Abstract
IMPORTANCE
Depression among hearing impaired US adults has not been studied previously.
OBJECTIVE
To estimate the prevalence of and risk factors for depression among adults with hearing loss.
DESIGN, SETTING, AND PARTICIPANTS
Adults aged 18 years or older (N = 18 318) who participated in the National Health and Nutrition Examination Survey (NHANES), 2005–2010, a nationally representative sample.
INTERVENTIONS
Multistage probability sampling of US population.
MAIN OUTCOMES AND MEASURES
Depression, assessed by the 9-item Patient Health Questionnaire (PHQ-9) scale, and hearing impairment (HI), assessed by self-report and audiometric examination for adults aged 70 years or older.
RESULTS
The prevalence of moderate to severe depression (PHQ-9 score, ≥10) was 4.9% for individuals reporting excellent hearing, 7.1% for those with good hearing, and 11.4% for participants who reported a little trouble or greater HI. Using excellent hearing as the reference, after adjusting for all covariates, multivariate odds ratios (ORs) for depression were 1.4 (95% CI, 1.1–1.8) for good hearing, 1.7 (1.3–2.2) for a little trouble, 2.4 (1.7–3.2) for moderate trouble, 1.5 (0.9–2.6) for a lot of trouble, and 0.6 (0.1–2.6) for deaf. Moderate HI (defined by better ear pure-tone average of hearing thresholds at 0.5, 1, 2, and 4 kHz within the range 35- to 49-dB hearing level) was significantly associated with depression among older women (OR, 3.9; 95% CI, 1.3–11.3), after adjusting for age, sex, race/ethnicity, lifestyle characteristics, and selected health conditions.
CONCLUSIONS AND RELEVANCE
After accounting for health conditions and other factors, including trouble seeing, self-reported HI and audiometrically determined HI were significantly associated with depression, particularly in women. Health care professionals should be aware of an increased risk for depression among adults with hearing loss.
Unipolar depressive disorders have been reported1 as the leading cause and adult-onset hearing impairment (HI) as the second leading cause of years of life lived with disability among adults in high-income countries. Furthermore, depression and HI have been associated2,3 with personal, societal, and economic burden. However, the relationship between depression and HI has not been reported in a nationally representative sample of US adults. Previous studies4–8 have been limited primarily to older adults or specific geographically or ethnically distinct populations, and these have shown conflicting results.
Using data from the 2005–2010 National Health and Nutrition Examination Survey (NHANES),9 we examined the relationship between depression and self-reported HI for US adults aged 18 years or older. Because audiometric examination data were collected for adults aged 70 years or older, we also examined the association between depression and HI defined by hearing thresholds in this age range.
Methods
Participants
The NHANES, a nationally representative survey conducted by the National Center for Health Statistics, Centers for Disease Control and Prevention, uses a complex, multistage, probability sampling design to select participants representative of the civilian, noninstitutionalized US population.9 In NHANES 2005–2010, a total of 18 318 persons aged 18 years or older were interviewed at home and invited to a mobile examination center. Audiometric examinations, funded by the National Institute on Deafness and Other Communication Disorders, National Institutes of Health, were conducted on adolescents aged 12 to 19 years and adults aged 70 years or older.
The NHANES protocol was approved by the National Center for Health Statistics human subjects review board. Informed consent was obtained from all participants, who were financially compensated and received a report of the medical findings. In addition, transportation was provided to and from the mobile NHANES center, if necessary.
Outcome Measures
Self-reported Hearing Status
In a home interview before the mobile examination center examination, participants were asked the following question to rate their hearing (without a hearing aid): “Would you say your hearing is excellent, good, that you have a little trouble, moderate trouble, a lot of trouble, or are you deaf?” In this study, self-reported hearing difficulty was defined by responses of a little trouble or greater.
Audiometric Measure
In the NHANES 2005–2006 and 2009–2010 studies, the audiometric examination was administered to the full sample of older adults, aged 70 years or older (n = 1535). Air-conduction pure-tone thresholds were obtained in a sound-treated booth (Delta 143; Acoustic Systems) in the mobile examination center by trained examiners at 7 frequencies (0.5, 1, 2, 3, 4, 6, and 8 kHz, each ear) using an audiometer (AD226; Interacoustics) with supra-aural headphones (TDH-39; Telephonics) (replaced by insert earphones [E·A·Rtone 3A; Etymotic Research] for individuals with asymmetric hearing loss or collapsing ear canals). Ambient noise was monitored with a bioacoustic simulator (BA-201–25; Quest) and octave band monitor. Some participants with hearing aids (n = 30) were unable to remove them for the examination and were excluded. Additional people (n = 18) were excluded because of ear pain at the time of the examination. In this study, analysis of the hearing thresholds was based on a new HI classification recommended by the 2010 Global Burden of Disease Hearing Loss Expert Group.10 The recommendation uses better ear (BE) pure-tone averages (PTAs) of thresholds at 0.5,1, 2, and 4 kHz. An earlier World Health Organization classification11 used separate categories for children and adults; the new proposal is a unified classification based on uniform 15-dB hearing level (HL) increments in BE PTA. Six bilateral HI categories are recommended: mild (20- to 34-dB HL), moderate (35- to 49-dB HL), moderately severe (50- to 64-dB HL), severe (65- to 79-dB HL), profound (80- to 94-dB HL), and deaf (≥95-dB HL).
Depression Measure
The 9-item Patient Health Questionnaire (PHQ-9)12 depression scale was used to assess the frequency of symptoms experienced and reported by participants during the past 2 weeks. The PHQ-9 scores, ranging from 0 to 27, indicate the presence and severity of depression, with scores of 5, 10, 15, and 20 being the cut-points for mild, moderate, moderately severe, and severe depression, respectively. The validity and reliability of the PHQ and its 9-item depression module to establish depressive diagnosis and grade severity have been documented.12,13 Scores of 10 or higher on the PHQ-9 have a sensitivity of 88% and specificity of 88% for major depression.12 In the present study, the severity of depressive symptoms was evaluated using 2 categories: mild (PHQ-9 score, 5–9) and moderate to severe (PHQ-9 score, 10–27).
Covariates
Several potential confounding variables were taken into account, including sociodemographic and lifestyle characteristics, medical history, and health status, including trouble seeing. Variables included in the analyses were categorized as follows: age (18–44, 45–69, and ≥70 years), race/ethnicity (Hispanic, non-Hispanic black, non-Hispanic white, and other), educational level (<high school, high school graduate, and >high school), married or living with a partner (yes/no), living alone (yes/no), health insurance coverage (yes/no), body mass index (<25, 25 to <30, and ≥30 [calculated as weight in kilograms divided by height in meters squared]), smoking status (current, former, and never), binge drinking (ie, ever consumed ≥5 drinks of any alcoholic beverage almost every day [yes/no]), self-reported general health status (excellent, very good, or good; fair; and poor), trouble seeing even with glasses or contact lenses (yes/no), sleep disorder if diagnosed by a physician or other health professional (yes/no), self-reported history of cancer (yes/no), and ever worn a hearing aid (yes/no). Tinnitus was defined as experiencing ringing, roaring, or buzzing in the ears or head lasting 5 minutes or longer during the past year (yes/no). Poverty income ratio (PIR) is the ratio of annual income to the poverty threshold based on family size. If a family’s total income is less than the official poverty threshold, then PIR is less than 1.00, whereas PIR values of 1.00 or greater indicate income above the poverty level. This variable was categorized as PIR less than 1, 1 ≤ PIR < 3, and PIR of 3or more. Hypertension was defined by antihypertensive medication use or blood pressure of 140/90 mm Hg or higher. History of cardiovascular diseases (yes/no) was ascertained by self-report of coronary heart disease, angina, myocardial infarction, stroke, or congestive heart failure. Diabetes mellitus was defined as self-report of a diagnosis of the disease by a health care professional (excluding gestational diabetes mellitus) or hemoglobin A1c level of 6.5% or more (to convert to a percentage of total hemoglobin, multiply by 0.01).
Statistical Analysis
Statistical analyses were performed using SAS, version 9.3 (SAS Institute, Inc), and SUDAAN, version 11.0 (Research Triangle Institute), to calculate national estimates and SEs while taking into account the survey’s complex sampling design. Two-sided tests and a 5% significance level were used in the analysis. Participant characteristics are described using means for continuous variables and percentages for categorical variables. Multivariable logistic regression analysis with the calculation of odds ratios (ORs) and 95% CIs was used to assess associations between HI and depression after adjusting for selected covariates. Some analyses were stratified by sex and age groups. In all, 13.4% of participants (n = 2462) who did not have depression scores were excluded from subsequent analysis, leaving a sample of 15 856. Missing values were imputed for 0.6% of the participants who were missing some items in the depression score (n = 96) (75% were missing only 1 item). The multiple imputation procedure and the fully conditional specification method were used to impute missing data to minimize the bias associated with listwise deletion of participants with missing values. Five imputations per missing observation were performed, and the average measure was calculated using the SUDAAN software.
Results
The sample number and nationally weighted percentages with levels of significance for differences within variable categories are reported in Table 1 for various sociodemographic, lifestyle, and medical history characteristics. In this NHANES 2005–2010 sample of 18 318 adults, the mean age was 49.6 years (range, 18 to ≥85 years), and 51.7% were women. The race/ethnicity distribution was 12.9% Hispanic, 11.5% non-Hispanic black, 69.4% non-Hispanic white, and 6.2% other. This table also provides results separately by hearing status and depression status. For example, it is evident that older adults (≥70 years) are much more likely to report HI, but this is not true for either mild or moderate to severe depression. In addition, women were much more likely to report depression symptoms than were men, but they were less likely to report HI. Non- Hispanic whites were more likely to report HI but less likely to report depression. Lower educational level was strongly associated with depression but also significantly associated with HI. Several lifestyle factors, such as living alone, higher body mass index, current/former smoker, binge drinking, and poorer self-rated health status were associated with HI and depression. Also, most of the specific health conditions (eg, hypertension, diabetes mellitus, cardiovascular disease, cancer, trouble seeing, and sleep disorders) were strongly associated with HI and depression.
Table 1.
Selected Characteristics of US Adults Aged 18 Years or Older by Reported Hearing and Depression Status, NHANES 2005–2010a
| Characteristic | Sample Size, No. (N = 18 318 | All | Excellent or Good Hearing (n = 14 152) | HI (n = 4162) | P Value for χ2 | No Depression (n = 12 013) | Mild Depression (n = 2480) | Moderate to Severe Depression (n = 1363) | P Value for χ2 |
|---|---|---|---|---|---|---|---|---|---|
| Age, y | |||||||||
| 18 to 44 | 8569 | 49.4 | 56.0 | 25.4 | <.001 | 48.0 | 53.5 | 47.3 | <.001 |
| 45 to 69 | 6600 | 39.1 | 36.5 | 48.7 | 40.5 | 36.2 | 45.7 | ||
| ≥70 | 3149 | 11.5 | 7.5 | 25.9 | 11.5 | 10.3 | 7.0 | ||
| Sex | |||||||||
| Male | 8918 | 48.3 | 46.3 | 55.6 | <.001 | 51.4 | 41.6 | 35.8 | <.001 |
| Female | 9400 | 51.7 | 53.7 | 44.4 | 48.4 | 58.4 | 64.2 | ||
| Race/ethnicity | |||||||||
| Non-Hispanic white | 8569 | 69.4 | 66.4 | 79.9 | <.001 | 71.5 | 69.1 | 63.3 | <.001 |
| Non-Hispanic Black | 3836 | 11.5 | 12.9 | 6.8 | 10.8 | 10.7 | 15.9 | ||
| Hispanic | 5052 | 12.9 | 14.1 | 8.5 | 12.2 | 13.9 | 16.0 | ||
| Other | 861 | 6.2 | 6.6 | 4.8 | 5.5 | 6.3 | 4.8 | ||
| Educational level | |||||||||
| <High school | 5382 | 19.3 | 18.4 | 22.9 | <.001 | 16.6 | 23.3 | 30.2 | <.001 |
| High school graduate | 4561 | 25.1 | 24.3 | 27.8 | 24.4 | 26.4 | 28.6 | ||
| >High school | 8310 | 55.6 | 57.3 | 49.3 | 59.0 | 50.3 | 41.2 | ||
| Poverty income ratio | |||||||||
| <1 | 3598 | 18.6 | 19.0 | 17.3 | <.005 | 15.2 | 22.7 | 35.0 | <.001 |
| 1 to <3 | 7089 | 48.3 | 47.2 | 52.2 | 47.7 | 48.4 | 47.8 | ||
| ≥3 | 3234 | 33.1 | 33.8 | 30.5 | 37.1 | 28.8 | 17.2 | ||
| Married/living with partner | 10 345 | 63.4 | 63.1 | 64.3 | .32 | 66.8 | 58.4 | 50.9 | <.00l |
| Living alone | 2544 | 13.3 | 12.0 | 17.7 | <.001 | 12.3 | 14.5 | 16.8 | <.001 |
| Uninsured | 4394 | 19.6 | 20.9 | 14.7 | <.001 | 17.7 | 23.9 | 29.2 | <.001 |
| BMI | |||||||||
| <25 (Normal/underweight) | 6139 | 36.4 | 38.1 | 30.4 | <.001 | 36.3 | 33.8 | 31.3 | <.001 |
| 25 to <30 (Overweight) | 6025 | 34.0 | 33.3 | 36.5 | 35.1 | 31.2 | 29.7 | ||
| ≥30 (Obese) | 5437 | 29.5 | 28.6 | 33.1 | 28.5 | 35.0 | 39.0 | ||
| Smoking | |||||||||
| Current | 3754 | 22.4 | 22.4 | 22.3 | <.001 | 19.4 | 28.2 | 41.9 | <.001 |
| Former | 4261 | 24.4 | 21.7 | 33.7 | 25.5 | 24.3 | 19.6 | ||
| Never | 9104 | 53.2 | 55.9 | 44.0 | 55.1 | 47.5 | 38.5 | ||
| Binge drinker | 2261 | 12.1 | 10.4 | 18.2 | <.00l | 11.8 | 17.7 | 26.6 | <.00l |
| Self-rated health status | |||||||||
| Excellent, very good, or good | 13 928 | 82.7 | 85.7 | 71.7 | <.001 | 88.3 | 73.3 | 49.2 | <.001 |
| Fair | 3529 | 14.0 | 11.9 | 21.7 | 10.4 | 21.2 | 33.5 | ||
| Poor | 851 | 3.3 | 2.4 | 6.6 | 1.3 | 5.5 | 17.3 | ||
| Hypertension | 5549 | 26.9 | 23.0 | 40.7 | <.00l | 26.3 | 28.4 | 36.4 | <.00l |
| Diabetes mellitus | 2012 | 8.0 | 6.8 | 12.6 | <.001 | 7.2 | 9.7 | 13.3 | <.001 |
| Cardiovascular disease history | 1946 | 8.2 | 5.8 | 16.5 | <.001 | 7.0 | 9.3 | 14.8 | <.001 |
| Cancer history | 1610 | 8.7 | 6.8 | 15.6 | <.001 | 7.9 | 8.4 | 12.0 | .04 |
| Trouble seeing, even with glasses/contact lenses | 3574 | 17.1 | 13.9 | 28.5 | <.001 | 13.7 | 23.4 | 39.4 | <.001 |
| Sleep disorder | 1304 | 7.3 | 6.3 | 10.9 | <.001 | 5.6 | 9.8 | 22.1 | <.001 |
| Ever worn a hearing aid, age, yb | |||||||||
| 18 to 19 | 7.0 | 0.8 | 0.1 | 10.3 | <.05 | 0.3 | 0.8 | 0 | .13 |
| ≥70 | 578 | 18.6 | 1.4 | 36.5 | <.001 | 18.3 | 16.6 | 19.5 | .68 |
| Tinnitus, age, yb | |||||||||
| 18 to 19 | 111 | 10.3 | 8.3 | 37.9 | <.005 | 7.4 | 15.2 | 27.6 | .01 |
| ≥70 | 452 | 15.5 | 11.3 | 19.8 | <.001 | 16.2 | 16.2 | 19.8 | .66 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HI, hearing impairment; NHANES, National Health and Nutrition Examination Survey; PIR, poverty income ratio.
Hearing impairment was defined as any difficulty hearing. Depression categories were defined as follows: none, 9-item Patient Health Questionnaire (PHQ-9) score less than 5; mild, PHQ-9 score of 5 to 9; and moderate to severe, PHQ-9 score of 10 or higher. Data are given as population-weighted percentages unless otherwise indicated. Denominators vary because of missing data.
Data were available only among those aged 18 to 19 years (n = 1186) and 70 years or older (n = 3149).
Prevalence of Self-reported HI
Among all participants, the prevalence of self-reported hearing status was 41.4% with excellent hearing; 36.9% with good hearing; 13.9%, a little trouble; 5.2%, moderate trouble; 2.3%, a lot of trouble; and 0.2%, deaf. The estimated prevalence of self-reported HI, defined as a little trouble hearing or greater difficulty, was 21.7% (95% CI, 20.6%–22.9%) for all participants, 25.0% (23.3%–26.8%) for men, and 18.7% (17.8%–19.6%) for women; hence, the estimated prevalence of any self-reported HI was higher in men than in women.
Prevalence of Depression
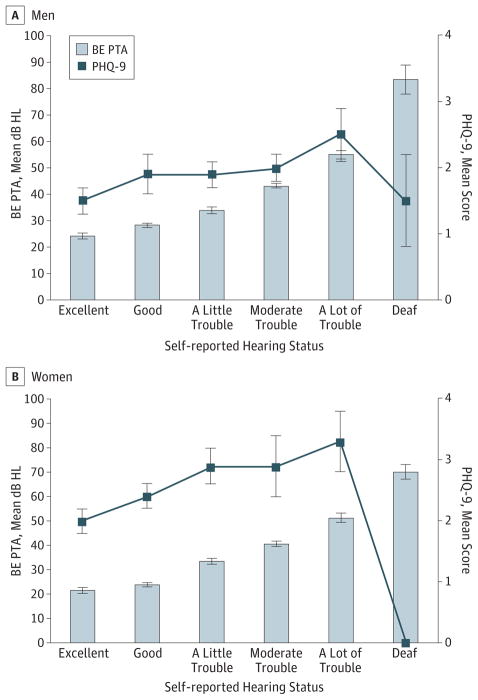
The estimated prevalence of moderate to severe depression (PHQ-9 score, ≥10) was 11.4% (95% CI, 10.1%–13.0%) for adults with any self-reported HI and 5.9% (5.3%–6.6%) for those without HI. Among those with HI, the prevalence of depression was 9.0% (95% CI, 7.5%–l0.8%) for men and 14.7% (12.7%–16.9%) for women. The estimated prevalence of depression was higher among adults with HI than in those without HI and higher among women than among men. The estimated prevalence of mild and moderate to severe depression, with and without HI, is presented in Figure 1. The prevalence of both levels of depression was significantly higher among men and women with HI.
Figure 1.
Prevalence of Depression Among US Adults by Sex and Reported Hearing Status, National Health and Nutrition Examination Survey 2005–2010
Limit lines indicate 95% CI.
Association Between Self-reported HI and Depression
Multivariate ORs (95% CI) for moderate to severe depression (PHQ-9 score, ≥10) are presented in Table 2 by each reported level of hearing. In model 1, after controlling for age, sex, and race/ethnicity, significantly higher odds of depression were associated with any HI (except being deaf) compared with excellent hearing. In model 2, after controlling for socioeconomic characteristics and marital status in addition to age, sex, and race/ethnicity, the significant associations with HI category were slightly reduced in magnitude but remained highly significant. In model 3, self-reported HI remained significantly associated with depression in men and women, even after controlling for factors in model 2 as well as body mass index, smoking, binge drinking, general health status, hypertension, history of cardiovascular disease, cancer, diabetes, sleep disorder, and trouble seeing. Self-reported HI was significantly associated with depression in US adults after taking into account numerous other covariates.
Table 2.
Prevalence and Multivariate ORs (95% CI) for Moderate to Severe Depression by Reported Hearing Status, US Adults, NHANES 2005–2010a
| Characteristic | Sample Size, No. | Prevalence,% (95% CI)b | OR (95% CI)c | ||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||
| All | 15 854 | 7.1 (6.5–7.9) | |||
| Excellent | 6174 | 4.9 (4.2–5.6) | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| Good hearing | 6031 | 7.1 (6.2–8.2) | 1.6 (1.3–1.9)d | 1.4 (1.1–1.8)d | 1.4 (1.1–1.8)e |
| A little trouble hearing | 2284 | 11.1 (9.4–13.1) | 3.1 (2.5–3.9)d | 2.6 (2.0–3.4)d | 1.7 (1.3–2.2)d |
| Moderate trouble hearing | 898 | 12.0 (9.5–15.0) | 3.9 (2.9–5.3)d | 3.7 (2.8–5.0)d | 2.4 (1.7–3.2)d |
| A lot of trouble hearing | 438 | 12.7 (9.4–17.0) | 4.5 (2.9–6.8)d | 3.2 (2.0–5.1)d | 1.5 (0.9–2.6) |
| Deaf | 29 | 5.2 (0.7–31.4) | 1.5 (0.2–12.4) | 1.5 (0.2–15.3) | 0.6 (0.1–2.6) |
| Male sex | 7808 | 5.2 (4.5–6.0) | |||
| Excellent | 2789 | 3.1 (2.4–3.9) | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| Good hearing | 2928 | 4.8 (3.9–6.0) | 1.7 (1.2–2.4)d | 1.4 (0.9–2.0) | 1.2 (0.8–1.8) |
| A little trouble hearing | 1233 | 8.5 (6.6–10.8) | 3.7 (2.4–5.6)d | 2.9 (1.8–4.8)d | 1.8 (1.0–3.1)e |
| Moderate trouble hearing | 563 | 8.9 (5.9–13.2) | 4.2 (2.6–6.9)d | 3.7 (2.1–6.4)d | 1.9 (1.1–3.2)e |
| A lot of trouble hearing | 279 | 12.7 (8.6–18.5) | 6.6 (3.9–11.2)d | 3.9 (2.0–7.7)d | 1.7 (0.9–3.2) |
| Deaf | 16 | 0 | |||
| Female sex | 8046 | 9.0 (8.1–9.9) | |||
| Excellent | 3385 | 6.3 (5.4–7.3) | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| Good hearing | 3103 | 9.3 (8.1–10.7) | 1.6 (1.3–1.9)d | 1.5 (1.2–1.9)d | 1.5 (1.1–1.9)d |
| A little trouble hearing | 1051 | 14.2 (11.7–17.1) | 2.9 (2.3–3.6)d | 2.5 (1.9–3.2)d | 1.6 (1.2–2.1)d |
| Moderate trouble hearing | 335 | 17.1 (12.6–22.9) | 3.8 (2.6–5.6)d | 3.8 (2.5–5.6)d | 2.8 (1.8–4.2)d |
| A lot of trouble hearing | 159 | 12.7 (8.6–18.2) | 2.9 (1.8–4.7)d | 2.6 (1.6–4.2)d | 1.4 (0.7–2.6) |
| Deaf | 13 | 10.7 (1.4–50.5) | 2.5 (0.3–20.3) | 2.6 (0.3–26.0) | 0.9 (0.2–4.0) |
Abbreviations: NHANES, National Health and Nutrition Examination Survey; OR, odds ratio; Ref, reference.
Moderate to severe depression was categorized as a 9-item Patient Health Questionnaire score of 10 or higher. Data are presented for individuals who were not missing data about depression.
Population-weighted percentages.
Model 1 was controlled for age, sex, and race/ethnicity; model 2 was controlled for age, sex, race/ethnicity, marriage, living alone, educational level, income, and health insurance; and model 3 was controlled for age, sex, race/ethnicity, marriage, living alone, educational level, income, health insurance, body mass index, smoking, binge drinking, self-reported health status, cardiovascular disease, cancer, diabetes mellitus, hypertension, sleep disorder, and trouble seeing.
P < .01.
P < .05.
Risk Factors for Depression With Self-reported HI
Among adults with any reported HI, the results listed in Table 3 from multivariate logistic regression models (reported overall and separately by sex) indicate that being female, having a PIR less than 1, being a current smoker, binge drinking, fair or poor health status, trouble seeing, and sleep disorder were significantly associated with increased higher odds of depression. In participants aged 70 years or older, HI was significantly associated with decreased odds of depression. The strongest associations were with the self-rated health status categories fair and, especially, poor. Race/ethnicity, educational level, living alone, uninsured status, body mass index, and hypertension were not significant in any of the multivariate models in which all factors were adjusted for simultaneously.
Table 3.
Multivariate-Adjusted ORs (95% CI) for Moderate to Severe Depression in US Adults Who Reported HI, NHANES 2005–2010a
| Characteristic | Sample Size, No. (N = 3649)b | Multivariate-Adjusted OR (95% CI)c | ||
|---|---|---|---|---|
| All | Male | Female | ||
| Sex | ||||
| Male | 2091 | 1 [Reference] | ||
| Female | 1558 | 2.0 (1.4–2.9)d | ||
| Age, y | ||||
| 18 to 44 | 782 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 45 to 69 | 1593 | 1.0 (0.7–1.4) | 1.5 (0.8–3.0) | 0.7 (0.4–1.3) |
| ≥70 | 1274 | 0.4 (0.2–0.7)d | 0.7 (0.3–1.7) | 0.3 (0.1–0.6)d |
| Race/ethnicity | ||||
| Non-Hispanic white | 2260 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Non-Hispanic black | 480 | 0.9 (0.6–1.5) | 0.8 (0.4–1.6) | 1.0 (0.5–1.9) |
| Hispanic | 794 | 0.9 (0.6–1.2) | 0.9 (0.6–1.5) | 0.8 (0.5–1.2) |
| Other | 115 | 0.7 (0.3–1.5) | 1.1 (0.4–3.3) | 0.4 (0.1–1.1) |
| Educational level | ||||
| <High school | 1193 | 0.9 (0.6–1.3) | 0.7 (0.4–1.3) | 1.1 (0.7–1.8) |
| High school graduate | 952 | 1.0 (0.6–1.5) | 0.7 (0.4–1.2) | 1.3 (0.8–2.3) |
| >High school | 1497 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Poverty income ratio | ||||
| <1 | 668 | 2.3 (1.4–3.8)d | 2.7 (1.4–5.3)d | 2.4 (1.2–4.8)e |
| 1 to <3 | 1584 | 1.3 (0.8–2.2) | 1.3 (0.7–2.6) | 1.4 (0.7–2.9) |
| ≥3 | 605 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Married/living with partner | 2189 | 0.8 (0.5–1.1) | 0.5 (0.3–0.8)e | 0.9 (0.5–1.7) |
| Living alone | 678 | 1.3 (0.8–2.2) | 1.0 (0.5–2.0) | 1.5 (0.8–2.8) |
| Uninsured | 644 | 1.3 (0.9–1.9) | 1.6 (0.9–2.8) | 1.1 (0.6–1.9) |
| BMI | ||||
| <25 (Normal/underweight) | 1046 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 25 to <30 (Overweight) | 1320 | 0.9 (0.6–1.4) | 0.8 (0.5–1.4) | 1.0 (0.6–1.9) |
| ≥30 (Obese) | 1173 | 1.0 (0.7–1.4) | 1.1 (0.6–2.1) | 1.1 (0.7–1.7) |
| Smoking | ||||
| Current | 770 | 1.5 (1.1–2.2)e | 1.8 (1.0–3.2)e | 1.3 (0.8–2.2) |
| Former | 1297 | 1.1 (0.7–1.6) | 1.2 (0.6–2.5) | 0.9 (0.5–1.6) |
| Never | 1504 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Binge drinker | 742 | 1.5 (1.0–2.2)e | 1.2 (0.7–1.9) | 2.0 (1.1–3.7)e |
| Self-rated health status | ||||
| Excellent, very good, or good | 2345 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Fair | 986 | 3.5 (2.3–5.2)d | 3.6 (2.1–6.1)d | 3.4 (2.1–5.7)d |
| Poor | 315 | 11.5 (6.5–20.6)d | 10.0 (4.9–20.6)d | 14.0 (5.9–33.6)d |
| Hypertension | 1678 | 0.9 (0.6–1.3) | 1.0 (0.6–1.7) | 0.7 (0.4–1.2) |
| Diabetes mellitus | 596 | 0.9 (0.6–1.2) | 0.6 (0.3–1.1) | 1.2 (0.7–2.0) |
| Cardiovascular disease history | 754 | 0.8 (0.6–1.3) | 1.3 (0.7–2.2) | 0.6 (0.3–1.0) |
| Cancer history | 613 | 1.2 (0.8–1.9) | 1.2 (0.5–2.7) | 1.3 (0.8–2.1) |
| Trouble seeing, even with glasses or contact lenses | 1122 | 2.1 (1.7–2.7)d | 2.7 (1.8–4.3)d | 1.7 (1.2–2.3)d |
| Sleep disorder | 409 | 2.4 (1.7–3.4)d | 2.1 (1.2–3.9)e | 2.8 (1.6–4.9)d |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HI, hearing impairment; NHANES, National Health and Nutrition Examination Survey; OR, odds ratio.
Hearing impairment was defined as any difficulty hearing, that is, a little trouble hearing or greater difficulty.
Denominators vary because of missing data.
The ORs were calculated after controlling for all other variables listed in the table.
P <.01.
P <.05.
The sex-specific models revealed that men and women share many of the same risk factors associated with depression, such as lower household income, binge drinking, general health status, trouble seeing, and sleep disorders. However, men have some specific risk factors; for example, the risk if married/living with partner was significantly reduced and if a current smoker was significantly increased only for men.
Global Burden of Disease Hearing Classification and Depression
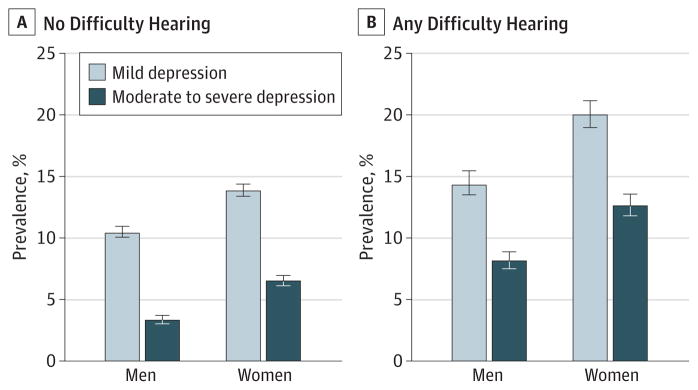
Hearing loss based on air-conduction PTAs of thresholds at 0.5, 1, 2, and 4 kHz (PTA5124) were calculated for participants aged 70 years or older. The mean BE PTA5124 is displayed by self-reported hearing categories for that population in Figure 2. The PTA5124 increased as self-reported hearing category progressed from excellent to deaf for both men and women. Compared with men, women had lower PTA5124 values but higher PHQ-9 scores in the categories of hearing from excellent to a lot of trouble.
Figure 2.
Better Ear Pure-Tone Average (BE PTA) and 9-Item Patient Health Questionnaire (PHQ-9) Mean Score by Reported Hearing Status, National Health and Nutrition Examination Survey 2005–2006 and 2009–2010
Air conduction, BE PTA of thresholds at 0.5,1,2, and 4 kHz, measured in decibels hearing level (HL) scale, for men (A) and women (B) for US adults aged 70 years or older. Limit lines indicate 95% CI.
The prevalence of depression among persons with HI based on hearing thresholds using the Global Burden of Disease classification is presented in Table 4. Results from multivariable logistic regression with adjustment for different sets of covariates described in models 1, 2, and 3 indicate that moderate HI (35 dB HL ≤ BE PTA < 50 dB HL) in women aged 70 years or older was associated with increased odds of depression after adjusting for covariates, but this was not true in men. Hearing loss in the BE of this degree of severity, PTA5124 of 35 dB HL or higher, is considered disabling hearing loss in the Global Burden of Disease classification.10
Table 4.
Multivariate ORs (95% CI) for Moderate to Severe Depression in US Adults Aged 70 Years or Older, NHANES 2005–2006 and 2009–2010
| GBD Hearing Classification, dB HL | Sample No. | Depression, % | Mean PHQ-9 Score | OR (95% CI)a | |||
|---|---|---|---|---|---|---|---|
| Crude | Model 1 | Model 2 | Model 3 | ||||
| All | |||||||
| BE PTA <20 | 299 | 4.7 | 2.2 | 1 [Ref] | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| 20 ≤ BE PTA < 35 | 614 | 3.9 | 2.2 | 0.9 (0.6–1.4) | 0.9 (0.6–1.5) | 0.9 (0.6–1.5) | 1.4 (0.6–2.9) |
| 35 ≤ BE PTA < 50 | 412 | 5.8 | 2.6 | 1.3 (0.8–2.4) | 1.5 (0.8–2.8) | 1.5 (0.8–2.8) | 2.1 (0.8–5.4) |
| BE PTA ≥50 | 210 | 2.8 | 1.9 | 0.6 (0.2–1.5) | 0.8 (0.3–2.0) | 0.7 (0.3–1.8) | 1.1 (0.3–3.9) |
| Men | |||||||
| BE PTA <20 | 109 | 5.5 | 1.7 | 1 [Ref] | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| 20 ≤ BE PTA < 35 | 295 | 4.0 | 1.8 | 1.0 (0.5–1.9) | 1.0 (0.5–2.0) | 1.1 (0.5–2.4) | 2.0 (0.5–8.1) |
| 35 ≤ BE PTA < 50 | 236 | 2.2 | 2.3 | 0.5 (0.2–1.1) | 0.5 (0.2–1.2) | 0.5 (0.2–1.2) | 0.5 (0.1–2.8) |
| BE PTA ≥ 50 | 149 | 2.8 | 1.7 | 0.6 (0.2–1.8) | 0.7 (0.2–2.1) | 0.6 (0.2–1.8) | 1.0 (0.1–9.3) |
| Women | |||||||
| BE PTA <20 | 190 | 4.4 | 2.4 | 1 [Ref] | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| 20 ≤ BE PTA < 35 | 319 | 3.8 | 2.5 | 0.8 (0.4–1.7) | 0.8 (0.4–1.7) | 0.8 (0.4–1.6) | 1.5 (0.6–3.5) |
| 35 ≤ BE PTA < 50 | 176 | 9.3 | 3.0 | 2.2 (1.1–4.2)b | 2.5 (1.2–5.1)b | 2.6 (1.3–5.3)b | 3.9 (1.3–11.3)b |
| BE PTA ≥ 50 | 61 | 2.9 | 2.4 | 0.5 (0.1–3.0) | 0.8 (0.1–3.9) | 0.7 (0.1–3.6) | 0.9 (0.1–5.8) |
Abbreviations: BE, better ear; GBD, Global Burden of Disease; HL, hearing level; NHANES, National Health and Nutrition Examination Survey; OR, odds ratio; PHQ-9,9-item Patient Health Questionnaire; PTA, pure-tune average of thresholds at frequency 0.5, 1, 2, and 4 KHz; Ref, reference.
Model 1 was controlled for age, sex, and race/ethnicity; model 2 was controlled for age, sex, race/ethnicity, marriage, living alone, educational level, income, and health insurance; and model 3 was controlled for age, sex, race/ethnicity, marriage, living alone, educational level, income, health insurance, body mass index, smoking, binge drinking, self-reported health, cardiovascular disease, cancer, diabetes mellitus, hypertension, sleep disorder, hearing aids, tinnitus, and trouble seeing.
P <.05.
Discussion
In this recent nationally representative survey, 11.4% of US adults with self-reported HI had moderate to severe depression (PHQ-9 score, ≥10) and an additional 19.1% had mild depressive symptoms (PHQ-9 score, 5–9); depression rates were higher in women than in men. The prevalence of depression increased as HI became worse, except among participants who, by self-report, were deaf and least likely to report depression. Among people aged 70 years or older, no significant association between self-reported HI and depression was found; however, a significant association between a hearing threshold- based measure of moderate HI and depression was found in women, but not in men. To our knowledge, this is the first report using the PHQ-9 instrument to assess depressive symptoms in conjunction with questions on self-reported HI and hearing threshold-based measures of HI in a racially diverse, multiethnic national sample.
Hearing impairment, an invisible handicap and one of the most common chronic conditions of later life,14 can impose a heavy social and economic burden on individuals, families, communities, and countries. Hearing impairment tends to isolate people from friends and family because of a decreased ability to communicate; as such, untreated HI may have considerable negative social, psychological, cognitive, and health effects.3 The impact of HI may be profound, with consequences for social, functional, and psychological well-being as well as the overall health of the individual. A meta-analysis15 reported that HI is among the most common chronic conditions associated with depression in people aged 65 years or older.
In the present study based on a nationally representative sample, HI was significantly associated with an increased risk of depression in adults of all ages, but was most pronounced in those aged 18 to 69 years. The findings are consistent with the results from a Norwegian population-based study16 of 50 398 adults aged 20 to 101 years. In a subsequent Dutch study, Nachtegaal et al17 reported that poorer hearing is significantly associated with depression in middle-aged adults (aged 40–49 years). Consistent with previous studies,7,18 the Dutch study did not find a significant association among participants aged 50 to 70 years. For older adults (aged >85 years), HI appeared to be protective against depression.8 Persons in different age groups may need to cope with psychosocial issues differently because of differences in lifestyle, responsibility, and circumstances.
Our results differ from those of Harada et al,19 who reported that HI is associated with depression in males but not in females. We found HI to be associated with depression in both men and women, although the prevalence of depression among those with any HI was higher in women (14.7%) than in men (9.0%). In the Blue Mountains Study,20 the investigators also found depressive symptoms to be more common in women than in men with HI. The present study shows that women had a higher prevalence of depression compared with men. On average, men begin to lose their hearing at high frequencies (3–6 k Hz) during middle age, probably resulting from a variety of factors but especially due to noise.21 Women, on average, have fairly well-preserved hearing at the higher frequencies, which are critical for understanding speech in noisy environments, until after reaching age 65 or 70 years, when they experience a steady decline.22,23
Additionally, we found that self-reported HI was significantly associated with increased odds of depression in each of our 3 major racial/ethnic groups: Hispanics, non-Hispanic blacks, and non-Hispanic whites (Figure 3). After controlling for covariates, no significant differences were observed in terms of race/ethnicity (Table 3). Unlike the present study, the investigation of Lee and Gomez-Marin18 evaluated associations between depression and HI defined by an audiometric threshold measure in targeted samples of US Hispanics living in geographic clusters (ie, Cuban-American, Mexican- American, and Puerto Rican adults aged 20–74 years) based on the Hispanic Health and Nutrition Examination Survey, 19841986. They concluded that the HI sample of Hispanics overall was not at increased risk of major depressive disorder despite the finding that the odds of HI were significantly greater among Puerto Ricans reporting more depressive symptoms.
Figure 3.
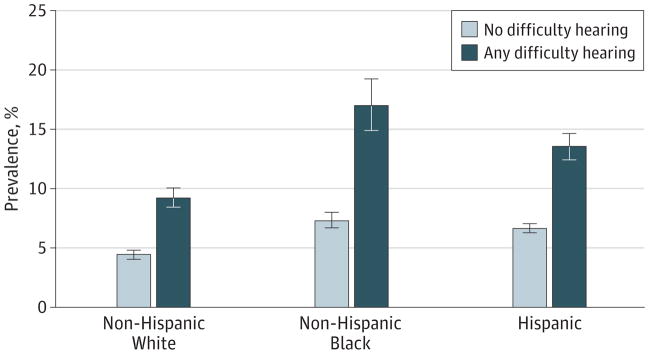
Prevalence of Moderate to Severe Depression Among US Adults by Race/Ethnicity and Reported Hearing Status Based on the National Health and Nutrition Examination Survey 2005–2006 and 2009–2010
Limit lines indicate 95% CI.
We did not find a significant relationship between depression and self-reported HI among men or women aged 70 years or older. Rather, we found a significant association between depression and a threshold-based measure of moderate HI, defined as BE PTA5124 between 35 and 50 dB HL, among women. These apparently inconsistent results may reflect the tendency of people in different age groups to assess their HI differently. For example, older people may be less likely to self-report HI activity limitations compared with younger people.24 Lee et al25 also found an independent association between depression and measured hearing loss in older people, but not between depression and self-reported hearing loss. Self-reported HI may not adequately substitute for threshold- based measures of HI among older people. Alternatively, Andersson and Green26 reported that anxiety scores did not correlate with pure-tone thresholds for hearing; however, anxiety did correlate with self-reported hearing difficulty in elderly patients with HI. Anxiety is important, but it is possible that signs of depression are strongly related to self-perceived HI.
In the present study, the prevalence of depression increased as HI became greater, ie, from excellent hearing to a lot of trouble, but decreased among those who self-reported as being deaf. Kvam et al27 reported that people who are deaf have significantly more symptoms of mental health problems compared with those who are not deaf. Nevertheless, our findings are consistent with those of previous studies8 that did not find a significant association between depression and self-reported deafness or a threshold-based measure of deafness. In the Blue Mountains Study,28 depression symptoms were significantly higher in participants aged 60 years or older with mild HI, but not in those with moderate to severe hearing loss.
The strongest association was for participants with moderate trouble hearing. Among respondents reporting at least some hearing loss, the categories with weakest association (ie, lowest ORs in model 3) (Table 2) with depression were the two with the most trouble hearing (ie, a lot of trouble or deaf). One reason for this result may be that people with severe to profound HI have had a different experience in their exposure and access to health care interventions for hearing. They are much more likely to have been identified and encouraged to try rehabilitation (eg, hearing aids, alternative listening devices, and cochlear implants). Thus, their lower prevalence of depression may be because more of them have had access to hearing health care services and thereby have obtained more help and earlier interventions compared with those with mild to moderate HI.29
Reduction in depressive symptoms and an improved quality of life were reported in previous studies4,8,20 of older adults using hearing aids. No information was collected on the use of hearing aids among persons aged 20 to 69 years in the present study. Data were available on the use of hearing aids among individuals aged 70 years or older, but we did not find a significant association between nonuse of hearing aids and depression among the older adults. The National Council on the Aging30 found that people with HI who did not use hearing aids more often stated that they had sadness, depression, worry, anxiety, paranoia, less social activity, emotional turmoil, and insecurity. In that study, both those with HI (56%) and their family members (66%) reported benefits from hearing aid use in terms of better relationships at home, more confidence, and better relationships with others. However, only 36% of people who had hearing aids and 39% of family members of hearing aid users stated there had been improvement of mental health.
Although data on the use of hearing aids were not available for all participants, as noted in Table 1, we attempted to investigate the effect of hearing aid use on depression. The prevalence of depression among participants who reported use of a hearing aid (9.1%) was lower than that among persons who did not report use of a hearing aid (11.7%). However, after controlling for potential confounders, no significant difference was found between the 2 groups (data not shown). Our result is consistent with the report by Nachtegaal et al.17 However, the NHANES question was phrased as, “Have you ever worn a hearing aid?” We do not know whether respondents answering in the affirmative used a hearing aid during the time interval for which they were asked about depressive symptoms. We concluded that it was not possible to assess whether hearing aid use affects depression based on our analysis of NHANES 2005–2010 data.
Although this study has several strengths, including a nationally representative adult sample and an effective detection of depressive symptoms using a short, easy-to-administer, well-validated instrument, there are some limitations. Audiometric threshold measurements were available only for adults aged 70 years or older, thus precluding our assessment of the association between depression and hearing threshold-based measures of HI in young or middle-aged adults. In the audiometric sample of participants aged 70 years or older, 11% partially completed the examination and 8% did not have an audiometric examination. Among those who did not have or complete the audiometric examination, “time constraint” was listed most frequently as the reason because the mobile examination center evaluations in NHANES overall include many other tests, all of which need to be completed in a period of 2.5 to 3.0 hours. Also, because of the limited sample size of NHANES (approximately 3000 adults per year aged ≥18 years), detailed results are not available for many smaller racial/ ethnic groups represented in the United States. Finally, because of the cross-sectional design of the survey, we cannot determine whether HI predates depression or to what extent self-reported depression may affect self-perceived HI.
Conclusions
We found a strong association between HI and depression among US adults of all ages, particularly women and those younger than 70 years. The prevalence of moderate to severe depression was higher among US adults aged 18 years or older with self-reported HI (11.4%) compared with those without HI (5.9%). Health professionals may be better able to improve the quality of life among people with HI by recognizing the signs and symptoms of depression and referring patients for mental health services.
Acknowledgments
Funding/Support: The National Health and Nutrition Examination Survey (NHANES) hearing questionnaire and examination component was supported with research contract funds via Interagency Agreement between the National Institute on Deafness and Other Communication Disorders (NIDCD)/National Institutes of Health and the National Center for Health Statistics (NCHS)/Centers for Disease Control and Prevention (CDC). The NIDCD also provided funding via Interagency Agreement to the National Institute for Occupational Safety and Health/CDC for calibration and maintenance of the audiometric equipment, training and monitoring the performance of health technicians conducting the hearing examinations, and jointly editing the preliminary data files.
Footnotes
Author Contributions: Dr Li had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Li, Zhang, Hoffman, Cotch.
Acquisition, analysis, or interpretation of data: Li, Hoffman, Themann.
Analysis and interpretation of data: All authors.
Drafting of the manuscript: Li, Hoffman, Themann.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Li, Zhang, Hoffman.
Obtained funding: Hoffman.
Administrative, technical, or material support: Zhang, Hoffman, Cotch, Themann, Wilson.
Study supervision: Hoffman.
Conflict of Interest Disclosures: None reported.
Role of the Sponsor: The NCHS staff contributed to the design and conduct of NHANES overall but were not involved in the analysis or interpretation of results in this manuscript; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of their respective federal agencies.
Previous Presentation: Preliminary findings from this report were presented orally at the annual meeting of the American Auditory Society; March 9, 2013; Scottsdale, Arizona.
Additional Contributions: We thank the NHANES participants, without whom this study would not have been possible, and the professional staff of NHANES and Westat Inc who conducted the study. May Chiu, BS, and Katalin Losonczy, MA, members of the Epidemiology and Statistics Program at the NIDCD, provided technical support. No financial compensation was given for these services.
References
- 1.World Health Organization. The Global Burden of Disease: 2004 Update. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 2.Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58(3):249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 3.Hogan A, O’Loughlin K, Miller P, Kendig H. The health impact of a hearing disability on older people in Australia. J Aging Health. 2009;21(8):1098–1111. doi: 10.1177/0898264309347821. [DOI] [PubMed] [Google Scholar]
- 4.Cacciatore F, Napoli C, Abete P, Marciano E, Triassi M, Rengo F. Quality of life determinants and hearing function in an elderly population: Osservatorio Geriatrico Campano Study Group. Gerontology. 1999;45(6):323–328. doi: 10.1159/000022113. [DOI] [PubMed] [Google Scholar]
- 5.Capella-McDonnall ME. The effects of single and dual sensory loss on symptoms of depression in the elderly. Int J Geriatr Psychiatry. 2005;20(9):855–861. doi: 10.1002/gps.1368. [DOI] [PubMed] [Google Scholar]
- 6.McDonnall MC. The effects of developing a dual sensory loss on depression in older adults: a longitudinal study. J Aging Health. 2009;21(8):1179–1199. doi: 10.1177/0898264309350077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernabei V, Morini V, Moretti F et al. Vision and hearing impairments are associated with depressive–anxiety syndrome in Italian elderly. Aging Ment Health. 2011;15(4):467–474. doi: 10.1080/13607863.2011.562483. [DOI] [PubMed] [Google Scholar]
- 8.Boorsma M, Joling K, Dussel M et al. The incidence of depression and its risk factors in Dutch nursing homes and residential care homes. Am J Geriatr Psychiatry. 2012;20(11):932–942. doi: 10.1097/JGP.0b013e31825d08ac. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention National Center for Health Statistics. [Accessed July 30, 2012];National Health and Nutrition Examination Survey. http://www.cdc.gov/nchs/nhanes.htm.
- 10.Stevens G, Flaxman S, Brunskill E, Mascarenhas M, Mathers CD, Finucane M Global Burden of Disease Hearing Loss Expert Group. Global and regional hearing impairment prevalence: an analysis of 42 studies in 29 countries. Eur J Public Health. 2013;23(1):146–152. doi: 10.1093/eurpub/ckr176. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. [Accessed June 5, 2013];Prevention of deafness and hearing impaired grades of hearing impairment. http://www.who.int/pbd/deafness/hearing_impairment_grades/en/index.html.
- 12.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study: Primary Care Evaluation of Mental Disorders: Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 14.Campbell VA, Crews JE, Moriarty DG, Zack MM, Blackman DK. Surveillance for sensory impairment, activity limitation, and health-related quality of life among older adults—United States, 1993–1997. MMWR CDC Surveill Summ. 1999;48(8):131–156. [PubMed] [Google Scholar]
- 15.Huang CQ, Dong BR, Lu ZC, Yue JR, Liu QX. Chronic diseases and risk for depression in old age: a meta-analysis of published literature. Ageing Res Rev. 2010;9(2):131–141. doi: 10.1016/j.arr.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Tambs K. Moderate effects of hearing loss on mental health and subjective well-being: results from the Nord-Trøndelag Hearing Loss Study. Psychosom Med. 2004;66(5):776–782. doi: 10.1097/01.psy.0000133328.03596.fb. [DOI] [PubMed] [Google Scholar]
- 17.Nachtegaal J, Smit JH, Smits C et al. The association between hearing status and psychosocial health before the age of 70 years: results from an Internet-based national survey on hearing. Ear Hear. 2009;30(3):302–312. doi: 10.1097/AUD.0b013e31819c6e01. [DOI] [PubMed] [Google Scholar]
- 18.Lee DJ, Gomez-Marin O. Major depressive disorder, depressive symptoms, and bilateral hearing loss in Hispanic adults. J Affect Disord. 1997;44(2–3):189–195. doi: 10.1016/s0165-0327(97)00044-x. [DOI] [PubMed] [Google Scholar]
- 19.Harada S, Nishiwaki Y, Michikawa T et al. Gender difference in the relationships between vision and hearing impairments and negative well-being. Prev Med. 2008;47(4):433–437. doi: 10.1016/j.ypmed.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 20.Gopinath B, Wang JJ, Schneider J et al. Depressive symptoms in older adults with hearing impairments: the Blue Mountains Study. J Am Geriatr Soc. 2009;57(7):1306–1308. doi: 10.1111/j.1532-5415.2009.02317.x. [DOI] [PubMed] [Google Scholar]
- 21.Hoffman HJ, Dobie RA, Ko CW, Themann CL, Murphy WJ. Americans hear as well or better today compared with 40 years ago: hearing threshold levels in the unscreened adult population of the United States, 1959–1962 and 1999–2004. Ear Hear. 2010;31(6):725–734. doi: 10.1097/AUD.0b013e3181e9770e. [DOI] [PubMed] [Google Scholar]
- 22.Hoffman HJ, Dobie RA, Ko CW, Themann CL, Murphy WJ. Hearing threshold levels at age 70 years (65–74 years) in the unscreened older adult population of the United States, 1959–1962 and 1999–2006. Ear Hear. 2012;33(3):437–440. doi: 10.1097/AUD.0b013e3182362790. [DOI] [PubMed] [Google Scholar]
- 23.Jerger J, Chmiel R, Stach B, Spretnjak M. Gender affects audiometric shape in presbyacusis. J Am Acad Audiol. 1993;4(1):42–49. [PubMed] [Google Scholar]
- 24.Gatehouse S. Determinants of self-reported disability in older subjects. Ear Hear. 1990;11(5):57S–65S. [PubMed] [Google Scholar]
- 25.Lee AT, Tong MC, Yuen KC, Tang PS, Vanhasselt CA. Hearing impairment and depressive symptoms in an older Chinese population. J Otolaryngol Head Neck Surg. 2010;39(5):498–503. [PubMed] [Google Scholar]
- 26.Andersson G, Green M. Anxiety in elderly hearing impaired persons. Percept Mot Skills. 1995;81(2):552–554. doi: 10.1177/003151259508100238. [DOI] [PubMed] [Google Scholar]
- 27.Kvam MH, Loeb M, Tambs K. Mental health in deaf adults: symptoms of anxiety and depression among hearing and deaf individuals. J Deaf Stud Deaf Educ. 2007;12(1):1–7. doi: 10.1093/deafed/enl015. [DOI] [PubMed] [Google Scholar]
- 28.Gopinath B, Rochtchina E, Wang JJ, Schneider J, Leeder SR, Mitchell P. Prevalence of age-related hearing loss in older adults: Blue Mountains Study. Arch Intern Med. 2009;169(4):415–416. doi: 10.1001/archinternmed.2008.597. [DOI] [PubMed] [Google Scholar]
- 29.Meyer C, Hickson L. What factors influence help-seeking for hearing impairment and hearing aid adoption in older adults? Int J Audiol. 2012;51(2):66–74. doi: 10.3109/14992027.2011.611178. [DOI] [PubMed] [Google Scholar]
- 30.Seniors Research Group. The Consequences of Untreated Hearing Loss in Older Persons. Washington, DC: National Council on the Aging; 1999. [PubMed] [Google Scholar]