Abstract
Defining the proper geographic scale for built environment exposures continues to present challenges. In this study, size attributes and exposure calculations from two commonly used neighborhood boundaries were compared to those from neighborhoods that were self-defined by a sample of 145 urban minority adolescents living in subsidized housing estates. Associations between five built environment exposures and physical activity, overweight and obesity were also examined across the three neighborhood definitions. Limited spatial overlap was observed across the various neighborhood definitions. Further, many places where adolescents were active were not within the participants’ neighborhoods. No statistically significant associations were found between counts of facilities and the outcomes based on exposure calculations using the self-defined boundaries; however, a few associations were evident for exposures using the 0.75 mile network buffer and census tract boundaries. Future investigation of the relationship between the built environment, physical activity and obesity will require practical and theoretically-based methods for capturing salient environmental exposures.
Keywords: Built environment, Physical activity, Obesity, Neighborhood, Geographic information system
Background
The number of research studies that examine the effect of the built environment (e.g., parks, walkability) on physical activity and obesity has increased dramatically in the past decade (Ding and Gebel, 2012). The majority of this research has focused on the role of the neighborhood environment (Feng et al., 2010). For example, a recent review of environmental correlates of cardio-metabolic risk factors (e.g., obesity, hypertension) found that 90% of the studies in the review examined the neighborhood environment exclusively (Leal and Chaix, 2011). The remaining 10% examined non-neighborhood environments, including school, worksite, and shopping environments sometimes in conjunction with neighborhood environments. Although the majority of studies consider the neighborhood environment, the definition of a neighborhood varies markedly across studies. In order to represent a neighborhood, researchers often use administrative boundaries such as census geography or a buffer drawn around the participant’s home. Buffers are usually constructed using a straight line (Euclidean buffer) or along roadways (Network buffer). Even within studies that use buffer boundaries, a large degree of variability exists for their dimensions. Radii as small as .25 miles (Jago et al., 2005) and as large as 5 miles (Gordon-Larsen et al., 2006) have been used. Despite the growing research attention in this area, little is known about whether an individual’s conceptualization of his or her neighborhood correlates with the neighborhood boundaries defined by research studies or the degree to which physical activity occurs within these ascribed areas, particularly for adolescents.
In fields such as urban sociology and environmental psychology, precedent exists for examining individually-defined neighborhood boundaries to understand the effect of neighborhood factors on various aspects of a resident’s life using cognitive maps (e.g., (Downs and Stea, 1973; Haney and Knowles, 1978)). However, few behavioral health studies have examined the degree to which individually-drawn neighborhood boundaries overlay commonly used boundaries. Furthermore, no published studies could be located that have examined multiple neighborhood boundaries, including self-defined neighborhood boundaries, and whether the use of these different definitions results in differential associations between the environment and physical activity and/or obesity in adolescents.
Several recent studies have suggested that there is a fair amount of variability in how adults from similar areas self-define their neighborhoods. For example, Coulton and colleagues found that residents of the same block group differed considerably in their neighborhood definitions (Coulton et al., 2001). Also, while the average resident-drawn neighborhood map was approximately the size of a census tract, typical resident maps contained portions of several census tracts around a given participant’s home rather than a complete single census tract. A replication of this methodology in 10 cities showed a similar lack of consensus concerning neighborhood boundaries among adult residents living in close proximity with regional variation in the size of resident-drawn maps (Coulton et al., 2011; Coulton et al., 2013).
Studies of how children spatially define their neighborhoods are less common than studies in adults, although a precedent exists for examining neighborhood boundaries based on the views of children and adolescents (Ladd, 1970; Maurer and Baxter, 1972). One recent study asked children, during a neighborhood walk, to define their neighborhood boundaries and the area in which they were allowed to walk alone or with a friend (Spilsbury et al., 2009). The children’s parents/guardians also drew neighborhood boundaries on a city map. The study found that children and parents had different conceptualizations of neighborhood boundaries. Children’s maps were on average 11% the size of the parent maps. Comparisons to commonly used neighborhood definitions were not described, although the mean square miles of the child’s neighborhood map was .11 (median .04), which, if symmetrical, would be roughly equivalent to a 0.2 mile Euclidean buffer. In another study of 55 older adolescents (15-19), adolescent self-drawn maps showed considerable variability in size and did not overlay census tract boundaries (Basta et al., 2010).
The use of multiple buffer sizes has also been proposed as a way to address the possibility that neighborhood size may differ by population or activity and/or as a means to discover the appropriate spatial scale (Brownson et al., 2009). A number of researchers have used multiple buffer sizes within the same population to examine associations between physical activity facilities and physical activity across the different buffer sizes. These studies have shown mixed results with some studies finding no association regardless of buffer size used (Prins et al., 2011) and others finding variable associations depending on the buffer size (Boone-Heinonen et al., 2010). However, simulation work has suggested that using model fit as a means to identify the most salient spatial scale is problematic because the simulations across a large range of neighborhood sizes showed little variability in model fit. In addition, the model fit was not a reliable predictor of the most appropriate spatial scale (Spielman and Yoo, 2009).
This study sought to address the previously mentioned research gaps by examining how adolescents conceptualized their neighborhoods and the degree to which their self-defined neighborhood boundaries overlaid common neighborhood boundaries and the places where adolescents were physically active. In addition, relationships between environmental attributes and physical activity and obesity were investigated using three different neighborhood boundaries (self-defined, census tract, buffer based). We examined five attributes of the built environment that have been examined in previous studies of physical activity levels or obesity in adolescents: park availability, commercial physical activity facilities, recreation centers, restaurants, and food stores (Ding and Gebel, 2012; Dunton et al., 2009; Galvez et al., 2010; Giles-Corti et al., 2009; Rahman et al., 2011). While the majority of research on the food environment has examined its effect on healthy eating and obesity, we retained these exposures in our models for physical activity because we hypothesized, a priori, that the availability of these types of facilities in the neighborhood could facilitate active transport.
We hypothesized that self-defined neighborhood size characteristics would be significantly different from census tract and buffer-based neighborhood size characteristics and that counts of environmental features within each of these neighborhood boundaries would differ significantly. We also hypothesized that environmental features (e.g., number of parks) would have more significant associations with physical activity and overweight/obesity status across a range of environmental exposures when using self-defined neighborhood boundaries than when using neighborhood boundaries defined by census tracts or buffers.
METHODS
We conducted a mixed-methods study of 145 urban minority adolescents who lived in one of 13 subsidized housing estates in Cuyahoga County, Ohio. Eligible adolescents were those aged 14-17, living in a family public housing estate within the study area, and with the ability to complete the study protocol without assistance. Participants were recruited via mailed information packets, public information sessions, flyers, posters, and referrals from youth programs (e.g., Boys’ and Girls’ Clubs, librarians). Written parental/guardian consent and adolescent assent were obtained in person. This study was approved by the University Hospitals Case Medical Center Institutional Review Board. Adolescents were given $35 to complete the full protocol which included an interview, completion of a one-day travel diary with concurrent accelerometer wear, and measurement of their height and weight.
Participants completed either a 90-minute semi-structured interview (N=20) or a 60- minute structured interview (N=125). As part of these in-person interviews, a trained facilitator instructed adolescents to draw the boundaries of their neighborhood by hand on a 19” x 19” acetate sheet overlaying a detailed map of the area surrounding their homes. The colored map included an aerial photograph, points of interest (e.g., schools, libraries, fire/police stations), and designations for all food and physical activity locations, street names, and highways. Two maps with different scales (1:10,000 or 2 square miles and 1:16,500 or 5 square miles) were presented. The adolescent could choose either map for drawing his/her neighborhood boundaries. To facilitate the drawing of neighborhood boundaries, the adolescent participants were instructed, “Using this pen, draw a line around the area you think of as your neighborhood. The line you draw can make any shape and be any size you want, but the ends of the line must meet.” If the adolescent was unclear about the task, the following probe was provided: “Think about the borders of your neighborhood and draw a shape to represent those borders. So everything inside the shape would be what you consider your neighborhood and everything outside the shape would not be your neighborhood.”
After drawing his/her neighborhood, each participant was asked what factors she/he considered in drawing the neighborhood boundaries. In the semi-structured interviews (N=20), adolescents were asked this question in an open-ended manner, with a series of probes. The responses from these participants were used to generate 12 closed-ended response options for the structured interviews (N=125). The latter group constitutes the sample for the analysis of factors associated with neighborhood boundaries. All other findings are based on the full sample of adolescents.
All participants were asked to list the places (including addresses) over the past week where they were physically active outside of their homes. If the address was unknown, they were asked to report the nearest cross streets and/or landmarks. Participants also provided information about their home address, age, gender, Hispanic/Latino origin, and race. Race was self-defined as one or more of the following: White, Black or African American, Asian, American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander, and/or they could write in additional categories. We dichotomized race and Hispanic ethnicity into non-Hispanic black versus all other race/ethnicities. Physical activity levels were measured by the following Youth Risk Behavior Surveillance System survey item: “During the past 7 days, on how many days were you physically active for a total of at least 60 minutes per day?” Participants were classified as active if physical activity was ≥ 60 minutes on ≥ 5 days per week or as inactive if otherwise. This question has been shown to have acceptable validity and reliability (Prochaska et al., 2001; Ridgers et al., 2012). Participants’ weight and height were measured with a Seca scale and stadiometer in a private area in light clothing (i.e., shoes and outerwear removed). The average of three height and weight measures was used in the analysis. Weight classification: overweight was defined as body mass index (BMI) ≥ the 85th BMI-for-age percentile and obese was defined as BMI ≥ 95th BMI-for-age percentile according to the CDC BMI-for-age classification (Kuczmarski et al., 2002).
Calculating Neighborhood Boundaries
Three different neighborhoods were created in a Geographic Information System (GIS). The neighborhoods drawn by each adolescent were digitized in a GIS, where geographic entities are translated into their machine-readable equivalent elements of planar geometry (points, lines, and polygons) (Cowen, 1988). Digitizing allowed the hand-drawn neighborhoods to be measured with precision and their relationship to other entities in the built environment to be quantified. In addition to the self-defined neighborhood produced by adolescents, two additional neighborhoods were created for each adolescent in ArcGIS v. 9.3. These two additional neighborhoods are those often used in neighborhood-based research: (1) a buffer around participants’ home addresses and (2) the boundaries of participants’ census tracts. The home buffer-based neighborhood was generated by first geocoding each participant’s home street address (provided by the participant) and then creating a 0.75 mile network buffer around this point. A network buffer differs from a straight-line (Euclidean) distance in that the underlying street network is considered; thus, the buffers can differ in area with respect to street density. Network buffers were used because they are more relevant when considering walking or driving distance along street routes. To create the census tract neighborhood, the census tract that contained each adolescent’s home was identified, and the census tract boundaries were used as the neighborhood boundary.
Location data on restaurants, recreation centers, food stores, parks, and commercial physical activity facilities were obtained through secondary data sources including InfoUSA, Internet Yellow pages, and the local Department of City Planning. The locations were geocoded and compiled in ArcGIS. The physical activity facilities within a mile buffer of the adolescent’s home were ground-truthed for accuracy (i.e., a study team member verified that the facilities still existed and were available for use). Closed locations were deleted from the database and additional locations, not identified through secondary data sources, were added.
The physical activity places visited over the week prior to each participant’s interview were geocoded in ArcGIS. When participants only reported cross streets and/or landmarks, information from our GIS database, Internet searches, maps, and local knowledge were used to assign an address to locations. Of the 445 locations given by the participants, 54% were coded to an exact location, 25% were coded to an intersection, 9% were coded to a street segment, and 12% could not be geocoded. In the last category, many of the locations included non-public spaces such as a cousin’s or friend’s house.
Using these geocoded locations for each participant along with their home address, physical activity spaces (PASs) were created. A PAS in the context of this study is defined as the minimum convex polygon that contains all the points of interest (here, the physical activity locations visited in the time period of interest and the participant’s home address). This method required a minimum of three locations for each individual, including their home location. Most adolescents had at least three locations (N=115). Physical activity spaces for individuals who identified only one location in which they were active were created by joining the one activity location and their home location with a line and buffering the line by three meters (N=24). If no physical activity places were visited over the time period of interest, the participant was deemed to not have a PAS (N=6).
Neighborhood size attributes, including area, length-EW (defined as furthest distance from east to west) and length-NS (defined as furthest distance from north to south), were calculated in ArcGIS for each of the three neighborhood definitions (i.e., self-defined, census tract, and 0.75-mile buffer around the home). Counts of each facility type for restaurants, recreation centers, food stores, parks, and commercial physical activity facilities within each of the three neighborhood definitions were calculated using point-in-polygon methods. The spatial relationship across the three definitions of neighborhood was considered by examining the degree of spatial overlap between the definitions (i.e., the number of census tracts that were at least partially contained within a self-defined neighborhood; the degree of spatial overlap between the self-defined neighborhood and the census tract; and the relative size of the 0.75 mile buffer compared to the self-defined neighborhood). Lastly, the proportions of facilities used within each of the three neighborhood boundaries (i.e., self-defined neighborhood, 0.75 mile buffer and census tract) were calculated.
Finally, the area of the PAS was calculated in ArcGIS, and the percent of overlap between an individual’s PAS and their self-defined neighborhood and 0.75 mile buffer were calculated. For each participant, it was also determined whether the PAS was fully contained within the self-defined neighborhood or within the 0.75 buffer neighborhood.
ANALYSES
Descriptive statistics of the size characteristics (area, length-EW, length-NS) for the three neighborhood definitions were examined. For the self-defined neighborhood attributes, linear regression models were used to determine whether the variability in any size characteristics (i.e., area, length-EW, length-NS) were related to age, race/ethnicity, gender, self-reported physical activity level and/or overweight status. Neighborhood size characteristics were log-transformed because they were right skewed.
Participant responses as to which factors were important in defining neighborhood boundaries were summarized, and differences by age, race/ethnicity, gender, self-reported physical activity level and overweight status were explored using chi-square statistics in bivariate models. For this analysis only, the sample size was 125 adolescents (i.e., those that participated in the structured interview).
Differences in facility counts between pairs of neighborhood definitions were examined with Wilcoxon signed rank sum tests. Specifically, counts of restaurants within the self-defined neighborhood were compared to counts of restaurants within a 0.75-mile buffer, counts of restaurants within a census tract were compared to counts of restaurants within a 0.75-mile buffer, and counts of restaurants within a census tract were compared to counts of restaurants within the self-defined neighborhood. These three sets of comparison were repeated for each of the remaining categories of facilities (i.e., food stores, commercial physical activity facilities, parks, recreation centers).
The association between the facility counts and three outcomes (i.e., physical activity, overweight status, and obesity status) were examined by logistic regression. The regressions were run across each of the five facility types (i.e., restaurants, parks, commercial physical activity facilities, food stores, recreation centers) using counts derived from the three neighborhood definitions for three outcomes, which resulted in a set of 3 regressions across 5 exposures for each of the 3 outcomes. All regression models controlled for age, gender, and race/ethnicity and accounted for the clustering within housing estates by utilizing robust standard errors. An example of one of these models is the examination of whether the number of parks in the self-defined neighborhood was associated with reported physical activity levels controlling for age, gender and race/ethnicity.
Lastly, summary statistics for a number of metrics that document the spatial overlap across the three neighborhood boundaries and the neighborhood boundary and a PAS were completed. These metrics included the number of census tracts within a self-defined neighborhood, the proportion of overlap between a self-defined neighborhood and a participant’s census tract, the ratio of size between the 0.75 mile buffer around a home and a self-defined neighborhood, the size of a PAS, the degree of overlap between an individual’s PAS and their self-defined neighborhood and 0.75 mile buffer, and the proportions of facilities used within each of the three neighborhood boundaries. In addition, the proportion of participants that had a PAS that was fully contained within their self-defined neighborhood or within their 0.75- mile buffer around their home was determined.
RESULTS
Participants were mostly male (57%), self-identified their race/ethnicity as non-Hispanic Black/African American (74%) and had a mean age of 15 years (range = 14-17). Forty-two percent were overweight/obese while 26% were obese. Approximately one-third of participants (32%) were active for at least 60 minutes for at least 5 days of the week. One participant refused to draw neighborhood boundaries, leaving 144 participants for all analyses involving self-defined neighborhood boundaries.
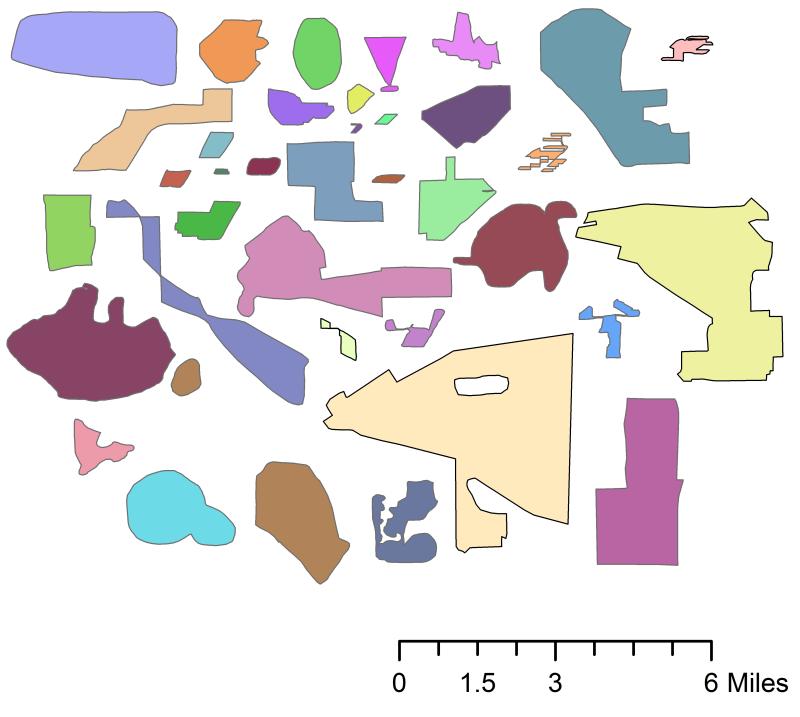
There was great variability in the size and shape of the neighborhoods drawn on the maps (see Figure 1 for sample of drawings). The total size of the self-defined neighborhoods ranged from 0.004 square miles to over 10 square miles (median 0.3 square miles) (see Table 1). The median length-EW was 4287ft, and the median length-NS was 3558ft. Comparatively, the neighborhoods defined by a 0.75 mile network buffer ranged from 0.47 square miles to 1.11 square miles (median 0.95 square miles), whereas the census tract boundaries ranged from 0.09 square miles to 3.46 square miles (median 0.20 square miles).
Figure 1.
Sample of self-defined neighborhood boundaries
Table 1.
Characteristics of three neighborhood definitions
| Neighborhood Unit | Mean Area (Sq. Mi.) |
Median Area (Sq. Mi.) |
Minimum Area (Sq. Mi.) |
Maximum Area (Sq. Mi.) |
Median WidthX(feet) | Median LengthY (feet) |
|---|---|---|---|---|---|---|
| Self-defined | 0.69 | 0.30 | 0.004 | 10.39 | 4286.7 | 3557.8 |
| 0.75 mile Buffer | 0.87 | 0.95 | 0.47 | 1.11 | 6554.0 | 6209.2 |
| Census Tract | 0.25 | 0.20 | 0.09 | 3.46 | 3493.6 | 1964.1 |
Age was the only demographic variable that was a significant predictor (p<=.05) in multiple variable regression models that examined whether age, gender, race/ethnicity, overweight status, or physical activity levels were predictive of length-NS of the self-defined neighborhoods (results not shown). Older participants drew larger neighborhoods than younger participants. When considering variables whose significance level was less than .10, age predicted the length-EW of the neighborhood (p=.08) and overall neighborhood size (p=.055) such that older participants drew larger neighborhoods. Gender also predicted overall neighborhood size (p=.08), length-NS (p=.06), and length-EW (p=.08) such that boys drew larger neighborhoods than girls. Race, overweight status, and physical activity did not significantly predict neighborhood size characteristics in any models.
The most frequently endorsed reasons for why the adolescents (N=125) drew their neighborhood the way they did were as follows: Where you live or hang out (82%); where friends live or hang out (74%); where you know or don’t know people (74%); where you have fun (72%), and specific streets where you travel (71%). Least frequently endorsed items included: Physical boundaries (18%); where you are allowed or not allowed to go (42%); border of housing estate (47%); and how far from your home (48%). None of the endorsed factors were significantly associated with participant characteristics (i.e., age, gender, race/ethnicity, overweight status, and physical activity levels) in the bivariate models (results not shown).
Count of parks, commercial physical activity facilities, recreation centers, food stores, and restaurants within each of the three neighborhood buffers are given in Table 2. Counts of each facility type were highly variable across neighborhood definitions. For example, the average number of parks in the self-defined neighborhood was 3.4 versus 5.2 in the 0.75 buffer and 1.4 in the census tract (medians were 2, 5, and 1, respectively). In all pairwise comparisons across all facility types, the counts were statistically significantly different based on the neighborhood definition used; the one exception was that counts of recreation centers in the 0.75 buffer and self-defined neighborhood were not significantly different.
Table 2.
Counts of facilities using three neighborhood definitions
| Neighborhood Unit | Restaurants Mean (median) |
Rec Center Mean (median) |
Food Store Mean (median) |
Park Mean (median) |
Commercial PA Mean (median) |
|---|---|---|---|---|---|
| Self-defined | 9.05 (2.00)a | 1.38 (1.00) | 4.58 (1.50)a | 3.38 (2.00)a | 0.57 (0.00)a |
| 0.75 mile Buffer | 9.19 (6.00)a | 1.54 (1.00) | 4.77 (4.00)a | 5.19 (5.00)a | 0.57 (1.00)a |
| Census Tract | 2.14 (1.00)a | 0.66 (1.00) a | 0.80 (0.00)a | 1.39 (1.00)a | 0.11 (0.00)a |
All counts within a category (e.g., restaurants) were significantly different at p <.05 from other counts in same category based on Wilcoxon signed rank sum tests except recreation centers in the 0 .75 mile network buffer and self-defined neighborhood.
The results from regression models that examined the association between the counts of each facility with the three outcomes (i.e., obesity status, overweight status, physical activity) were different depending on which neighborhood boundary was chosen. Using counts from within the participants’ self-defined boundaries, none of the associations were significant. When using the 0.75 buffer, having more parks was associated with lower odds of obesity. Also, having more restaurants or food stores in a 0.75 mile buffer was associated with higher odds of being physically active. Finally, at the census tract level, having more recreation centers in one’s census tract was associated with increased odds of being physically active, but having more commercial facilities was associated with increased odds of overweight.
There was limited spatial overlap amongst the neighborhood boundaries and between the neighborhood boundaries and the area identified as their PAS. On average, about 45% of a given participants’ census tract was represented by their self-defined neighborhood. The median number of census tracts that were fully or partially contained within a self-defined neighborhood boundary was 6. The 0.75 mile buffer was on average almost three times larger than the self-defined neighborhoods. The PASs created for each participant showed great variability. Amongst those who had a PAS (N=139), the median size of a participant’s PAS was 0.14 square miles (mean 2.06, sd=7.1). The smallest was 0.000003 square miles (e.g., 78.1 square feet); the largest PAS was 59.6 square miles. Across participants, the average proportion of PASs within a neighborhood boundary was 54% for a network buffer and 43% for the self-defined neighborhood. The PAS was completely contained within a 0.75 mile network buffer around their home for only 32% of participants. For self-defined neighborhoods, only 22% of adolescents’ PASs was completely contained within their neighborhood. On average, 45% of physical activity facilities used by adolescents were in their self-defined neighborhood. The corresponding numbers for the percent of physical activity facilities used in the 0.75 mile network buffer and census tract are 48% and 27%, respectively.
DISCUSSION
The median size of the neighborhoods drawn by urban minority adolescents living in subsidized housing estates (.30 square miles) was similar to the median size of neighborhoods drawn by adults (.35 square miles) in a very large study across 10 different cities (Coulton et al., 2013). The median neighborhood size drawn by adolescents in the present study was much smaller than the average size of the neighborhood drawn by older adolescents living in Philadelphia, PA, which was 2.55 square miles (Basta et al., 2010). Across the participants in this study, the neighborhoods as self-defined by the adolescents were highly variable, similar to other findings with both adults and adolescents (Basta et al., 2010; Coulton et al., 2011; Coulton et al., 2013; Coulton et al., 2001). There was little evidence of symmetry in the neighborhood definitions as evidenced by the dimensions of the length-EW and length-NS across the self-defined neighborhoods.
Participant characteristics associated with the size of neighborhood were age (p<.05) and gender (p<.10). Our results were similar to those of Guest and Lee who found that age was associated with neighborhood size in adults (Guest and Lee, 1984). Associations between gender and neighborhood size in previous studies have been inconsistent. Two studies showed no association (Haney and Knowles, 1978; Pebley and Sastry, 2009), but one study showed that men draw larger neighborhoods than women (Guest and Lee, 1984), similar to findings in our study. Methodological differences (such as calibration of neighborhood size) may be the reason for the inconsistent findings across studies when examining the association between various factors and neighborhood size or boundaries (Guest and Lee, 1984; Haney and Knowles, 1978; Lee and Campbell, 1997; Pebley and Sastry, 2009). For example, one study used a four-point scale for neighborhood size ranging from (1) the block or street you live on to (4) an area larger than a 15- minute walk (Pebley and Sastry, 2009), while another study required residents to estimate how many blocks were in their neighborhood to generate a continuous measure of neighborhood size (Lee and Campbell, 1997). Additionally, all of the studies differ in the range of places represented and the density of sampling within places. Coulton and colleagues found in a study of 6000 adults that individual variables were only able to explain 4% of the within-context variability across neighborhood definitions (Coulton et al., 2013). Taken together, these studies suggest that there is a large amount of individual variability in self-defined neighborhoods that cannot be systematically explained by commonly considered individual attributes.
Social factors were mentioned more frequently than physical or spatial factors when the adolescents were asked which factors most influenced their definitions of neighborhoods. Only a few studies have inquired about factors associated with neighborhood-based boundaries. A study based on interviews with adolescents and their parents found that their neighborhood definitions were influenced by the built and institutional environment, population demographics, social class, safety concerns and symbolic neighborhood identity (Campbell et al., 2009). Another study of neighborhood descriptions during a guided walk of children aged 8-11 suggested people, buildings, streets, institutions and activity spaces were factors considered in their neighborhood definitions (Spilsbury et al., 2009). The differences in salient factors across these studies could be due to methodological differences, geographic differences, or age differences. Alternatively, it could be that institutions can serve as a unifying structure for defining larger local areas or communities but are less salient for definitions of smaller neighborhoods (Guest and Lee, 1984).
Neighborhood definitions used in this study, including the self-defined neighborhood and the 0.75 mile buffer, missed many areas in which physical activity occurred. This was evidenced by the lack of spatial overlap between the participants’ PASs and their neighborhood boundaries as well as the proportion of physical activity facilities used outside their self-defined neighborhoods and the 0.75 mile buffer around their home. This finding is supported by other studies. For example, a study of 15 adolescents who wore a GPS found that female adolescents spend about one-third of their time more than one kilometer away from their home (Wiehe et al., 2008). Troped and colleagues found that adults accumulated only 18% of their moderate to vigorous activity within one kilometer of their home based on concurrent GPS and accelerometer wear (Troped et al., 2010). In a similar study to ours, 42% of adults reported at least one usual walking destination outside of their self-defined neighborhoods (Smith et al., 2010).
The 0.75 mile network buffers were nearly three times larger than self-defined neighborhoods. Smith and colleagues similarly found that adult self-drawn neighborhoods represented only 16% (+/− 20%) of a one mile Euclidean buffer and 36% (+/− 36%) of the one mile network buffer (Smith et al., 2010). As a result of the size differences across neighborhood definitions in this study, the counts across each neighborhood definition were highly variable. Thus, for a single participant, the neighborhood exposure assessment would differ substantially depending on which definition is used. Not surprisingly, regression results across neighborhood definitions were inconsistent.
Overall, few regressions showed a significant association between any facility count and either physical activity, overweight, or obesity. The lack of association in many of the analyses is consistent with the mixed findings in the built environment literature (Davison and Lawson, 2006; Ding and Gebel, 2012; Dunton et al., 2009), but the lack of associations could be due to several other issues. First, because of the small sample size, this study had low power to detect differences. That being said, given the interest in comparing results within sets of neighborhood exposures across the three definitions, the power to detect differences would be the same within a set. Secondly, the homogeneity of the neighborhoods where the participants lived could have limited our power to detect differences. Nonetheless, it is notable that when significant associations between the five environmental exposures and physical activity, overweight/obesity, or obesity were detected, they were only detected when neighborhood was defined by census tract or buffer, not by individuals. This is contrary to our hypothesis and suggests that obtaining self-defined neighborhoods for all participants in a study even were it feasible, may not be the best method for ascribing environmental exposures for physical activity and obesity.
Many physical activity studies that attempt to look at the role of the neighborhood environment on physical activity report as a limitation that it is not known how to exactly measure the neighborhood environment and therefore employ many different definitions. In our study, having an adolescent’s definition of his or her neighborhood did not produce the strongest associations with physical activity or obesity. Associations may have been found with the 0.75 network buffer (and not the self-defined neighborhood) because the 0.75 mile buffer was generally larger and more likely to contain facilities utilized for adolescent activity. However, the direction and magnitude of error from inaccurately defining the correct spatial scale is dependent on a number of factors such as the difference between the “true” neighborhood size and that used in the study, the strength of the association, and the configuration of the environment (Spielman and Yoo, 2009).
Taken together, these findings suggest the need for a paradigm shift in studies of the effect of the built environment on health. There was little geographic overlap in the various definitions of neighborhood and little consistency across neighborhood definitions in characterizing the built environment features of one’s neighborhood. Equally important is the finding that many of the locations in which the adolescents were active were not within the neighborhood, regardless of how neighborhood was defined. These findings call into question whether the neighborhood is the salient geography for environmental effects on adolescent physical activity even if the term “neighborhood” is evoked by researchers to represent simply what is spatially proximate. In fact, the adolescents in this study seemed to define their neighborhoods in social terms rather than based on physical features or activity locations. This uncertainty about the correct spatial scale for examining contextual effects has been called the “uncertain geographic context problem” (UGCoP) by Kwan (Kwan, 2012a). This study adds support for the recent calls by Kwan (Kwan, 2012a; Kwan, 2012b), Rainham (Rainham et al., 2010), Matthews (Matthews, 2012) and others to conduct studies of environmental effects on health that move beyond concepts of space that are static in terms of time and space.
Some of these next generation studies are underway. Several studies have used GPS tracking data to define neighborhoods and/or activity spaces. In one of the first studies to explore activity space, 120 adults wore GPS and their resulting activity spaces were calculated (Zenk et al., 2011). In another study, 41 older adults wore GPS devices, and their travel behavior was used to create new definitions of a participant neighborhood (Boruff et al., 2012). Other GPS studies, including some with adolescents, have examined whether activity levels are higher near or within specific features regardless of whether those features are in or outside the neighborhood (Rodriguez et al., 2012; Wheeler et al., 2010). These studies use a contemporaneous momentary design, which is an examination of physical activity level by location during the same time frame (e.g., minute) (Chaix et al., 2013). While these studies help unravel the complex relationships between environments and health behavior, associations of exposure within activity spaces to participant behavior or between exposure and behavior using contemporaneous momentary designs cannot determine causal ordering (Chaix et al., 2013). For example, associations between fast food restaurant exposure based on activity spaces and eating fast food will be biased by the fact that the exposure (traveling to a fast food restaurant) is a likely necessary condition for the outcome. Thus, in attempting to solve the dilemma of the relevant scale for geographic exposure, we must be mindful that our methods do not add new biases to our research studies. In fact, the dilemma of causal ordering is also a potential bias of using self-defined neighborhoods in studies of behavior. Participant’s definitions of their neighborhood could be influenced by their behavior as opposed to their behavior being influenced by features of the neighborhood. That being said, this study showed limited evidence of this because the spatial overlap of places in which kids were active and their self-defined neighborhoods was low.
These next generation studies may, however, begin to address the black box issue of contextual effects. As Macintrye, Ellaway and Cummins (Macintyre et al., 2002) argued a decade ago, we need to begin to understand the underlying mechanisms of contextual effects. While many studies have suggested that environmental features affect physical activity levels and obesity, there have been few studies that have directly tested the mechanism by which the environment affects these behaviors and outcomes (e.g., via utilization of facilities, social norms, etc.).
Further, to date, few studies have simultaneously considered both location and context (e.g., the influence of friends and family in specific locations) or whether any interactions exist by individual demographics like age and gender. A notable exception is a study by Mennis and Mason in which they examined how substance use was affected by spatial attributes (e.g., a list of places traveled to in the past week that were ranked from highest likelihood of risky activity to lowest likelihood), social network data and the intersection of these data (i.e., who within their social network was most likely to be with them at various locations (e.g., risky vs. safe locations)) (Mennis and Mason, 2011). More studies that investigate not only where people travel and are active but also place-specific contextual data (i.e., who they are with as the behavior occurs) are needed.
The current study must be considered in light of its limitations. Our study included a small sample size (N=145) and a relatively homogenous population and environment, and would need to be replicated in other populations. However, the high variability seen in this study across neighborhood definitions is likely to be even greater in settings that are more diverse than this study’s setting. The study is also limited by the self-report method of capturing physical activity outside of the home. The study did not directly address active transport, which accounts for a large amount of MVPA by adolescents (Rainham et al., 2012). This study used a 0.75 buffer mile buffer as one of the neighborhood definitions. Based on the literature, a number of additional buffer radii could have been selected. This buffer size was selected because it has been shown to be an easy walking distance for adolescents and because it falls midway between the range of buffers often used (Colabianchi et al., 2007); however, other buffers may have resulted in different findings. Finally, some significant findings may be due to chance given the large number of regression models estimated.
The current study has a number of strengths. It is one of the first studies to examine adolescent self-defined neighborhood in conjunction with other neighborhood boundaries. Further, it examined the differential effect of various neighborhood definitions on the associations between environmental exposures and physical activity and obesity. We were able to concurrently assess self-defined neighborhoods and places in which adolescents were active. The environmental exposures are based on comprehensive GIS data and fieldwork, which included ground-truthing the physical activity locations near the participant’s homes. Finally, the study included low income minority adolescents who are at particularly high-risk for exposure to obesogenic environments and have high rates of physical inactivity and obesity.
Conclusion
Quantifying built environmental exposures is essential for examining the environmental effects on physical activity and obesity. However, much remains to be learned about the proper manner and scale for defining and calculating these exposures. In our study, individually drawn neighborhood boundaries exhibited significant variability across participants. Self-defined boundaries were generally small in size and did not capture many of the places where adolescents were physically active. Additionally, self-defined neighborhoods were markedly different than commonly used neighborhood boundaries. Future research needs to develop practical and theoretically-based methods for measuring salient environmental exposures.
Highlights.
Adolescents drew self-defined neighborhoods that were highly variable in size
Self-defined neighborhoods had little overlap with other neighborhood delineations
Many physical activity facilities used weren’t in self-defined neighborhoods
Facilities and activity/obesity were not related using self-defined neighborhoods
Table 3.
Logistic regression models of the association between facility count and obesity, overweight or physical activity1 across three different neighborhood boundaries with robust standard errors2
| Parks OR4 (CI) 5 |
Rec Center OR (CI) |
Commercial PA3 OR (CI) |
Restaurant OR (CI) |
Food Store OR (CI) |
|
|---|---|---|---|---|---|
| Obesity | |||||
| Self-Defined | 0.97 (.92, 1.02) | 1.10 (.83, 1.45) | 0.99 (.81, 1.22) | 0.99 (.99, 1.00) | 0.99 (.96, 1.02) |
| 0.75 Mile Buffer | 0.79 (.66, .94)** | 1.16 (.79, 1.71) | 1.02 (.39, 2.70) | 0.97 (.92, 1.02) | 0.83 (.69, 1.01) |
| Census Tract | 1.02 (.80, 1.30) | 1.44 (.56, 3.65) | 1.17 (.50, 2.71) | 1.09 (.91, 1.31) | 1.01 (.75, 1.35) |
| Overweight | |||||
| Self-Defined | 1.01 (.92, 1.12) | 1.09 (.80, 1.47) | 1.04 (.77, 1.41) | 1.00 (.98, 1.02) | 1.02 (.95, 1.09) |
| 0.75 Mile Buffer | 0.93 (.84, 1.03) | 1.09 (.89, 1.33) | 1.14 (.72, 1.78) | 0.99 (.97, 1.02) | 0.96 (.87, 1.06) |
| Census Tract | 1.01 (.87, 1.17) | 1.58 (.86, 2.90) | 1.94 (1.04, 3.64)* | 1.08 (.98, 1.19) | 0.98 (.85, 1.14) |
| Physical Activity | |||||
| Self-Defined | 0.98 (.92, 1.05) | 0.90 (.70, 1.14) | 0.97 (.75, 1.26) | 1.00 (.98,1.01) | 0.99 (.96, 1.02) |
| 0.75 Mile Buffer | 1.09 (.99, 1.20) | 1.06 (.79, 1.43) | 1.50 (.94, 2.40) | 1.05 (1.02, 1.09)** | 1.15 (1.05, 1.27)** |
| Census Tract | 1.01 (.76, 1.35) | 3.85 (1.95, 7.63)*** | 0.95 (.38, 2.41) | 1.08 (.98, 1.19) | 0.82 (.55, 1.22) |
Regression models controlled for age, gender and race/ethnicity
Robust standard errors were used to account for the clustering of participants within housing estates
PA= Physical Activity
OR = Odds Ratio
CI = Confidence Interval
p<.05;
p<.01;
p<.001
Funding Acknowledgement
This study was supported by a grant from National Institutes of Health/National Cancer Institute R21CA121151 and a grant from the Robert Wood Johnson Foundation Active Living Research program.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Natalie Colabianchi, University of Michigan.
Claudia Coulton, Case Western Reserve University.
James D. Hibbert, University of South Carolina.
Stephanie McClure, Washington University.
Carolyn E. Ievers-Landis, Case Western Reserve University.
Esa M. Davis, University of Pittsburgh.
References
- Basta LA, Richmond TS, Wiebe DJ. Neighborhoods, daily activities, and measuring health risks experienced in urban environments. Soc Sci Med. 2010;71:1943–1950. doi: 10.1016/j.socscimed.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone-Heinonen J, Popkin BM, Song Y, Gordon-Larsen P. What neighborhood area captures built environment features related to adolescent physical activity? Health Place. 2010;16:1280–1286. doi: 10.1016/j.healthplace.2010.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boruff BJ, Nathan A, Nijenstein S. Using GPS technology to (re)-examine operational definitions of ‘neighbourhood’ in place-based health research. Int J Health Geogr. 2012:11. doi: 10.1186/1476-072X-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownson RC, Hoehner CM, Day K, Forsyth A, Sallis JF. Measuring the Built Environment for Physical Activity State of the Science. Am J Prev Med. 2009;36:S99–S123. doi: 10.1016/j.amepre.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell E, Henly JR, Elliott DS, Irwin K. Subjective Constructions of Neighborhood Boundaries: Lessons from a Qualitative Study of Four Neighborhoods. Journal of Urban Affairs. 2009;31:461–490. [Google Scholar]
- Chaix B, Méline J, Duncan S, Merrien C, Karusisi N, Perchoux C, Lewin A, Labadi K, Kestens Y. GPS tracking in neighborhood and health studies: A step forward for environmental exposure assessment, a step backward for causal inference? Health Place. 2013;21:46–51. doi: 10.1016/j.healthplace.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Colabianchi N, Dowda M, Pfeiffer KA, Porter DE, Almeida MJ, Pate RR. Towards an understanding of salient neighborhood boundaries: adolescent reports of an easy walking distance and convenient driving distance. Int J Behav Nutr Phys Act. 2007;4:66. doi: 10.1186/1479-5868-4-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulton C, Chan T, Mikelbank K. Finding Place in Community Change Initiatives: Using GIS to Uncover Resident Perceptions of their Neighborhoods. Journal of Community Practice. 2011;19:10–28. [Google Scholar]
- Coulton CJ, Jennings MZ, Chan T. How Big is My Neighborhood? Individual and Contextual Effects on Perceptions of Neighborhood Scale. American Journal of Community Psychology. 2013;51:140–150. doi: 10.1007/s10464-012-9550-6. [DOI] [PubMed] [Google Scholar]
- Coulton CJ, Korbin J, Chan T, Su M. Mapping residents’ perceptions of neighborhood boundaries: A methodological note. American Journal of Community Psychology. 2001;29:371–383. doi: 10.1023/A:1010303419034. [DOI] [PubMed] [Google Scholar]
- Cowen DJ. Gis Versus Cad Versus Dbms - What Are the Differences. Photogrammetric Engineering and Remote Sensing. 1988;54:1551–1555. [Google Scholar]
- Davison KK, Lawson CT. Do attributes in the physical environment influence children’s physical activity? A review of the literature. Int J Behav Nutr Phys Act. 2006;3:19. doi: 10.1186/1479-5868-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding D, Gebel K. Built environment, physical activity, and obesity: What have we learned from reviewing the literature? Health Place. 2012;18:100–105. doi: 10.1016/j.healthplace.2011.08.021. [DOI] [PubMed] [Google Scholar]
- Downs RM, Stea D. Cogmitive maps and spatial behavior: Process and products. In: Downs RM, Stea D, editors. Image and environment. Aldine; Chicago: 1973. pp. 8–26. [Google Scholar]
- Dunton GF, Kaplan J, Wolch J, Jerrett M, Reynolds KD. Physical environmental correlates of childhood obesity: a systematic review. Obes Rev. 2009;10:393–402. doi: 10.1111/j.1467-789X.2009.00572.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: A systematic review of the epidemiologic evidence. Health Place. 2010;16:175–190. doi: 10.1016/j.healthplace.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Galvez MP, Pearl M, Yen IH. Childhood obesity and the built environment. Current Opinion in Pediatrics. 2010;22:202–207. doi: 10.1097/MOP.0b013e328336eb6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giles-Corti B, Kelty SF, Zubrick SR, Villanueva KP. Encouraging walking for transport and physical activity in children and adolescents: how important is the built environment? Sports Med. 2009;39:995–1009. doi: 10.2165/11319620-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- Guest AM, Lee BA. How Urbanites Define Their Neighborhoods. Population and Environment. 1984;7:32–56. [Google Scholar]
- Haney WG, Knowles ES. Perception of Neighborhoods by City and Suburban Residents. Human Ecology. 1978;6:201–214. [Google Scholar]
- Jago R, Baranowski T, Zakeri I, Harris M. Observed environmental features and the physical activity of adolescent males. Am J Prev Med. 2005;29:98–104. doi: 10.1016/j.amepre.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Kuczmarski R, Ogden C, Guo S, Grummer-Strawn L, Flegal K, Mei Z, Wei R, Curtin L, Roche A, Johnson C. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11:246, 1–190. [PubMed] [Google Scholar]
- Kwan M-P. The Uncertain Geographic Context Problem. Annals of the Association of American Geographers. 2012a;102:958–968. [Google Scholar]
- Kwan MP. How GIS can help address the uncertain geographic context problem in social science research. Annals of GIS. 2012b;18:245–255. [Google Scholar]
- Ladd FC. Black Youths View Their Environment - Neighborhood Maps. Environment and Behavior. 1970;2:74–99. [Google Scholar]
- Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obesity Reviews. 2011;12:217–230. doi: 10.1111/j.1467-789X.2010.00726.x. [DOI] [PubMed] [Google Scholar]
- Lee BA, Campbell KE. Common ground? Urban neighborhoods as survey respondents see them. Social Science Quarterly. 1997;78:922–936. [Google Scholar]
- Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55:125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- Matthews SA. Thinking About Place, Spatial Behavior, and Spatial Processes in Childhood Obesity. Am J Prev Med. 2012;42:516–520. doi: 10.1016/j.amepre.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maurer R, Baxter JC. Images of Neighborhood and City among Black-American, Anglo-American, and Mexican-American Children. Environment and Behavior. 1972;4:351–388. [Google Scholar]
- Mennis J, Mason MJ. People, Places, and Adolescent Substance Use: Integrating Activity Space and Social Network Data for Analyzing Health Behavior. Annals of the Association of American Geographers. 2011;101:272–291. [Google Scholar]
- Pebley AR, Sastry N. Our place: Perceived neighborhood size and names in los angeles. California Center for Population Research; Los Angeles, CA: 2009. Working Paper # 2009-026 ed. [Google Scholar]
- Prins RG, Ball K, Timperio A, Salmon J, Oenema A, Brug J, Crawford D. Associations between availability of facilities within three different neighbourhood buffer sizes and objectively assessed physical activity in adolescents. Health Place. 2011;17:1228–1234. doi: 10.1016/j.healthplace.2011.07.012. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Sallis JF, Long B. A physical activity screening measure for use with adolescents in primary care. Arch Pediatr Adolesc Med. 2001;155:554–559. doi: 10.1001/archpedi.155.5.554. [DOI] [PubMed] [Google Scholar]
- Rahman T, Cushing RA, Jackson RJ. Contributions of Built Environment to Childhood Obesity. Mount Sinai Journal of Medicine. 2011;78:49–57. doi: 10.1002/msj.20235. [DOI] [PubMed] [Google Scholar]
- Rainham D, McDowell I, Krewski D, Sawada M. Conceptualizing the healthscape: Contributions of time geography, location technologies and spatial ecology to place and health research. Soc Sci Med. 2010;70:668–676. doi: 10.1016/j.socscimed.2009.10.035. [DOI] [PubMed] [Google Scholar]
- Rainham DG, Bates CJ, Blanchard CM, Dummer TJ, Kirk SF, Shearer CL. Spatial Classification of Youth Physical Activity Patterns. Am J Prev Med. 2012;42:E87–E96. doi: 10.1016/j.amepre.2012.02.011. [DOI] [PubMed] [Google Scholar]
- Ridgers ND, Timperio A, Crawford D, Salmon J. Validity of a brief self-report instrument for assessing compliance with physical activity guidelines amongst adolescents. Journal of Science and Medicine in Sport. 2012;15:136–141. doi: 10.1016/j.jsams.2011.09.003. [DOI] [PubMed] [Google Scholar]
- Rodriguez DA, Cho GH, Evenson KR, Conway TL, Cohen D, Ghosh-Dastidar B, Pickrel JL, Veblen-Mortenson S, Lytle LA. Out and about: Association of the built environment with physical activity behaviors of adolescent females. Health Place. 2012;18:55–62. doi: 10.1016/j.healthplace.2011.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith G, Gidlow C, Davey R, Foster C. What is my walking neighbourhood? A pilot study of English adults’ definitions of their local walking neighbourhoods. International Journal of Behavioral Nutrition and Physical Activity. 2010:7. doi: 10.1186/1479-5868-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielman SE, Yoo EH. The spatial dimensions of neighborhood effects. Soc Sci Med. 2009;68:1098–1105. doi: 10.1016/j.socscimed.2008.12.048. [DOI] [PubMed] [Google Scholar]
- Spilsbury JC, Korbin JE, Coulton CJ. Mapping Children’s Neighborhood Perceptions: Implications for Child Indicators. Child Indicators Research. 2009;2:111–131. [Google Scholar]
- Troped PJ, Wilson JS, Matthews CE, Cromley EK, Melly SJ. The built environment and location-based physical activity. Am J Prev Med. 2010;38:429–438. doi: 10.1016/j.amepre.2009.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler BW, Cooper AR, Page AS, Jago R. Greenspace and children’s physical activity: A GPS/GIS analysis of the PEACH project. Prev Med. 2010;51:148–152. doi: 10.1016/j.ypmed.2010.06.001. [DOI] [PubMed] [Google Scholar]
- Wiehe SE, Carroll AE, Liu GC, Haberkorn KL, Hoch SC, Wilson JS, Fortenberry JD. Using GPS-enabled cell phones to track the travel patterns of adolescents. Int J Health Geogr. 2008:7. doi: 10.1186/1476-072X-7-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenk SN, Schulz AJ, Matthews SA, Odoms-Young A, Wilbur J, Wegrzyn L, Gibbs K, Braunschweig C, Stokes C. Activity space environment and dietary and physical activity behaviors: a pilot study. Health Place. 2011;17:1150–1161. doi: 10.1016/j.healthplace.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]