Dear Drs. Ravussin and Ryan
The September issue of Obesity featured articles by Tobias and Hu (1) and Flegal and Kalantar-Zadeh (2) that explored the observation that, in clinical populations, such as individuals with heart failure, chronic kidney disease, or diabetes, those with higher BMI often have lower mortality rates than leaner individuals. The articles disagree whether this phenomenon, known as the obesity paradox, is a true causal effect. Flegal and Kalantar-Zadeh assert that the research on the obesity paradox is consistent with greater BMI conferring “modest survival advantages” (2). Tobias and Hu disagree, arguing that the obesity paradox is likely an “artifact of methodological limitations” (1).
Notably absent from the discussion is selection bias, one potential explanation for the obesity paradox. Selection bias can occur when the probability of being included in a study population is influenced by the exposure and outcome, or by factors that causally affect the exposure and outcome (3). The result of this bias is that the association between exposure and outcome among those selected for analysis differs from the association among those eligible (3). Selection bias could occur if heavier, sicker patients die faster, before they can be included in studies. Selection bias could also occur if an unmeasured factor influences disease risk and is a stronger predictor of mortality than obesity (see Figure 1). For instance, assume that the study population is restricted to those with disease (e.g., diabetes), and one gets disease via only two pathways: (a) one pathway involving obesity or (b) another involving an unmeasured disease risk factor (e.g., chronic hepatitis C infection). If the mortality rate among people who have the unmeasured risk factor is greater than among those with obesity, then obesity will appear inversely associated with mortality among patients (e.g., diabetics) since all non-obese patients must have the factor (e.g., hepatitis C) associated with higher mortality.
Figure 1.
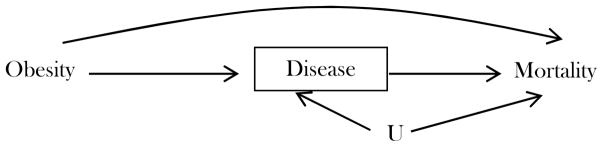
Directed acyclic graph representing causal relations between obesity, chronic disease, mortality, and unmeasured factor(s) U.
A frequently cited example of selection bias from the perinatal epidemiology literature is the birthweight paradox. Similar to the inverse association between obesity and mortality in clinical populations, maternal smoking appears protective against infant mortality in analyses restricted to low birthweight infants. The birthweight paradox led to many investigations into mechanisms underlying the seemingly protective effect of maternal smoking against infant death. However, simulation studies and causal analysis demonstrated that the protective effect of smoking was likely a spurious association induced by restricting to a clinically defined subpopulation (4). Analogously, Banack and Kaufman recently demonstrated that the obesity paradox among heart failure patients could be due to selection bias (5). Reweighting back to the average association between obesity and mortality in the total population revealed that being obese could increase mortality risk among heart failure patients even if obesity appears associated with lower mortality in conventional analyses.
Statistical methods exist to determine the possible extent of and to correct for selection bias, but have not been widely adopted. We applaud the journal’s focus on methodological considerations related to the obesity paradox and encourage future investigations into selection bias as a potential explanation for these associations.
Sincerely,
References
- 1.Tobias DK, Hu FB. Does being overweight really reduce mortality? Obesity (Silver Spring) 2013 Sep;21(9):1746–9. doi: 10.1002/oby.20602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flegal KM, Kalantar-Zadeh K. Overweight, mortality and survival. Obesity (Silver Spring) 2013 Sep;21(9):1744–5. doi: 10.1002/oby.20588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hernan MA, Hernandez-Diaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004 Sep;15(5):615–25. doi: 10.1097/01.ede.0000135174.63482.43. Epub 2004/08/17.eng. [DOI] [PubMed] [Google Scholar]
- 4.Whitcomb BW, Schisterman EF, Perkins NJ, Platt RW. Quantification of collider-stratification bias and the birthweight paradox. Paediatr Perinat Epidemiol. 2009 Sep;23(5):394–402. doi: 10.1111/j.1365-3016.2009.01053.x. Epub 2009/08/20.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Banack HR, Kaufman JS. The “obesity paradox” explained. Epidemiology. 2013 May;24(3):461–2. doi: 10.1097/EDE.0b013e31828c776c. [DOI] [PubMed] [Google Scholar]


