Abstract
Background
According to recent studies, the newest strategy for the treatment of exudative age-related macular degeneration is to combine anti-VEGF agents with non-steroid anti-inflammatory drugs (NSAIDs) such as nepafenac and bromfenac to decrease the frequency of intravitreal injections. Since most research has focused on ranibizumab, the aim of this study is to evaluate whether an alternative drug such as bevacizumab could lead to similar outcomes.
Material/Methods
The study was conducted on a group of 26 patients who were administered intravitreal bevacizumab and topical bromfenac (study group) and 26 patients with single bevacizumab therapy (control group). Cases that were not qualified for ranibizumab therapy were included in the study group.
Results
The study revealed that the visual acuity and parameters observed in OCT improved more in the study group than in the control group. However, the correlations between the above factors and the frequency of intravitreal injections were statistically significant only in visual acuity.
Conclusions
We recommend the combined therapy of bevacizumab and bromfenac as an alternative and beneficial method of treatment in patients with exudative AMD who do not qualify for ranibizumab therapy. This combined therapy might efficiently reduce the number of intravitreal injections of bevacizumab.
MeSH Keywords: Anti-Inflammatory Agents, Non-Steroidal, Macular Degeneration, Vascular Endothelial Growth Factor, Endocrine-Gland-Derived
Background
According to the worldwide guidelines for the treatment of exudative age-related macular degeneration (AMD), the use of intravitreal injections of anti-VEGF agents, such as ranibizumab (Lucentis) or bevacizumab (Avastin), is regarded as the most common therapy. However, several researchers are in favor of additional topical non-steroidal anti-inflammatory drugs (NSAIDs), such as bromfenac [1,2].
Both ranibizumab and bevacizumab are humanized monoclonal IgG1 antibodies that inhibit VEGF, which is responsible for choroidal neovascularization [3,4]. While ranibizumab (Lucentis) is registered in Poland for the treatment of the wet form of AMD and is approved by the U.S. Food and Drug Administration for this indication, bevacizumab (Avastin) is licensed for the treatment of metastatic colon cancer, diffused breast cancer, advanced and diffused renal cancer, ovarian cancer, non-small-cell lung cancer, and glioblastoma multiforme [4–7]. However, anti-VEGF therapy with the application of Avastin also acts as an off-label therapy in the treatment of AMD.
The most common regimen of the described approach refers to ranibizumab and is based on 3 initial monthly injections (the ‘loading dose’) [8]. The MARINA and ANCHOR clinical trials were the first studies in which the above scheme was found beneficial, although several limitations such as serious systemic adverse effects were mentioned. In the PIER clinical trial, loading dose was followed by quarterly injections depending on the CNV activity detected by optical coherence tomography (OCT), while the PrONTO study revealed comparable results of visual acuity after 1 year of treatment, yet with half the number of injections.
Therefore, new strategies leading to reduced injection frequency are the subject of experimental studies. For instance, it has been recently found that non-steroidal anti-inflammatory drugs can also play a major role in ophthalmology, especially in the treatment of exudative AMD [9]. The application of NSAIDs is based on their ability to suppress prostaglandin-induced inflammation, which is linked to the development and maintenance of choroidal neovascularization [10]. Bromfenac belongs to the class of non-steroidal anti-inflammatory agents, which suppress the production of prostaglandins by inhibiting cyclooxygenase (COX), the enzyme responsible for the conversion of arachidonic acid to cyclic endoperoxides, which are precursors of prostaglandins. Bromfenac and other non-steroidal anti-inflammatory drugs are approved for the treatment of inflammation after cataract surgery. Retinal levels have also been investigated after topical administration and were found to be within the therapeutic index [11].
Recent research on possible co-factors in pathogenesis of diabetic macular edema and AMD has shown that anti-VEGF agents and anti-inflammatory drugs are not the only participants in the therapeutic process. Specifically, Das states that lipoxins A4, resolvins, and protectins may prevent the development and progression of the disease. According to Das, these anti-inflammatory compounds derived from omega-3 fatty acids could be administered intravitreally. He also reports that this alternative therapy seems to be safer and less toxic [12,13].
The results of many studies reveal that due to the combined therapy, the number of injections can be limited throughout the year. Most trials evaluated intravitreal ranibizumab and topical bromfenac, and little is known about other anti-VEGF agents in the combination of NSAIDs. Therefore, the aim of our study was to evaluate the combined therapy of bevacizumab and bromfenac in patients with exudative AMD and to determine whether the treatment reduces the number of injections.
Material and Methods
The study was conducted in a group of 26 patient (16 females, 10 males, mean age 72.38 years) who received both intravitreal bevacizumab 1.25 mg (Avastin) and topical bromfenac 0.09% (Yellox) and 26 patients (16 females, 10 males, mean age 72.26 years) who were treated with bevacizumab only and were used as the control group. Basic demographic characteristics of both groups are presented in Table 1.
Table 1.
Characteristics of the groups.
| Group | Gender | Total – gender | Age | |
|---|---|---|---|---|
| Female | Male | |||
| Control group | 16 | 10 | 26 (50.0%) | 74 (median) |
| Study group | 16 | 10 | 26 (50.0%) | 74 (median) |
| Total | 32 (61.5%) | 20 (38.5%) | 52 | |
All patients signed an informed consent regarding the nature and possible consequences of the treatment and study. The research was conducted in accordance with the WMA Declaration of Helsinki.
Inclusion criteria for the study and control group were as follows: age above 50 years; active choroidal neovascularization (CNV) manifesting exudative AMD in fluorescein angiography; subretinal fluid detected by OCT (iVue, Optovue, USA); and typical image in fundus examination. All patients failed to qualify for ranibizumab therapy according to the standard qualification criteria (age above 50 years; BCVA within 0.05 and 0.9; due to active CNV; all active CNV types; location of the lesion: subfoveal and perifoveal in a case of active or with a risk of involving fovea or deteriorating visual acuity). In subjects with bilateral exudative AMD, the eye with lower visual acuity was studied. In bilateral AMD and the same VA in both eyes, the left eye was studied.
Exclusion criteria included myopia greater than -6 D, aphakia, previous ranibizumab therapy and/or vitrectomy history, other conditions that the investigator believed hazardous to a patient (e.g., active inflammation of the eyeball and ocular adnexa, recurrent chorioiditis, advanced glaucoma, stroke and myocardial infarction within the previous 6 months, and anticoagulation therapy with INR over 1.5). Vitamin supplementation and photodynamic therapy with verteporfin (PTD) were allowed.
Patients of both groups were treated with 3 initial intravitreal injections of bevacizumab (1.25 mg), followed by additional injections until 6 months, depending on the subretinal fluid leakage assessed by OCT and/or deterioration of visual acuity. Each time a minimally higher or new amount of subretinal fluid was observed on OCT examination, an additional injection was administered. Intravitreal injections were performed under standard protocol with preoperative topical anaesthesia and surface disinfection with 5% povidone-iodine solution and 0.3% ciprofloxacin eye drops (Floxal) were used 4 times daily 3 days before and 7 days after each injection.
From the day after the first dose of bevacizumab, each patient from the study group was instructed to apply 1 drop of bromfenac to the treated eye twice daily for 3 months.
Any ocular and non-ocular adverse events were assessed at all study visits.
A complete ophthalmic examination was conducted at each visit, consisting of distance best-corrected visual acuity (BCVA), slit-lamp biomicroscopy (SL-3G Topcon Corporation, Tokyo, Japan), intraocular pressure with Goldmann applanation tonometry (XPERT NCT PLUS Reichert, USA), fundus examination, and OCT. Fluorescein angiography (TRC NW8F Topcon Corporation, Tokyo, Japan) was performed at the beginning of the treatment and acted as an inclusion criteria.
For the purpose of the analysis, the following outcomes were measured at 3 stages of the study: on the day of first injection (baseline – visit 0), 4 months after (visit 1) the third dose, and 6 months (visit 2) from the start of treatment:
BCVA for distance (assessed with Snellen’s chart, than transformed into LogMar),
intraocular pressure (IOP),
central retinal thickness (CRT),
height and length of subretinal fluid.
The results were compared at each stage of the study and the number of injections was analyzed to determine the factors correlating with injection frequency.
Statistics
Statistical analysis was performed using MedCalc ver. 12.4.0.0. A ‘p’ value of less than 0.05 was regarded as statistically significant.
Descriptive statistics included mean, median, minimum and maximum value, lower and upper quartile, standard deviation, and 95% confidence interval for mean and median. The type of distribution was evaluated using D’Agostino-Pearson’s test and characteristics of a variable’s distribution were depicted in histograms with Gaussian curve. A non-parametric Mann-Whitney U-test was used to assess differences for unpaired variables and ANOVA-Friedman test for dependent variables. Multiple testing was also performed. Correlations for all variables were identified. Spearman’s rank correlation was evaluated.
Results
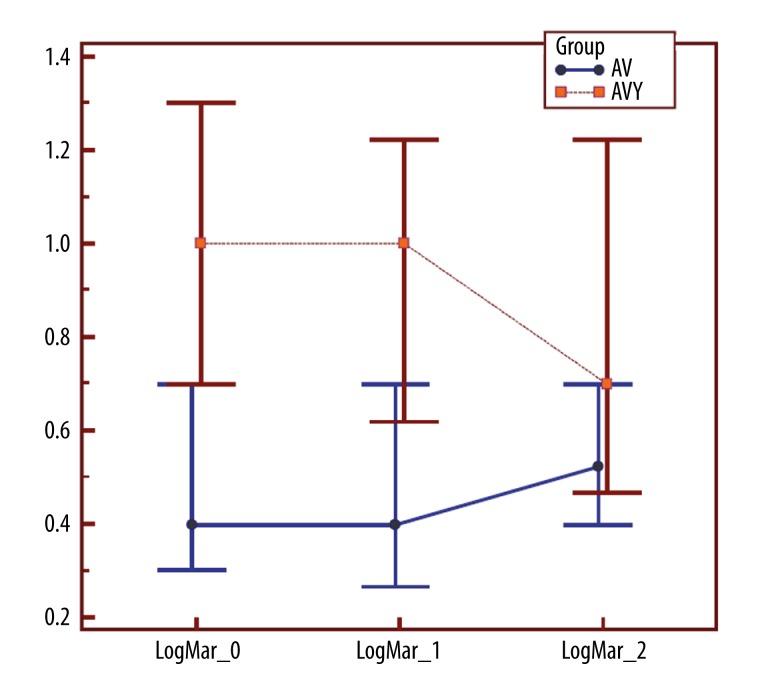
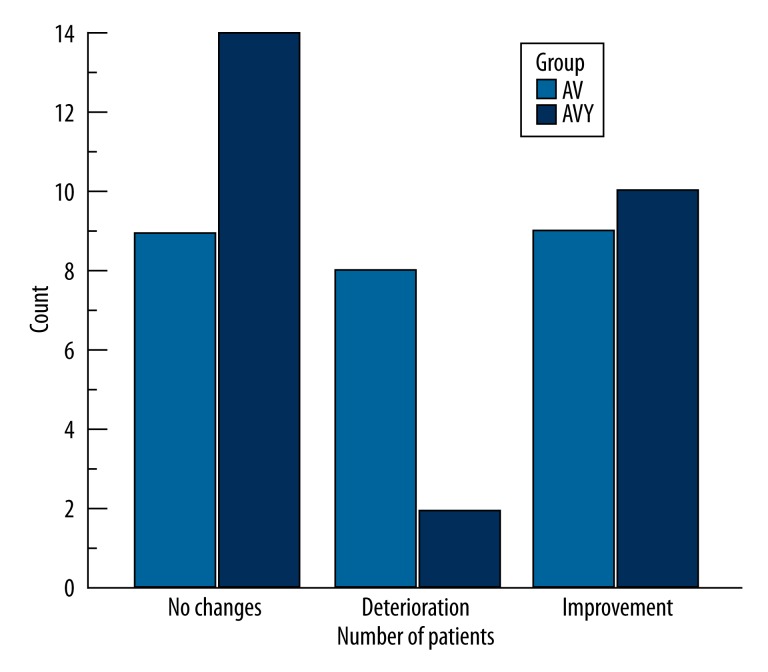
We found that visual acuity of study group patients improved significantly at visit 2, yet no differences were observed between visit 0 and 1 (Figure 1). The mean BVCA at visit 0 and 1 was about 0.1 (with a median of 0.1; 95% CI 0.05–0.2). The mean gain (measured at visit 2) was about 1 line. In 14 eyes (53.8%), unaltered visual acuity was observed. Ten eyes (38.5%) gained at least 1 line. Two subjects (7.7%) experienced vision loss (Figure 2).
Figure 1.
Visual acuity (LogMar) at visit 0, 1, and 2 for the study and control group (AV – control group, AVY – study group). For AV: p=0.302; for AVY: p=0.001 (ANOVA-Friedman test).
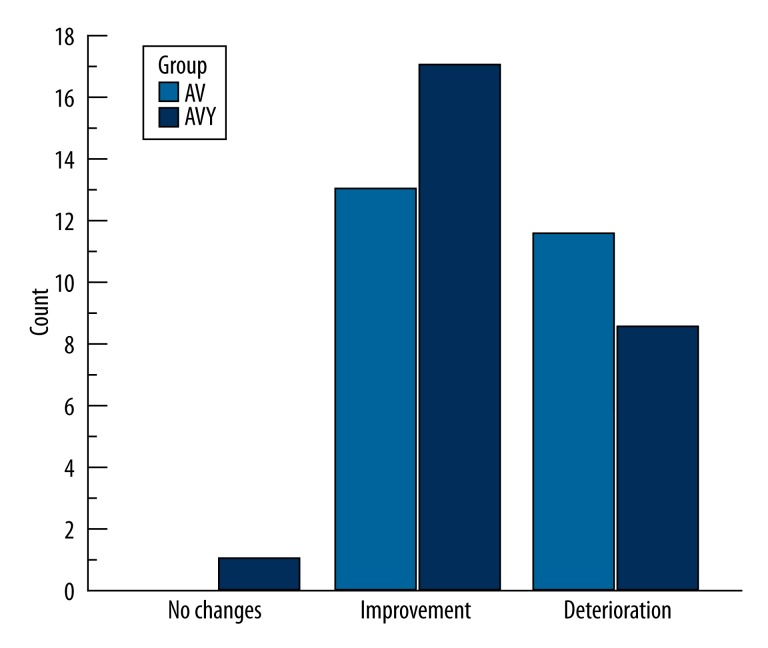
Figure 2.
Number of patients with the same, better, and worse visual acuity – comparison between visit 0 and 3 (AV – control group, AVY – study group); Mann-Whitney U-test; p=0.09.
In the control group, the comparison of the BCVA results for each visit showed statistically insignificant differences, with a median of 0.4 for visit 0 and 1 and 0.3 for visit 2 (Figure 1). We used ANOVA- Friedman test (with a=0.05) for the above assessments. The results revealed 9 (34.6%) subjects with improvement, 9 eyes with no changes, and 8 (30.8%) with deterioration of visual acuity (Figure 2). Also, positive correlations between BCVA and OCT results (CRT and height and length of subretinal fluid) and age were revealed.
Analysis of intraocular pressure (range, 13–16 mmHg) showed no significant differences within or between the groups (Table 2).
Table 2.
Intraocular pressure (IOP) between the groups (AV – control group, AVY – study group).
| Group | IOP – visit 0, 1, 2 | |
|---|---|---|
| AV | AVY | |
| N | 26 | 26 |
| Mean | 14.436 | 14.974 |
| 95% CI | 13.197–15.674 | 13.702–16.246 |
| Variance | 9.4024 | 9.9193 |
| SD | 3.0663 | 3.1495 |
| SEM | 0.6014 | 0.6177 |
| Median | 14.5 | 14.333 |
| 95% CI | 12.882–15.817 | 13.000–16.150 |
| Minimum | 7 | 10 |
| Maximum | 21 | 22 |
| 2.5–97.5 P | 7.500–20.850 | 10.150–21.850 |
| 25–75 P | 12.333–16.333 | 12.667–16.667 |
| Normal Distr. | 0.6895 | 0.3122 |
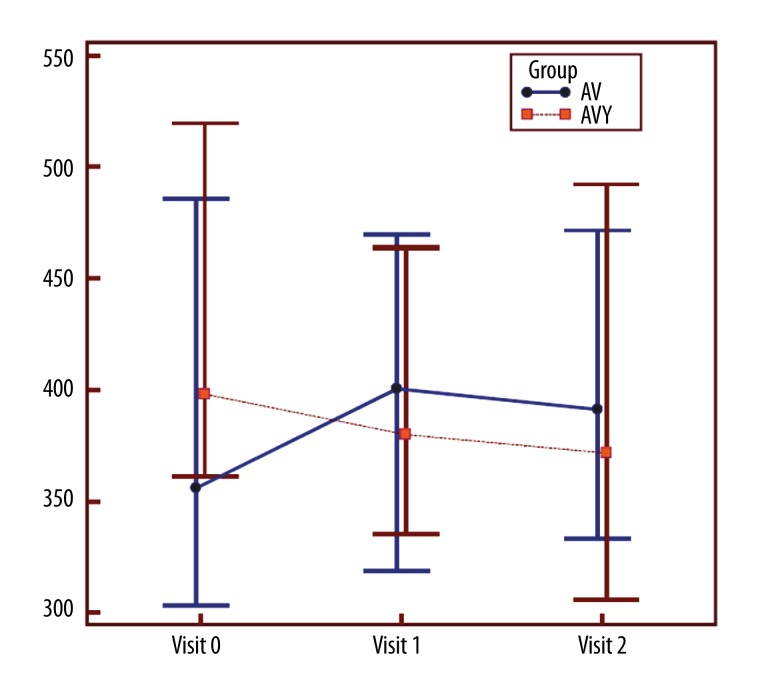
Baseline mean CRT as measured with OCT was 459 um, with a median of 398 and 95% CI of 361.293–519.414 in a study group and 419.5 um, with a median of 356 and 95% CI of 303.195–485.902 in the control group. A mean reduction of about 69.462 um was observed when comparing results from visit 0 and 2 in the study group (Figure 3). The reduction concerned 20 (76.9%) eyes. However, no reduction of CRT was revealed in the control group.
Figure 3.
CRT changes at visits 0, 1, and 2 in both groups (AVY – study group, AV – control group).
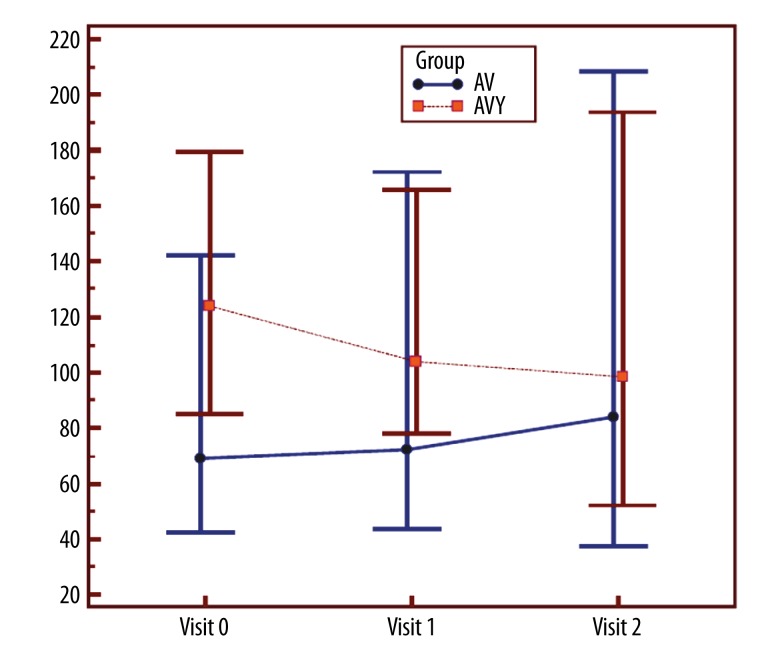
The height of subretinal fluid was measured with OCT at visit 0, 1, and 2. The median height of subretinal fluid decreased significantly in the study group and even increased in the control group (Figure 4). In the study group, there were 17 (65.4%) eyes in which the height of subretinal fluid decreased, 8 (30.8%) subjects with deterioration (i.e., higher subretinal fluid) and 1 (3.8%) eye without changes (Figure 5).
Figure 4.
Height of subretinal fluid (in um) at each visit for both groups (AVY – study group, AV – control group).
Figure 5.
Number of patients with deterioration, improvement, and no change in the height of subretinal fluid (in%) (AVY – study group, AV – control group). Chi-square test p=0.45.
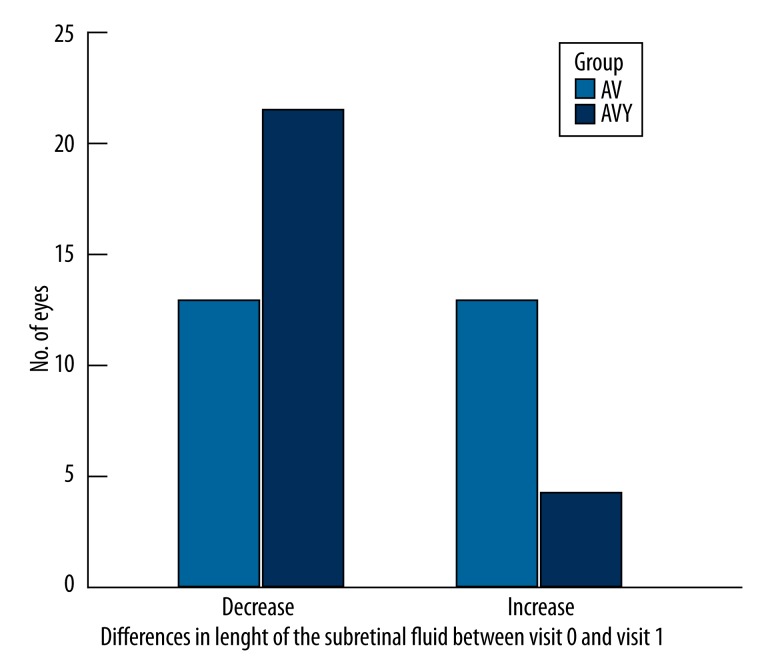
The median difference in the number of subjects in which the length of subretinal fluid changed was statistically significant (Figure 6). The length decreased in the study group and remained unchanged in the control group.
Figure 6.
The length of the subretinal fluid – differences between the groups and at visits 0 and 2 (AVY – study group, AV – control group). Chi-square test p=0.02.
An example of the changes in OCT is presented in Figures 7 and 8.
Figure 7.
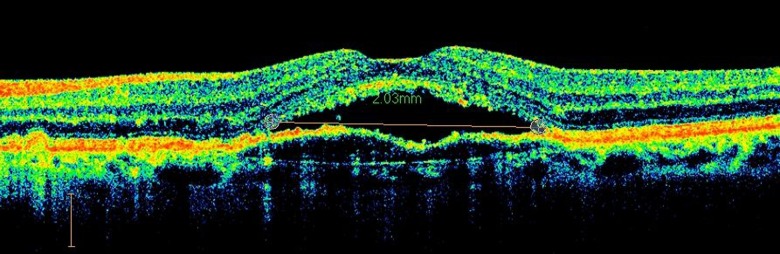
An example of the OCT examination before the therapy.
Figure 8.
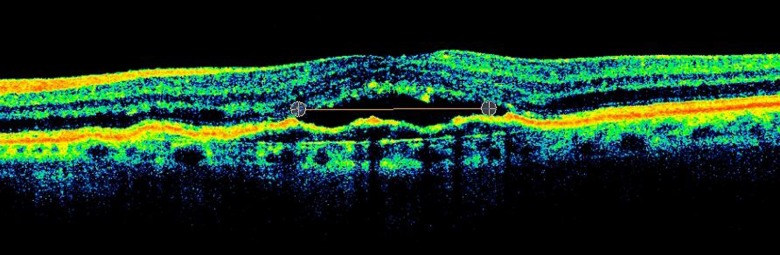
An example of the OCT examination after the combined therapy.
Analysis of the total number of injections and the number of injections between visit 1 and 2 revealed that more injections were required in the group with bevacizumab only (mean=1.346±SD 1.19) than in the group with bevacizumab and bromfenac (mean=0.885±SD 0.90). Similarly, the total number of the injections was lower in the study group (Table 3).
Table 3.
Total number of injections and number of injections between visit 1 and 2 in both groups.
| Control group | Study group | |||||
|---|---|---|---|---|---|---|
| Mean | Median | 95%CI | Mean | Median | 95%CI | |
| Total No. of injections | 6.923 | 6 | 5.000–8.000 | 5.808 | 5.5 | 4.549–6.451 |
| Injections between visit 1 and 2 | 1.346 | 1 | 0.000–2.000 | 0.885 | 1 | 0.000–1.000 |
We analyzed the correlation between BCVA and the total number of injections between visit 1 and 2 in both groups, but found no statistically significant correlations for either group.
We found a positive correlation between CRT and the number of injections, but it was statistically significant only in the control group. No significance was found in correlations between height and length of subretinal fluid and the frequency of injections in either group.
We observed no severe adverse effects in the study. Some minor symptoms were reported, such as dry eye and itchy eye. However, there was no overall difference in the number of ocular adverse events described by patients receiving bevacizumab alone and those receiving bevacizumab with bromfenac eye drops.
Discussion
The aim of all treatments used for exudative AMD is to improve or sustain visual acuity outcome. However, many therapies yield insufficient and unsatisfactory results. In addition to the combination of verteporfin photodynamic therapy with intravitreal steroids, more and more clinicians combine intravitreal anti-VEGF agents with topical non-steroid anti-inflammatory drugs. Nowak et al. reported that intravitreal bevacizumab injections (IVB) had the best efficacy in the improvement in final BCVA in comparison to transpupillary thermotherapy (TTT) and photodynamic therapy (PDT) [14]. However, one of the greatest limitations of anti-VEGF therapy is that it requires multiple injections [15]. Therefore, scientists try to introduce additional forms of treatment, such as topical NSAIDs. Because there are no publications regarding bevacizumab and bromfenac, for the purpose of further discussion, we emphasize that all comparisons refer to publications in which ranibizumab was used, because efficacy of these 2 therapies is regarded as equal [16,17].
Due to the inclusion criteria, the study group required much more intensified treatment and observation in comparison to patients treated with ranibizumab. The initial parameters of BCVA, CRT, and subretinal fluid were worse in the subjects who received bevacizumab therapy; therefore, predicted outcomes were unsatisfactory from the beginning. Since there are many patients receiving bevacizumab in Poland, we wanted to know if the combined therapy with bromfenac would be clinically beneficial; if so, the increase in the number of injections would therefore be economically beneficial for patients.
Grant et al. reported that injection frequency of ranibizumab used together with topical bromfenac was much lower (1.6±0.69) than in the group of patients who received ranibizumab alone (4.5±0.41) [18]. Gomi et al. confirmed these findings (mean number of injections for the study group=2.2 and for the sham group=3.2), indicating that topical bromfenac might reduce the number of injections of ranibizumab during 6 months eyes with relatively mild AMD lesions [19]. The conclusions of other authors mentioned above agree with our outcomes, but with a smaller ratio between the results (median number of injections was 5.5 for the study group and 6 for the control group). The reason for this may be patients’ initial poor parameters and advanced clinical staging.
Although there is no evidence to recommend using NSAIDs for prophylaxis or treatment of AMD, several authors have observed that patients taking aspirin were significantly less likely to develop neovascular AMD [20]. Furthermore, it has been found that patients with rheumatoidal diseases, who were given NSAIDs, were less likely to have AMD [21].
For visual acuity, most studies on intravitreal ranibizumab and topical NSAIDs showed improved therapy results. However, the tendencies show that the proper aim of this treatment is to sustain the BCVA [8,22].
We found slight differences (1 line) when the results from baseline and last visit were compared. Biarnes et al., who studied a group of 67 subjects treated with ranibizumab, reported that 70.1% of eyes remained stable or gained vision: 13.4% gained 3 or more lines of BCVA and 6% gained more than 6 lines of visual acuity [8]. Similarly, the reason for that difference between our study and the above study might be the poor initial visual parameters of our patients.
Another fact that should be taken into consideration is the lesion’s characteristics as evaluated with OCT (i.e., central retinal thickness (CRT) and subretinal fluid).
Baseline mean CRT in our study was 459 um, which is greater than that reported by Gomi et al. (mean CRT=365 um) and Biarnes et al. (mean CRT=329.5 um) [8,19], but the mean reduction of CRT was more satisfactory in our study (69.46 um) than that reported by Biarnes (44.6 um). However, in all studies the reduction was greater in the group with combined therapy than in the control group [8,19]. No correlations between CRT changes and the number of injections were evaluated in other publications, so it is difficult to form precise conclusions on that topic.
Although the height and length of the subretinal fluid diminished in the study group, it seems that the results do not correlate with the frequency of injections of bevacizumab. Also, it is difficult to compare our outcomes with others, as there are no publications regarding that parameter of OCT.
A long-term follow-up of all patients treated in our clinic shows that further injections do not improve visual acuity, but led to stable visus and efficiently reduced exudation. Similar findings were reported by other studies [22,23].
Conclusions
We could not detect a statistically significant beneficial effect of the combination therapy. However, this should be regarded as a pilot study that needs further observations before precise conclusions can be made. However, the possible reason for this outcome might be the relatively small number of subjects. Also, the differences between our findings and those of other authors who studied ranibizumab may be the result of initial differences in visual state of the eyes disqualified from Lucentis therapy and therefore having lower BCVA and worse retinal parameters.
We firmly believe that combining anti-VEGF therapy and NSAIDs might decrease the number of intravitreal injections needed in the first stage of treatment. This would improve patient quality of life and cost of therapy.
Acknowledgements
We would like to give thanks to Mr. Marek Pieczara and Tomasz Mozdyniewicz MD for their assistance in statistical analysis.
Footnotes
Source of support: Self financing
References
- 1.Flaxel C, Schain MB, Hamon SC, Francis PJ. Prospective randomized controlled trial of combination ranibizumab (Lucentis) and bromfenac (Xibrom) for neovascular age-related macular degeneration: a pilot study. Retina. 2012;32(3):417–23. doi: 10.1097/IAE.0b013e318229b0af. [DOI] [PubMed] [Google Scholar]
- 2.Schalnus R. Topical nonsteroidal anti-inflammatory therapy in ophthalmology. Ophthalmologica. 2003;217(2):89–98. doi: 10.1159/000068563. [DOI] [PubMed] [Google Scholar]
- 3.Lynch SS, Cheng CM. Bevacizumab for neovascular ocular diseases. Ann Pharmacother. 2007;41:614–25. doi: 10.1345/aph.1H316. [DOI] [PubMed] [Google Scholar]
- 4.Van Meter ME, Kim ES. Bevacizumab: current updates in treatment. Curr Opin Oncol. 2010;22:586–91. doi: 10.1097/CCO.0b013e32833edc0c. [DOI] [PubMed] [Google Scholar]
- 5.Strickler JH, Hurwitz HI. Bevacizumab-Based Therapies in the First-Line Treatment of Metastatic Colorectal Cancer. Oncologist. 2012;17(4):513–24. doi: 10.1634/theoncologist.2012-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stevenson CE, Nagahashi M, Ramachandran S, et al. Bevacizumab and breast cancer: what does the future hold? Future Oncol. 2012;8(4):403–14. doi: 10.2217/fon.12.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Su Y, Yang WB, Li S, et al. Effect of angiogenesis inhibitor bevacizumab on survival in patients with cancer: a meta-analysis of the published literature. PLoS One. 2012;7(4):e35629. doi: 10.1371/journal.pone.0035629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Biarnes M, Mones J, Villali JR, Arias L. As-needed treatment with ranibizumab 0.5 mg in patients with neovascular age-related macular degeneration. Eur J Ophthalmol. 2011;21(3):282–89. doi: 10.5301/EJO.2010.5766. [DOI] [PubMed] [Google Scholar]
- 9.Kim SJ, Flach AJ, Jampol LM. Nonsteroidal anti-inflammatory drugs in ophthalmology. Surv Ophthalmol. 2010;55(2):108–33. doi: 10.1016/j.survophthal.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Warren KA, Bahrani H, Fox JE. NSAIDs in combination therapy for the treatment of chronic pseudophakic cystoid macular edema. Retina. 2010;30(2):260–66. doi: 10.1097/iae.0b013e3181b8628e. [DOI] [PubMed] [Google Scholar]
- 11.Chen E, Benz MS, Fish RH, et al. Use of nepafenac (Nevanac) in combination with intravitreal anti-VEGF agents in the treatment of recalcitrant exudative macular degeneration requiring monthly injections. Clin Ophthalmol. 2010;4:1249–52. doi: 10.2147/OPTH.S14092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Das UN. Is lipoxins A4 a better alternative to anti-VEGF and anti-TNF-α antibody to prevent and treat age-related macular degeneration, diabetic macular edema and retinopathy? Med Sci Monit. 2012;18(1):LE1–2. doi: 10.12659/msm.882187. [DOI] [PubMed] [Google Scholar]
- 13.Das UN. Lipoxins, resolvins, and protectins in the prevention and treatment of diabetic macular edema and retinopathy. Nutrition. 2013;29(1):1–7. doi: 10.1016/j.nut.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Nowak MS, Jurowski P, Grzybowski A, et al. A prospective study on different methods for the treatment of choroidal neovascularization. The efficacy of verteporfin photodynamic therapy, intravitreal bevacizumab and transpupillary thermotherapy in patients with neovascular age-related macular degeneration. Med Sci Monit. 2012;18(6):CR374–80. doi: 10.12659/MSM.882907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zweifel SA, Engelbert M, Khan S, Freund KB. Retrospective review of the efficacy of topical bromfenac (0.09%) as an adjunctive therapy for patients with neovascular age-related macular degeneration. Retina. 2009;29(10):1527–31. doi: 10.1097/IAE.0b013e3181b32f4c. [DOI] [PubMed] [Google Scholar]
- 16.Royal College of Ophthalmologists. Royal College of Ophthalmologists’ Press Statement. College Statement on CATT Study 04/05/2011. [(accessed 23 August 2011)]. http://www.rcophth.ac.uk/news.asp7section=24§ionTitle=News&itemid=427.
- 17.Macular Degeneration Foundation. CATT study raises more questions than it answers. [(accessed 23 August 2011)]. www.mdfoundation.com.au.
- 18.Grant CA. Combination therapy: lucentis (ranibizumab injection) and xibrom (bromfenac ophthalmic solution) 0.09% in the treatment of choroidal neovascular membrane secondary to age-related macular degeneration. Invest Ophthalmol Vis Sci. 2008:49. (E-Abstract 563) [Google Scholar]
- 19.Gomi F, Sawa M, Tsujikawa M, Nishida K. Topical bromfenac as an adjunctive treatment with intravitreal ranibizumab for exudative age-related macular degeneration. Retina. 2012;32(9):1804–10. doi: 10.1097/IAE.0b013e31825be87f. [DOI] [PubMed] [Google Scholar]
- 20.Kim SJ, Flach AJ, Jampol LM. Major review. Nonsteroidal Anti-inflammatory Drugs in Ophthalmology. Surv Ophthalmol. 2010;55(2):108–33. doi: 10.1016/j.survophthal.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 21.McGreen PL, Sibley J. Sparing of age-related macular degeneration in rheumatoid arthritis. Neurobiol Aging. 2005;26(8):1199–203. doi: 10.1016/j.neurobiolaging.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Figurska M, Stankiewicz A. Effectiveness of ranibizumab intravitreal injections for exudative age-related macular degeneration treatment: 12-month outcomes. Med Sci Monit. 2011;17(9):CR485–90. doi: 10.12659/MSM.881934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lukács R, Resch M, Papp A, et al. Long-term treatment with intravitreal ranibizumab for exudative age-related macular degeneration. Orv Hetil. 2013;154(45):1790–97. doi: 10.1556/OH.2013.29729. [DOI] [PubMed] [Google Scholar]