/bjp.173.1.11. [DOI] [PubMed] [Google Scholar]
- 6.Degenhardt L, Bucello C, Mathers B, et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies. Addiction. 2011;106:32–51. doi: 10.1111/j.1360-0443.2010.03140.x. [DOI] [PubMed] [Google Scholar]
- 7.Bland JM, Altman DG. Statistics notes. The odds ratio. BMJ. 2000;320:1468. doi: 10.1136/bmj.320.7247.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viera AJ. Odds ratios and risk ratios: what's the difference and why does it matter? South Med J. 2008;101:730–4. doi: 10.1097/SMJ.0b013e31817a7ee4. [DOI] [PubMed] [Google Scholar]
- 9.Shea BJ, Hamel C, Wells GA, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62:1013–20. doi: 10.1016/j.jclinepi.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 10.Amato L, Minozzi S, Davoli M. Efficacy and safety of pharmacological interventions for the treatment of the Alcohol Withdrawal Syndrome. Cochrane Database Syst Rev. 2011;6:CD008537. doi: 10.1002/14651858.CD008537.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Charlson F, Degenhardt L, McLaren J, et al. A systematic review of research examining benzodiazepine-related mortality. Pharmacoepidemiol Drug Saf. 2009;18:93–103. doi: 10.1002/pds.1694. [DOI] [PubMed] [Google Scholar]
- 12.Pompili M, Gonda X, Serafini G, et al. Epidemiology of suicide in bipolar disorders: a systematic review of the literature. Bipolar Disord. 2013;15:457–90. doi: 10.1111/bdi.12087. [DOI] [PubMed] [Google Scholar]
- 13.James A, Lai FH, Dahl C. Attention deficit hyperactivity disorder and suicide: a review of possible associations. Acta Psychiatr Scand. 2004;110:408–15. doi: 10.1111/j.1600-0447.2004.00384.x. [DOI] [PubMed] [Google Scholar]
- 14.Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;76:S11–9. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Singleton J, Degenhardt L, Hall W, et al. Mortality among amphetamine users: a systematic review of cohort studies. Drug Alcohol Depend. 2009;105:1–8. doi: 10.1016/j.drugalcdep.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 16.Degenhardt L, Singleton J, Calabria B, et al. Mortality among cocaine users: a systematic review of cohort studies. Drug Alcohol Depend. 2011;113:88–95. doi: 10.1016/j.drugalcdep.2010.07.026. [DOI] [PubMed] [Google Scholar]
- 17.Arcelus J, Mitchell AJ, Wales J, et al. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68:724–31. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- 18.Preti A, Rocchi MB, Sisti D, et al. A comprehensive meta-analysis of the risk of suicide in eating disorders. Acta Psychiatr Scand. 2011;124:6–17. doi: 10.1111/j.1600-0447.2010.01641.x. [DOI] [PubMed] [Google Scholar]
- 19.Roerecke M, Rehm J. Alcohol use disorders and mortality: a systematic review and meta-analysis. Addiction. 2013;108:1562–78. doi: 10.1111/add.12231. [DOI] [PubMed] [Google Scholar]
- 20.Roerecke M, Rehm J. Cause-specific mortality risk in alcohol use disorder treatment patients: a systematic review and meta-analysis. Int J Epidemiol. doi: 10.1093/ije/dyu018. (in press) [DOI] [PubMed] [Google Scholar]
- 21.Woolfenden S, Sarkozy V, Ridley G, et al. A systematic review of two outcomes in autism spectrum disorder – epilepsy and mortality. Dev Med Child Neurol. 2012;54:306–12. doi: 10.1111/j.1469-8749.2012.04223.x. [DOI] [PubMed] [Google Scholar]
- 22.Shavelle RM, Paculdo DR, Strauss DJ, et al. Smoking habit and mortality: a meta-analysis. J Insur Med. 2008;40:170–8. [PubMed] [Google Scholar]
- 23.Todd S, Barr S, Roberts M, et al. Survival in dementia and predictors of mortality: a review. Int J Geriatr Psychiatry. 2013;28:1109–24. doi: 10.1002/gps.3946. [DOI] [PubMed] [Google Scholar]
- 24.Li D, Yang X, Ge Z, et al. Cigarette smoking and risk of completed suicide: a meta-analysis of prospective cohort studies. J Psychiatr Res. 2012;46:1257–66. doi: 10.1016/j.jpsychires.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 25.Cuijpers P, Vogelzangs N, Twisk J, et al. Comprehensive meta-analysis of excess mortality in depression in the general community versus patients with specific illnesses. Am J Psychiatry. doi: 10.1176/appi.ajp.2013.13030325. (in press) [DOI] [PubMed] [Google Scholar]
- 26.Neeleman J. A continuum of premature death. Meta-analysis of competing mortality in the psychosocially vulnerable. Int J Epidemiol. 2001;30:154–62. doi: 10.1093/ije/30.1.154. [DOI] [PubMed] [Google Scholar]
- 27.Baxter AJ, Page A, Whiteford HA. Factors influencing risk of premature mortality in community cases of depression: a meta-analytic review. Epidemiol Res Int. 2011;2011:1–12. [Google Scholar]
- 28.Calabria B, Degenhardt L, Hall W, et al. Does cannabis use increase the risk of death? Systematic review of epidemiological evidence on adverse effects of cannabis use. Drug Alcohol Rev. 2010;29:318–30. doi: 10.1111/j.1465-3362.2009.00149.x. [DOI] [PubMed] [Google Scholar]
- 29.Pompili M, Girardi P, Ruberto A, et al. Suicide in borderline personality disorder: a meta-analysis. Nord J Psychiatry. 2005;59:319–24. doi: 10.1080/08039480500320025. [DOI] [PubMed] [Google Scholar]
- 30.Li Z, Page A, Martin G, et al. Attributable risk of psychiatric and socio-economic factors for suicide from individual-level, population-based studies: a systematic review. Soc Sci Med. 2011;72:608–16. doi: 10.1016/j.socscimed.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 31.Kanwar A, Malik S, Prokop LJ, et al. The association between anxiety disorders and suicidal behaviors: a systematic review and meta-analysis. Depress Anxiety. 2013;30:917–29. doi: 10.1002/da.22074. [DOI] [PubMed] [Google Scholar]
- 32.Koedam EL, Pijnenburg YA, Deeg DJ, et al. Early-onset dementia is associated with higher mortality. Dement Geriatr Cogn Disord. 2008;26:147–52. doi: 10.1159/000149585. [DOI] [PubMed] [Google Scholar]
- 33.Appleby L, Mortensen PB, Faragher EB. Suicide and other causes of mortality after post-partum psychiatric admission. Br J Psychiatry. 1998;173:209–11. doi: 10.1192/bjp.173.3.209. [DOI] [PubMed] [Google Scholar]
- 34.Kjelsberg E. Adolescent psychiatric in-patients. A high-risk group for premature death. Br J Psychiatry. 2000;176:121–5. doi: 10.1192/bjp.176.2.121. [DOI] [PubMed] [Google Scholar]
- 35.Callaghan RC, Cunningham JK, Verdichevski M, et al. All-cause mortality among individuals with disorders related to the use of methamphetamine: a comparative cohort study. Drug Alcohol Depend. 2012;125:290–4. doi: 10.1016/j.drugalcdep.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 36.Castagnini A, Foldager L, Bertelsen A. Excess mortality of acute and transient psychotic disorders: comparison with bipolar affective disorder and schizophrenia. Acta Psychiatr Scand. 2013;128:370–5. doi: 10.1111/acps.12077. [DOI] [PubMed] [Google Scholar]
- 37.Fok ML, Hayes RD, Chang CK, et al. Life expectancy at birth and all-cause mortality among people with personality disorder. J Psychosom Res. 2012;73:104–7. doi: 10.1016/j.jpsychores.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 38.Talaslahti T, Alanen HM, Hakko H, et al. Mortality and causes of death in older patients with schizophrenia. Int J Geriatr Psychiatry. 2012;27:1131–7. doi: 10.1002/gps.2833. [DOI] [PubMed] [Google Scholar]
- 39.Tyrer F, McGrother C. Cause-specific mortality and death certificate reporting in adults with moderate to profound intellectual disability. J Intellect Disabil Res. 2009;53:898–904. doi: 10.1111/j.1365-2788.2009.01201.x. [DOI] [PubMed] [Google Scholar]
- 40.Crump C, Sundquist K, Winkleby MA, et al. Comorbidities and mortality in bipolar disorder: a Swedish national cohort study. JAMA Psychiatry. 2013;70:931–9. doi: 10.1001/jamapsychiatry.2013.1394. [DOI] [PubMed] [Google Scholar]
- 41.Barbaresi WJ, Colligan RC, Weaver AL, et al. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131:637–44. doi: 10.1542/peds.2012-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mykletun A, Bjerkeset O, Overland S, et al. Levels of anxiety and depression as predictors of mortality: the HUNT study. Br J Psychiatry. 2009;195:118–25. doi: 10.1192/bjp.bp.108.054866. [DOI] [PubMed] [Google Scholar]
- 43.Chang CK, Hayes RD, Perera G, et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS One. 2011;6:e19590. doi: 10.1371/journal.pone.0019590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nordentoft M, Wahlbeck K, Hallgren J, et al. Excess mortality, causes of death and life expectancy in 270,770 patients with recent onset of mental disorders in Denmark, Finland and Sweden. PLoS One. 2013;8:e55176. doi: 10.1371/journal.pone.0055176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Laursen TM. Life expectancy among persons with schizophrenia or bipolar affective disorder. Schizophr Res. 2011;131:101–4. doi: 10.1016/j.schres.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 46.Kodesh A, Goldshtein I, Gelkopf M, et al. Epidemiology and comorbidity of severe mental illnesses in the community: findings from a computerized mental health registry in a large Israeli health organization. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1775–82. doi: 10.1007/s00127-012-0478-9. [DOI] [PubMed] [Google Scholar]
- 47.Laursen TM, Wahlbeck K, Hallgren J, et al. Life expectancy and death by diseases of the circulatory system in patients with bipolar disorder or schizophrenia in the Nordic countries. PLoS One. 2013;8:e67133. doi: 10.1371/journal.pone.0067133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nielsen RE, Uggerby AS, Jensen SO, et al. Increasing mortality gap for patients diagnosed with schizophrenia over the last three decades – a Danish nationwide study from 1980 to 2010. Schizophr Res. 2013;146:22–7. doi: 10.1016/j.schres.2013.02.025. [DOI] [PubMed] [Google Scholar]
- 49.Crump C, Winkleby MA, Sundquist K, et al. Comorbidities and mortality in persons with schizophrenia: a Swedish national cohort study. Am J Psychiatry. 2013;170:324–33. doi: 10.1176/appi.ajp.2012.12050599. [DOI] [PubMed] [Google Scholar]
- 50.Brodaty H, Seeher K, Gibson L. Dementia time to death: a systematic literature review on survival time and years of life lost in people with dementia. Int Psychogeriatr. 2012;24:1034–45. doi: 10.1017/S1041610211002924. [DOI] [PubMed] [Google Scholar]
- 51.Hayes RD, Chang CK, Fernandes A, et al. Associations between substance use disorder sub-groups, life expectancy and all-cause mortality in a large British specialist mental healthcare service. Drug Alcohol Depend. 2011;118:56–61. doi: 10.1016/j.drugalcdep.2011.02.021. [DOI] [PubMed] [Google Scholar]
- 52.Prescott E, Osler M, Hein HO, et al. Life expectancy in Danish women and men related to smoking habits: smoking may affect women more. J Epidemiol Community Health. 1998;52:131–2. doi: 10.1136/jech.52.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sakata R, McGale P, Grant EJ, et al. Impact of smoking on mortality and life expectancy in Japanese smokers: a prospective cohort study. BMJ. 2012;345:e7093. doi: 10.1136/bmj.e7093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mamun AA, Peeters A, Barendregt J, et al. Smoking decreases the duration of life lived with and without cardiovascular disease: a life course analysis of the Framingham Heart Study. Eur Heart J. 2004;25:409–15. doi: 10.1016/j.ehj.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 55.Gellert C, Schottker B, Brenner H. Smoking and all-cause mortality in older people: systematic review and meta-analysis. Arch Intern Med. 2012;172:837–44. doi: 10.1001/archinternmed.2012.1397. [DOI] [PubMed] [Google Scholar]
- 56.Tollefsen IM, Hem E, Ekeberg O. The reliability of suicide statistics: a systematic review. BMC Psychiatry. 2012;12:9. doi: 10.1186/1471-244X-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Crump C, Ioannidis JP, Sundquist K, et al. Mortality in persons with mental disorders is substantially overestimated using inpatient psychiatric diagnoses. J Psychiatr Res. 2013;47:1298–303. doi: 10.1016/j.jpsychires.2013.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ioannidis JP. Are mortality differences detected by administrative data reliable and actionable? JAMA. 2013;309:1410–1. doi: 10.1001/jama.2013.3150. [DOI] [PubMed] [Google Scholar]
- 59.De Hert M, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10:52–77. doi: 10.1002/j.2051-5545.2011.tb00014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21:655–79. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]


