Abstract
In India the sand fly, Phlebotomus argentipes, transmitted parasitic disease termed kala-azar is caused by Leishmania donovani (LD) in humans. These immune-evading parasites have increasingly developed resistance to the drug sodium antimony gluconate in endemic regions.
Lack of early diagnosis methods for the disease limits the information available regarding the early interactions of this parasite with either human tissues or cell lineages. We reasoned that peripheral blood mononuclear cells (PBMCs) from healthy human beings could help compare some of their immune signatures once they were exposed for up to 8 days, to either pentavalent antimony sensitive (SbS-LD) or resistant (SbR-LD) Leishmania donovani isolates.
At day 2, PBMC cultures exposed to SbS-LD and SbR-LD stationary phase promastigotes had four and seven fold higher frequency of IL-10 secreting monocyte-macrophage respectively, compared to cultures unexposed to parasites. Contrasting with the CD4+CD25−CD127− type-1 T-regulatory (Tr1) cell population that displayed similar features whatever the culture conditions, there was a pronounced increase in the IL-10 producing CD4+CD25+CD127low/− inducible T-regulatory cells (iTregs) in the PBMC cultures sampled at day 8 post addition of SbR-LD.
Sorted iTregs from different cultures on day 8 were added to anti-CD3/CD28 induced naïve PBMCs to assess their suppressive ability. We observed that iTregs from SbR-LD exposed PBMCs had more pronounced suppressive ability compared to SbS-LD counterpart on a per cell basis and is dependent on both IL-10 and TGF-β, whereas IL-10 being the major factor contributing to the suppressive ability of iTregs sorted from PBMC cultures exposed to SbS–LD. Of note, iTreg population frequency value remained at the basal level after addition of genetically modified SbR-LD lacking unique terminal sugar in surface glycan.
Even with limitations of this artificial in vitro model of L. donovani-human PBMC interactions, the present findings suggest that SbR-LD have higher immunomodulatory capacity which may favour aggressive pathology.
Author Summary
The disease Kala-azar is caused by Leishmania donovani (LD). The disease is characterized by the depression of cellular immune response. In the Indian subcontinent LD parasites are mostly resistant to commonly used antileishmanial drug, like sodium antimony gluconate (SAG). It is known that infection with pentavalent antimony (Sb)-resistant parasites induces aggressive pathology- the cause is still not known. Sb-resistant parasites endowed with unique glycan which may also play an important role in the pathogenesis as following removal of terminal sugar of glycan these parasites behave like sensitive parasites. The diagnosis of the disease is possible after the disease sets in and therefore limited information is available on the host-parasite interaction at the onset of disease. As a surrogate of in vivo scenario we studied the interaction between normal human PBMC with Sb-sensitive and Sb-resistant parasites. The Sb-resistant parasites upon interaction with human peripheral blood mononuclear cells (PBMC) in vitro produced two distinct inhibitory cytokines, IL-10 and TGF-β. Similar experiment with Sb-sensitive LD induced much less amount of above cytokines. Thus aggressive pathology induced by Sb-resistant LD, may be, in part attributed to production of dual inhibitory cytokines where surface glycan of the parasite may play a decisive role.
Introduction
Visceral leishmaniasis (VL) or Kala-azar has emerged as a major public health issue in India and neighbouring countries in the last few decades. Pentavalent antimonial compound is the first line drug for therapy of leishmaniasis, with Amphotericin B, Miltefosine and Paramomycin serving as the second line of drugs. Emergence of drug resistance against these drugs has made the situation more alarming for the effective treatment of the disease [1]–[3]. In VL patients, a strong Th1 response is required to prevent the parasitic dissemination while Th2 like cytokines, have shown to aggravate VL [4]–[6]. Suppression of T cell mediated immunity in VL is reported to be mediated by diverse mechanism(s) including i) elicitation of Th2 skewed host immune response [6], ii) effect in macrophage function [7], [8] and iii) regulatory T-cell (Treg) mediated suppression of effector T cell function [9]. However, the detailed mechanism of T cell suppression among VL patients still remains inconclusively elucidated and requires better delineation.
The simplified view that Th1 response leads to cure and Th2 response indicates disease susceptibility cannot fully explain the immune response during active VL. Numerous cytokines from many different cellular sources are involved following Leishmania infection and their fine balance may define final outcome of the disease [10]. Remarkable heterogeneity is known to exist among the T cells in terms of their distinct phenotype, function and their proportional participation is believed to dictate the overall T-cell function against parasitic invasion [10], [11]. Suppressive influence of regulatory T cells on effector T cell function suggests their critical involvement in experimental Leishmaniasis [12] and human VL [13]. Subtypes of Treg cells include thymus derived natural Treg cells (nTreg) or adaptive/induced Treg (iTreg). Peripherally induced T regulatory cells (iTreg) may be CD25+FoxP3+CD127low/− iTregs or other FoxP3− induced T regulatory cells such as Tr1 and TH3 cells [14], [15].Throughout this article we would mention CD4+CD25+CD127low/− cells as iTreg cells and CD4+CD25−CD127− cells as Tr1 cells.
Till date all the studies in human VL deals with either active patients or recovered cases of VL. Understanding of immune response on early interaction with the parasite and subsequently the disease onset in host still remains inconclusive. With the emergence of drug resistance, it is imperative to get more conclusive picture of host response during early onset of the disease. This will help us to adopt a better therapeutic approach in controlling human VL, especially for the drug unresponsive cases.
The role of IL-10 as an immunosuppressive molecule is increasingly becoming important in human VL. According to reports, there is an increase in the production of IL-10 among drug-unresponsive cases [6], [16]. In vitro infection of murine macrophages and dendritic cells with Pentavalent antimonial resistant (SbR) LD isolates also triggers greater production of IL-10, compared to that of Pentavalent antimonial sensitive (SbS) LD infection [16], [17]. There can be multiple cellular sources of IL-10 in VL patients [18], [19]. However, identities of the distinct cell types contributing to higher IL-10 in drug resistant LD infection remain elusive.
The present study highlights sequential events during the interaction of host PBMCs with SbS and SbR LD isolates. Most animal studies with needle injection challenge use very high infection dose (106 to 108 parasites) but in natural transmission the actual dose of parasite is much lower [20]. Using naive human PBMCs in an in vitro set up, we investigated the possible sources of IL-10 during host-parasite interaction. Here we showed that SbR and SbS-LD isolates sensitise the host cell differentially even at low inoculum. As an immediate interaction response, at early time points several immune cells including monocyte/macrophage, CD4+CD25−CD127− Tr1 and CD4+CD25+CD127low/− iTreg cells produce IL-10 in both SbS and SbR-LD infection. Interestingly, at a later time point, CD4+CD25+CD127low/− iTreg cells contribute towards the enhanced suppression of effector cells in SbR-LD infection by generating more IL-10 and TGF-β. This study analysed the differential immune modulation by SbR-LD isolates during their interaction with human PBMCs.
Materials and Methods
Ethics statement
Use of Human subjects was approved by “Ethical Committee of Human Subjects” of Indian Institute of Chemical Biology. Blood were drawn from normal healthy individuals after their written informed consent.
Parasites
Stationary phase promastigotes of well characterized Pentavalent antimonial sensitive (SbS) Leishmania donovani strain AG83 (MHOM/IN/83/AG83), 777 (MHOM/IN/09/BHU777/0), 816 (MHOM/IN/10/BHU816/1) and Pentavalent antimonial resistant (SbR) Leishmania donovani strain 138 (MHOM/IN/2005/BHU138), 575 (MHOM/IN/09/BHU575/0), 814 (MHOM/IN/10/BHU814/1) were used [16].We selected the drug resistant parasites depending on different parameters like their IC50 values, surface expression of multidrug receptors, different biophysical properties of the parasite membranes; the details of which is described elsewhere [16]. Parasites were harvested on day 5 of culture for in vitro evaluation of the response of peripheral blood mononuclear cells (PBMCs).GALT Knock down SbR-Leishmania donovani (KDSbR-LD) parasites were generated as described previously [21].
Isolation and in vitro culture of mononuclear cells
Fifty millilitres of human blood was collected during each blood draw from healthy individuals after their informed consent. The donors reported to have never suffered from leishmaniasis and have never travelled to leishmaniasis endemic regions. They were all tested rK39 negative and considered as Leishmania naïve. The PBMC were isolated from heparinized venous blood by passage over a Ficoll-Hypaque 1.077 (Sigma-Aldrich) gradient. PBMC were washed three times and resuspended at a concentration of 2.5×106 cells/mL in complete medium consisting of RPMI 1640 medium supplemented with 2 mM L-glutamine, penicillin (100 U/mL), gentamicin (100 µg/mL), and 10% heat-inactivated human AB serum (Sigma-Aldrich). The cells were plated in 24-well tissue culture plates (Costar, Corning, NY) in a volume of 1 mL/well. Leishmania donovani promastigotes were opsonised for 1 h at 37°C in RPMI 1640 containing 10% heat-inactivated AB+ serum in a humidified 5% CO2 atmosphere, washed, and resuspended in complete RPMI 1640. Opsonisation was conducted to optimize infection and approximate the vivo conditions. PBMC's were cultured with 2.5×105/mL of opsonised promastigotes (approximate parasite to monocyte ratio, 1∶1) or medium alone. Supernatants were harvested at 1, 2, 3 and 8 days post parasite addition for cytokine quantification.
For parasite burden enumeration the same assay was set up on coverglass. On early (day 2) and later time point (day 8), coverglasses were washed, fixed with methanol followed by staining with Giemsa. Stained coverglasses were then mounted on a slide and observed under light microscope.
Cytokine detection
Cytokines were quantified in supernatant samples obtained from cultures at 24, 48, 72 hrs and day 8 using the BD human Th1/Th2 cytokine kit II (BD Pharmingen) and BD CBA human inflammatory kit. To double check the results, IFN-γ and IL-10 were also measured by enzyme-linked immunosorbent assay (ELISA) [22]. IL-27 and TGF-β levels were determined by using human DUO set (R and D system). CBA analysis was done using FCAP array in a BD FACS ARIAII flow cytometer.
FACS analysis
Cells were stained with relevant antibodies on ice for 30 minutes in PBS buffer containing 2% FCS and 0.1% sodium azide. Before staining for surface markers, cells were incubated with Fc Blocker (CD16/CD32) for 30 minutes to minimize non-specific staining. Cells were washed twice before being analysed by BD FACS ARIA II flow cytometer. Live cells were gated based on forward and side scatter profiles and based on exclusion with live/dead aqua marker (Invitrogen). The following antibodies were used for staining: anti-human CD3 PerCP, CD4 APC or CD4 PE-Texas red, CD25 APC-Cy7, CD127 PE-Cy7, GARP PE (All from BD Biosciences) and anti-human Latency associated peptide (LAP)-TGF-β1 Alexa Fluor 488 (R and D systems). Recombinant human LAP (rLAP) that associates with TGF-β1 was purchased from R and D systems. Analysis was performed using FlowJo software (Tree Star).
The Tr1 and iTreg cells were sorted on the BD FACS ARIAII Flow Cytometer aseptically for further experiments. 2.5 million PBMCs from each well of tissue culture plate were sorted in approximately 5 minutes. Sorted cells were collected in 12×75 mm polypropylene tubes pre-coated with human AB serum and containing complete RPMI-1640 with 10% human AB serum.
IL-10 secretion assay
IL-10 secretion assay was used for evaluation of IL-10 production from different subset of cells (Milteny Biotech) according to manufacturer's protocol. Briefly PBMCs were harvested after in vitro infection with different LD parasites at early (48 hr p.i) and late time point (8 day p.i) cells These PBMC's were then labelled with IL-10 catch reagents and kept for 45 minutes to 1 hr in rocking condition at 37°C.During this time period secreted IL-10 binds to the IL-10 catch reagent. After that the cells were stained with PE labelled anti-IL-10 detection antibody along with fluorescent labelled anti-human CD4, anti-human CD3, anti-human CD14, anti-human CD127, anti-human CD25 antibody and acquired on FACS ARIA II flow cytometer. Data analysis was performed using FlowJo software (Tree Star).
Quantitative PCR
Total RNA from the sorted cells was isolated and cDNA was synthesized using SuperScript VILO cDNA Synthesis Kit (Invitrogen). 50–100 ng of total RNA was used for the synthesis of cDNA. RT2 qPCR Primer Assay Primers were purchased from SA Biosciences. Real-time quantitative PCR was conducted as per the protocol described earlier [23], [24]. Briefly, it was carried out with 12.5 µl of SYBR green PCR master mix (ABI), 1 µl of cDNA from RT reaction mix, and gene specific primers in a final volume of 25 µl. PCR was conducted under the following conditions: initial denaturation at 95°C for 10 min followed by 40 cycles, each consisting of denaturation at 95°C for 15 s, annealing at 60°C for 1 min, and extension at 72°C for 40 s per cycle using the ABI 7500 Real time PCR system. cDNAs from normal uninfected controls were used as “comparator samples” for quantification of those corresponding to test samples. All quantifications were normalized to the housekeeping gene 18SrRNA. A no-template control c-DNA was included to eliminate contaminations or nonspecific reactions. The cycle threshold value was defined as the number of PCR cycles required for the fluorescence signal to exceed the detection threshold value background noise [25]. Differences in gene expression were calculated by the comparative CT method [24]. This method compares test samples to a comparator sample and uses results obtained with a uniformly expressed control gene (18SrRNA) to correct for differences in the amounts of RNA present in the two samples being compared to generate a ΔCT value. Results are expressed as the degrees of difference between ΔCT values of test and comparator samples.
Co-cultures and proliferation assays
To verify the regulatory function of iTreg cells (CD4+CD25+CD127low/−), iTreg cells were isolated by sorting from 8 days SbR, SbS-LD infected and unstimulated PBMC's. This isolated Treg cells were co-cultured with autologous freshly isolated PBMC at different iTreg: responder ratio in 96-well U-bottom plates in the presence of anti-CD3/CD28/CD2 mixed beads (T Cell Activation/Expansion Kit, Milteny Biotech) at 37°C and 5% CO2. On day three, 4 h before the end of incubation period, BrdU solution was added to the cells. BrdU will be incorporated in the proliferating cells. The level of BrdU incorporation was measured according to manufacturer's protocol (Millipore) and the absorbance was measured at 450 nm using ELISA plate reader (DTX 800 multimode detector: Beckman Coulter).The suppression index was calculated as described earlier [26], when the assay was performed in the presence of neutralizing IL-10 (25 µg/ml) or rLAP (20 µg/ml), the reagents were added at the start of the assay in the co-culture experiment.
Statistical analysis
All experiments were done on blood from individual donor and a representative/pooled data are presented, interassay variation being within 5–10%. All graphs and statistical analyses were generated in GraphPad Prism 5.01 (GraphPad, San Diego,CA). Student's two tailed paired t test, Mann-Whitney test and Wilcoxon matched-pairs test was used to determine differences between different groups with 95% confidence intervals. P values less than 0.05 were considered to be significant for all analyses.
Results
SbS-LD or SbR-LD induced IL-10 production from normal PBMC
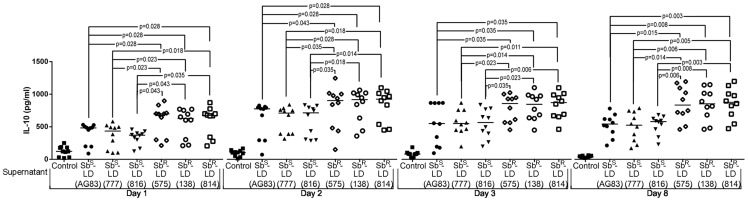
The kinetics of IL-10 production in culture supernatants from PBMC upon co-culturing with SbS-LD or SbR-LD was quantified. The experiment was conducted up to day 8 beyond which the culture could not be maintained ( Figure 1 ). The results were plotted as individual value and expressed as median. There is statistically significant enhancement in IL-10 production from PBMC in response to in vitro parasite challenged with respect to unstimulated control ( Figure 1 ).The maximum IL-10 production was noted on day 2 ( Figure 1 , Table 1 ). There was essentially 50% increase in IL-10 production in SbR-LD driven PBMC culture supernatants (SbR-supernatant) as compared to SbS-LD driven PBMC culture supernatant (SbS-supernatant) from day 1–3. However, on day 8, SbS-supernatant showed more substantial decrease in IL-10 production as compared to resistant counterpart ( Table 1 ). In this investigation three SbR-LD (LD-575, LD-138 and LD-814) and three SbS-LD (AG83, LD-777 and LD-816) strains were used. Since, SbR-LD-575, SbR-LD-138 and SbR-LD-814 induced essentially similar level of IL-10 production as evident from the median values ( Figure 1 , Table 1 ), we used SbR-LD-575 (henceforth defined as SbR-LD) as the representative of pentavalent antimony (Sb)-resistant parasites for further studies. Similarly AG83 (henceforth defined as SbS-LD) was used as the representative of pentavalent antimony (Sb)-sensitive parasites. We focused our studies on day 2 (early time point) and day 8 (late time point) for the rest of the investigation.
Figure 1. SbR-LD parasites induce greater IL-10 production than SbS-LD isolates.
Kinetics of IL-10 production during early interaction with different SbS and SbR-LD isolates. Briefly, freshly isolated PBMCs were incubated with SbS and SbR-LD isolates and culture supernatants (SbS and SbR-Sup) were isolated on day- one, two, three and eight, and IL-10 level was measured by ELISA/CBA. The level of IL-10 production at different time points are represented (day one, two, three and eight), n = 10, median values of different time points were indicated. Data were analysed by the Mann-Whitney test, and levels of significance are indicated by P values.
Table 1. Median values of IL-10 production (pg/ml) at different time points.
| CONTROL | SbS-sup. (AG83) | SbS-sup. (BHU-777) | SbS-sup. (BHU-816) | SbR-sup. (BHU-575) | SbR-sup. (BHU-138) | SbR-sup. (BHU-814) | |
| DAY 1 | 121.8 | 483.4 | 434.2 | 371.0 | 696.8 | 627.5 | 673.7 |
| DAY 2 | 105.3 | 783.5 | 716.7 | 721.0 | 911.4 | 925.4 | 932.5 |
| DAY 3 | 82.48 | 553.9 | 554.5 | 569.5 | 865.4 | 852.6 | 879.3 |
| DAY 8 | 40.20 | 547.5 | 529.7 | 585.6 | 842.0 | 861.5 | 885.0 |
The median values of IL-10 production at different time points are tabulated. Freshly isolated PBMCs were incubated with different SbS and SbR-LD isolates and culture supernatants (SbS and SbR-Sup) were isolated on day- one, two, three and eight, and IL-10 level (pg/ml) was measured by ELISA/CBA.
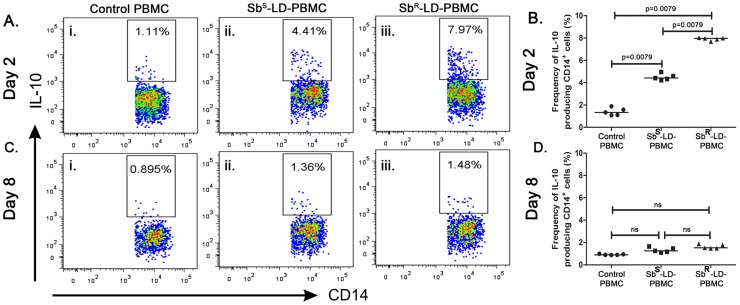
CD14+ cells as a source of IL-10 in response to SbS-LD and SbR-LD
The frequencies of CD14+IL-10+ cells were enumerated in PBMCs in response to SbS-LD or SbR-LD challenge. It was observed that in response to SbS-LD and SbR-LD challenge, frequency of CD14+IL-10+ cells increased four and seven folds on day2 respectively compared to control ( Figure 2A, B ). The frequency of CD14+IL-10+ was decreased on day 8 as compared to day 2, regardless of input parasites ( Figure 2C, D ). Interestingly, one could see IL-10 in the culture supernatants on day 8 suggesting there are other potential sources of IL-10.
Figure 2. CD14+ monocyte/macrophage cells produce IL-10 during initial interaction.
Production of IL-10 from CD14+ monocyte/macrophage cells. The frequencies of CD14+IL-10+ cells from SbS-LD-PBMC and SbR-LD-PBMC at different time points are represented. A–B. Percentage of IL-10 producing CD14+ cells on day two and C–D; on day eight. Pseudo colour plot indicate one representative data set. Data were analysed by the Mann-Whitney test, and levels of significance are indicated by P values.
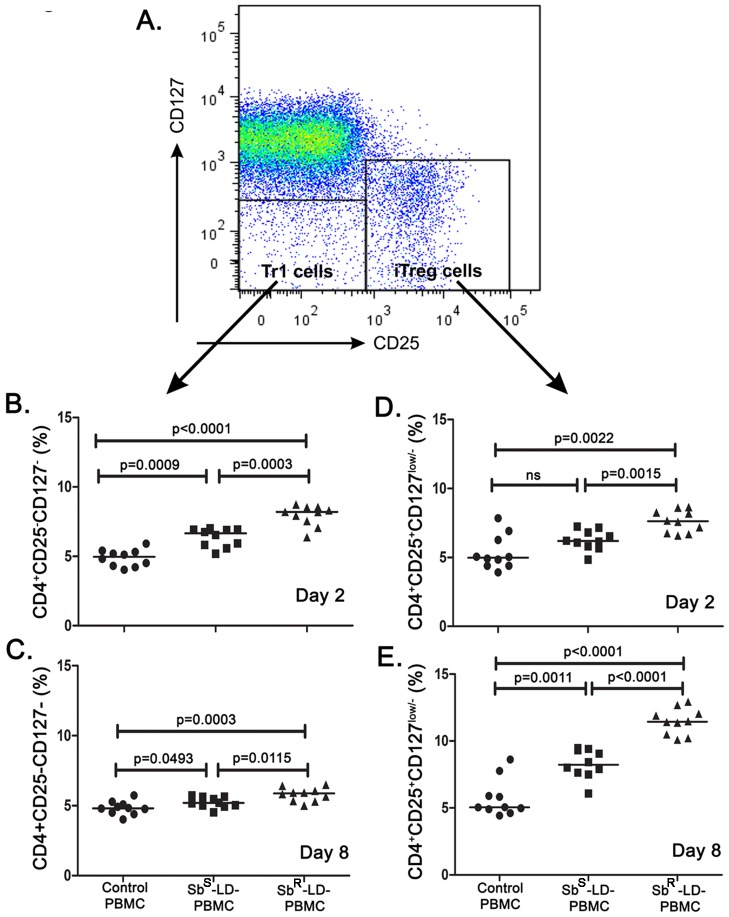
Induction of CD4+CD25−CD127− (Tr1) and CD4+CD25+CD127low/− (iTreg) cells in response to SbS-LD and SbR-LD
Based on earlier reports [27], here we have used IL-7 receptor (CD127) to define the T regulatory cells. CD4+CD25+CD127low/− cells were designated as iTreg cells and CD4+CD25−CD127− cells were designated as the Tr1 cells ( Figure 3A ).
Figure 3. Different regulatory T-cells are induced upon interaction with Leishmania donovani.
Percentage of Tr1 (CD4+CD25−CD127−) and iTreg (CD4+CD25+CD127low/−) cells among gated CD4+ cells (n = 10). Briefly, freshly isolated PBMCs were incubated with SbS and SbR-LD isolates and after day 2 and day 8 cells were stained and percentage of Tr1 and iTreg cells were analysed by Flow Cytometry. Lymphocytes were gated based on forward and side scatter profiles, and live cells were identified on the basis of exclusion of LIVE/DEAD Aqua dye (Invitrogen), followed by CD3+ and subsequently on CD4+ cells. A. CD4+ cells were further gated based on the expression of CD25 and CD127 to identify Tr1 (CD4+CD25−CD127−) and iTreg (CD4+CD25+CD127low/−) populations. B–C. Percentage of Tr1 cells on day two and eight respectively, D–E. Percentage of iTreg cells on day two and eight respectively. Data were analysed by the Mann-Whitney test, and levels of significance are indicated by P values.
On day 2, a significant increase in Tr1 cells was noted in PBMC culture in response to SbS-LD (SbS-LD-PBMC) or SbR-LD (SbR-LD-PBMC). In the latter case the response was significantly higher as compared to former ( Figure 3B ). However, there was low but significant increase in Tr1 cells was noted regardless of input parasites on day 8 ( Figure 3C ). The frequencies of iTreg cells on day 2, in SbS-LD-PBMC or in SbR-LD-PBMC, were essentially similar as observed in the case of Tr1 cells ( Figure 3D ). However, there was a significant increase in iTreg cells in SbS-LD-PBMC and SbR-LD-PBMC on day 8 as compared to normal but the SbR-LD triggered significantly higher frequency of iTregs than the SbS-LD ( Figure 3E ).
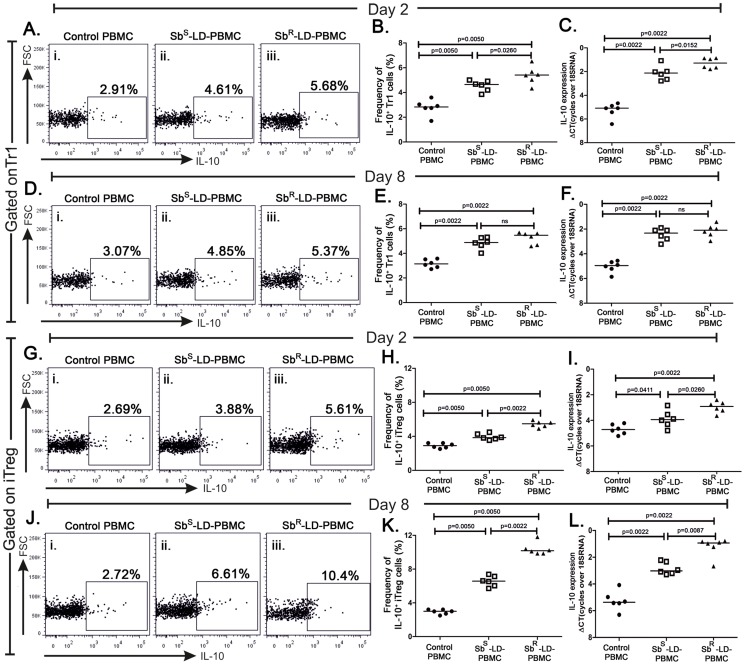
Frequencies of IL-10 producing Tr1 and iTreg cells
The frequencies of IL-10 producing Tr1 cells (IL10+ Tr1) and iTreg (IL-10+ iTreg) in SbR-LD-PBMC and SbS-LD-PBMC were enumerated. In general, the frequencies of such cells in both the compartments increased significantly regardless of input parasites as compared to their respective controls ( Figure 4A–L ). There is low but significant difference in IL-10+ Tr1 cells between SbS-LD-PBMC and SbR-LD-PBMC on day 2 ( Figure 4A–C ). But on day 8, difference in IL10+ Tr1 cells between SbS-LD-PBMC and SbR-LD-PBMC cannot be seen ( Figure 4D–F ). On the other hand, there was a significant difference in IL-10+ iTreg between SbS-LD-PBMC and SbR-LD-PBMC which was higher in later case in both the time points ( Figure 4G–L ). Most interestingly, there is a remarkable difference in IL-10+ iTreg between SbS-LD-PBMC and SbR-LD-PBMC where frequency was much higher in the latter case ( Figure 4J–L ) on day 8. The results observed by flow cytometry analysis were corroborated well with the quantitative PCR data for IL-10 signal ( Figure 4C, F, I, L ).
Figure 4. IL-10 producing Tr1 and iTReg cells are induced in response to SbS and SbR-LD.
Percentages of IL-10 producing Tr1 and iTreg cells from SbS-LD-PBMC and SbR-LD-PBMC at early and late time point are represented. A, B. Percentage of IL10+Tr1 cells on day two, C. Real-Time RTPCR of IL-10 mRNA level in sorted population of Tr1 cells on day two. D, E. Percentage of IL10+Tr1 cells on day eight, F. Real-Time RTPCR of IL-10 mRNA level in sorted population of Tr1 cells on day eight. G, H. Percentage of IL10+iTreg cells on day two, I. Real-Time RTPCR of IL-10 mRNA level in sorted population of iTeg cells on day two. J, K. Percentage of IL10+iTreg cells on day eight, L. Real-Time RTPCR of IL-10 mRNA level in sorted population of iTreg cells on day eight. Dot plots indicate one representative data set. Data were analyzed by the Mann-Whitney test, and levels of significance are indicated by P values.
iTreg cells from SbRLD driven PBMC show profound suppressive ability
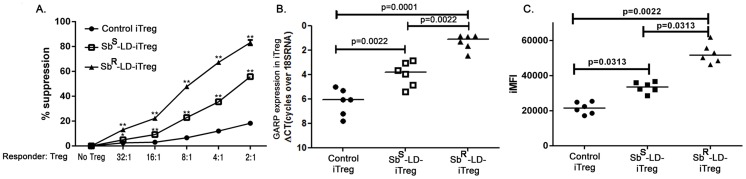
To assess their suppressive ability, if any, sorted iTreg cells derived from day 8 culture were co-cultured with freshly isolated autologous PBMCs as responders, in the presence of anti-CD3 and anti-CD28 beads. It was observed that T-cell proliferation decreased as a function of iTreg number and maximum suppression was achieved at a ratio of 2∶1 (responder : iTreg) ( Figure 5A ). The iTregs isolated from SbR-LD-PBMC showed about 80% suppression whereas similar iTregs from SbS-LD-PBMC showed about 55% suppression. In contrast, iTregs derived from normal subjects only minimally suppressed the proliferation of responder cells ( Figure 5A ).
Figure 5. Isolated iTregs are active and shows pronounced suppressive ability.
A. Percentage suppression analysed after co-culturing isolated iTreg cells (described earlier) at day eight with autologous freshly isolated PBMC at different Treg: responder ratio. Expression of GARP/LRRC32 in iTreg cells. B. mRNA expression level of LRRC32 gene in sorted iTreg cells with median values indicated and C. iMFI values was calculated by multiplying the frequency of GARP protein expressing iTregs and their mean fluorescence intensity. Data were analyzed by the Mann-Whitney test, and levels of significance are indicated by P values. Groups SbS-iTreg and SbR-iTreg were compared to control iTregs. “*” indicates 0.0001<P<0.05 and “**” indicates P<0.0001.
In human, expression of a transmembrane protein, glycoprotein A repetitions predominant (GARP or LRRC32) selectively identifies activated T-regulatory cells [28]. We measured the surface expression of GARP in iTreg cells in SbR-LD-PBMC and SbS-LD-PBMC on day 8. When GARP expression was monitored in the iTregs at the mRNA level, substantial difference was detected between SbS-LD-PBMC and SbR-LD-PBMC ( Figure 5B ). Frequency of GARP expressing iTreg cells and the level of its expression was taken into account when calculating iMFI (integrated MFI) values. It displays that iMFI values for GARP expressing iTreg cells are noticeably higher in SbR-LD-PBMC compared to SbS-LD-PBMC samples ( Figure 5C ).
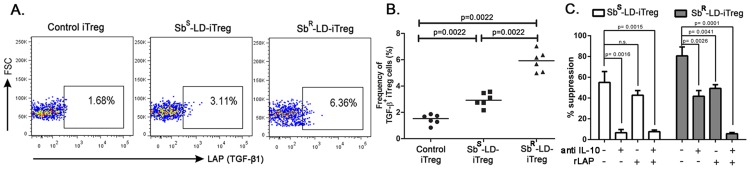
Induced T regulatory cells (iTreg) mediates suppression in a IL-10 and TGF-β dependent manner in Sb-R infection
We investigated expression of cell surface LAP/TGF-β1 in LD infection, as GARP in activated Treg is known to remain associated with it. We were able to detect membrane bound LAP/TGF-β1 in iTreg cells. The percentage of LAP/TGF-β1+ iTreg cells being significantly higher in SbR-LD-PBMC (Median 5.925%) in contrast to SbS-LD-PBMC (Median 2.925%) ( Figure 6A, B ).
Figure 6. iTReg from SbR-LD-PBMC mediates their suppressive activity through IL-10 and TGF- β.
Percentages of rLAP (TGF-β1) containing iTreg cells from SbS-LD-PBMC and SbR-LD-PBMC at day eight are represented. A, B. Percentage of LAP (TGF-β1)+ iTreg cells on day eight. Pseudo colour plot indicate one representative data set. C. Suppression assay in presence of neutralizing IL-10 antibody and/or rLAP. Data were analysed by Mann-Whitney test and two-tailed paired student t test, and levels of significance are indicated by P values.
Based on the fact that iTreg of SbR-LD-PBMC expressed both IL-10 and TGF-β, we endeavoured to study the effects of neutralizing/blocking antibodies to above mentioned cytokines on the iTreg mediated suppression of T-cell repertoire at day 8. It was observed that the presence of anti-IL-10 antibody alone almost abolishes the suppressive function of iTreg from SbS-LD-PBMC ( Figure 6C ). Exactly identical experiment was performed with iTreg from SbR-LD-PBMC. Here, addition of anti-IL-10 induced about 50% inhibitions whereas; recombinant human LAP (rLAP), which neutralizes active TGF-β1, induced about 45% inhibition of iTreg's suppressive capacity. Addition of combination of anti-IL-10 and rLAP led to complete inhibition of these iTreg's suppressive ability ( Figure 6C ). It is to note that apart from TGF-β1, the rLAP can also neutralize other active isoforms of TGF-β. Hence involvement of other isoforms of TGF-β cannot be ruled out.
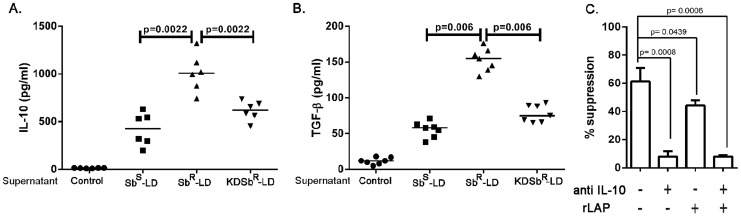
Role of surface glycans in differential immune modulation
Our group earlier showed that expression of a unique glycan with N-acetylgalactosamine as a terminal sugar on SbR-LD plays an important part in up-regulation of IL-10 and MDR1 in infected macrophages and removal of this glycan makes this parasite to behave like their antimony sensitive counterpart [21]. Here by using the galactosyl transferase knock down parasite (KD-SbR-LD) we got the level of IL-10 almost close to the amount we observed in infection with SbS-LD ( Figure 7A ), which indicates towards a possible role of this glycan in the observed differential immune response. Our earlier experiments showed that rLAP reverses the suppressive effect of iTReg cells from SbR-LD-PBMC. Here; we acid neutralize the culture supernatant and measured the TGF-β from culture supernatants by ELISA at day 8. Our results showed that SbR-LD driven PBMC culture supernatants produced higher level of TGF-β compared to that of SbS-LD driven PBMC culture supernatants but the production of TGF-β from knock down parasite (KD- SbR-LD driven PBMC culture supernatants) was considerably low and was comparable to SbS-supernatant ( Figure 7B ). Next we did the same suppression assay performed earlier by isolating iTreg from KD-SbR-LD infection and addition of neutralizing IL-10 alone abolished the suppressive activity compared to that of iTreg from wild type SbR-LD-PBMC ( Figure 7C ).
Figure 7. GalT Knock down parasites (KDSbR-LD) behaves like SbS-LD isolates.
A. Production of IL-10, B. TGF-β from KDSbR, SbS and SbR-Sup. For TGF-β measurement the culture supernatants were acidified followed by neutralization, the level of TGF-β was measured by ELISA. C. Suppression assay performed in presence of neutralizing IL-10 antibody and/or rLAP using iTreg from KDSbR-LD-PBMC at day eight. Data were analysed by Mann-Whitney test and two-tailed paired Student t test, and levels of significance are indicated by P values.
Another important thing to consider is the level of infection induced by these parasites in human PBMC. For that we set up the same experiment on a coverglass. On day 2 and day 8 we measured the level of infection in the adherent cells. We found that there was hardly any difference in the level of infection between SbS-LD, SbR-LD and KD-SbR-LD though the median values indicated a slightly higher level of infection load in the case of SbR-LD infection (Figure S1).
Discussion
There is very little information available about the early immune responses (first few days) when human host is infected with L. donovani. We adopted an approach proposed by Rogers et al that allows us to study such interactions over a defined period of time in an in vitro setting [29], [30]. We did this study with both SbS and SbR-LD isolates; it allowed us to dissect the differences in their immune modulation capacity during their interaction with the host PBMCs. Infectious dose of the parasite transmitted by the sand flies varies considerably [31]–[33], so choosing an inoculums size was a challenging task. We used opsonised live LD parasite (approximate parasite to monocyte ratio, 1∶1) to get as closely as possible to the in vivo scenario in human [29], [34], as reports suggests that the response of PBMC's to dead versus live parasites differs significantly [35]. These studies are not possible with the PBMCs from Leishmania infected, cured or exposed individuals, as we are unaware about the time of infection, dose, frequency or sometimes also the species of the parasites [29], [30], [36]. If we use PBMCs from these study subjects, then the immune response will be more close to secondary immune response [29], [30]. It is noteworthy that use of PBMCs from asymptomatic individuals would have been interesting. A high incidence of asymptomatic cases indicates that many individuals are indeed capable of mounting effective immune response to keep Leishmania infection in check. Prognosis of individual markers responsible for asymptomatic infection at individual level is still lacking. There are reports that unlike individuals with active disease, PBMCs from some of the asymptomatic individuals indeed respond to antigens of L. chagasi with proliferative response and secretion of cytokines such as IL-2, IFN-γ and IL-12 which are implicated in anti-leishmanial response. Also level of disease promoting cytokine IL-10 following L. chagasi antigen encounter remains lower in asymptomatic individuals compared to patients with active pathology [37], [38]. Earlier reports showed that following stimulation of whole-blood with L. donovani soluble Leishmania antigen (SLA), cells from individuals with active disease responds by secretion of both IFN-γ and IL-10 but asymptomatic individuals do not produce the disease promoting IL-10 [39].
Diverse reports exist about the source of IL-10 in Leishmania infection. There is a lot of discrepancy about the source of IL-10 in various previous studies with VL patients or using murine model. In a non-healing mouse model of Leishmaniasis, high frequency of IL-10 producing regulatory T cells (CD4+CD25+FoxP3+) is observed at local site [9]. Recent study by Nylen et al, 2007 has evidently shown the IL-10 mediated suppression of immunity among patients suffering from VL [19]. However, in a subsequent study the source of IL-10 among VL patient was identified as CD25−FoxP3− cells, not the CD25+FoxP3+ Treg cells as presumed on the basis of data obtained from some studies [18]. Regulatory T-cells are part of body's physiologic regulatory mechanisms used by the immune system to maintain homeostasis for preventing autoimmunity and temper inflammation after infection or injury [15].T-regulatory cells are considered to be pivotal mediators of peripheral tolerance and immune suppression [15]. Our studies revealed the role played by different T-regulatory cells during early interactions of host with SbR-LD and SbS-LD parasites. CD4+CD25−CD127− Tr1 cells produce IL-10 and are constant source of IL-10 at both early and late time point. Increase in the level of IL-27 in interactions with both SbS-LD and SbR-LD isolates correlates with the generation of IL-10 producing Tr1 cells (Figure S2). But interestingly the percentage of CD4+CD25+CD127low/− iTreg cells increases at late time point in SbR-LD infection and these cells also contributes to IL-10 production considerably. SbS-LD infections also result in production of IL-10 from iTreg cells but not to same extent. Earlier studies from our group have shown that SbR-LD infection generates more IL-10 from both macrophages and dendritic cells [16], [17]. Verreck et al. reported the existence of different macrophage population derived from same CD14+ monocytic lineage [40], one such population produces high levels of IL-10 and has a capacity to induce differentiation of T regulatory cells [41]. These reports and our observation indicate a possible role of these anti-inflammatory macrophages in the induction of Treg cell during SbR-LD infection. Walther et al reported that there is a strong co-relation between rapid growths of virulent strains of malaria with increase in the frequency of CD4+CD25+CD127low/− T regulatory cells [42]. Generation of iTreg cells or expansion of nTreg cells with concomitant IL-10 production in SbR-LD infection may be one of reasons behind the persistence of Treg cells even after successful chemotherapy as reported by Rai et al [13]. Many chronic infections are associated with this increase in Treg cell numbers [43], [44]. Presence of these Treg cells during these infections becomes an important barrier for any vaccination or other treatment strategies [45]. A successful vaccine against Leishmaniasis is still elusive despite several recent encouraging reports [46]–[48] and success of such vaccine depends on the IL-10 production by Treg cells [49]. Presence of Treg cells and associated IL-10 production is reported in reactivation of disease in the form of PKDL [50].
We have shown here that these iTreg cells are capable of suppressing the proliferation of autologous cells. Enhanced suppressive ability of the iTreg cells isolated from SbR-LD infection emphasizes the role played by these cells in the suppression of effector T cells in drug-unresponsive cases. Reports suggest that activated T regulatory cells express a surface molecule called glycoprotein A repetitions predominant (GARP) [51].Our data confirms the upregulation of this activation marker in the iTreg cells from SbR-LD infection, which further substantiates the suppressive role of these active iTreg cells in SbR-LD infection.
T-regulatory cells exert their suppressive function in many ways, by secreting soluble factors, in contact dependent manner or by quenching growth factors [52]. SbR-LD infection enhances IL-10 production indicating its importance in observed immune suppression. But addition of neutralizing IL-10 can't rescue the suppressive effect of iTreg cells from SbR-LD-PBMC. GARP acts as a receptor for membrane bound TGF-β in activated Tregs [53]. This prompts us to check whether TGF-β also has some role in this immune suppression. Addition of rLAP, which binds to TGF-β1 together with anti-IL-10, does rescue the suppressive effect of iTreg from SbR-LD-PBMC. On the other hand addition of neutralizing IL-10 alone can almost entirely inhibit suppressive effect of iTreg isolated from SbS-LD-PBMC. Higher level of TGF-β from acid neutralized SbR-supernatant and higher expression of surface bound TGF-β in iTreg isolated from SbS-LD-PBMC proves the association of IL-10 and TGF-β in the iTreg mediated immune suppression in SbR-LD infection. Activated Treg cells induce the differentiation of naïve cells to FoxP3+ Treg cells in a TGF-β-dependent cell contact-dependent manner [54].The continuous generation of suppressive iTreg cells in SbR-LD infection may be responsible for greater immune-suppression and persistence of the parasite after successful chemotherapy. The terminal sugar residue N-acetylgalactosamine present on the surface of SbR-LD may have some role in their differential immune response as knocking down of galactosyl transferase enzyme, which adds these residues, reverses this differential immune response and SbR-LD behaves like their sensitive counterpart as shown by us in our earlier studies [21] and in this present study. Furthermore previous study with KD-SbR-LD parasites resulted in significantly less parasite burden in BALB/c mice compared to infection induced by SbR-LD [21]. It is a well-known fact that glycans can interact with dendritic cells/macrophages to produce cytokines that can modulate T-cell response [55], [56]. But in our case, actually how the surface glycoprotein affects the antigen presenting cells to induce differential T-cell response needs further careful and thorough investigation. Our earlier report showed that the SbR-LD isolates expressed surface glycoconjugates with a terminal sugar N-acetyl-D-galactosaminyl residue, which was almost absent in SbS-LD [21]. The induction of more potent iTregs secreting both IL-10 and TGF-β as effectors by SbR-LD parasites was abrogated in case of KD-SbR -LD driven iTregs, as reported in this work. These results further establish that the terminal sugar present in the SbR-LD isolates is one of the key components responsible for differential immune-modulation following interaction with human PBMCs. Earlier reports suggest that SbR-LD infection may lead to greater infection load and more aggressive disease pathology [57]. But this observed differential immune-modulation is completely an intrinsic property of SbR-LD which is evident from the fact that KD-SbR-LD parasites behaves like their sensitive counterpart by virtue of losing its surface glycoconjugates with terminal sugar N-acetyl-D-galactosaminyl residue. But our observations do not exclude the possibility of other parasite derived factors that may contribute to differential immune modulation capacity of SbR-LD parasites. Further characterization of the nature of the glycoconjugate is needed to understand the specific interaction with host immune system components.
There are other studies that establishes role of regulatory DCs in the induction of IL-10 from Th1 cells [58], [59], but the mechanism behind potent iTreg induction by SbR-LD, remains under further investigation. This study allowed us for controlled experimentation and exploration of specific immune responses elicited by SbR-LD infection which is difficult to achieve in actual human VL patients. The early infection process involves interaction of human immune system, the parasites themselves, promastigote secretory gel (PSG) [60] and the complex sand fly saliva with more than 50 active peptides and other components [61], [62]. This presents an enormous challenge for the researchers to dissect the role of the isolated individual players in this process and even more so, how these individual components interact with each other during natural infection process. Our in vitro system cannot address this bewildering complexity of natural infection process and may not exactly mimic the in vivo scenario. Studies with natural sand fly mediated infection cannot be extended to humans and we need to keep in mind the doubtful predictive value of animal models. In this context our work focuses on one isolated part of the early infection process when low inoculum of parasites interact with PBMCs with the emphasis on the differences in the intrinsic immune-modulation properties of pentavalent antimonial (Sb) sensitive and resistant L. donovani isolates. This may be one piece of the puzzle when it comes to the biology of Sb sensitive and resistant parasites and surely there are other components that are involved in the early infection process during natural transmission. Despite limitations of this model, it demonstrates how only a small number of parasites have potent immune-modulatory effect and can influence the local cytokine environment to suppress anti-parasitic activity; with drug resistant parasites having greater immune-modulation capacity. This knowledge about the immune-suppressive mechanisms associated with LD infection may allow us to design a more potent therapeutic approach to treat this dreaded disease.
Supporting Information
Similar parasite burden pattern in SbS and SbR-LD-PBMCs. The amount of percent infected adherent cells and number of amastigotes per hundred adherent cells were almost similar in both SbS and SbR-LD-PBMCs (A,B,C and D). Freshly isolated PBMCs were incubated with SbS and SbR-LD isolates on coverglass and after day two and day eight, coverglasses were washed, fixed with methanol and stained with Giemsa. The numbers of parasites in the adherent cells were enumerated after observing under light microscope. Data were analysed by Mann-Whitney test, and levels of significance are indicated by P values.
(TIF)
Both SbS and SbR-LD infection results in enhanced IL-27 production. Level of IL-27 measured at early and late time point of interaction. Freshly isolated PBMCs were incubated with SbS and SbR-LD isolates and after day two and day eight, culture supernatants (SbS and SbR-sup) were collected and level of IL-27 was measured by ELISA. Median values were indicated (n = 10). Data were analysed by the Mann-Whitney test, and levels of significance are indicated by P values.
(TIF)
Acknowledgments
We want to thank Late Dr. Richard Titus, whose encouraging advice helped us to design the project. We would also like to acknowledge Mr. Surjendu Bikash Debnath for his technical help. We want to thank all the volunteers without whom the present project wouldn't have been completed.
Funding Statement
This research was supported by the European Commission-funded Kaladrug-R Project (Health-F3-2008-222895) and the Council of Scientific and Industrial Research (grant no. BSC-0114 and BSC-0120), New Delhi. Fellowships from the CSIR, Government of India was awarded to RG, SD, and JG. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Croft SL, Sundar S, Fairlamb AH (2006) Drug resistance in leishmaniasis. Clin Microbiol Rev 19: 111–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sundar S, Chatterjee M (2006) Visceral leishmaniasis - current therapeutic modalities. Indian J Med Res 123: 345–352. [PubMed] [Google Scholar]
- 3. Vanaerschot M, Decuypere S, Downing T, Imamura H, Stark O, et al. (2012) Genetic markers for SSG resistance in Leishmania donovani and SSG treatment failure in visceral leishmaniasis patients of the Indian subcontinent. J Infect Dis 206: 752–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Awasthi A, Mathur RK, Saha B (2004) Immune response to Leishmania infection. Indian J Med Res 119: 238–258. [PubMed] [Google Scholar]
- 5. Biedermann T, Zimmermann S, Himmelrich H, Gumy A, Egeter O, et al. (2001) IL-4 instructs TH1 responses and resistance to Leishmania major in susceptible BALB/c mice. Nat Immunol 2: 1054–1060. [DOI] [PubMed] [Google Scholar]
- 6. Thakur CP, Mitra DK, Narayan S (2003) Skewing of cytokine profiles towards T helper cell type 2 response in visceral leishmaniasis patients unresponsive to sodium antimony gluconate. Trans R Soc Trop Med Hyg 97: 409–412. [DOI] [PubMed] [Google Scholar]
- 7. Chakraborty D, Banerjee S, Sen A, Banerjee KK, Das P, et al. (2005) Leishmania donovani affects antigen presentation of macrophage by disrupting lipid rafts. J Immunol 175: 3214–3224. [DOI] [PubMed] [Google Scholar]
- 8. Meier CL, Svensson M, Kaye PM (2003) Leishmania-induced inhibition of macrophage antigen presentation analyzed at the single-cell level. J Immunol 171: 6706–6713. [DOI] [PubMed] [Google Scholar]
- 9. Mendez S, Reckling SK, Piccirillo CA, Sacks D, Belkaid Y (2004) Role for CD4(+) CD25(+) regulatory T cells in reactivation of persistent leishmaniasis and control of concomitant immunity. J Exp Med 200: 201–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alexander J, Brombacher F (2012) T helper1/t helper2 cells and resistance/susceptibility to leishmania infection: is this paradigm still relevant? Front Immunol 3: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liew FY (1989) Functional heterogeneity of CD4+ T cells in leishmaniasis. Immunol Today 10: 40–45. [DOI] [PubMed] [Google Scholar]
- 12. Belkaid Y, Piccirillo CA, Mendez S, Shevach EM, Sacks DL (2002) CD4+CD25+ regulatory T cells control Leishmania major persistence and immunity. Nature 420: 502–507. [DOI] [PubMed] [Google Scholar]
- 13. Rai AK, Thakur CP, Singh A, Seth T, Srivastava SK, et al. (2012) Regulatory T cells suppress T cell activation at the pathologic site of human visceral leishmaniasis. PLoS One 7: e31551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Curotto de Lafaille MA, Lafaille JJ (2009) Natural and adaptive foxp3+ regulatory T cells: more of the same or a division of labor? Immunity 30: 626–635. [DOI] [PubMed] [Google Scholar]
- 15. Facciabene A, Motz GT, Coukos G (2012) T-regulatory cells: key players in tumor immune escape and angiogenesis. Cancer Res 72: 2162–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mukhopadhyay R, Mukherjee S, Mukherjee B, Naskar K, Mondal D, et al. (2011) Characterisation of antimony-resistant Leishmania donovani isolates: biochemical and biophysical studies and interaction with host cells. Int J Parasitol 41: 1311–1321. [DOI] [PubMed] [Google Scholar]
- 17. Haldar AK, Yadav V, Singhal E, Bisht KK, Singh A, et al. (2010) Leishmania donovani isolates with antimony-resistant but not -sensitive phenotype inhibit sodium antimony gluconate-induced dendritic cell activation. PLoS Pathog 6: e1000907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nylen S, Maurya R, Eidsmo L, Manandhar KD, Sundar S, et al. (2007) Splenic accumulation of IL-10 mRNA in T cells distinct from CD4+CD25+ (Foxp3) regulatory T cells in human visceral leishmaniasis. J Exp Med 204: 805–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nylen S, Sacks D (2007) Interleukin-10 and the pathogenesis of human visceral leishmaniasis. Trends Immunol 28: 378–384. [DOI] [PubMed] [Google Scholar]
- 20. Aslan H, Dey R, Meneses C, Castrovinci P, Jeronimo SM, et al. (2013) A new model of progressive visceral leishmaniasis in hamsters by natural transmission via bites of vector sand flies. J Infect Dis 207: 1328–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mukherjee B, Mukhopadhyay R, Bannerjee B, Chowdhury S, Mukherjee S, et al. (2013) Antimony-resistant but not antimony-sensitive Leishmania donovani up-regulates host IL-10 to overexpress multidrug-resistant protein 1. Proc Natl Acad Sci U S A 110: E575–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bosque F, Saravia NG, Valderrama L, Milon G (2000) Distinct innate and acquired immune responses to Leishmania in putative susceptible and resistant human populations endemically exposed to L. (Viannia) panamensis infection. Scand J Immunol 51: 533–541. [DOI] [PubMed] [Google Scholar]
- 23. Samant M, Gupta R, Kumari S, Misra P, Khare P, et al. (2009) Immunization with the DNA-encoding N-terminal domain of proteophosphoglycan of Leishmania donovani generates Th1-type immunoprotective response against experimental visceral leishmaniasis. J Immunol 183: 470–479. [DOI] [PubMed] [Google Scholar]
- 24. Rama Iniguez S, Dea-Ayuela MA, Sanchez-Brunete JA, Torrado JJ, Alunda JM, et al. (2006) Real-time reverse transcription-PCR quantification of cytokine mRNA expression in golden Syrian hamster infected with Leishmania infantum and treated with a new amphotericin B formulation. Antimicrob Agents Chemother 50: 1195–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Perez-Victoria JM, Perez-Victoria FJ, Parodi-Talice A, Jimenez IA, Ravelo AG, et al. (2001) Alkyl-lysophospholipid resistance in multidrug-resistant Leishmania tropica and chemosensitization by a novel P-glycoprotein-like transporter modulator. Antimicrob Agents Chemother 45: 2468–2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Saha S, Mondal S, Ravindran R, Bhowmick S, Modak D, et al. (2007) IL-10- and TGF-beta-mediated susceptibility in kala-azar and post-kala-azar dermal leishmaniasis: the significance of amphotericin B in the control of Leishmania donovani infection in India. J Immunol 179: 5592–5603. [DOI] [PubMed] [Google Scholar]
- 27. Liu W, Putnam AL, Xu-Yu Z, Szot GL, Lee MR, et al. (2006) CD127 expression inversely correlates with FoxP3 and suppressive function of human CD4+ T reg cells. J Exp Med 203: 1701–1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wang R, Kozhaya L, Mercer F, Khaitan A, Fujii H, et al. (2009) Expression of GARP selectively identifies activated human FOXP3+ regulatory T cells. Proc Natl Acad Sci U S A 106: 13439–13444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rogers KA, Titus RG (2004) Characterization of the early cellular immune response to Leishmania major using peripheral blood mononuclear cells from Leishmania-naive humans. Am J Trop Med Hyg 71: 568–576. [PubMed] [Google Scholar]
- 30. Rogers KA, Titus RG (2004) The human cytokine response to Leishmania major early after exposure to the parasite in vitro. J Parasitol 90: 557–563. [DOI] [PubMed] [Google Scholar]
- 31. Kimblin N, Peters N, Debrabant A, Secundino N, Egen J, et al. (2008) Quantification of the infectious dose of Leishmania major transmitted to the skin by single sand flies. Proc Natl Acad Sci U S A 105: 10125–10130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Maia C, Seblova V, Sadlova J, Votypka J, Volf P (2011) Experimental transmission of Leishmania infantum by two major vectors: a comparison between a viscerotropic and a dermotropic strain. PLoS Negl Trop Dis 5: e1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rogers ME, Corware K, Muller I, Bates PA (2010) Leishmania infantum proteophosphoglycans regurgitated by the bite of its natural sand fly vector, Lutzomyia longipalpis, promote parasite establishment in mouse skin and skin-distant tissues. Microbes Infect 12: 875–879. [DOI] [PubMed] [Google Scholar]
- 34. Diaz YR, Rojas R, Valderrama L, Saravia NG (2010) T-bet, GATA-3, and Foxp3 expression and Th1/Th2 cytokine production in the clinical outcome of human infection with Leishmania (Viannia) species. J Infect Dis 202: 406–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nylen S, Mortberg U, Kovalenko D, Satti I, Engstrom K, et al. (2001) Differential induction of cellular responses by live and dead Leishmania promastigotes in healthy donors. Clin Exp Immunol 124: 43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hviid L, Sorensen AL, Kharazmi A, Theander TG (1990) Functional and phenotypic changes in human lymphocytes after coincubation with Leishmania donovani in vitro. Infect Immun 58: 3163–3167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Costa SR, D'Oliveira A Jr, Bacellar O, Carvalho EM (1999) T cell response of asymptomatic Leishmania chagasi infected subjects to recombinant leishmania antigens. Mem Inst Oswaldo Cruz 94: 367–370. [DOI] [PubMed] [Google Scholar]
- 38. White AC Jr, Castes M, Garcia L, Trujillo D, Zambrano L (1992) Leishmania chagasi antigens recognized in cured visceral leishmaniasis and asymptomatic infection. Am J Trop Med Hyg 46: 123–131. [DOI] [PubMed] [Google Scholar]
- 39. Singh OP, Gidwani K, Kumar R, Nylen S, Jones SL, et al. (2012) Reassessment of immune correlates in human visceral leishmaniasis as defined by cytokine release in whole blood. Clin Vaccine Immunol 19: 961–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Verreck FA, de Boer T, Langenberg DM, Hoeve MA, Kramer M, et al. (2004) Human IL-23-producing type 1 macrophages promote but IL-10-producing type 2 macrophages subvert immunity to (myco)bacteria. Proc Natl Acad Sci U S A 101: 4560–4565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Savage ND, de Boer T, Walburg KV, Joosten SA, van Meijgaarden K, et al. (2008) Human anti-inflammatory macrophages induce Foxp3+ GITR+ CD25+ regulatory T cells, which suppress via membrane-bound TGFbeta-1. J Immunol 181: 2220–2226. [DOI] [PubMed] [Google Scholar]
- 42. Walther M, Tongren JE, Andrews L, Korbel D, King E, et al. (2005) Upregulation of TGF-beta, FOXP3, and CD4+CD25+ regulatory T cells correlates with more rapid parasite growth in human malaria infection. Immunity 23: 287–296. [DOI] [PubMed] [Google Scholar]
- 43. Li S, Gowans EJ, Chougnet C, Plebanski M, Dittmer U (2008) Natural regulatory T cells and persistent viral infection. J Virol 82: 21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Peng G, Li S, Wu W, Sun Z, Chen Y, et al. (2008) Circulating CD4+ CD25+ regulatory T cells correlate with chronic hepatitis B infection. Immunology 123: 57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Nasser R, Pelegrin M, Plays M, Gros L, Piechaczyk M (2013) Control of regulatory T cells is necessary for vaccine-like effects of antiviral immunotherapy by monoclonal antibodies. Blood 121: 1102–1111. [DOI] [PubMed] [Google Scholar]
- 46. Guha R, Das S, Ghosh J, Naskar K, Mandala A, et al. (2013) Heterologous priming-boosting with DNA and vaccinia virus expressing kinetoplastid membrane protein-11 induces potent cellular immune response and confers protection against infection with antimony resistant and sensitive strains of Leishmania (Leishmania) donovani. Vaccine 31: 1905–1915. [DOI] [PubMed] [Google Scholar]
- 47. Guha R, Gupta D, Rastogi R, Vikram R, Krishnamurthy G, et al. (2013) Vaccination with leishmania hemoglobin receptor-encoding DNA protects against visceral leishmaniasis. Sci Transl Med 5: 202ra121. [DOI] [PubMed] [Google Scholar]
- 48. Alvar J, Croft SL, Kaye P, Khamesipour A, Sundar S, et al. (2013) Case study for a vaccine against leishmaniasis. Vaccine 31 Suppl 2: B244–249. [DOI] [PubMed] [Google Scholar]
- 49. Stober CB, Lange UG, Roberts MT, Alcami A, Blackwell JM (2005) IL-10 from regulatory T cells determines vaccine efficacy in murine Leishmania major infection. J Immunol 175: 2517–2524. [DOI] [PubMed] [Google Scholar]
- 50. Katara GK, Ansari NA, Verma S, Ramesh V, Salotra P (2011) Foxp3 and IL-10 expression correlates with parasite burden in lesional tissues of post kala azar dermal leishmaniasis (PKDL) patients. PLoS Negl Trop Dis 5: e1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Battaglia M, Roncarolo MG (2009) The Tregs' world according to GARP. Eur J Immunol 39: 3296–3300. [DOI] [PubMed] [Google Scholar]
- 52. Maloy KJ, Powrie F (2001) Regulatory T cells in the control of immune pathology. Nat Immunol 2: 816–822. [DOI] [PubMed] [Google Scholar]
- 53. Stockis J, Colau D, Coulie PG, Lucas S (2009) Membrane protein GARP is a receptor for latent TGF-beta on the surface of activated human Treg. Eur J Immunol 39: 3315–3322. [DOI] [PubMed] [Google Scholar]
- 54. Nakamura K, Kitani A, Strober W (2001) Cell contact-dependent immunosuppression by CD4(+)CD25(+) regulatory T cells is mediated by cell surface-bound transforming growth factor beta. J Exp Med 194: 629–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. van Vliet SJ, Garcia-Vallejo JJ, van Kooyk Y (2008) Dendritic cells and C-type lectin receptors: coupling innate to adaptive immune responses. Immunol Cell Biol 86: 580–587. [DOI] [PubMed] [Google Scholar]
- 56. Kapsenberg ML (2003) Dendritic-cell control of pathogen-driven T-cell polarization. Nat Rev Immunol 3: 984–993. [DOI] [PubMed] [Google Scholar]
- 57. Vanaerschot M, De Doncker S, Rijal S, Maes L, Dujardin JC, et al. (2011) Antimonial resistance in Leishmania donovani is associated with increased in vivo parasite burden. PLoS One 6: e23120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Resende M, Moreira D, Augusto J, Cunha J, Neves B, et al. (2013) Leishmania-infected MHC class IIhigh dendritic cells polarize CD4+ T cells toward a nonprotective T-bet+ IFN-gamma+ IL-10+ phenotype. J Immunol 191: 262–273. [DOI] [PubMed] [Google Scholar]
- 59. Owens BM, Beattie L, Moore JW, Brown N, Mann JL, et al. (2012) IL-10-producing Th1 cells and disease progression are regulated by distinct CD11c(+) cell populations during visceral leishmaniasis. PLoS Pathog 8: e1002827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Rogers M, Kropf P, Choi BS, Dillon R, Podinovskaia M, et al. (2009) Proteophosophoglycans regurgitated by Leishmania-infected sand flies target the L-arginine metabolism of host macrophages to promote parasite survival. PLoS Pathog 5: e1000555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ready PD (2013) Biology of phlebotomine sand flies as vectors of disease agents. Annu Rev Entomol 58: 227–250. [DOI] [PubMed] [Google Scholar]
- 62. Gomes R, Oliveira F (2012) The immune response to sand fly salivary proteins and its influence on leishmania immunity. Front Immunol 3: 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Similar parasite burden pattern in SbS and SbR-LD-PBMCs. The amount of percent infected adherent cells and number of amastigotes per hundred adherent cells were almost similar in both SbS and SbR-LD-PBMCs (A,B,C and D). Freshly isolated PBMCs were incubated with SbS and SbR-LD isolates on coverglass and after day two and day eight, coverglasses were washed, fixed with methanol and stained with Giemsa. The numbers of parasites in the adherent cells were enumerated after observing under light microscope. Data were analysed by Mann-Whitney test, and levels of significance are indicated by P values.
(TIF)
Both SbS and SbR-LD infection results in enhanced IL-27 production. Level of IL-27 measured at early and late time point of interaction. Freshly isolated PBMCs were incubated with SbS and SbR-LD isolates and after day two and day eight, culture supernatants (SbS and SbR-sup) were collected and level of IL-27 was measured by ELISA. Median values were indicated (n = 10). Data were analysed by the Mann-Whitney test, and levels of significance are indicated by P values.
(TIF)