Abstract
Over the past 5 years, many novel approaches to early diagnosis, prevention, and treatment of acute graft-versus-host disease (aGVHD) have been translated from the bench to the bedside. In this review, we highlight recent discoveries in the context of current aGVHD care. The most significant innovations that have already reached the clinic are prophylaxis strategies based upon a refinement of our understanding of key sensors, effectors, suppressors of the immune alloreactive response, and the resultant tissue damage from the aGVHD inflammatory cascade. In the near future, aGVHD prevention and treatment will likely involve multiple modalities, including small molecules regulating immunologic checkpoints, enhancement of suppressor cytokines and cellular subsets, modulation of the microbiota, graft manipulation, and other donor-based prophylaxis strategies. Despite long-term efforts, major challenges in treatment of established aGVHD still remain. Resolution of inflammation and facilitation of rapid immune reconstitution in those with only a limited response to corticosteroids is a research arena that remains rife with opportunity and urgent clinical need.
Introduction
Acute graft-versus-host disease (aGVHD) is a frequent and at times unpredictably severe inflammatory complication of allogeneic hematopoietic cell transplantation (HCT). Despite over 5 decades of extensive laboratory and clinical investigation into methods to prevent severe aGVHD, this complication remains a significant cause of morbidity and mortality in allogeneic HCT recipients. Each year, ∼6800 patients undergo HCT (Center for International Blood & Marrow Transplant Research [CIBMTR] data), and the majority will suffer some manifestations of aGVHD. Several advancements have led to novel aGVHD detection, prophylaxis, and treatment methods. In this review, we highlight aGVHD advancements in the context of current care. With many new modalities that target host and donor responses under investigation, an era of multimodal, personalized immunomodulation in HCT may emerge. However, significant challenges to elimination of aGVHD remain. These include developing treatment regimens that retain infectious immunity and graft-versus-tumor effects, as well as identification of effective therapy for steroid-refractory aGVHD.
The classic description of aGVHD pathophysiology begins with activation of host antigen-presenting cells (APCs) by danger signals expressed on damaged tissues (damage-associated molecular patterns [DAMPs]) and/or pathogens (pathogen-associated molecular patterns [PAMPs], eg, lipopolysaccharide).1 Activated host APCs then present host antigens to donor T cells, leading to alloactivation and inflammatory cytokine release. These inflammatory cytokines then recruit and induce proliferation of additional immune effector cells, perpetuating the cycle of alloreactive tissue injury and inflammation. Although a simplified description of the complexity underlying graft-versus-host (GVH) interactions,2 it is the established foundation for disentangling the pathways involved. A more detailed overview of each phase of acute GVHD (the initiation, lymphocyte trafficking, expansion and effector, and treatment phases) will serve as background for emerging, novel diagnostic and therapeutic approaches.
Initiation phase
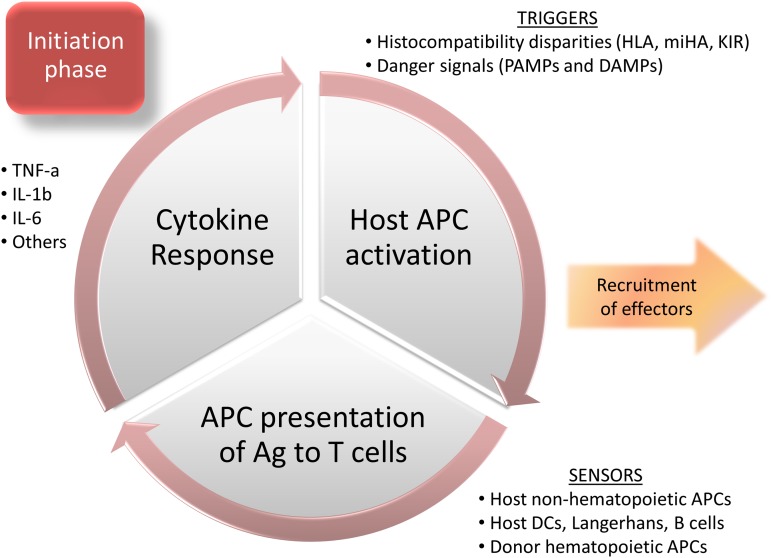
The initiation phase of aGVHD broadly involves triggers and sensors of GVH reactions (Figure 1). Many aGVHD triggers have been identified, with the most critical being disparities in major histocompatibility antigens (reviewed in detail by Petersdorf3). HLA-matched donors are not available for all eligible HCT recipients, making the identification of permissive mismatches of clinical interest. Several high-risk HLA allele mismatch combinations associated with severe aGVHD have been identified,4 although a provocative update suggests that HLA allele mismatches have had a lesser impact on outcomes in recent years (2002 and beyond) compared with HCT pre-2002.5 Recently, the identification of amino acid substitutions at peptide-binding pockets of HLA class I molecules HLA-B and HLA-C has been associated with increased GVHD risk.6 This report suggests that unrelated donor selection might be enhanced by avoiding donor/recipient amino acid substitutions at positions 99 and 116 of HLA-C, and at position 9 of HLA-B.6 In addition, avoiding mismatches at low expression loci (HLA-DP, DQ, and DRB3/4/5) could help further reduce adverse outcomes in 7 of 8 mismatched unrelated HCT.7 Minor histocompatibility antigens (miHAs) are also implicated as GVHD triggers, particularly in HLA-matched siblings. The best-described miHA differences involve immune responses against Y-chromosome–encoded antigens elicited in female to male HCT, leading to the preferential selection of male donors.8 Differences in autosomal miHA, especially HA-8 mismatches in related donor HCT, have also been associated with aGVHD.9 Finally, donor/recipient differences in killer immunoglobulin-like receptor (KIR) and KIR-ligand interactions can alter the risk of aGVHD,10 adding complexity to the immunogenetic determinants.
Figure 1.
Initiation phase of aGVHD.
Several nongenetic triggers of aGVHD have been identified, predominantly danger signals: DAMPs and/or PAMPs. DAMPs include extracellular matrix components, adenosine triphosphate (ATP), and uric acid. Heparan sulfate, a component of extracellular matrix and endogenous Toll-like receptor 4 (TLR4) agonist, can promote alloreactive T-cell responses, is elevated in both murine and human GVHD, but is not increased by tissue damage related to conditioning.11 Heparan sulfate levels and GVHD severity could both be reduced by α1-antitrypsin treatment in a murine model.11 ATP released by dying cells can also induce inflammatory responses, and ATP neutralization or blockade of its receptor on immune cell subsets, P2X7R, reduced experimental GVHD.12 Uric acid can act as a DAMP, leading to NLRP3 inflammasome-mediated interleukin-1β (IL-1β) production, a key cytokine involved in aGVHD pathophysiology.13 In addition to endogenous danger signals, bacterial14 and viral15 PAMPs can both contribute to the inflammatory milieu. The role of danger signals and pattern recognition receptors in GVHD has been recently reviewed.16 Interestingly, not all PAMPs cause detrimental immune responses in aGVHD. Flagellin, a component of bacterial flagella and TLR5 agonist, has been shown to reduce GVHD while enhancing immune reconstitution in experimental HCT.17
APCs are the predominant sensors of GVHD-initiating signals. APCs capable of contributing to GVH reactions include residual host hematopoietic APCs that remain viable after the conditioning regimen, host nonhematopoietic APCs, and donor APCs transferred with the allograft. Because they are central to the initiation of GVHD,18,19 targeting host APCs is an attractive GVHD prevention strategy. However, recent animal models have challenged this dogma, as depletion of host dendritic cells (DCs),20 Langerhans cells,21 and B cells22 failed to prevent experimental GVHD. In contrast, depletion of host macrophages from lymphoid organs was shown to exacerbate GVHD, revealing an unexpected protective role.23 Therefore, it has been unclear which APC subsets are most critical for the initiation phase of aGVHD. Recent evidence suggests that nonhematopoietic APCs are the most potent GVHD inducers by 100- to 1000-fold, rendering host and donor professional hematopoietic APCs redundant or at least nonessential in GVH reactions.24 How to apply prophylaxis strategies related to this recent finding is not yet known.
Lymphocyte trafficking, expansion, and effector phase
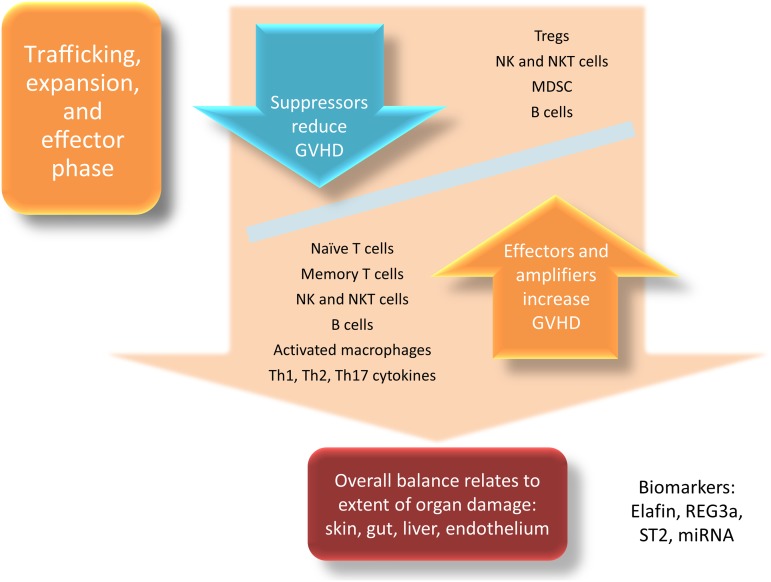
The net result of the initiation phase of aGVHD is the cytokine response made by sensors resulting in recruitment and activation of donor T cells which home to secondary lymphoid organs (nodes plus submucosal gastrointestinal and pulmonary sites) and proliferate. The effector phase of aGVHD consequently begins when cytolytic donor effector T cells, neutrophils, natural killer cells (NKs), NK T cells (NKTs), and macrophages begin to cause end-organ damage in a reaction that overwhelms any tolerance-promoting response from suppressor cells (Figure 2). Donor T cells are the best-studied effectors of aGVHD, and most prophylaxis and treatment strategies are aimed at attenuating their function. T-cell activation requires 2 stimulatory signals. First, the T-cell receptor (TCR) must be engaged and recognize antigens in the context of HLA. Recently, a small population of T cells expressing dual TCRs, potentially resulting from stochastic processes during thymic selection, was found to be disproportionately responsible for alloreactivity in human GVHD.25 Next, T cells must receive adequate costimulation from APCs to become activated and acquire effector functions. Many costimulatory ligand/receptor interactions and their involvement in aGVHD have been described, including the B7/CD28/CTLA4, CD30/CD30L, CD40/CD40L, OX40/OX40L, and ICOS/ICOS-L pathways (recently reviewed by Briones et al26). Once activated, these alloreactive T cells can proliferate and migrate in response to an inflamed environment27 and the activation of chemokine receptors, including CCR2,28 CCR5,29 CCR6,30 and CCR731 among others (reviewed by Kittan and Hildebrandt32). Homing of activated T cells to target tissues may yield change in these cell subsets in the peripheral blood. For example, fewer circulating CCR6+ T cells have been observed in patients with aGVHD due to homing toward CCL20+ target tissues.33 Similarly, fewer circulating CD8+CD45RA+β7 integrin+ T cells have also been observed in allogeneic HCT recipients experiencing gastrointestinal GVHD,34 although increased memory CD8+α4β7 integrin+ T cells have also been observed at the onset of aGVHD.35 Naïve donor T cells are central for clinical aGVHD manifestations.36,37 Memory T-cell subsets are less alloresponsive and do not appear to initiate GVHD to the same degree.38-40 However, even if less important as initiators of aGVHD, memory T cells may perpetuate GVH reactions.41
Figure 2.
Expansion, trafficking, and effector phase of aGVHD.
Other immune effector cells have inflammatory roles in the pathophysiology of aGVHD, including neutrophils, NKTs, NKs, B cells, and mononuclear phagocytes, although their individual contributions to aGVHD reactions in humans can be difficult to isolate. Neutrophils engraft rapidly after allogeneic HCT and are secondary effectors of GVHD, recruited into target organs by cytokines including IL-8.42 Indirect evidence supports an inflammatory role of neutrophils in GVHD given the observation of increased rates of acute and chronic GVHD with granulocyte colony-stimulating factor administration post-HCT.43,44 Regarding NKs, bioluminescence studies have demonstrated rapid trafficking and homeostatic proliferation of NKs in a manner similar to allogeneic T cells after infusion, although NKs did not cause GVHD in this model.45 Classically, NKs have been implicated as a component of the effector phase in descriptions of GVHD pathophysiology,46 although in clinical HCT, an increased allograft NK dose is associated with less severe aGVHD,47 possibly due to host APC depletion by donor NKs. A contribution from B cells in the pathogenesis of human aGVHD is possible considering reports of a reduced incidence of aGVHD with B-cell depletion48,49 and reduced risks of chronic GVHD after rituximab-containing conditioning regimens.50 Finally, activated macrophages can be observed colocalized with T cells in areas of highest macrophage migration inhibitory factor expression in GVHD target organs,51 adding to the cytolytic effector-induced tissue damage during this phase of aGVHD.
Conversely, several cell populations have been demonstrated to function as suppressors of GVH reactions, dampening inflammation and promoting tolerance. Intense current investigation involves regulatory T cells (Tregs), with extensive preclinical and emerging clinical reports of their function in prevention and treatment of aGVHD.52-54 Tregs are CD4+ T cells that function to suppress runaway immune responses mediated by mature APCs and effector T cells.55 Mechanisms of Treg suppression of GVHD are pleiotropic and only partially known, but include downregulation of aGVHD-associated TLR5 expression.56,57 Another recently described CD4+ T-cell subset, T helper 9 (Th9) cells, secrete IL-9 and dampen interferon-γ–mediated GVHD while preserving graft-versus-tumor effects in a murine model.58 Whether this subset can suppress human aGVHD is not yet known. Myeloid-derived suppressor cells (MDSCs) can also mitigate GVHD via multiple mechanisms.59,60 Finally, even though these subsets have potential pathogenic roles in aGVHD, NKs,61 NKTs,62 B cells,63 and macrophages23 can also play tolerogenic roles in HCT, which adds further complexity to the landscape of effectors and suppressors of aGVHD.
The final components of the effector phase of aGVHD are cytokines. They can amplify or attenuate GVH reactions, and the balance between proinflammatory and anti-inflammatory cytokines (as opposed to differing concentrations of a single cytokine) shapes the overall milieu and GVHD response (reviewed by Reikvam et al64). The prototypic effector cytokines in aGVHD are tumor necrosis factor α (TNF-α), IL-1β, and IL-6, although IL-17,65 IL-23,66 and Th2 cytokines67 can also enhance the inflammatory milieu, depending upon organ involvement and other factors.
During the effector phase of aGVHD, inflammation escalates rapidly and target tissues are damaged. The inflammatory cascade and continued tissue damage can lead to release of biomarkers of aGVHD into the circulation, reflecting both effector activation and tissue injury. These biomarkers include soluble CD30 from activated T cells,68 elafin (skin-specific),69 regenerating islet-derived 3-α (REG3α; gut-specific),70 suppressor of tumorigenicity 2 (ST2; a member of the IL-1 receptor family–binding IL-33),71 microRNA,72 and others (reviewed by Paczesny73), even before the onset of clinical signs of aGVHD become apparent and potentially predicting therapy responses.
Treatment phase
At present, clinicians rely on history, physical examination, and routine clinical laboratory parameters to determine when treatment of aGVHD must commence. The classic target organs of aGVHD are the skin (severity ranging from maculopapular rash to erythroderma and bullae formation), the gastrointestinal tract (resulting in nausea, vomiting, abdominal cramps, and/or diarrhea), and the liver (resulting in hyperbilirubinemia, jaundice, and/or elevated transaminases). The hematopoietic system can also be targeted, resulting in complete donor lymphohematopoietic chimerism and the graft-versus-tumor response against hematologic malignancies. Endothelium,74,75 lungs, and other organs can also be targeted, although skin, gut, and liver involvement are the only organs scored in the current grading system.76 Clinical laboratory clues regarding the onset of aGVHD frequently include lymphopenia,77 eosinophilia,78 thrombocytopenia,79 and hypoalbuminemia.77 Histologic confirmation is routinely obtained to rule out opportunistic infections or other alternate explanation for the clinical symptoms, though the classic (mostly apoptotic) histologic findings of aGVHD are somewhat nonspecific and can be mimicked by conditioning regimen injury, infections, and other syndromes. Noninvasive imaging modalities that visualize processes at the cellular level may be a component of future GVHD diagnostic and monitoring techniques, but are not reliably accepted or available at the moment.80,81 The decision to treat is based upon severity of symptoms, with grade 1 skin involvement typically treated only with topical corticosteroids. For those requiring systemic therapy, the standard first-line treatment is oral or IV corticosteroids.
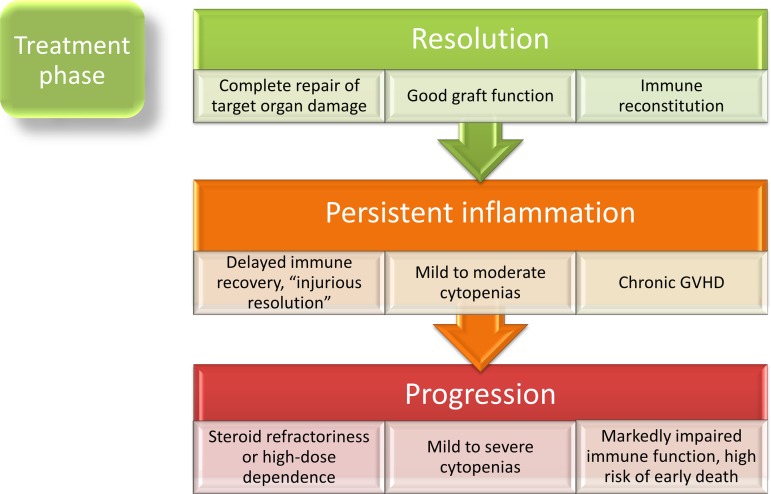
Once treatment begins, 3 primary immunologic outcomes are possible: the aGVHD inflammatory response (1) is completely resolved after therapy, (2) partially responds clinically, but incompletely resolves immunologically, leading to what may be a persistent state of “injurious resolution,”82 or (3) progresses despite therapy (Figure 3). It is not entirely known how steroids resolve aGVHD, but their lympholytic effects as well as alteration in cell adhesion molecules and chemokines in target organs are involved in reducing signs of GVHD.83 Symptoms can regress rapidly (within days), unless the patient is refractory, and plasma biomarkers of aGVHD respond accordingly.84 Reduction in lymphocyte and monocyte counts may be expected to a degree with corticosteroid therapy, although severe leukopenia (<200 cells/μL) and a major (median 10-fold) decrease of total circulating leukocytes during acute GVHD treatment are associated with a significantly lower likelihood of response to first-line therapy.85 In the wake of severe aGVHD, many patients are left with compromised hematopoietic and immune function, endothelial damage,86 and an increased risk of death even if without ongoing aGVHD signs and symptoms.87 In these patients, chronic GVHD can emerge through a variety of incompletely understood mechanisms that may include failure of NKs to eradicate CD4+ cells undergoing constant antigenic stimulation.88
Figure 3.
Treatment phase of aGVHD.
It is difficult to predict at the onset of aGVHD who will respond fully or partially to first-line therapy, or who will be refractory. Approximately half of patients will not achieve a sustained complete response of aGVHD to first-line therapy with steroids,89 and timely determination of steroid nonresponse is important for institution of salvage therapies. Those at higher risk of treatment failure have been identified clinically as those with hyperacute GVHD,90 sex-mismatched HCT,90 or with a certain constellation of organ involvement.91 A recently described biomarker, ST2, the receptor for IL-33,71 correlates with resistance to initial GVHD therapy and death.92 During uncontrolled inflammation in refractory disease, additional rising biomarkers of epithelial cell death can be observed,93 macrophages heavily infiltrate into the skin in response to continued inflammation,94 and the chance of long-term survival drops dramatically. Survival is poor in steroid-resistant aGVHD, ∼15% at 2 years.90
Update in prevention and treatment
Prophylaxis
Based upon extensive preclinical studies in canines, post-HCT methotrexate (MTX) was the first widely used GVHD prophylaxis drug in clinical HCT,95 followed by cyclosporine (for historical perspective of early trials, see review by Vogelsang et al96). MTX and cyclosporine exert their antiproliferative effects on donor T cells by interfering with purine synthesis and calcium-dependent signal transduction pathways downstream of the TCR, respectively. Tacrolimus, with mechanism of action similar to cyclosporine, came to the fore in the 1990s showing similar or superior efficacy to cyclosporine in prospective, comparative trials97 and now is widely used in clinical HCT.
Today, the backbone of most T-cell replete conventional aGVHD prophylaxis regimens includes 2 drugs: (1) a calcineurin inhibitor plus (2) MTX or mycophenylate mofetil (MMF), the latter used more frequently in nonmyeloablative regimens and umbilical cord blood transplants.98 Steroids are typically not used as prophylaxis due to lack of proven benefit.99 Sirolimus, a mammalian target of rapamycin inhibitor, has also been demonstrated to have an impact in the treatment and prophylaxis of aGVHD. Comparison between sirolimus/tacrolimus to standard MTX/tacrolimus in a single-center study demonstrated an improved rate of aGVHD-free survival in the first 100 days posttransplant (43% vs 89%, P < .001).100 However, a multicenter, randomized phase 3 trial comparing these 2 regimens (Blood and Marrow Transplant Clinical Trials Network [BMT CTN] clinical trial 0402) did not show a significant difference in the primary end point of 114-day aGVHD-free survival. Furthermore, an increase in endothelial injury syndromes was observed in the sirolimus/tacrolimus arm, particularly following busulfan-containing conditioning.101,102
Additional methods of GVHD prophylaxis include T-cell depletion (ex vivo, ie, CD34+ positive selection or through T-cell subset depletion methods targeting CD3, α-β T cells,103 or in vivo via administration of antithymocyte globulin or alemtuzumab). Graft manipulation by CD34 selection decreases the numbers of T cells in the graft by several logs, although this alone does not completely abrogate aGVHD. This is particularly important in haploidentical HCT, where further immune modulation is required to avoid lethal GVHD given the significant HLA mismatch. High-dose cyclophosphamide (Cy) administered after stem cell infusion is currently used commonly in this setting, relying on the premise of direct lytic depletion of rapidly proliferating T cells with concomitant sparing of stem cells and regulatory T cells, possibly due to differential aldehyde dehydrogenase expression (higher in stem cells and Tregs).104 This simple in vivo graft manipulation is able to break the HLA barrier by allowing the infusion of haploidentical donor cells with similar or reduced rates of aGVHD compared with transplants using HLA-matched grafts.105,106
The results of these studies, as well as the results of 3 recently published novel though preliminary aGVHD prophylaxis trials, have prompted new multicenter comparative clinical trials. First, a phase 1/2 study of maraviroc, a CCR5 inhibitor that blocks lymphocyte chemotaxis while preserving effector functions, demonstrated very low rates of grade II-IV acute GVHD (∼15%) and no visceral GVHD at day 100 post-HCT in 35 evaluable patients.107 Infection and relapse rates were not significantly increased. Next, addition of bortezomib, an NF-κB–inhibiting immunomodulator, given on days +1, +4, and +7 in addition to standard tacrolimus and MTX in mismatched unrelated donor HCT, resulted in a day 180 cumulative incidence of grade II-IV aGVHD of 22%, notable given the mismatch donor source.108 Finally, a phase 1/2 study of vorinostat, used for its tolerogenic effects on APCs109 and apoptotic effects on alloreactive T cells,110 given from 10 days prior to transplant through day +100 in addition to the backbone of tacrolimus and MMF-based prophylaxis, resulted in a grade II-IV aGVHD rate of only 22% by day 100.111
Based upon the above studies, the BMT CTN is implementing 2 trials to identify optimal prophylaxis approaches. The first is in the setting of reduced-intensity conditioning, comparing 3 novel approaches: addition of maraviroc or bortezomib to a tacrolimus/MTX platform vs posttransplant Cy follow by tacrolimus/MMF. This trial (BMT CTN 1203) is a phase 2 trial that will compare the outcomes of a novel composite end point of GVHD-free, relapse-free survival to a contemporaneous control population receiving tacrolimus/MTX identified from the CIBMTR database. The second trial (BMT CTN 1301) is a 3-arm phase 3 that compares 2 approaches without calcineurin inhibitors (CD34+ cell selection and posttransplant Cy) to a standard tacrolimus/MTX approach in HLA-matched HCT using myeloablative conditioning. These 2 trials are part of the PROGRESS (Prevention and Reduction of GVHD and Relapse and Enhancing Survival after Stem Cell Transplant) initiative in the BMT CTN.
At present, several GVHD prophylaxis trials are ongoing, including sirolimus, cyclosporine plus MMF prior to nonmyeloablative HCT (NCT01251575), ustekinumab (IL-12/23 antagonist) in addition to a tacrolimus/sirolimus backbone (NCT01713400), bortezomib in addition to cyclosporine/MTX in pediatric HCT (NCT01926899), brentuximab vedotin (targeting CD30) in addition to tacrolimus plus MTX for mismatched HCT (NCT01700751), atorvastatin (NCT01665677), CD45RA+ (naïve) T-cell graft depletion (NCT01858740), extracorporeal photopheresis (NCT01174940), gene-modified donor T cells for haploidentical HCT (NCT01494103, NCT01744223), inducible Tregs (NCT01634217), and α-β T-cell depletion (NCT01810120). With many mechanisms to target in different HCT settings, it is unlikely that a 1-size-fits-all approach to aGVHD prophylaxis will be adopted in the near future. Importantly, promising results from phase 2 studies nearly always need broader testing in a multicenter comparative setting, such as in the US National Heart, Lung, and Blood Institute/National Cancer Institute/National Institute of Allergy and Infectious Diseases sponsored BMT CTN.
Initial therapy of aGVHD
The standard treatment of patients requiring systemic therapy is corticosteroids at a daily dose of 2 mg/kg,112 although there appears to be little detriment to a lower daily dose of 1 mg/kg for overall grade 1-2 aGVHD113,114 thereby sparing some of the side effects of high-dose steroids for milder disease. The determination of steroid-responsive or refractory disease should be made within a few days of initial therapy, recognizing nonresponse after 7 to 10 days and progression even sooner if the patient is clearly worsening 3 to 4 days after the start of high-dose steroids.115 The optimal duration of steroid therapy is unknown, but should be limited if possible to avoid side effects of long-term administration. The preferred rate to taper steroids for aGVHD has been rarely studied,116 but tapering limits have been included in some prospective trials.117 For trial purposes, important clinical end points for control of aGVHD include the day 28 response,118 day 56 aGVHD-free survival,118 and 6-month freedom from treatment failure,119 as well as rates of cGVHD, nonrelapse mortality, and survival. In an effort to safely improve responses to first-line steroid therapy, the BMT CTN recently conducted 2 clinical trials: BMT CTN 0302 and 0802. In BMT CTN 0302, patients were randomized to receive 1 of 4 immunomodulatory drugs in combination with steroids as first-line therapy: etanercept, MMF, denileukin diftitox, or pentostatin.120 In this study, the day 28 complete response rate for MMF was 60%, compared with 26% for etanercept, 53% for denileukin, and 38% for pentostatin. Therefore, MMF was selected as the agent of choice to be compared with placebo in a phase 3 trial, BMT CTN 0802. However, in 0802, addition of MMF did not improve outcomes compared with steroids alone for first-line therapy.117 At present, there are few registered trials of treatment of aGVHD, and they are often uncontrolled phase 1-2 pilots. For grade I/II aGVHD, a trial of cannabidiol is ongoing (NCT01596075), and for grades II-IV aGVHD, a trial of novel histone deacetylase inhibitor LBH589 (NCT01111526) is ongoing.
Refractory and steroid-resistant aGVHD
Refractory aGVHD remains a vexing problem and leads to poor prognosis. It is a broad category that includes different clinical scenarios, usually requiring escalation of immunosuppressive therapy. Minimal, delayed, or absent response to first-line corticosteroids defines steroid-resistant aGVHD, as does inability to maintain aGVHD control upon tapering corticosteroid therapy. There is no standard treatment of refractory GVHD, however, anti-thymocyte globulin (ATG) or TNF inhibitors are most frequently used clinically, along with the other agents tested in BMT CTN 0302 (pentostatin, MMF, or denileukin diftitox). Although used clinically, agents such as ATG and pentostatin have a very low durable complete response rate (20% or less).121,122 Other immunosuppressants available include anti-IL-2 receptor–, anti-IL6 receptor–, anti-CD20–, and anti-CD52–targeted therapies. There is some data in support of extracorporeal photopheresis123 and infusion of mesenchymal stromal cells (MSCs)124 in refractory aGVHD. Current clinical trials available for the treatment of steroid-refractory aGVHD include a combination of basiliximab plus infliximab (combined targeting of the IL-2 receptor and TNFα, NCT01485055). tocilizumab (targeting the IL-6 receptor, NCT01475162, NCT01757197), α1 antitrypsin (NCT01523821, NCT01700036), and brentuximab vedotin (NCT01596218).
Emerging approaches
Many additional novel aGVHD prevention and treatment strategies are undergoing preclinical study or clinical development based upon a deeper understanding of the complex immunologic processes involved. These treatments include small molecules that target different checkpoints in the aGVHD cascade, cytokine/growth factor milieu-based therapies, cell-based therapies, alteration of host microbiota, infusion of Tregs or other suppressor populations, as well as new approaches to tolerize donor cells prior to collection. A summary of these new approaches is detailed in Table 1 (Brunstein et al,54 Highfill et al,59 Das et al,66 Valenzuela et al125-Rotta et al158). Several of these have reached the early clinical trial stage or will be clinically tested in the coming years.
Table 1.
Emerging approaches for the prevention and treatment of aGVHD
| Treatment or pathway | Potential mechanism(s) of action | Level of evidence | References |
|---|---|---|---|
| Small molecules | |||
| PKC inhibitors, such as R524 (Rigel Pharmaceuticals), and sotrastaurin (Novartis) | Inhibition of PKCα/θ, proteins that maintain immunologic synapse between APC and effector T cell | Preclinical (mouse) Sotrastaurin being investigated in solid organ transplant clinical trials | 125,126 |
| Sphingosine 1-phosphate receptor agonist FTY720 (fingolimod; Gilenya Pharmaceuticals) | Modulates DC function and lymphocyte efflux from secondary lymphoid organs, enhancement of endothelial barrier function | Preclinical (mouse) | 127 |
| Hypomethylating agents azacitidine and decitabine | Induction of FOXP3 expression | Preclinical (mouse) phase 1/2 clinical | 128,129 |
| Retinoic acid signaling | Reduction of T-cell homing, reducing Th1 differentiation, inducing Tregs | Preclinical (mouse) | 130 |
| Tim-3/Gal-9 pathway | Increased activation-induced T-cell death in the absence of Tregs | Preclinical (mouse) | 131 |
| PDL-1 pathway | Coinhibitory molecule, conversion of Th1 cells to Tregs | Preclinical (mouse) | 132 |
| IDO | Rate-limiting enzyme in tryptophan (required for T-cell proliferation) metabolism | Preclinical (mouse, human) | 133,134 |
| Arginase-1 | L-arginine depletion, reducing T-cell signaling and inflammatory cytokines | Preclinical (mouse) | 59 |
| TLR/MyD88 signaling inhibitors | Interfere with danger signaling, especially via inhibitory oligonucleotides against TLR9, to reduce inflammation | Preclinical (mouse) | 135 |
| Notch/notch ligand inhibitors | Detal-like1/4 (notch ligand) inhibitor given peritransplant prevented GVHD, while Notch 1 inhibitor lead to intestinal toxicity | Preclinical (mouse) | 136 |
| Cytokine/growth factor modulation | |||
| JAK/STAT inhibition | Reduction in inflammatory cytokines | Preclinical, case report | 137,138 |
| IL-17 downregulation | Curcumin downregulates IFNγ and IL-17 production, ameliorating aGVHD | Preclinical (mouse) | 139 |
| IL-21 blockade | Enhances generation of inducible Tregs | Preclinical (mouse) | 140 |
| IL-22 augmentation | Protective factor for intestinal stem cells under immune attack | Preclinical (mouse) | 141 |
| IL-23 blockade | Reduces inflammatory cytokines, T-cell trafficking, gut protection | Preclinical (mouse) | 66,142 |
| Case report, phase 2 (ongoing) | |||
| Cell-based therapies | |||
| MSCs | Suppress immune effector functions, secrete cytokines/growth factors for tissue repair and angiogenesis, can be obtained from related donors or third party | Phase 3, not yet reported in peer-reviewed literature (NCT00366145) | 124,143 |
| MAPCs | No expression of classical HLA class I markers (distinct from MSC), suppress T-cell activation via prostaglandin E2 synthesis, but only if colocalized with T cells at sites of activation | Preclinical (mouse) | 144,145 |
| Tregs | Expanded from umbilical cord blood, reduced aGVHD grade II-IV incidence from 61% to 43% in double UCB HCT (historical control); in haploidentical-related donors, Tregs reduced GVHD and enhanced immune reconstitution | Phase 1 | 54,146 |
| TRAIL+ T cells | Cytolytic mechanism against both tumor cells and alloreactive T cells | Preclinical (mouse) | 147 |
| NKs | GVHD protection only conferred if infusion was derived from Ly49-mismatched donor | Preclinical (mouse) | 148 |
| NKTs | Invariant NKTs attenuated murine GVHD in association with increased IL-2, IL-4, and IL-5 levels | Preclinical (mouse) | 149 |
| DCs | Tolerogenic DCs enhanced immunosuppressive cytokines in circulation, increased Tregs | Preclinical (mouse) | 150 |
| MDSCs | L-arginine depletion, contact-dependent immunosuppression | Preclinical (mouse) | 59 |
| Microbiota | |||
| α-defensins | Antimicrobial peptides secreted by intestinal Paneth cells, a target of GVHD | Preclinical (mouse) | 151 |
| Physiologic diversity | GVHD causes increase in Lactobacillales and decreases in Clostridiales, resulting in loss of physiologic diversity in gut bacteria | Preclinical (mouse and human) | 152 |
| Candida colonization | Patients colonized with Candida spp. had an increased incidence of grade II-IV GVHD (50% vs 32%) | Preclinical (human) | 153 |
| α-galactosylceramide (RGI-2001; RegImmune) | Produced by microbiome, can bind C1d and activate NKTs, induce Tregs | Preclinical (mouse) | 154,155 |
| Phase 1/2a (ongoing) | |||
| Donor-based immunomodulation | |||
| KGF (palifermin) | Epithelial, including thymic cytoprotection, inflammatory cytokine response, skewing toward Th2 cytokine response, although there was no reduction in GVHD when recipients were treated with palifermin in a phase 1/2 clinical trial | Preclinical (mouse) | 156,157 |
| Statins | Retrospective study demonstrated reduced grade III-IV GVHD in related HCT from statin-treated donors | Preclinical (mouse, human) | 158 |
| Phase 2 (ongoing) |
IDO, indoleamine 2,3 dioxygenase; IFN, interferon; JAK, Janus kinase; KGF, keratinocyte growth factor; MAPC, multipotent adult stromal cell; PDL, programmed death ligand; PKC, protein kinase C; STAT, signal transducer and activator of transcription; TRAIL, TNF-related apoptosis inducing ligand; UCB, umbilical cord blood.
Conclusion
Many new components of the aGVHD cascade have recently been identified, and translation of findings from bench to bedside has been faster than ever. Although prevention of aGVHD is clearly an important goal, finding new methods to resolve established aGVHD is critically needed today. Compared with prophylaxis studies, relatively fewer models dealing with the complicated problem of resistant aGVHD exist. Clinical features plus biomarkers may identify those most likely to fail and thereby classify those most suitable for study of intensified early treatment. Novel tolerance induction regimens that systematically and durably reprogram immune responses may become possible with ongoing research efforts. Identifying tolerizing factors and methods of manipulating microbiota may represent additional options for adjunctive aGVHD therapy that can be rapidly translated into clinical trials. Finally, more in-depth study of how to rescue patients from the cycle of incompletely resolved inflammation, where organ function has improved, but poor graft and immune function persist in the wake of severe aGVHD, remains an unmet need. Although we have seen significant innovation in methods to approach aGVHD in recent years, much work remains.
Acknowledgments
This work was supported in part by the Office of Research in Women’s Health and the National Institutes of Health Eunice Kennedy Shriver National Institute of Child Health and Human Development, Oregon Building Interdisciplinary Research Careers in Women’s Health, Award number 2K12HD043488-12 (S.G.H.).
Authorship
Contribution: S.G.H. wrote the paper; M.P. and D.J.W. edited the paper; and all authors approved the final manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Daniel J. Weisdorf, Blood and Marrow Transplant Program, University of Minnesota, Mayo Mail Code 480, 420 Delaware St SE, Minneapolis, MN 55455; e-mail: weisd001@umn.edu.
References
- 1.Blazar BR, Murphy WJ, Abedi M. Advances in graft-versus-host disease biology and therapy. Nat Rev Immunol. 2012;12(6):443–458. doi: 10.1038/nri3212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paczesny S, Hanauer D, Sun Y, Reddy P. New perspectives on the biology of acute GVHD. Bone Marrow Transplant. 2010;45(1):1–11. doi: 10.1038/bmt.2009.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petersdorf EW. The major histocompatibility complex: a model for understanding graft-versus-host disease. Blood. 2013;122(11):1863–1872. doi: 10.1182/blood-2013-05-355982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kawase T, Morishima Y, Matsuo K, et al. Japan Marrow Donor Program. High-risk HLA allele mismatch combinations responsible for severe acute graft-versus-host disease and implication for its molecular mechanism. Blood. 2007;110(7):2235–2241. doi: 10.1182/blood-2007-02-072405. [DOI] [PubMed] [Google Scholar]
- 5.Kanda Y, Kanda J, Atsuta Y, et al. HLA working group of the Japan Society for Hematopoietic Cell Transplantation. doi: 10.1016/j.bbmt.2014.01.003. Changes in the clinical impact of high-risk human leukocyte antigen allele mismatch combinations on the outcome of unrelated bone marrow transplantation. Biol Blood Marrow Transplant. 2014;20(4):526-535. [DOI] [PubMed] [Google Scholar]
- 6.Pidala J, Wang T, Haagenson M, et al. Amino acid substitution at peptide-binding pockets of HLA class I molecules increases risk of severe acute GVHD and mortality. Blood. 2013;122(22):3651–3658. doi: 10.1182/blood-2013-05-501510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fernández-Viña MA, Klein JP, Haagenson M, et al. Multiple mismatches at the low expression HLA loci DP, DQ, and DRB3/4/5 associate with adverse outcomes in hematopoietic stem cell transplantation. Blood. 2013;121(22):4603–4610. doi: 10.1182/blood-2013-02-481945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stern M, Brand R, de Witte T, et al. Female-versus-male alloreactivity as a model for minor histocompatibility antigens in hematopoietic stem cell transplantation. Am J Transplant. 2008;8(10):2149–2157. doi: 10.1111/j.1600-6143.2008.02374.x. [DOI] [PubMed] [Google Scholar]
- 9.Spierings E, Kim YH, Hendriks M, et al. Multicenter analyses demonstrate significant clinical effects of minor histocompatibility antigens on GvHD and GvL after HLA-matched related and unrelated hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2013;19(8):1244–1253. doi: 10.1016/j.bbmt.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Miller JS, Cooley S, Parham P, et al. Missing KIR ligands are associated with less relapse and increased graft-versus-host disease (GVHD) following unrelated donor allogeneic HCT. Blood. 2007;109(11):5058–5061. doi: 10.1182/blood-2007-01-065383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brennan TV, Lin L, Huang X, et al. Heparan sulfate, an endogenous TLR4 agonist, promotes acute GVHD after allogeneic stem cell transplantation. Blood. 2012;120(14):2899–2908. doi: 10.1182/blood-2011-07-368720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilhelm K, Ganesan J, Müller T, et al. Graft-versus-host disease is enhanced by extracellular ATP activating P2X7R. Nat Med. 2010;16(12):1434–1438. doi: 10.1038/nm.2242. [DOI] [PubMed] [Google Scholar]
- 13.Jankovic D, Ganesan J, Bscheider M, et al. The Nlrp3 inflammasome regulates acute graft-versus-host disease. J Exp Med. 2013;210(10):1899–1910. doi: 10.1084/jem.20130084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooke KR, Hill GR, Crawford JM, et al. Tumor necrosis factor- alpha production to lipopolysaccharide stimulation by donor cells predicts the severity of experimental acute graft-versus-host disease. J Clin Invest. 1998;102(10):1882–1891. doi: 10.1172/JCI4285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kinnier CV, Martinu T, Gowdy KM, Nugent JL, Kelly FL, Palmer SM. Innate immune activation by the viral PAMP poly I:C potentiates pulmonary graft-versus-host disease after allogeneic hematopoietic cell transplant. Transpl Immunol. 2011;24(2):83–93. doi: 10.1016/j.trim.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zeiser R, Penack O, Holler E, Idzko M. Danger signals activating innate immunity in graft-versus-host disease. J Mol Med (Berl) 2011;89(9):833–845. doi: 10.1007/s00109-011-0767-x. [DOI] [PubMed] [Google Scholar]
- 17.Hossain MS, Jaye DL, Pollack BP, et al. Flagellin, a TLR5 agonist, reduces graft-versus-host disease in allogeneic hematopoietic stem cell transplantation recipients while enhancing antiviral immunity. J Immunol. 2011;187(10):5130–5140. doi: 10.4049/jimmunol.1101334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duffner UA, Maeda Y, Cooke KR, et al. Host dendritic cells alone are sufficient to initiate acute graft-versus-host disease. J Immunol. 2004;172(12):7393–7398. doi: 10.4049/jimmunol.172.12.7393. [DOI] [PubMed] [Google Scholar]
- 19.Teshima T, Ordemann R, Reddy P, et al. Acute graft-versus-host disease does not require alloantigen expression on host epithelium. Nat Med. 2002;8(6):575–581. doi: 10.1038/nm0602-575. [DOI] [PubMed] [Google Scholar]
- 20.Li H, Demetris AJ, McNiff J, et al. Profound depletion of host conventional dendritic cells, plasmacytoid dendritic cells, and B cells does not prevent graft-versus-host disease induction. J Immunol. 2012;188(8):3804–3811. doi: 10.4049/jimmunol.1102795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li H, Kaplan DH, Matte-Martone C, et al. Langerhans cells are not required for graft-versus-host disease. Blood. 2011;117(2):697–707. doi: 10.1182/blood-2010-07-299073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matte-Martone C, Wang X, Anderson B, et al. Recipient B cells are not required for graft-versus-host disease induction. Biol Blood Marrow Transplant. 2010;16(9):1222–1230. doi: 10.1016/j.bbmt.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hashimoto D, Chow A, Greter M, et al. Pretransplant CSF-1 therapy expands recipient macrophages and ameliorates GVHD after allogeneic hematopoietic cell transplantation. J Exp Med. 2011;208(5):1069–1082. doi: 10.1084/jem.20101709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koyama M, Kuns RD, Olver SD, et al. Recipient nonhematopoietic antigen-presenting cells are sufficient to induce lethal acute graft-versus-host disease. Nat Med. 2012;18(1):135–142. doi: 10.1038/nm.2597. [DOI] [PubMed] [Google Scholar]
- 25.Morris GP, Uy GL, Donermeyer D, Dipersio JF, Allen PM. Dual receptor T cells mediate pathologic alloreactivity in patients with acute graft-versus-host disease. Sci Transl Med. 2013;5(188):188ra174. [DOI] [PMC free article] [PubMed]
- 26.Briones J, Novelli S, Sierra J. T-cell costimulatory molecules in acute-graft-versus host disease: therapeutic implications. Bone Marrow Res. 2011;2011:976793. doi: 10.1155/2011/976793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chakraverty R, Côté D, Buchli J, et al. An inflammatory checkpoint regulates recruitment of graft-versus-host reactive T cells to peripheral tissues. J Exp Med. 2006;203(8):2021–2031. doi: 10.1084/jem.20060376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Terwey TH, Kim TD, Kochman AA, et al. CCR2 is required for CD8-induced graft-versus-host disease. Blood. 2005;106(9):3322–3330. doi: 10.1182/blood-2005-05-1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murai M, Yoneyama H, Harada A, et al. Active participation of CCR5(+)CD8(+) T lymphocytes in the pathogenesis of liver injury in graft-versus-host disease. J Clin Invest. 1999;104(1):49–57. doi: 10.1172/JCI6642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Varona R, Cadenas V, Gómez L, Martínez-A C, Márquez G. CCR6 regulates CD4+ T-cell-mediated acute graft-versus-host disease responses. Blood. 2005;106(1):18–26. doi: 10.1182/blood-2004-08-2996. [DOI] [PubMed] [Google Scholar]
- 31.Yakoub-Agha I, Saule P, Depil S, et al. A high proportion of donor CD4+ T cells expressing the lymph node-homing chemokine receptor CCR7 increases incidence and severity of acute graft-versus-host disease in patients undergoing allogeneic stem cell transplantation for hematological malignancy. Leukemia. 2006;20(9):1557–1565. doi: 10.1038/sj.leu.2404308. [DOI] [PubMed] [Google Scholar]
- 32.Kittan NA, Hildebrandt GC. The chemokine system: a possible therapeutic target in acute graft versus host disease. Curr Top Microbiol Immunol. 2010;341:97–120. doi: 10.1007/82_2010_23. [DOI] [PubMed] [Google Scholar]
- 33.van der Waart AB, van der Velden WJ, van Halteren AG, et al. Decreased levels of circulating IL17-producing CD161+CCR6+ T cells are associated with graft-versus-host disease after allogeneic stem cell transplantation. PLoS ONE. 2012;7(12):e50896. doi: 10.1371/journal.pone.0050896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Avanzini MA, Maccario R, Locatelli F, et al. Low percentages of circulating CD8(+)/CD45RA(+) human T lymphocytes expressing beta7 integrin correlate with the occurrence of intestinal acute graft-versus-host disease after allogeneic hematopoietic stem cell transplantation. Exp Hematol. 2006;34(10):1429–1434. doi: 10.1016/j.exphem.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 35.Chen YB, McDonough S, Chen H, et al. Expression of α4β7 integrin on memory CD8(+) T cells at the presentation of acute intestinal GVHD. Bone Marrow Transplant. 2013;48(4):598–603. doi: 10.1038/bmt.2012.191. [DOI] [PubMed] [Google Scholar]
- 36.Xystrakis E, Bernard I, Dejean AS, Alsaati T, Druet P, Saoudi A. Alloreactive CD4 T lymphocytes responsible for acute and chronic graft-versus-host disease are contained within the CD45RChigh but not the CD45RClow subset. Eur J Immunol. 2004;34(2):408–417. doi: 10.1002/eji.200324528. [DOI] [PubMed] [Google Scholar]
- 37.Dutt S, Tseng D, Ermann J, et al. Naive and memory T cells induce different types of graft-versus-host disease. J Immunol. 2007;179(10):6547–6554. doi: 10.4049/jimmunol.179.10.6547. [DOI] [PubMed] [Google Scholar]
- 38.Chen BJ, Deoliveira D, Cui X, et al. Inability of memory T cells to induce graft-versus-host disease is a result of an abortive alloresponse. Blood. 2007;109(7):3115–3123. doi: 10.1182/blood-2006-04-016410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang P, Wu J, Deoliveira D, Chao NJ, Chen BJ. Allospecific CD4(+) effector memory T cells do not induce graft-versus-host disease in mice. Biol Blood Marrow Transplant. 2012;18(10):1488–1499. doi: 10.1016/j.bbmt.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Juchem KW, Anderson BE, Zhang C, et al. A repertoire-independent and cell-intrinsic defect in murine GVHD induction by effector memory T cells. Blood. 2011;118(23):6209–6219. doi: 10.1182/blood-2011-01-330035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miller WP, Srinivasan S, Panoskaltsis-Mortari A, et al. GVHD after haploidentical transplantation: a novel, MHC-defined rhesus macaque model identifies CD28- CD8+ T cells as a reservoir of breakthrough T-cell proliferation during costimulation blockade and sirolimus-based immunosuppression. Blood. 2010;116(24):5403–5418. doi: 10.1182/blood-2010-06-289272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Uguccioni M, Meliconi R, Nesci S, et al. Elevated interleukin-8 serum concentrations in beta-thalassemia and graft-versus-host disease. Blood. 1993;81(9):2252–2256. [PubMed] [Google Scholar]
- 43.Ringdén O, Labopin M, Gorin NC, et al. Treatment with granulocyte colony-stimulating factor after allogeneic bone marrow transplantation for acute leukemia increases the risk of graft-versus-host disease and death: a study from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. J Clin Oncol. 2004;22(3):416–423. doi: 10.1200/JCO.2004.06.102. [DOI] [PubMed] [Google Scholar]
- 44.Ringden O, Hassan Z, Karlsson H, et al. Granulocyte colony-stimulating factor induced acute and chronic graft-versus-host disease. Transplantation. 2010;90(9):1022–1029. doi: 10.1097/TP.0b013e3181f585c7. [DOI] [PubMed] [Google Scholar]
- 45.Olson JA, Zeiser R, Beilhack A, Goldman JJ, Negrin RS. Tissue-specific homing and expansion of donor NK cells in allogeneic bone marrow transplantation. J Immunol. 2009;183(5):3219–3228. doi: 10.4049/jimmunol.0804268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ghayur T, Seemayer TA, Kongshavn PA, Gartner JG, Lapp WS. Graft-versus-host reactions in the beige mouse. An investigation of the role of host and donor natural killer cells in the pathogenesis of graft-versus-host disease. Transplantation. 1987;44(2):261–267. doi: 10.1097/00007890-198708000-00017. [DOI] [PubMed] [Google Scholar]
- 47.Tanaka M, Kobayashi S, Numata A, et al. The impact of the dose of natural killer cells in the graft on severe acute graft-versus-host disease after unrelated bone marrow transplantation. Leuk Res. 2012;36(6):699–703. doi: 10.1016/j.leukres.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 48.Schultz KR, Paquet J, Bader S, HayGlass KT. Requirement for B cells in T cell priming to minor histocompatibility antigens and development of graft-versus-host disease. Bone Marrow Transplant. 1995;16(2):289–295. [PubMed] [Google Scholar]
- 49.Crocchiolo R, Castagna L, El-Cheikh J, et al. Prior rituximab administration is associated with reduced rate of acute GVHD after in vivo T-cell depleted transplantation in lymphoma patients. Exp Hematol. 2011;39(9):892–896. doi: 10.1016/j.exphem.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 50.Ratanatharathorn V, Logan B, Wang D, et al. Center for International Blood and Marrow Transplant Research, Milwaukee, WI. Prior rituximab correlates with less acute graft-versus-host disease and better survival in B-cell lymphoma patients who received allogeneic peripheral blood stem cell transplantation. Br J Haematol. 2009;145(6):816–824. doi: 10.1111/j.1365-2141.2009.07674.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lo JW, Leung AY, Huang XR, et al. Macrophage migratory inhibitory factor (MIF) expression in acute graft-versus-host disease (GVHD) in allogeneic hemopoietic stem cell transplant recipients. Bone Marrow Transplant. 2002;30(6):375–380. doi: 10.1038/sj.bmt.1703639. [DOI] [PubMed] [Google Scholar]
- 52.Hoffmann P, Ermann J, Edinger M, Fathman CG, Strober S. Donor-type CD4(+)CD25(+) regulatory T cells suppress lethal acute graft-versus-host disease after allogeneic bone marrow transplantation. J Exp Med. 2002;196(3):389–399. doi: 10.1084/jem.20020399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taylor PA, Lees CJ, Blazar BR. The infusion of ex vivo activated and expanded CD4(+)CD25(+) immune regulatory cells inhibits graft-versus-host disease lethality. Blood. 2002;99(10):3493–3499. doi: 10.1182/blood.v99.10.3493. [DOI] [PubMed] [Google Scholar]
- 54.Brunstein CG, Miller JS, Cao Q, et al. Infusion of ex vivo expanded T regulatory cells in adults transplanted with umbilical cord blood: safety profile and detection kinetics. Blood. 2011;117(3):1061–1070. doi: 10.1182/blood-2010-07-293795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vignali DA, Collison LW, Workman CJ. How regulatory T cells work. Nat Rev Immunol. 2008;8(7):523–532. doi: 10.1038/nri2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sawitzki B, Brunstein C, Meisel C, et al. Prevention of graft-versus-host disease by adoptive T regulatory therapy is associated with active repression of peripheral blood Toll-like receptor 5 mRNA expression. Biol Blood Marrow Transplant. 2014;20(2):173–182. doi: 10.1016/j.bbmt.2013.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Skert C, Fogli M, Perucca S, et al. Profile of Toll-like receptors on peripheral blood cells in relation to acute graft-versus-host disease after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2013;19(2):227–234. doi: 10.1016/j.bbmt.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 58.Mangus CW, Massey PR, Fowler DH, Amarnath S. Rapamycin resistant murine th9 cells have a stable in vivo phenotype and inhibit graft-versus-host reactivity. PLoS ONE. 2013;8(8):e72305. doi: 10.1371/journal.pone.0072305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Highfill SL, Rodriguez PC, Zhou Q, et al. Bone marrow myeloid-derived suppressor cells (MDSCs) inhibit graft-versus-host disease (GVHD) via an arginase-1-dependent mechanism that is up-regulated by interleukin-13. Blood. 2010;116(25):5738–5747. doi: 10.1182/blood-2010-06-287839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mougiakakos D, Jitschin R, von Bahr L, et al. Immunosuppressive CD14+HLA-DRlow/neg IDO+ myeloid cells in patients following allogeneic hematopoietic stem cell transplantation. Leukemia. 2013;27(2):377–388. doi: 10.1038/leu.2012.215. [DOI] [PubMed] [Google Scholar]
- 61.Asai O, Longo DL, Tian ZG, et al. Suppression of graft-versus-host disease and amplification of graft-versus-tumor effects by activated natural killer cells after allogeneic bone marrow transplantation. J Clin Invest. 1998;101(9):1835–1842. doi: 10.1172/JCI1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chaidos A, Patterson S, Szydlo R, et al. Graft invariant natural killer T-cell dose predicts risk of acute graft-versus-host disease in allogeneic hematopoietic stem cell transplantation. Blood. 2012;119(21):5030–5036. doi: 10.1182/blood-2011-11-389304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Knoechel B, Lohr J, Kahn E, Abbas AK. The link between lymphocyte deficiency and autoimmunity: roles of endogenous T and B lymphocytes in tolerance. J Immunol. 2005;175(1):21–26. doi: 10.4049/jimmunol.175.1.21. [DOI] [PubMed] [Google Scholar]
- 64.Reikvam H, Fredly H, Kittang AO, Bruserud O. The possible diagnostic and prognostic use of systemic chemokine profiles in clinical medicine—the experience in acute myeloid leukemia from disease development and diagnosis via conventional chemotherapy to allogeneic stem cell transplantation. Toxins (Basel) 2013;5(2):336–362. doi: 10.3390/toxins5020336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yi T, Chen Y, Wang L, et al. Reciprocal differentiation and tissue-specific pathogenesis of Th1, Th2, and Th17 cells in graft-versus-host disease. Blood. 2009;114(14):3101–3112. doi: 10.1182/blood-2009-05-219402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Das R, Komorowski R, Hessner MJ, et al. Blockade of interleukin-23 signaling results in targeted protection of the colon and allows for separation of graft-versus-host and graft-versus-leukemia responses. Blood. 2010;115(25):5249–5258. doi: 10.1182/blood-2009-11-255422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brüggen MC, Klein I, Greinix H, et al. Diverse T-cell responses characterize the different manifestations of cutaneous graft-versus-host disease. Blood. 2014;123(2):290–299. doi: 10.1182/blood-2013-07-514372. [DOI] [PubMed] [Google Scholar]
- 68.Hübel K, Cremer B, Heuser E, von Strandmann EP, Hallek M, Hansen HP. A prospective study of serum soluble CD30 in allogeneic hematopoietic stem cell transplantation. Transpl Immunol. 2010;23(4):215–219. doi: 10.1016/j.trim.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 69.Paczesny S, Braun TM, Levine JE, et al. Elafin is a biomarker of graft-versus-host disease of the skin. Sci Transl Med. 2010;2(13):13ra2. doi: 10.1126/scitranslmed.3000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ferrara JL, Harris AC, Greenson JK, et al. Regenerating islet-derived 3-alpha is a biomarker of gastrointestinal graft-versus-host disease. Blood. 2011;118(25):6702–6708. doi: 10.1182/blood-2011-08-375006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schmitz J, Owyang A, Oldham E, et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23(5):479–490. doi: 10.1016/j.immuni.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 72.Xiao B, Wang Y, Li W, et al. Plasma microRNA signature as a noninvasive biomarker for acute graft-versus-host disease. Blood. 2013;122(19):3365–3375. doi: 10.1182/blood-2013-06-510586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Paczesny S. Discovery and validation of graft-versus-host disease biomarkers. Blood. 2013;121(4):585–594. doi: 10.1182/blood-2012-08-355990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yan Z, Zeng L, Jia L, Xu S, Ding S. Increased numbers of circulating ECs are associated with systemic GVHD. Int J Lab Hematol. 2011;33(5):507–515. doi: 10.1111/j.1751-553X.2011.01322.x. [DOI] [PubMed] [Google Scholar]
- 75.Luft T, Dietrich S, Falk C, et al. Steroid-refractory GVHD: T-cell attack within a vulnerable endothelial system. Blood. 2011;118(6):1685–1692. doi: 10.1182/blood-2011-02-334821. [DOI] [PubMed] [Google Scholar]
- 76.Filipovich AH, Weisdorf D, Pavletic S, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11(12):945–956. doi: 10.1016/j.bbmt.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 77.Lee KH, Choi SJ, Lee JH, et al. Prognostic factors identifiable at the time of onset of acute graft-versus-host disease after allogeneic hematopoietic cell transplantation. Haematologica. 2005;90(7):939–948. [PubMed] [Google Scholar]
- 78.Imahashi N, Miyamura K, Seto A, et al. Eosinophilia predicts better overall survival after acute graft-versus-host-disease. Bone Marrow Transplant. 2010;45(2):371–377. doi: 10.1038/bmt.2009.135. [DOI] [PubMed] [Google Scholar]
- 79.Ramírez P, Brunstein CG, Miller B, Defor T, Weisdorf D. Delayed platelet recovery after allogeneic transplantation: a predictor of increased treatment-related mortality and poorer survival. Bone Marrow Transplant. 2011;46(7):981–986. doi: 10.1038/bmt.2010.218. [DOI] [PubMed] [Google Scholar]
- 80.Stelljes M, Hermann S, Albring J, et al. Clinical molecular imaging in intestinal graft-versus-host disease: mapping of disease activity, prediction, and monitoring of treatment efficiency by positron emission tomography. Blood. 2008;111(5):2909–2918. doi: 10.1182/blood-2007-10-119164. [DOI] [PubMed] [Google Scholar]
- 81.Brede C, Friedrich M, Jordán-Garrote AL, et al. Mapping immune processes in intact tissues at cellular resolution. J Clin Invest. 2012;122(12):4439–4446. doi: 10.1172/JCI65100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fullerton JN, O’Brien AJ, Gilroy DW. Pathways mediating resolution of inflammation: when enough is too much. J Pathol. 2013;231(1):8–20. doi: 10.1002/path.4232. [DOI] [PubMed] [Google Scholar]
- 83.Bouazzaoui A, Spacenko E, Mueller G, et al. Steroid treatment alters adhesion molecule and chemokine expression in experimental acute graft-vs.-host disease of the intestinal tract. Exp Hematol. 2011;39(2):238-249.e1. [DOI] [PubMed]
- 84.Levine JE, Logan BR, Wu J, et al. Acute graft-versus-host disease biomarkers measured during therapy can predict treatment outcomes: a Blood and Marrow Transplant Clinical Trials Network study. Blood. 2012;119(16):3854–3860. doi: 10.1182/blood-2012-01-403063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bolaños-Meade J, Wu J, Logan BR, et al. Blood and Marrow Transplant Clinical Trials Network. Lymphocyte phenotype during therapy for acute graft-versus-host disease: a brief report from BMT-CTN 0302. Biol Blood Marrow Transplant. 2013;19(3):481–485. doi: 10.1016/j.bbmt.2012.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tichelli A, Gratwohl A. Vascular endothelium as ‘novel’ target of graft-versus-host disease. Best Pract Res Clin Haematol. 2008;21(2):139–148. doi: 10.1016/j.beha.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 87.Gress RE, Emerson SG, Drobyski WR. Immune reconstitution: how it should work, what’s broken, and why it matters. Biol Blood Marrow Transplant. 2010;16(suppl 1):S133–S137. doi: 10.1016/j.bbmt.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Noval Rivas M, Hazzan M, Weatherly K, Gaudray F, Salmon I, Braun MY. NK cell regulation of CD4 T cell-mediated graft-versus-host disease. J Immunol. 2010;184(12):6790–6798. doi: 10.4049/jimmunol.0902598. [DOI] [PubMed] [Google Scholar]
- 89.MacMillan ML, Weisdorf DJ, Wagner JE, et al. Response of 443 patients to steroids as primary therapy for acute graft-versus-host disease: comparison of grading systems. Biol Blood Marrow Transplant. 2002;8(7):387–394. doi: 10.1053/bbmt.2002.v8.pm12171485. [DOI] [PubMed] [Google Scholar]
- 90.Westin JR, Saliba RM, De Lima M, et al. Steroid-refractory acute GVHD: predictors and outcomes. Adv Hematol. 2011;2011:601953. [DOI] [PMC free article] [PubMed]
- 91.MacMillan ML, DeFor TE, Weisdorf DJ. What predicts high risk acute graft-versus-host disease (GVHD) at onset? Identification of those at highest risk by a novel acute GVHD risk score. Br J Haematol. 2012;157(6):732–741. doi: 10.1111/j.1365-2141.2012.09114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Vander Lugt MT, Braun TM, Hanash S, et al. ST2 as a marker for risk of therapy-resistant graft-versus-host disease and death. N Engl J Med. 2013;369(6):529–539. doi: 10.1056/NEJMoa1213299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jitschin R, Mougiakakos D, Von Bahr L, et al. Alterations in the cellular immune compartment of patients treated with third-party mesenchymal stromal cells following allogeneic hematopoietic stem cell transplantation. Stem Cells. 2013;31(8):1715–1725. doi: 10.1002/stem.1386. [DOI] [PubMed] [Google Scholar]
- 94.Nishiwaki S, Terakura S, Ito M, et al. Impact of macrophage infiltration of skin lesions on survival after allogeneic stem cell transplantation: a clue to refractory graft-versus-host disease. Blood. 2009;114(14):3113–3116. doi: 10.1182/blood-2009-03-209635. [DOI] [PubMed] [Google Scholar]
- 95.Thomas ED, Buckner CD, Rudolph RH, et al. Allogeneic marrow grafting for hematologic malignancy using HL-A matched donor-recipient sibling pairs. Blood. 1971;38(3):267–287. [PubMed] [Google Scholar]
- 96.Vogelsang GB, Hess AD, Santos GW. Acute graft-versus-host disease: clinical characteristics in the cyclosporine era. Medicine (Baltimore) 1988;67(3):163–174. doi: 10.1097/00005792-198805000-00003. [DOI] [PubMed] [Google Scholar]
- 97.Ratanatharathorn V, Nash RA, Przepiorka D, et al. Phase III study comparing methotrexate and tacrolimus (prograf, FK506) with methotrexate and cyclosporine for graft-versus-host disease prophylaxis after HLA-identical sibling bone marrow transplantation. Blood. 1998;92(7):2303–2314. [PubMed] [Google Scholar]
- 98.Storb R, Antin JH, Cutler C. Should methotrexate plus calcineurin inhibitors be considered standard of care for prophylaxis of acute graft-versus-host disease? Biol Blood Marrow Transplant. 2010;16(suppl1):S18–S27. doi: 10.1016/j.bbmt.2009.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ram R, Gafter-Gvili A, Yeshurun M, Paul M, Raanani P, Shpilberg O. Prophylaxis regimens for GVHD: systematic review and meta-analysis. Bone Marrow Transplant. 2009;43(8):643–653. doi: 10.1038/bmt.2008.373. [DOI] [PubMed] [Google Scholar]
- 100.Pidala J, Kim J, Jim H, et al. A randomized phase II study to evaluate tacrolimus in combination with sirolimus or methotrexate after allogeneic hematopoietic cell transplantation. Haematologica. 2012;97(12):1882–1889. doi: 10.3324/haematol.2012.067140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cutler C, Stevenson K, Kim HT, et al. Sirolimus is associated with veno-occlusive disease of the liver after myeloablative allogeneic stem cell transplantation. Blood. 2008;112(12):4425–4431. doi: 10.1182/blood-2008-07-169342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cutler C, Logan BR, Makamura R, et al. Tacrolimus/sirolimus vs. tacrolimus/methotrexate for graft-vs.-host disease prophylaxis after HLA-matched, related donor hematopoietic stem cell transplantation: results of Blood and Marrow Transplant Clinical Trials Network Trial 0402 [abstract]. Blood. 2012;122(21). Abstract 739. [Google Scholar]
- 103.Handgretinger R. Negative depletion of CD3(+) and TcRαβ(+) T cells. Curr Opin Hematol. 2012;19(6):434–439. doi: 10.1097/MOH.0b013e3283582340. [DOI] [PubMed] [Google Scholar]
- 104.Kanakry CG, Ganguly S, Zahurak M, et al. Aldehyde dehydrogenase expression drives human regulatory T cell resistance to posttransplantation cyclophosphamide. Sci Transl Med. 2013;5(211):211ra157. [DOI] [PMC free article] [PubMed]
- 105.Munchel AT, Kasamon YL, Fuchs EJ. Treatment of hematological malignancies with nonmyeloablative, HLA-haploidentical bone marrow transplantation and high dose, post-transplantation cyclophosphamide. Best Pract Res Clin Haematol. 2011;24(3):359–368. doi: 10.1016/j.beha.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bashey A, Zhang X, Sizemore CA, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013;31(10):1310–1316. doi: 10.1200/JCO.2012.44.3523. [DOI] [PubMed] [Google Scholar]
- 107.Reshef R, Luger SM, Hexner EO, et al. Blockade of lymphocyte chemotaxis in visceral graft-versus-host disease. N Engl J Med. 2012;367(2):135–145. doi: 10.1056/NEJMoa1201248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Koreth J, Stevenson KE, Kim HT, et al. Bortezomib-based graft-versus-host disease prophylaxis in HLA-mismatched unrelated donor transplantation. J Clin Oncol. 2012;30(26):3202–3208. doi: 10.1200/JCO.2012.42.0984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Reddy P, Sun Y, Toubai T, et al. Histone deacetylase inhibition modulates indoleamine 2,3-dioxygenase-dependent DC functions and regulates experimental graft-versus-host disease in mice. J Clin Invest. 2008;118(7):2562–2573. doi: 10.1172/JCI34712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.He S, Wang J, Kato K, et al. Inhibition of histone methylation arrests ongoing graft-versus-host disease in mice by selectively inducing apoptosis of alloreactive effector T cells. Blood. 2012;119(5):1274–1282. doi: 10.1182/blood-2011-06-364422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Choi SW, Braun T, Chang L, et al. Vorinostat plus tacrolimus and mycophenolate to prevent graft-versus-host disease after related-donor reduced-intensity conditioning allogeneic haemopoietic stem-cell transplantation: a phase 1/2 trial. Lancet Oncol. 2014;15(1):87–95. doi: 10.1016/S1470-2045(13)70512-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Martin PJ, Rizzo JD, Wingard JR, et al. First- and second-line systemic treatment of acute graft-versus-host disease: recommendations of the American Society of Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2012;18(8):1150–1163. doi: 10.1016/j.bbmt.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mielcarek M, Storer BE, Boeckh M, et al. Initial therapy of acute graft-versus-host disease with low-dose prednisone does not compromise patient outcomes. Blood. 2009;113(13):2888–2894. doi: 10.1182/blood-2008-07-168401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mielcarek MD, Furlong T, Storer BE, et al. Efficacy and safety of lower-dose glucocorticoids for initial treatment of acute graft-versus-host disease: a randomized controlled trial [abstract]. Blood. 2013;122(21). Abstract 703. [Google Scholar]
- 115.Deeg HJ. How I treat refractory acute GVHD. Blood. 2007;109(10):4119–4126. doi: 10.1182/blood-2006-12-041889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Hings IM, Filipovich AH, Miller WJ, et al. Prednisone therapy for acute graft-versus-host disease: short- versus long-term treatment. A prospective randomized trial. Transplantation. 1993;56(3):577–580. doi: 10.1097/00007890-199309000-00016. [DOI] [PubMed] [Google Scholar]
- 117.Bolaños-Meade J, Logan BR, Alousi AM, et al. A multi-center, randomized, double blind, phase III clinical trial comparing steroids/placebo vs. steroids/mycophenolate mofetil as initial therapy for acute graft-versus-host disease. Blood and Marrow Transplant Clinical Trials Network Study 0802. Biol Blood Marrow Transplant. 2013;19(suppl 2):S137. [Google Scholar]
- 118.MacMillan ML, DeFor TE, Weisdorf DJ. The best endpoint for acute GVHD treatment trials. Blood. 2010;115(26):5412–5417. doi: 10.1182/blood-2009-12-258442. [DOI] [PubMed] [Google Scholar]
- 119.Sengsayadeth S, Savani BN, Jagasia M, et al. Six-month freedom from treatment failure is an important end point for acute GVHD clinical trials. Bone Marrow Transplant. 2014;49(2):236–240. doi: 10.1038/bmt.2013.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Alousi AM, Weisdorf DJ, Logan BR, et al. Blood and Marrow Transplant Clinical Trials Network. Etanercept, mycophenolate, denileukin, or pentostatin plus corticosteroids for acute graft-versus-host disease: a randomized phase 2 trial from the Blood and Marrow Transplant Clinical Trials Network. Blood. 2009;114(3):511–517. doi: 10.1182/blood-2009-03-212290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.MacMillan ML, Weisdorf DJ, Davies SM, et al. Early antithymocyte globulin therapy improves survival in patients with steroid-resistant acute graft-versus-host disease. Biol Blood Marrow Transplant. 2002;8(1):40–46. doi: 10.1053/bbmt.2002.v8.pm11858189. [DOI] [PubMed] [Google Scholar]
- 122.Alam N, Atenafu EG, Tse G, et al. Limited benefit of pentostatin salvage therapy for steroid-refractory grade III-IV acute graft-versus-host disease. Clin Transplant. 2013;27(6):930–937. doi: 10.1111/ctr.12268. [DOI] [PubMed] [Google Scholar]
- 123.Jagasia M, Greinix H, Robin M, et al. Extracorporeal photopheresis versus anticytokine therapy as a second-line treatment for steroid-refractory acute GVHD: a multicenter comparative analysis. Biol Blood Marrow Transplant. 2013;19(7):1129–1133. doi: 10.1016/j.bbmt.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 124.Newell LF, Deans RJ, Maziarz RT. Adult adherent stromal cells in the management of graft-versus-host disease. Expert Opin Biol Ther. 2014;14(2):231–246. doi: 10.1517/14712598.2014.866648. [DOI] [PubMed] [Google Scholar]
- 125.Valenzuela JO, Iclozan C, Hossain MS, et al. PKCtheta is required for alloreactivity and GVHD but not for immune responses toward leukemia and infection in mice. J Clin Invest. 2009;119(12):3774–3786. doi: 10.1172/JCI39692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Haarberg KM, Li J, Heinrichs J, et al. Pharmacologic inhibition of PKCα and PKCθ prevents GVHD while preserving GVL activity in mice. Blood. 2013;122(14):2500–2511. doi: 10.1182/blood-2012-12-471938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Taylor PA, Ehrhardt MJ, Lees CJ, et al. Insights into the mechanism of FTY720 and compatibility with regulatory T cells for the inhibition of graft-versus-host disease (GVHD). Blood. 2007;110(9):3480–3488. doi: 10.1182/blood-2007-05-087940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Choi J, Ritchey J, Prior JL, et al. In vivo administration of hypomethylating agents mitigate graft-versus-host disease without sacrificing graft-versus-leukemia. Blood. 2010;116(1):129–139. doi: 10.1182/blood-2009-12-257253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Goodyear OC, Dennis M, Jilani NY, et al. Azacitidine augments expansion of regulatory T cells after allogeneic stem cell transplantation in patients with acute myeloid leukemia (AML). Blood. 2012;119(14):3361–3369. doi: 10.1182/blood-2011-09-377044. [DOI] [PubMed] [Google Scholar]
- 130.Aoyama K, Saha A, Tolar J, et al. Inhibiting retinoic acid signaling ameliorates graft-versus-host disease by modifying T-cell differentiation and intestinal migration. Blood. 2013;122(12):2125–2134. doi: 10.1182/blood-2012-11-470252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Veenstra RG, Taylor PA, Zhou Q, et al. Contrasting acute graft-versus-host disease effects of Tim-3/galectin-9 pathway blockade dependent upon the presence of donor regulatory T cells. Blood. 2012;120(3):682–690. doi: 10.1182/blood-2011-10-387977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Amarnath S, Mangus CW, Wang JC, et al. The PDL1-PD1 axis converts human TH1 cells into regulatory T cells. Sci Transl Med. 2011;3(111):111ra120. [DOI] [PMC free article] [PubMed]
- 133.Jasperson LK, Bucher C, Panoskaltsis-Mortari A, et al. Indoleamine 2,3-dioxygenase is a critical regulator of acute graft-versus-host disease lethality. Blood. 2008;111(6):3257–3265. doi: 10.1182/blood-2007-06-096081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ratajczak P, Janin A, Peffault de Larour R, et al. IDO in human gut graft-versus-host disease. Biol Blood Marrow Transplant. 2012;18(1):150–155. doi: 10.1016/j.bbmt.2011.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Heimesaat MM, Nogai A, Bereswill S, et al. MyD88/TLR9 mediated immunopathology and gut microbiota dynamics in a novel murine model of intestinal graft-versus-host disease. Gut. 2010;59(8):1079–1087. doi: 10.1136/gut.2009.197434. [DOI] [PubMed] [Google Scholar]
- 136.Tran IT, Sandy AR, Carulli AJ, et al. Blockade of individual Notch ligands and receptors controls graft-versus-host disease. J Clin Invest. 2013;123(4):1590–1604. doi: 10.1172/JCI65477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Leng C, Gries M, Ziegler J, et al. Reduction of graft-versus-host disease by histone deacetylase inhibitor suberonylanilide hydroxamic acid is associated with modulation of inflammatory cytokine milieu and involves inhibition of STAT1. Exp Hematol. 2006;34(6):776–787. doi: 10.1016/j.exphem.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 138.Jaekel N, Behre G, Behning A, et al. Allogeneic hematopoietic cell transplantation for myelofibrosis in patients pretreated with the JAK1 and JAK2 inhibitor ruxolitinib. Bone Marrow Transplant. 2014;49(2):179–184. doi: 10.1038/bmt.2013.173. [DOI] [PubMed] [Google Scholar]
- 139.Park MJ, Moon SJ, Lee SH, et al. Curcumin attenuates acute graft-versus-host disease severity via in vivo regulations on Th1, Th17 and regulatory T cells. PLoS ONE. 2013;8(6):e67171. doi: 10.1371/journal.pone.0067171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bucher C, Koch L, Vogtenhuber C, et al. IL-21 blockade reduces graft-versus-host disease mortality by supporting inducible T regulatory cell generation. Blood. 2009;114(26):5375–5384. doi: 10.1182/blood-2009-05-221135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hanash AM, Dudakov JA, Hua G, et al. Interleukin-22 protects intestinal stem cells from immune-mediated tissue damage and regulates sensitivity to graft versus host disease. Immunity. 2012;37(2):339–350. doi: 10.1016/j.immuni.2012.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Pidala J, Perez L, Beato F, Anasetti C. Ustekinumab demonstrates activity in glucocorticoid-refractory acute GVHD. Bone Marrow Transplant. 2012;47(5):747–748. doi: 10.1038/bmt.2011.172. [DOI] [PubMed] [Google Scholar]
- 143.Galipeau J. The mesenchymal stromal cells dilemma—does a negative phase III trial of random donor mesenchymal stromal cells in steroid-resistant graft-versus-host disease represent a death knell or a bump in the road? Cytotherapy. 2013;15(1):2–8. doi: 10.1016/j.jcyt.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 144.Singh SP, Tripathy NK, Nityanand S. Comparison of phenotypic markers and neural differentiation potential of multipotent adult progenitor cells and mesenchymal stem cells. World J Stem Cells. 2013;5(2):53–60. doi: 10.4252/wjsc.v5.i2.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Highfill SL, Kelly RM, O’Shaughnessy MJ, et al. Multipotent adult progenitor cells can suppress graft-versus-host disease via prostaglandin E2 synthesis and only if localized to sites of allopriming. Blood. 2009;114(3):693–701. doi: 10.1182/blood-2009-03-213850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Di Ianni M, Falzetti F, Carotti A, et al. Tregs prevent GVHD and promote immune reconstitution in HLA-haploidentical transplantation. Blood. 2011;117(14):3921–3928. doi: 10.1182/blood-2010-10-311894. [DOI] [PubMed] [Google Scholar]
- 147.Ghosh A, Dogan Y, Moroz M, et al. Adoptively transferred TRAIL+ T cells suppress GVHD and augment antitumor activity. J Clin Invest. 2013;123(6):2654–2662. doi: 10.1172/JCI66301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Lundqvist A, McCoy JP, Samsel L, Childs R. Reduction of GVHD and enhanced antitumor effects after adoptive infusion of alloreactive Ly49-mismatched NK cells from MHC-matched donors. Blood. 2007;109(8):3603–3606. doi: 10.1182/blood-2006-05-024315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Yang J, Gao L, Liu Y, et al. Adoptive therapy by transfusing expanded donor murine natural killer T cells can suppress acute graft-versus-host disease in allogeneic bone marrow transplantation. Transfusion. 2010;50(2):407–417. doi: 10.1111/j.1537-2995.2009.02395.x. [DOI] [PubMed] [Google Scholar]
- 150.Yang J, Li R, Ren Y, Yang Y, Xie R, Fan H. Third-party tolerogenic dendritic cells reduce allo-reactivity in vitro and ameliorate the severity of acute graft-versus-host disease in allo-bone marrow transplantation. Scand J Immunol. 2013;78(6):486–496. doi: 10.1111/sji.12113. [DOI] [PubMed] [Google Scholar]
- 151.Eriguchi Y, Takashima S, Oka H, et al. Graft-versus-host disease disrupts intestinal microbial ecology by inhibiting Paneth cell production of α-defensins. Blood. 2012;120(1):223–231. doi: 10.1182/blood-2011-12-401166. [DOI] [PubMed] [Google Scholar]
- 152.Jenq RR, Ubeda C, Taur Y, et al. Regulation of intestinal inflammation by microbiota following allogeneic bone marrow transplantation. J Exp Med. 2012;209(5):903–911. doi: 10.1084/jem.20112408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.van der Velden WJ, Netea MG, de Haan AF, Huls GA, Donnelly JP, Blijlevens NM. Role of the mycobiome in human acute graft-versus-host disease. Biol Blood Marrow Transplant. 2013;19(2):329–332. doi: 10.1016/j.bbmt.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 154.Hashimoto D, Asakura S, Miyake S, et al. Stimulation of host NKT cells by synthetic glycolipid regulates acute graft-versus-host disease by inducing Th2 polarization of donor T cells. J Immunol. 2005;174(1):551–556. doi: 10.4049/jimmunol.174.1.551. [DOI] [PubMed] [Google Scholar]
- 155.Wieland Brown LC, Penaranda C, Kashyap PC, et al. Production of α-galactosylceramide by a prominent member of the human gut microbiota. PLoS Biol. 2013;11(7):e1001610. doi: 10.1371/journal.pbio.1001610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ellison CA, Makar BM, Wiseman JM, Gheorghiu I, Taniguchi M, Gartner JG. Palifermin mediates immunoregulatory effects in addition to its cytoprotective effects in mice with acute graft-versus-host disease. J Clin Immunol. 2008;28(5):600–615. doi: 10.1007/s10875-008-9216-1. [DOI] [PubMed] [Google Scholar]
- 157.Levine JE, Blazar BR, DeFor T, Ferrara JL, Weisdorf DJ. Long-term follow-up of a phase I/II randomized, placebo-controlled trial of palifermin to prevent graft-versus-host disease (GVHD) after related donor allogeneic hematopoietic cell transplantation (HCT). Biol Blood Marrow Transplant. 2008;14(9):1017–1021. doi: 10.1016/j.bbmt.2008.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Rotta M, Storer BE, Storb RF, et al. Donor statin treatment protects against severe acute graft-versus-host disease after related allogeneic hematopoietic cell transplantation. Blood. 2010;115(6):1288–1295. doi: 10.1182/blood-2009-08-240358. [DOI] [PMC free article] [PubMed] [Google Scholar]