Abstract
The role of macrophages (Mφ) as the first line of host defense is well accepted. These cells play a central role in orchestrating crucial functions during schistosomal infection. Thus, understanding the functional diversity of these cells in the process of infection as well as the mechanisms underlying these events is crucial for developing disease control strategies. In this study, we adopted a Mφ polarization recognition system. M1 macrophage was characterized by expressing CD16/32, IL-12 and iNOS. M2 macrophage was characterized by expressing CD206, IL-10 and arg-1. In vivo (mouse peritoneal macrophages of different infection stages were obtained) and in vitro (different S. japonicum antigens were used to stimulate RAW264.7) were characterized by using the above mentioned system. NCA and ACA stimulated RAW264.7 express significantly higher levels of IL-12 while significantly higher levels of IL-10 were detected after soluble egg antigen (SEA) stimulation. The results showed that dramatic changes of antigen in the microenvironment before and after egg production led to macrophage polarization. Furthermore, through TLR blocking experiments, the TLR4 signaling pathway was found to play a role in the process of macrophage polarization toward M1. Our data suggest that macrophage polarization during S. japonicum infection had significant effects on host immune responses to S. japonicum.
Keywords: macrophage, polarization, schistosome japonicum, TLRs
INTRODUCTION
Schistosomiasis is a zoonotic parasitic diseases and poses a serious hazard to human health[1]. Schistosoma japonicum invades mammalian hosts and triggers complex immune responses. Researchers are gradually uncovering the complex interplay between this helminth and its appropriate hosts including humans. It has been reported that specific cellular immunity plays a vital role in the immune response of schistosomiasis. Th1 type immune response plays a dominant role at the early stage of S. mansoni and S. japonicum infection[8], while Th2 type immune response predominates after egg production. A large number of studies have summarized the characteristics of host immune response after S. japonicum infection: in the initial 2 to 4 weeks after infection, under the stimulation of migrating schistosomula, the host shows Th1 type (IFN-γ, TNF) response; once egg production begins, Th1 type response drops rapidly, and Th2 type (IL-4, IL-13, IL-10, IL-5) response starts[2]-[8]. Therefore, host cytokine environment changes before and after egg production. But so far, the mechanism underlying this immune phenomenon has not been fully elucidated. Thus, it is very important to continue to explore and understand the immune responses induced by S. japonicum so as to manipulate host immune responses toward the direction that will facilitate human immunity against schistosomiasis.
Macrophages (Mφ) occupy a unique position in the immune system. They function in both non-specific defense (innate immunity) as well as help initiate specific defense mechanisms (adaptive immunity) of vertebrate animals. It has been found that macrophage are highly heterogeneous cells that can differentiate into distinct subtypes in response to local microenvironmental signals[9]. There are two major subtypes of macrophage: M1 and M2. M1 is classically activated and phagocytoses and destroys pathogens and malignant cells. It also activates adaptive immune responses by secretion of proinflammatory cytokines and chemokines and acting as professional antigen-presenting cell. M2 is alternatively activated macrophages induced by GM-CSF, IL-4, -13, -10, glucocorticoid, TGF-beta, vitamin D3, PGE2 and etc. M2 has low antigen presentation capacity and can down-regulate adaptive immune responses by secretion of IL-10, CCL17, CCL18 and TGF-β[10]-[17]. Obviously, M1 and M2 can lead to either positive or negative regulatory signals to the immune responses, respectively. It is important to determine whether macrophage polarization may be linked to the change of microenvironments before and after egg production during schistosome infection and then regulates the development of adaptive immune responses, including Th polarization shift. The aim of this study was to find the molecular evidence of Mφ polarization associated with the change of antigen microenvironments before and after egg production during schistosome infection. We carried out in vitro (macrophage cell line RAW264.7) and in vivo (experimental infection of mice with S. japonicum) experiments. Our study may enrich our knowledge of host immune responses during S. japonicum infection, and add experimental evidence of immune suppression induced by egg antigens. We also discuss possible strategies of S. japonicum escape from host immune responses, which may provide insight into developing anti-schistosomiasis vaccines and more effective anti-schistosome drugs. Our study points to the possibility of enhancing anti-schistosome immune responses by skewing in vivo macrophage polarization as part of vaccination strategy.
MATERIALS AND METHODS
Experimental mice and parasites
Six to eight-week-old C57BL/6J (B6) mice (female, 120) were purchased from the Animal Research Center of Nanjing University (Nanjing, China). All mice were maintained and bred under specific pathogen-free conditions. All experiments were undertaken with the approval of Nanjing Medical University Animal Ethics Committee. Schistosoma japonicum (S. japonicum, a Chinese mainland strain) cercariae were maintained in Oncomelania hupensis snails as the intermediate host, which were purchased from Jiangsu Institute of Parasitic Disease (Wuxi, China).
Infection with S. japonicum and isolation of peritoneal macrophages
C57BL/6J (B6) mice were percutaneously infected with 20±2 S. japonicum cercariae through their shaved abdomen. All mice were sacrificed at different S. japonicum infection stages (at 0, 3, 6 and 9 weeks after infection) to obtain murine peritoneal macrophages according to the literature[18].
Culture and stimulation of murine macrophage cell line (RAW264.7)
The RAW264.7 murine macrophage cell line (TIB-71; American Type Culture Collection, Manassas, VA) was maintained at 37°C in 5% CO2 in 10-cm dishes with Dulbecco's modified Eagle's medium (DMEM) (Invitrogen, Carlsbad, CA, USA) supplemented with antibiotics and 10% fetal bovine serum (FBS). Cells in passages 5 to 8 were used in the experiments.
For stimulation, at 37°C in 5% CO2 for 48 hours, classic M1 inducer IFN-γ (2 ng/μL) (PeproTech, USA), lipopolysaccharide (LPS) (5 ng/mL) (Sigma, St. Louis, MA, USA) and M2 inducer IL-4 (10 ng/μL) (PeproTech, USA) were used. The normal cercaria antigen (NCA) (40 ng/μL), attenuated cercaria antigen (ACA) (40 ng/μL), soluble egg antigen (SEA) (40 ng/μL) and soluble worm anti-gen (SWAP) (40 ng/μL) were prepared as before[19]. The concentrations of antigens were assayed using Bicinchoninic Acid Protein Assay Kit (Pierce, Rockford, IL, USA).
Measurement of M1/M2 cytokine levels in the macrophage culture supernatants
Stimulated RAW264.7 cells or isolated peritoneal macrophages from different S. japonicum infection stages cultivated at 37°C in 5% CO2 for 48 hours. Next, the supernatants were collected for the M1/M2 cytokine assay. IL-12, IL-10, TNF-α and TGF-β1 levels were examined by enzyme-linked immuno sorbent assay (ELISA) kits (eBioscience, USA).
Flow cytometry method
Percentage of M1 and M2 was determined by two-color staining with FITC- and PECy5-labeled antibodies. For each staining, one antibody for lineage markers (CD16/32 or CD206) were used with one antibody for macrophage markers (F4/80). Totally, 4×105 cells were incubated with staining antibodies for 15 minutes at room temperature in the dark. Cells were washed three times with PBS before the expression of surface molecules was examined by flow cytometry on a FACSCalibur™ (BD Biosciences, Heidelberg, Germany). A total of 10,000 events were analyzed. Data analysis was performed by FCS Express (De Novo Software, Los Angeles, CA, USA).
Quantitative real-time PCR (qRT-PCR)
Total RNA was extracted from RAW264.7 stimulated by different stimuli and mouse peritoneal macrophages obtained from mice with different S. japonicum infection stages. Total RNA was transcribed to cDNA by using a commercially available reverse transcription kit (Epicentre Technologies, Madison, WI, USA). The cDNA was employed as a template in real-time PCR using the ABI 7900 real-time PCR system (ABI, USA). Primers specific for gapdh, iNOS (inos) and Arg-1 (arg1) are shown in Table 1. Reactions were performed using 2 μL of cDNA in a 10 μL reaction volume and the following thermal cycle profile: 10 minutes of denaturation at 95°C, 40 cycles of denaturation at 95°C for 15 seconds and then 60 seconds of extension at 60°C. PCR amplification of gapdh was performed to allow normalization between samples.
Table 1. qRT-PCR primers.
| GENE | GenBank NO. | Primer (5′→3′) | |
| gapdh | NM 008084.2 | F: | CTGCACCACCAACTGCTTAG |
| R: | GTCTGGGATGGAAATTGTGA | ||
| inos | NM 010927.3 | F: | CTGCAGCACTTGGATCAGGAACCTG |
| R: | GGAGAGCCTGTGTGCACCTGGAA | ||
| arg1 | NM 007482.3 | F: | CAGAAGAATGGAAGAGTCAG |
| R: | CAGATATGCAGGGAGTCACC |
Antibody blocking assay
Antibody blocking experiment was performed to understand the effect of TLR2 and TLR4 in S. japonicum antigen induced macrophage polarization. RAW 264.7 cells were incubated in 96-well flat-bottom plates (2.0×105 cells/well). For experiments blocking TLR4, adherent RAW 264.7 cells were treated with 50 μg/mL of anti-mouse TLR4 antibody or isotype control antibody IgG2a for 30 minutes at 37°C. Following incubation with antibodies, NCA, SEA, and SWAP (40 μg/mL), were respectively added, and cells were incubated for 48 hours at 37°C, 5% CO2. Then, these cells were collected and assayed for lineage markers (CD16/32 or CD206). The culture supernatants were collected and assayed for IL-12 and IL-10 production. Cells cultured with medium alone were used as controls.
Statistical analysis
The data were presented as mean ± SEM. ANOVA followed by the Newman-Keuls test was used for the analysis of differences among multiple groups. Student's t-test was used for comparisons between the two groups. All statistic analyses were performed with SPSS 16.0 software (SPSS Inc., Chicago, IL, USA). Significant difference was established when P was < 0.05.
RESULTS
Reading criteria foracrophage polarization
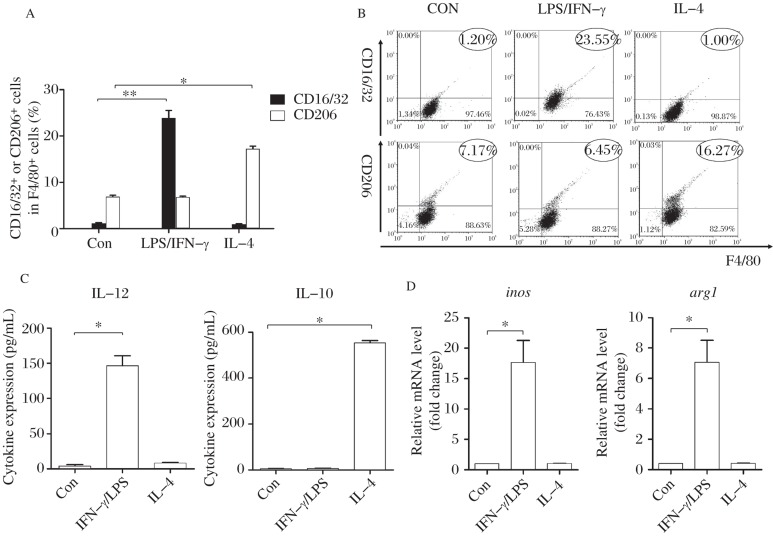
We used flow cytometry to detect CD16/32 and CD206 expression. The results showed that upon IFN-γ/LPS stimulation, CD16/32 expression increased significantly (P < 0.01) in RAW264.7 with no significant changes in CD206 expression. Following IL-4 stimulation, CD206 expression increased significantly in RAW264.7 compared to unstimulated cells (P < 0.01) while CD16/32 expression did not change (Fig. 1A and 1B). The ELISA assay results indicated that RAW264.7 secreted significantly higher levels of IL-12 following IFN-γ/LPS stimulation compared to cells without stimulation, but almost with no detectable level of IL-10; however, IL-4 stimulated RAW264.7 barely secreted IL-12 but significantly higher levels of IL-10 (P < 0.01) (Fig. 1C). Compared to unstimulated RAW264.7, IFN-γ/LPS stimulated cells expressed significantly higher levels of iNOS gene encoded fragments, but almost no expression of Arg-1 gene coding fragments (P < 0.01); However, IL-4 stimulated RAW264.7 expressed higher levels of Arg-1 gene encoded fragments with significance (P < 0.01), while there was almost no expression of iNOS gene encoded fragments (Fig. 1D).
Fig. 1. Mφ polarization recognition system adopted in this study.
A and B: Percentage of CD16/32+ or CD206+ cells among F4/80+ cells as determined by FACS after IFN-γ/LPS and IL-4 stimulation (compared with unstimulated cells as the control group, ∗P < 0.01). C: IL-12 and IL-10 cytokine levels in the supernatant of RAW264.7 cultures by ELISA after IFN-γ/LPS and IL-4 stimulation (compared with the control group, ∗P < 0.01). D: Relative transcription level of inos and arg1 level in RAW264.7 by real-time PCR after IFN-γ/LPS and IL-4 stimulation (compared with the control group, ∗P < 0.01). The results are shown as mean of three independent experiments.
Different antigens of S. japonicum induced Mφ polarization
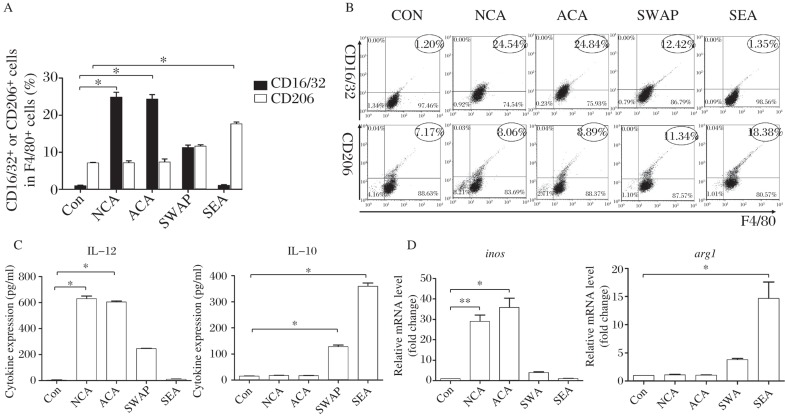
CD16/32 expression increased significantly in RAW264.7 with NCA and ACA stimulation while CD206 expression showed an insignificant difference. CD206 expression increased significantly in RAW264.7 SEA stimulation compared to unstimulated cells (P < 0.01) while CD16/32 expression showed an insignificant difference. SWAP stimulated RAW264.7 expressed both high levels of CD16/32 and CD206 (Fig. 2A and 2B). RAW264.7 secreted significantly higher levels of IL-12 as shown by ELISA with NCA and ACA stimulation compared to cells without stimulation, but almost with no IL-10. However, SEA stimulated RAW264.7 secreted significantly high levels of IL-10 with low levels of IL-12. SWAP stimulated RAW264.7 secreted both high levels of IL-12 and IL-10 (P < 0.01) (Fig. 2C). Compared to unstimulated RAW264.7, NCA and ACA stimulated cells expressed significantly high levels of iNOS gene encoded fragments, but almost no expression of Arg-1 gene encoded fragments (P < 0.01). However, SEA stimulated RAW264.7 expressed high levels of Arg-1 gene encoded fragments with significance (P < 0.01), while almost no expression of iNOS gene encoded fragments. SWAP stimulated RAW264.7 expressed both high levels of iNOS and Arg-1 gene encoded fragments (Fig. 2D).
Fig. 2. Different antigens of S. japonicum induced Mφ polarization.
A and B: Percentage of CD16/32+ or CD206+ cells among F4/80+ cells determined by FACS after NCA, ACA, SWAP and SEA (antigens from different stages of S. japonicum) stimulation compared with unstimulated cells as ( ∗P < 0.01). C: IL-12 and IL-10 cytokine levels in the supernatant of RAW264.7 cultures by ELISA after NCA, ACA, SWAP and SEA stimulation compared with unstimulated cells (∗P < 0.01). D: Relative transcription level of inos and arg1 level in RAW264.7 by RT-PCR after NCA, ACA, SWAP and SEA stimulation compared with unstimulated cells (∗P < 0.01). The results are shown as mean of three independent experiments.
Mφ polarization induced by schistosomal infection
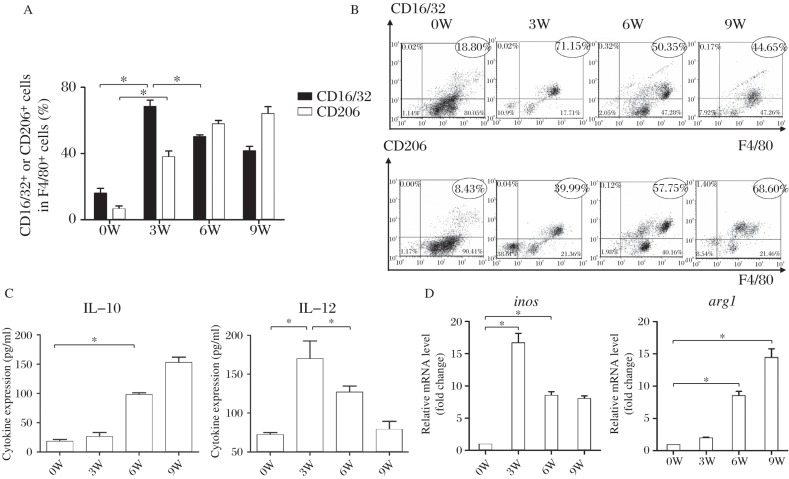
The highest expression of M1 surface marker CD16/32 appeared at 3 weeks after infection, and gradually declined from 6 weeks after infection (P < 0.01). M2 surface marker CD206 expression increased at 3 weeks after infection, reaching to the highest level at 9 weeks after infection (Fig. 3A and 3B). We also detected IL-12 and IL-10 secretion, and iNOS and Arg-1 mRNA expression to identify polarization properties. The results showed that mouse macrophages secreted high levels of IL-12 and before the production of worm egg, and then gradually decreased to a lower level after egg production, while IL-10 levels significantly increased at the time of egg deposition, which is 6 weeks after infection. iNOS mRNA expression reached the highest level at 3 weeks after infection, Arg-1 mRNA expression significantly increased after egg production (Fig. 3C and 3D). These results showed that M1 polarization dominated before egg production while M2 dominated after egg production.
Fig. 3. Mφ polarization during the process of schistosomal infection.
A and B: Percentage of CD16/32+ or CD206+ cells among F4/80+ cells according to FACS of peritoneal macrophages isolated at 0, 3, 6 and 9 weeks after infection (one-way analysis of variance (ANOVA), ∗P < 0.01). C: Dynamics of IL-12 and IL-10 cytokine levels according to ELISA of sera harvested at 0, 3, 6 and 9 weeks after infection (one-way ANOVA, ∗P < 0.01). D: Dynamics of relative transcription level of inos and arg1 level according to RT-PCR of RNA isolated at 0, 3, 6 and 9 weeks after infection (one-way ANOVA, ∗P < 0.01). Data are representative of two independent experiments.
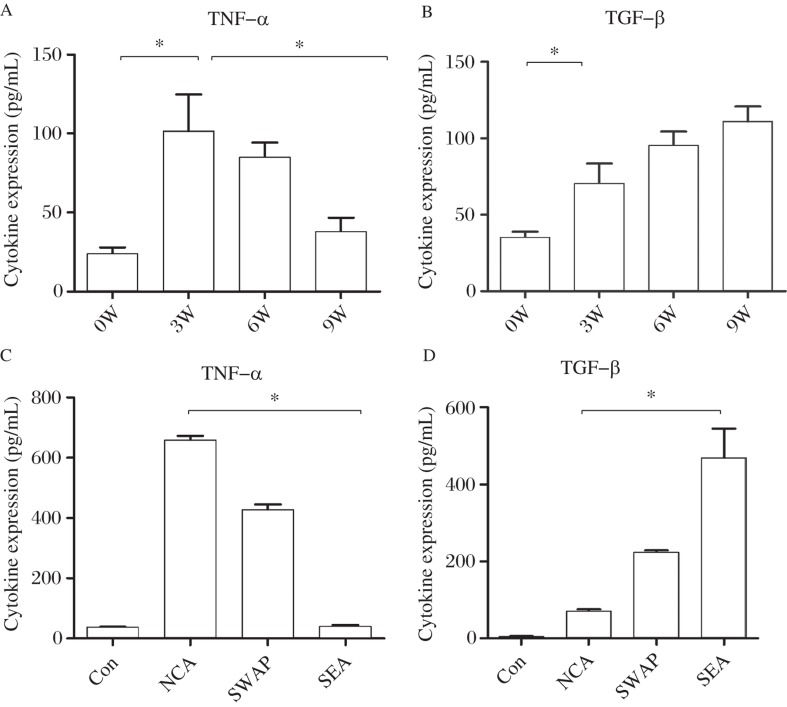
To investigate the Th1/Th2 cytokine levels of polarized macrophages, we used schistosome antigens of different developmental stages as stimuli. The ELISA assay results showed that compared to week 0, TNF-α secretion of peritoneal macrophages reached the highest level at 3 weeks (P < 0.01), and gradually declined from 6 weeks after infection; TGF-β expression increased at 3 weeks after infection, reaching the highest level at 9 weeks after infection (Fig. 4A and 4B). As the cytokine levels of peritoneal macrophage without stimulation were very low, we also used R264.7 cell line to verify the results of in vivo experiment. The results showed that TNF-α expression was significantly increased with NCA stimulation compared to SEA stimulated (P < 0.01); TGF-β expression was significantly increased following SEA stimulation compared to the NCA stimulated group, which was consistent with the in vivo results (Fig. 4C and 4D).
Fig. 4. TNF-a and TGF-b levels detected in different time points and antigents stimulation.
A and B: TNF-α and TGF-β cytokine levels according to ELISA of sera harvested at 0, 3, 6 and 9 weeks after- infection (one-way ANOVA, ∗P < 0.01). C and D: TNF-α and TGF-β cytokine levels in the supernatant of RAW264.7 cultures by ELISA after NCA, ACA, SWAP and SEA (antigens from different stages of S. japonicum) stimulation (one-way ANOVA, ∗P < 0.01). The results are shown as mean of three independent experiments.
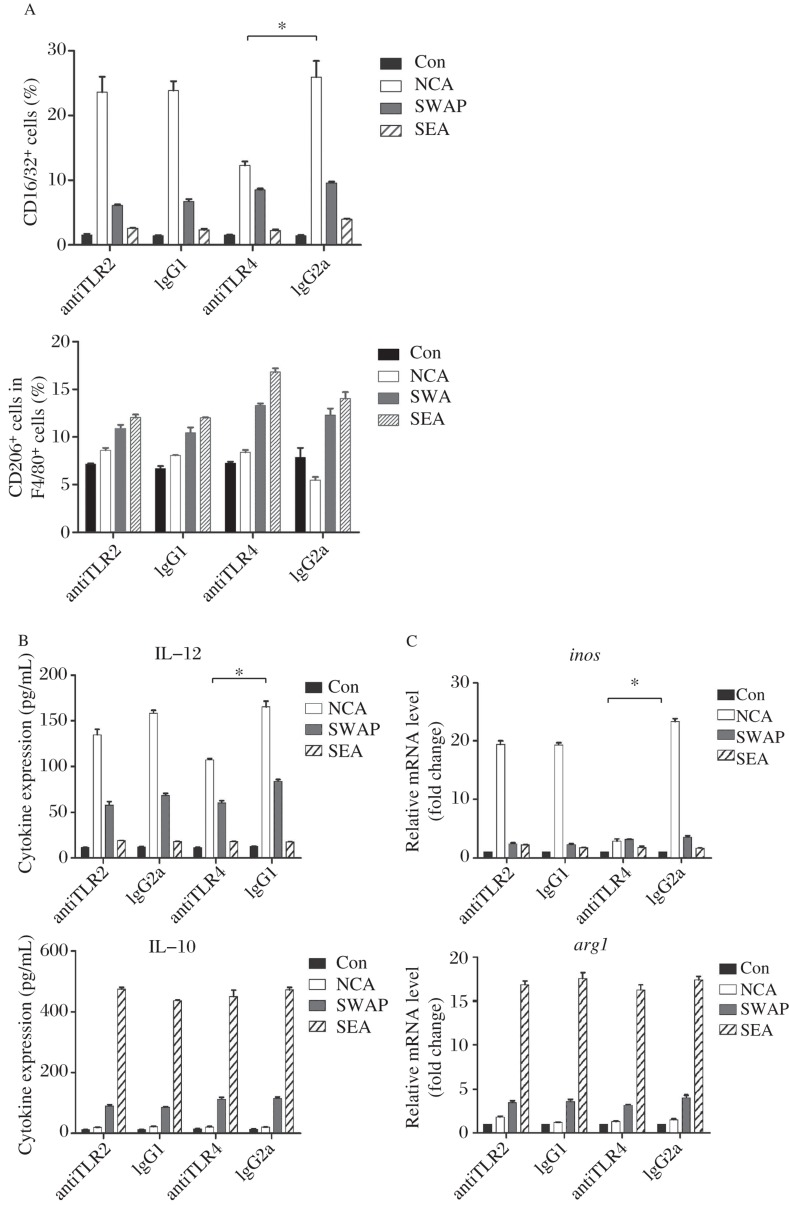
The TLR4 signaling pathway affected macrophage polarization
Flow cytometry showed that when TLR2 pathway was blocked, there was no significant influence in CD16/32 and CD206 expression in RAW264.7 with NCA, SWAP and SEA stimulation compared to the control group (P < 0.01). When the TLR4 pathway was blocked, NCA stimulated Mφ expressed lower levels of CD16/32 compared to the control group (P < 0.01), but with no significant difference in CD206 expression after SWAP and SEA stimulated (Fig. 5A and 5B). When the TLR2 pathway was blocked, there was no significant difference in the levels of IL-12 and IL-10 secretion by RAW264.7 with NCA, SWAP and SEA stimulation stimulated compared to the control group (P < 0.01). When the TLR4 pathway was blocked, NCA stimulated Mφ secreted lower levels of IL-12 compared to the control group (P < 0.01), but with no significant difference in IL-10 expression after SWAP and SEA stimulation (Fig. 5C). When the TLR2 pathway was blocked, there was no significant influence on inos and arg1 expression in RAW264.7 with NCA, SWAP and SEA stimulation compared to the control group (P < 0.01) When the TLR4 pathway was blocked, NCA stimulated Mφ expressed lower levels of inos compared to the control group (P < 0.01), but with no significant difference in arg1 expression after SWAP and SEA stimulation (Fig. 5D).
Fig. 5. The effect of TLR2 and TLR4 on Mφ polarization induced by different S. japonicum antigens.
A: Percentage of CD16/32+ or CD206+ cells among F4/80+ cells as determined by FACS after NCA, SWAP and SEA stimulation when the TLR2 or TLR4 pathway was blocked (compared with the isotype control, ∗P < 0.01). B: IL-12 and IL-10 cytokine levels in the supernatant of RAW264.7 cultures by ELISA after NCA, SWAP and SEA stimulation when the TLR2 or TLR4 pathway was blocked (compared with the isotype control, ∗P < 0.01). C: Relative transcription level of inos and arg1 level in RAW264.7 by RT-PCR after NCA, SWAP and SEA stimulation when the TLR2 or TLR4 pathway was blocked (compared with the isotype control, ∗P < 0.01). The results are shown as mean of 3 independent experiments.
DISCUSSION
S. japonicum experiences several developmental stages in the host. S. japonicum antigens derived from different stages may induce macrophage polarization and regulate immune responses. In this study, in vitro and in vivo experiments demonstrated the relationship between the stimulation of S. japonicum antigens and macrophage polarization, and provided molecular evidence of macrophage differentiation.
Firstly, we built a macrophage polarization recognition system, through which to observe the influence of S. japonicum antigens on macrophage polarization. Although there were functional differences between M1 and M2, their phenotypes were similar. According to the previous study[20], we chose the arginine metabolic pathway (inos, arg-1), surface markers (CD16/32, CD206) and cytokine secretion (IL-12, IL-10) to compose the macrophage polarization recognition system. As classic M1 inducer IFN-γ/LPS and M2 inducer IL-4 can stimulate M1/M2 polarization, we stimulated RAW264.7 (M0) with IFN-γ/LPS and IL-4. The result showed that the system was successfully reproduced under our experimental conditions.
Next, we found that S. japonicum antigens derived from different developmental stages could induced Mφ polarization. M1 marker (CD16/32, IL-12 and inos) expression was significantly increased in RAW264.7 following NCA and ACA stimulation (P < 0.01) while M2 marker (CD206, IL-10, arg1) expression was significantly increased in RAW264.7 following SEA stimulation compared with the control group (P < 0.01). These results showed that in vitro ACA and NCA (before laying eggs) induced M1 polarization, while SEA (after laying eggs) induced M2 polarization. In addition, SWAP could induce both M1 and M2 due to its complicated ingredients (contaminated with SEA).
Further experiments were performed in vivo to detect Mφ polarization shift during S. japonicum natural infection. By using the macrophage polarization recognition system, we detected M1 markers (CD16/32, IL-12 and inos) and M2 markers (CD206, IL-10, arg1) of mouse peritoneal macrophages from different stages of S. japonicum infection. The results showed that M1 polarization dominated before egg production while M2 dominated after egg production. Interestingly, during 3 to 9 weeks after infection, we observed that peritoneal cells were divided into two groups according to F4/80 fluorescence intensity. A small proportion of peritoneal cells did not stain positive for F4/80, and were likely not macrophages. Therefore, we compared macrophage polarization markers within those F4/80-positive cells. We found that a higher percentage of macrophages were positive for CD16/32 at the third week, but gradually decreased to less than 50% at the ninth week. On the other hand, CD206-positive macrophages increased through the course of infection, reaching 76% of all macrophages at the ninth week. This observation in peritoneal macrophages is consistent with macrophage polarization shift observed in vitro.
At the same time, we noticed that macrophages predominantly secreted Th1 cytokines (TNF alpha, IL-12) before egg production, but mainly Th2 cytokines (IL-10, TGF-beta) after egg production, which hypothesized that macrophages polarization regulated immune responses after S. japonicum infection. The results of in vivo and in vitro studies above showed that S. japonicum antigens derived from different developmental stages could induce macrophage polarization and regulate immune microenvironment through secreting cytokines, thus contributing to host immune responses after S. japonicum, such as Th cell shift in cellular immunology.
TLR2 and TLR4 are mainly expressed on cells that are related to the first line defense of the host[21]-[26], including dendritic cells, macrophages, mononuclear cells and neutrophils. Many studies have demonstrated that TLR2 and TLR4 play an important role in infections by viruses, bacteria, fungi and protozoa, and the functions of TLR2 or TLR4 vary according to the nature of pathogens[27]-[30].
Our previous study found that TLR2 and TLR4 deficiencies could lead to opposite results during S. japonicum infection[34]. The enhanced cytokine milieu in TLR2 deficien background was unfavorable for the parasite. On the contrary, TLR4 might be involved in the protection against the infection.
To understand the effect of TLR2 and TLR4 macrophage polarization induced by different S. japonicum antigens, we performed antibody blocking experiment. When TLR2 was blocked, there were no significant changes in both M1 marker (CD16/32, IL-12 and inos) and M2 marker (CD206, IL-10 and arg1) expression after antigen stimulation. However, when TLR4 was blocked, NCA stimulated Mφ expressed significantly lower levels of M1 marker (CD16/32, IL-12 and inos) compared with the isotype control group (P < 0.01), indicating that the TLR4 pathway may be related to M1 polarization, which is in accordance with our previous study[31] that the TLR4 signaling pathway played a protective role in S. japonicum infection. Cheng et al.[32] also found that macrophages were mainly regulated by S. japonicum eggs through the TLR4 signal pathway according to the analysis of microarray data. Recent studies showed that M2 macrophage polarization were related processes orchestrated by p50 nuclear factor κβ through the inhibition of NF-κB-driven, M1-polarizing and IFN-β production[33]. We speculate that the TLR4 signaling pathway may affect Mφ polarization through this downstream molecules-p50 NF-κB, which needs further exploration.
With the development of genetics and molecular biology study, we more in-depth and comprehensive understanding of M1 and M2. In recent years, researchers made progress in the study of characteristic gene expression of M2. The trypanosoma model set up by Namangala et al.[34] has been proved to have guiding significance in the study of alternative activation of macrophage. In the early stage of trypanosome infection, macrophage polarized into M1, while alternatively activated M2 is given priority in the late stage and chronic infection. It explained that macrophages exert both positive and negative effects on immune responses, and this may be related to its polarization. According to immune response shift during S. japonicum infection, we believe that macrophages and schistosomiasis antigen interaction have a key influence on the start-up and regulation of host immune responses.
In summary, changes of antigens in the microenvironment are the key point to the polarization of macrophages during schistosomal infection. S. japonicum antigens can stimulate macrophages to be polarized into different subtypes; thus, different subtypes of macrophages participate in the regulation of immune response caused by S. japonicum infection. Our study provided new interpretation and experimental evidence to uncover the regularity of complex immune responses after schistosome infection.
REFERENCES
- 1.Jia TW, Zhou XN, Wang XH, Utzinger J, Steinmann P, Wu XH. Assessment of the age-specific disability weight of chronic schistosomiasis japonica. Bull World Health Organ. 85:2007. 458–65. doi: 10.2471/BLT.06.033035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ross AG, Bartley PB, Sleigh AC, Olds GR, Li Y, Williams GM, et al. Schistosomiasis. N Engl J Med. 2002;346:1212–20. doi: 10.1056/NEJMra012396. [DOI] [PubMed] [Google Scholar]
- 3.Gryseels B, Polman K, Clerinx J, Kestens L. Human schistosomiasis. Lancet. 2006;368:1106–18. doi: 10.1016/S0140-6736(06)69440-3. [DOI] [PubMed] [Google Scholar]
- 4.Doherty JF, Moody AH, Wright SG. Katayama fever: an acute manifestation of schistosomiasis. BMJ. 1996;313:1071–2. doi: 10.1136/bmj.313.7064.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ross AG, Vickers D, Olds GR, Shah SM, McManus DP. Katayama syndrome. Lancet Infect Dis. 2007;7:218–24. doi: 10.1016/S1473-3099(07)70053-1. [DOI] [PubMed] [Google Scholar]
- 6.Pearce EJ, MacDonald AS. The immunobiology of schistosomiasis. Nat Rev Immunol. 2002;2:499–511. doi: 10.1038/nri843. [DOI] [PubMed] [Google Scholar]
- 7.Ji MJ, Su C, Wu HW, Zhu X, Cai XP, Li CL, et al. Gene expression profile of CD4+ T cells reveals an interferon signaling suppression associated with progression of experimental Schistosoma japonicum infection. Cell Immunol. 2003;224:55–62. doi: 10.1016/j.cellimm.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 8.Ji MJ, Su C, Wang Y, Wu HW, Cai XP, Li GF, et al. Characterization of CD4+ T cell responses in mice infected with Schistosoma japonicum. Acta Biochim Biophys Sin (Shanghai) 2006;38:327–34. doi: 10.1111/j.1745-7270.2006.00169.x. [DOI] [PubMed] [Google Scholar]
- 9.Gordon S. Macrophage heterogeneity and tissue lipids. J Clin Invest. 2007;117:89–93. doi: 10.1172/JCI30992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mosser DM. The many faces of macrophage activation. J Leukoc Biol. 2003;73:209–12. doi: 10.1189/jlb.0602325. [DOI] [PubMed] [Google Scholar]
- 11.Gordon S. Alternative activation of macrophages. Nat Rev Immunol. 2003;3:23–35. doi: 10.1038/nri978. [DOI] [PubMed] [Google Scholar]
- 12.Smith P, Walsh CM, Mangan NE, Fallon RE, Sayers JR, McKenzie AN, et al. Schistosoma mansoni worms induce anergy of T cells via selective up-regulation of programmed death ligand 1 on macrophages. J Immunol. 2004;173:1240–8. doi: 10.4049/jimmunol.173.2.1240. [DOI] [PubMed] [Google Scholar]
- 13.Mantovani A, Sica A, Locati M. Macrophage polarization comes of age. Immunity. 2005;23:344–6. doi: 10.1016/j.immuni.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest. 2007;117:175–84. doi: 10.1172/JCI29881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biswas SK, Gangi L, Paul S, Schioppa T, Saccani A, Sironi M, et al. A distinct and unique transcriptional program expressed by tumor-associated macrophages (defective NF-kappaB and enhanced IRF-3/STAT1 activation). Blood. 2006;107:2112–22. doi: 10.1182/blood-2005-01-0428. [DOI] [PubMed] [Google Scholar]
- 16.Mantovani A, Sica A, Locati M. New vistas on macrophage differentiation and activation. Eur J Immunol. 2007;37:14–6. doi: 10.1002/eji.200636910. [DOI] [PubMed] [Google Scholar]
- 17.Odegaard JI, Ricardo-Gonzalez RR, Goforth MH, Morel CR, Subramanian V, Mukundan L, et al. Macrophage-specific PPARgamma controls alternative activation and improves insulin resistance. Nature. 2007;447:1116–20. doi: 10.1038/nature05894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang X, Goncalves R, Mosser DM. The isolation and characterization of murine macrophages. Curr Protoc Immunol. 2008;Chapter 14:Unit 14.1. doi: 10.1002/0471142735.im1401s83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang M, Gao Y, Du X, Zhang D, Ji M, Wu G.Toll-like receptor (TLR) 2 and TLR4 deficiencies exert differential in vivo effects against Schistosoma japonicum. Parasite Immunol 2011 Apr33(4), 199–209.doi: 10.1111/j.1365-3024.2010.01265.x [DOI] [PubMed] [Google Scholar]
- 20.Li K, Guo Q, Wang C, Chen M, Xu W, Xiong S. Comparative analysis of phenotypes of classically (M1) and alternatively (M2) activated macrophages CURRENT IMMUNOLOLGY. 2008;28:177–183. [Google Scholar]
- 21.Murawski MR, Bowen GN, Cerny AM, Anderson LJ, Haynes LM, Tripp RA, et al. Respiratory syncytial virus activates innate immunity through Toll-like receptor 2. J Virol. 2009;83:1492–500. doi: 10.1128/JVI.00671-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feng CG, Scanga CA, Collazo-Custodio CM, Cheever AW, Hieny S, Caspar P, et al. Mice lacking myeloid differentiation factor 88 display profound defects in host resistance and immune responses to Mycobacterium avium infection not exhibited by Toll-like receptor 2 (TLR2)- and TLR4-deficient animals. J Immunol. 2003;171:4758–64. doi: 10.4049/jimmunol.171.9.4758. [DOI] [PubMed] [Google Scholar]
- 23.Pearl JI, Ma T, Irani AR, Huang Z, Robinson WH, Smith RL, et al. Role of the Toll-like receptor pathway in the recognition of orthopedic implant wear-debris particles. Biomaterials. 32:5535–42. doi: 10.1016/j.biomaterials.2011.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gelani V, Fernandes AP, Gasparoto TH, Garlet TP, Cestari TM, Lima HR, et al. The role of toll-like receptor 2 in the recognition of Aggregatibacter actinomycetemcomitans. J Periodontol. 2009;80:2010–9. doi: 10.1902/jop.2009.090198. [DOI] [PubMed] [Google Scholar]
- 25.Fuse ET, Tateda K, Kikuchi Y, Matsumoto T, Gondaira F, Azuma A, et al. Role of Toll-like receptor 2 in recognition of Legionella pneumophila in a murine pneumonia model. J Med Microbiol 200756(Pt 3), 305–12. [DOI] [PubMed] [Google Scholar]
- 26.Mun HS, Aosai F, Norose K, Chen M, Piao LX, Takeuchi O, et al. TLR2 as an essential molecule for protective immunity against Toxoplasma gondii infection. Int Immunol 200315(9), 1081–7. [DOI] [PubMed] [Google Scholar]
- 27.Campos MA, Almeida IC, Takeuchi O, Akira S, Valente EP, Procópio DO, et al. Activation of Toll-like receptor-2 by glycosylphosphatidylinositol anchors from a protozoan parasite. J Immunol. 2001;167:416–23. doi: 10.4049/jimmunol.167.1.416. [DOI] [PubMed] [Google Scholar]
- 28.Oliveira AC, Peixoto JR, de Arruda LB, Campos MA, Gazzinelli RT, Golenbock DT, et al. Expression of functional TLR4 confers proinflammatory responsiveness to Trypanosoma cruzi glycoinositolphospholipids and higher resistance to infection with T. cruzi. J Immunol. 2004;173:5688–96. doi: 10.4049/jimmunol.173.9.5688. [DOI] [PubMed] [Google Scholar]
- 29.Netea MG, Sutmuller R, Hermann C, Van der Graaf CA, Van der Meer JW, van Krieken JH, et al. Toll-like receptor 2 suppresses immunity against Candida albicans through induction of IL-10 and regulatory T cells. J Immunol. 2004;172:3712–8. doi: 10.4049/jimmunol.172.6.3712. [DOI] [PubMed] [Google Scholar]
- 30.Kurt-Jones EA, Chan M, Zhou S, Wang J, Reed G, Bronson R, et al. Herpes simplex virus 1 interaction with Toll-like receptor 2 contributes to lethal encephalitis. Proc Natl Acad Sci U S A. 2004;101:1315–20. doi: 10.1073/pnas.0308057100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang M, Gao Y, Du X, Zhang D, Ji M, Wu G. Toll-like receptor (TLR) 2 and TLR4 deficiencies exert differential in vivo effects against Schistosoma japonicum. Parasite Immunol. 33:199–209. doi: 10.1111/j.1365-3024.2010.01265.x. [DOI] [PubMed] [Google Scholar]
- 32.Cheng PC, Lin CN, Peng SY, Li LL, Luo TY, Fan CK, et al. A study of immunomodulatory genes responses to macrophages of Schistosoma japonicum infection during different stages by microarray analysis. Acta Trop. 2013;127:251–260. doi: 10.1016/j.actatropica.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 33.Porta C, Rimoldi M, Raes G, Brys L, Ghezzi P, Di Liberto D, et al. Tolerance and M2 (alternative) macrophage polarization are related processes orchestrated by p50 nuclear factor kappaB. Proc Natl Acad Sci U S A. 2009;106:14978–83. doi: 10.1073/pnas.0809784106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Namangala B, Brys L, Magez S, De Baetselier P. Beschin A.Trypanosoma brucei brucei infection impairs MHC class antigen presentation capacity of macrophages. Parasite II Immunol. 2000;22:361–70. doi: 10.1046/j.1365-3024.2000.00314.x. [DOI] [PubMed] [Google Scholar]