Abstract
CD123-positive plasmacytoid dendrocytes are prominent in the infiltrate of discoid lupus erythematosus (LE). We hypothesized that these cells would also be present in hypertrophic LE and would aid in the histopathologic distinction from squamous cell carcinoma (SCC) and hypertrophic actinic keratosis (AK). Five cases of hypertrophic LE and 10 cases each of SCC and hypertrophic AK were stained with CD123. A heavy band of CD123-positive cells was present at the epidermal–dermal junction in all cases of hypertrophic LE, and only single or rare scattered clusters of CD123-positive cells were seen in SCC and actinic keratoses. The pattern of CD123 staining can be a useful feature to distinguish hypertrophic LE from SCC and hypertrophic AK.
Keywords: actinic keratosis, CD123, keratoacanthoma, lupus erythematosus, squamous cell carcinoma
Hypertrophic lupus erythematosus (LE) is considered to be a variant of discoid LE. In hypertrophic LE, verrucous plaques and/or keratoacanthoma-like nodules are found on the face and arms,1–3 and patients generally have concomitant lesions of discoid LE.1,4 Clinically, patients may present with an initial lesion of hypertrophic LE in the absence of other obvious manifestations of LE, in which case the clinical impression generally does not include LE.5 Especially in such cases, there is risk for overdiagnosis of the pseudocarcinomatous hyperplasia present in hypertrophic LE as squamous cell carcinoma (SCC).5
CD123 represents the interleukin-3 receptor alpha chain. It is highly expressed on the surface of plasmacytoid dendrocytes, which are cells that are important in autoimmune responses and are known to accumulate in the infiltrate of various disorders.6–8 Lesions of LE (and related conditions), including subacute cutaneous LE, discoid LE, tumid LE and reticular erythematous mucinosis, have heavy clusters of CD123-positive plasmacytoid dendritic cells as a striking component of the infiltrate.8 Additionally, in discoid LE, the CD123-positive cells form a dense band at the epidermal–dermal junction.8 The staining pattern of hypertrophic LE with CD123 has not been published, to our knowledge. We hypothesized that (i) similar to discoid LE, hypertrophic LE would have a dense band of CD123-positive cells in the superficial dermis; (ii) that SCC and hypertrophic actinic keratoses would lack this positive band; and (iii) that CD123 staining could be used in difficult cases to distinguish hypertrophic LE from SCC.
Materials and methods
Ten cases of inflamed SCC and 10 cases of inflamed hypertrophic actinic keratosis (AK) were collected prospectively and stained with CD123 (BD Pharmingen, San Diego, CA, USA) at 1 : 75 dilution using heat-induced epitope retrieval, pH 6.0, buffer #s1699 (Dako, Carpinteria, CA, USA). All cases were shave biopsies. The cases of SCC and hypertrophic AK displayed epithelial hyperplasia with cytologic atypia and a clinical history compatible with SCC or hypertrophic AK. All 20 lesions had a patchy lichenoid lymphocytic infiltrate.
Five cases of hypertrophic LE were collected retrospectively from the files of the Yale Dermatopathology Laboratory (Table 1). These specimens were from three different patients; for two patients, the diagnosis of hypertrophic LE was made in consensus after presentation at a Dermatology Grand Rounds Conference.
Table 1.
Clinical information for patients with hypertrophic lupus erythematosus
| Site | Sex | Age | Discoid LE? | Clinical dx |
|---|---|---|---|---|
| R palm | F | 41 | N | r/o LE |
| R forearm | F | 49 | N | r/o SCC, LE |
| R upper arm* | M | 62 | Y | r/o SCC |
| R forearm* | M | 62 | Y | r/o SCC |
| R hand* | M | 62 | Y | r/o SCC |
LE, lupus erythematosus; F, female; M, male; N, no; R, right; SCC, squamous cell carcinoma; Y, yes.
From index patient.
Results
The index case was 62 years of age at the time he initially presented. He had lesions of discoid LE on his scalp. Over several years, he continually developed crops of crateriform lesions bilaterally on his heavily sun-damaged arms and hands, and the clinical differential diagnosis included SCC (Fig. 1). Although his initial lesions were diagnosed clinically and histopathologically as SCC; over time, on review of the patient’s lesions in concert with his clinical history, all lesions were deemed to be clinically and histopathologically consistent with hypertrophic LE. Many of his lesions were ultimately treated successfully with intralesional triamcinolone (Fig. 1B).
Fig. 1.
The index patient had keratoacanthoma-like lesions of hypertrophic lupus erythematosus appear in crops over his sun-damaged arms and hands. In panel (A), a crop of lesions is seen. Panel (B) shows partial resolution of the lesions at 1 month after injection of 10 mg/cc intralesional triamcinolone. Panel (C) shows further resolution of the lesions at 8 months time.
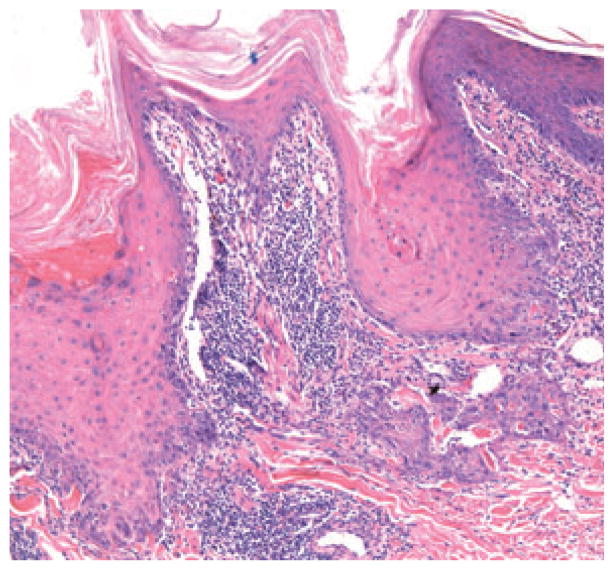
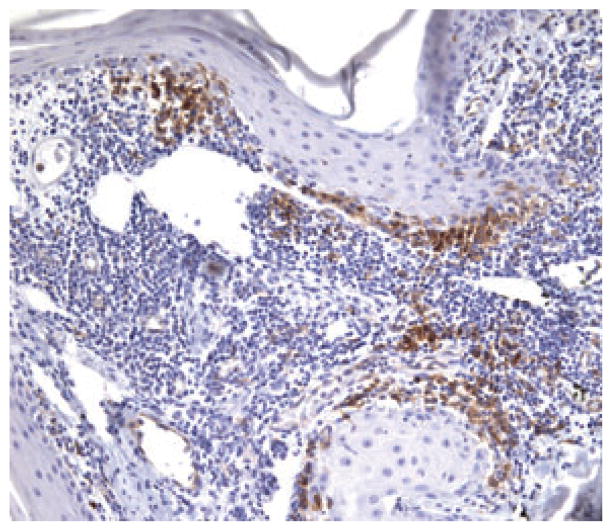
All five lesions of hypertrophic LE showed epithelial hyperplasia with hyperkeratosis, acanthosis and focal irregular buds of keratinocytes in the dermis; focal follicular plugging; elastic fibers in the epidermis; scattered necrotic keratinocytes and vacuolar change in the basal layer; cytologic atypia limited to the periphery of epidermal buds; pigment incontinence and a lichenoid inflammatory infiltrate (Fig. 2). Basement membrane thickening was not prominent, possibly because the combination of a lichenoid infiltrate and basal vacuolar change obscured the junction. Four of five cases were shave biopsies, and neither the depth of the inflammatory infiltrate nor the expression of CD123 in the deeper dermis (including around hair follicles and eccrine glands) could be assessed. An interesting histopathologic finding in all three patients’ biopsies (two of three specimens from the index case) was the presence of eosinophils in the infiltrate. All five lesions of hypertrophic LE showed a dense band of CD123-positive cells in the upper dermis clustered at the dermal–epidermal junction and around superficial follicles (Fig. 3).
Fig. 2.

Hypertrophic lupus erythematosus with pseudocarcinomatous hyperplasia. There is basal vacuolar change, cytologicatypia limited to the periphery of epidermal buds and a lichenoid inflammatory infiltrate.
Fig. 3.
A heavy band of CD123-positive cells is present beneath the epidermis.
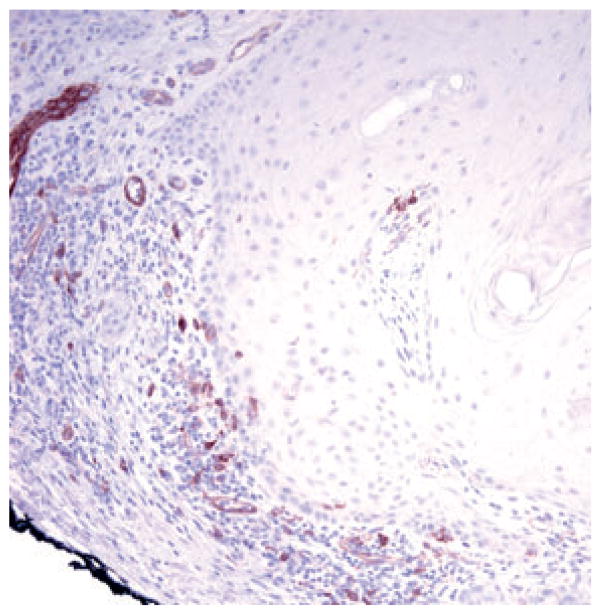
The cases of SCC and hypertrophic AK had cytologic atypicality (often involving multiple levels of the epidermis), absent to minimal vacuolar change, scattered necrotic keratinocytes and patchy lichenoid lymphocytic inflammation. Eight of 10 SCCs had expanded follicular infundibula with hyperkeratosis. Five of 10 SCCs showed engulfment of elastic fibers by atypical keratinocytes. Nine cases of SCC and nine cases of hypertrophic AK showed only scattered positivity with CD123 in single cells (Fig. 4), with one case of SCC and one case of hypertrophic AK showing small clusters of cells.
Fig. 4.
Scattered cells with CD123-positivity in this hypertrophic actinic keratosis.
Discussion
It can be difficult to distinguish hypertrophic LE from inflamed SCC and hypertrophic AK in superficial shave biopsies. On hematoxylin and eosin-stained sections, many features (hyperkeratosis, epithelial hyperplasia, expanded follicular infundibulae, necrotic keratinocytes, entrapped elastic fibers and lichenoid inflammation) can be seen in both hypertrophic LE and inflamed SCC or hypertrophic AK. On our review of 5 cases of hypertrophic LE and 10 cases each of inflamed SCC and hypertrophic AK, the presence of prominent vacuolar change of basal cells was only seen in cases of hypertrophic LE. In addition to this feature, hypertrophic LE showed a band of CD123-positive cells at the dermal–epidermal junction. In contrast, superficial biopsies of inflamed SCC or hypertrophic AK showed only individual or small clusters of CD123-positive cells. We propose the combination of prominent vacuolar change and band-like staining of CD123-positive cells may distinguish cases of hypertrophic LE from inflamed SCC and hypertrophic AK.
Although this is a small series, the literature supports our findings. Hypertrophic LE is considered to be a variant of discoid LE.4 In a recent report, 54 cases of discoid LE showed a similar band of CD123-positive cells at the junction, and prominent clusters of CD123-positive cells were also found around vessels and adnexal structures.8 That study found only scattered CD123-positive cells in the infiltrate of four cases of SCC and two cases of AK.8
While basal vacuolar change and a band of CD123-positive cells both favored a diagnosis of hypertrophic LE in our study, eosinophils and engulfed elastic fibers did not distinguish hypertrophic LE from SCC. Biopsies from all 3 of our patients with hypertrophic LE had eosinophils in the dermal infiltrate, and 3 of 14 patients in a separate study of hypertrophic LE also had eosinophils in the infiltrate.1 Thus, it is important to note that eosinophils are not helpful in differentiating hypertrophic LE from SCC, which may also be accompanied by an eosinophils-containing infiltrate.9 Additionally, although entrapment/engulfment of elastic fibers has been described as a relatively specific feature of hypertrophic LE,1,2 in our series, all lesions of hypertrophic LE and 50% of our cases of SCC showed entrapped elastic fibers within the epidermis. Thus, our results suggest that neither eosinophils nor entrapped elastic fibers are specific for hypertrophic LE.
The diagnosis of hypertrophic LE can be challenging both clinically and histopathologically. Careful clinicopathological correlation can be helpful, as was true for two of our three patients. Clinically, the development of verrucous plaques within pre-existing lesions of discoid LE favors a diagnosis of hypertrophic LE,2 as does the appearance of crops of keratoacanthoma-like nodules on sun-damaged skin, as occurred in our index patient.3 Microscopically, prominent vacuolar change at the epidermal–dermal junction and a heavy band of CD123-positive cells at the junction can be clues to the diagnosis of hypertrophic LE.
References
- 1.Daldon PEC, Macedo de Souza E, Cintra ML. Hypertrophic lupus erythematosus: a clinicopathologic study of 14 cases. J Cutan Pathol. 2003;30:443. doi: 10.1034/j.1600-0560.2003.00082.x. [DOI] [PubMed] [Google Scholar]
- 2.Jolly HW, Carpenter CL. Multiple keratoacanthomata. Arch Dermatol. 1966;93:348. doi: 10.1001/archderm.93.3.348. [DOI] [PubMed] [Google Scholar]
- 3.Fanti PA, Tosti A, Peluso AM, Bonelli U. Multiple keratoacanthoma in discoid lupus erythematosus. J Am Acad Dermatol. 1989;21:809. doi: 10.1016/s0190-9622(89)80282-8. [DOI] [PubMed] [Google Scholar]
- 4.Uitto J, Santa-Cruz DJ, Eisen AZ, Leone P. Verrucous lesions in patients with discoid lupus erythematosus. Br J Dermatol. 1978;98:507. doi: 10.1111/j.1365-2133.1978.tb01936.x. [DOI] [PubMed] [Google Scholar]
- 5.Perniciaro C, Randle HW, Perry HO. Hypertrophic discoid lupus erythematosus resembling squamous cell carcinoma. Dermatol Surg. 1995;21:255. doi: 10.1111/j.1524-4725.1995.tb00167.x. [DOI] [PubMed] [Google Scholar]
- 6.Farkas L, Beiske K, Lund-Johansen F, Brandtzaeg P, Jahnsen FL. Plasmacytoid dendritic cells (natural interferon-alpha/beta-producing cells) accumulate in cutaneous lupus erythematosus lesions. Am J Pathol. 2001;159:237. doi: 10.1016/s0002-9440(10)61689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McNiff JM, Kaplan DH. Plasmacytoid dendritic cells are present in cutaneous dermato-myositis lesions in a pattern distinct from lupus erythematosus. J Cutan Pathol. 2008;35:452. doi: 10.1111/j.1600-0560.2007.00848.x. [DOI] [PubMed] [Google Scholar]
- 8.Tomasini D, Mentzel T, Hantschke M, et al. Plasmacytoid dendritic cells: an overview of their presence and distribution in different inflammatory skin diseases, with special emphasis on Jessner’s lymphocytic infiltrate of the skin and cutaneous lupus erythematosus. J Cutan Pathol. 2010;37:1132. doi: 10.1111/j.1600-0560.2010.01587.x. [DOI] [PubMed] [Google Scholar]
- 9.Lowe D, Fletcher CDM, Shaw MP, McKee PH. Eosinophil infiltration in keratoacanthoma and squamous cell carcinoma of the skin. Histopathology. 1984;8:619. doi: 10.1111/j.1365-2559.1984.tb02374.x. [DOI] [PubMed] [Google Scholar]