Abstract
Background: Foreign bodies cause an aseptic reaction that does not have specific symptoms and may also result in peritonitis, acute abdominal pain, an intraperitoneal abscess, or intestinal obstruction or perforation. We present a case of a surgical instrument left in the abdomen that passed into the transverse colon via migration after a surgery.
Case Description: A 36-year-old female patient was operated upon, with a diagnosis of a hydatid cyst in her liver. Approximately 3 years after the surgery, she excreted part of a surgical forceps with her stool while she was defecating. In upright direct abdominal radiography, a surgical instrument was observed in the abdomen. The patient was operated to remove the foreign body from the abdomen. The surgical instrument that was taken out had corroded and turned black. It was observed that the material that had dropped out of the anus and the material that was taken out during the operation were parts of the same surgical instrument. The ascending colon and the abdomen were stitched anatomically. Follow-ups were conducted after the operation, and the patient was discharged with recovery.
Conclusions: It should be noted that a surgical instrument may be left inside the body of patients who have a history of surgery and that it can migrate.
Keywords: Surgical instrument, taken out, transverse colon
Introduction
Cotton foreign bodies surrounded by a foreign body reaction inside the body are called gossypibomas, and the most common ones are surgical sponges that are left inside the body during a surgery1-3. These materials cause a septic reaction that does not have specific symptoms and may also result in peritonitis, acute abdominal pain, an intraperitoneal abscess, or intestinal obstruction or perforation4,5. Cases of a surgical instrument left in the abdomen during abdominal surgeries are rare. We present a case of a surgical instrument left in the abdomen that passed into the transverse colon via migration after a surgery.
Case report
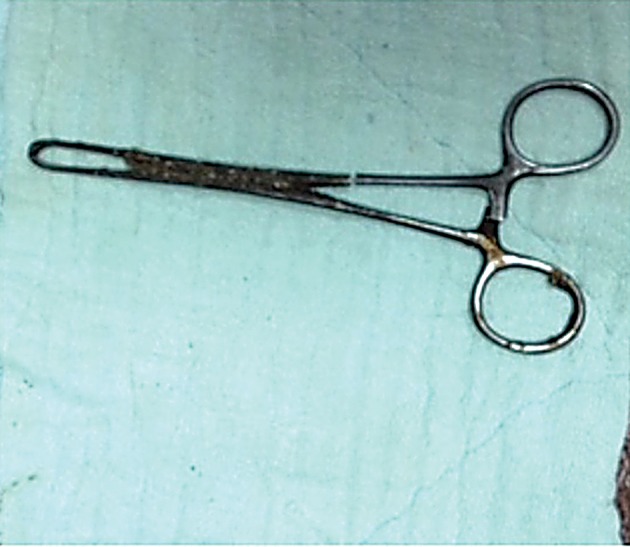
A 36-year-old female patient was operated, with a diagnosis of a hydatid cyst in her liver. Approximately 3 years after the surgery, she excreted a part of a surgical forceps with her stool while she was defecating (Figure 1). She visited a hospital with complaints of abdominal and pelvic pain. She had occasionally suffered from abdominal pain during the 3 years after the surgery. However, she had not presented to a medical service with this complaint. Radiological imaging of the abdomen was performed. In direct radiography, a surgical instrument was observed in the abdomen. The patient was sent to another department. In that department, physical and systemic examination findings were evaluated as normal. The patient was hospitalized with a pre-diagnosis of a foreign body in the abdomen. Direct abdominal radiography was again performed, and superposition of metallic density at the L5 vertebral body level and in the right inferior quadrant was detected (Figure 2). Because of the patient’s surgical history, the material was thought to be a surgical instrument. She was operated to remove the foreign body from the abdomen. During surgery, no pathology was observed inside the abdomen. Furthermore, a foreign body reaction was not observed in the peritoneal cavity. It was found that there was an instrument in parallel with the colon traces in the transverse colon, and the surgical instrument was taken out during the surgery (Figure 3). The surgical instrument that was taken out had corroded and turned black. Moreover, one grip of the instrument was not present. It was observed that the material that had dropped out of the anus and the material that was taken out during the operation were parts of the same surgical instrument (Figure 4). The colon primer and the abdomen were stitched anatomically. Follow-ups were conducted after the operation, and the patient was discharged with full recovery. The patient sued the doctor who conducted the operation and the hospital where the operation was performed.
Figure 1. Approximately 3 years after a surgery, the patient excreted a part of a surgical forceps with her stool while she was defecating.

Figure 2. The surgical instrument was observed in direct abdominal radiography.

Figure 3. The surgical instrument was removed from the transverse colon.
Figure 4. The material that had dropped out of the anus and the material that was taken out during the operation were parts of the same surgical instrument.
Discussion
Foreign bodies inside the body that are forgotten during surgeries occasionally cause symptoms after months and even after years. Our patient had a history of surgery for a hydatid cyst in her liver 3 years before. Operations on the liver are conducted with an open abdomen. Cases in which gauze bandages were left during open abdominal surgeries have been reported in the literature. We have never encountered a case in the literature in which a surgical instrument was taken out of the colon after it was left during a surgery, as in our case. There is no cavity between the abdomen and the transverse colon that allows direct migration. In our case, the surgical instrument was taken out of the 2nd part of the colon. It is known that metallic and other medical materials that are left in the abdomen may stay anywhere in intra-abdominal space and rarely move to the intestine or the colon, based on the literature6-8. We considered the possibility of oral or anal placement of the surgical instrument that was taken out of the transverse colon. We evaluated this possibility to have a low probability because of the size of the surgical instrument and the anatomical obstacles. Therefore, we decided that the surgical instrument that was taken out of the transverse colon had not been placed through the oral or anal route. Approximately 3 years had passed between the surgery during which the surgical instrument was left and the surgery during which the instrument was removed. We believe that the instrument moved from the intra-abdominal space to the transverse colon during this period. Although it is unclear for how long the instrument stayed in the colon, we think that it eroded there and was then easily broken. We also believe that the reason for not previously encountering a finding of migration in the periphery of the transverse colon, where the migration occurred, is a feature of the migration of metallic instruments toward hollow organs in the abdomen. We think that an inflammatory finding may be commonly observed when materials such as a gauze strip move. We are of the opinion that a part of a surgical instrument that is large and taken out after a surgery is not defecated because it has difficulty moving in the colon.
In conclusion, it should be noted that a surgical instrument may be left inside the body of patients who have a history of surgery and that it can migrate. We think that to avoid the risk of a gossypiboma, it is best to count all surgical instruments at least twice (once before the surgery and once after the surgery) and to perform an X ray before discharge.
Conflict of interest
None declared by Authors.
References
- 1.Nemati MH. Mediastinal gossypiboma simulating a malignant tumour. Interact Cardiovasc Thorac Surg. 2012;15:783–785. doi: 10.1093/icvts/ivs260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akbulut S, Arikanoglu Z, Yagmur Y, Basbug M. Gossypibomas mimicking a splenic hydatid cyst and ileal tumor : a case report and literature review. J Gastrointest Surg. 2011;11:2101–2107. doi: 10.1007/s11605-011-1592-9. [DOI] [PubMed] [Google Scholar]
- 3.Gümüş M, Gümüş H, Kapan M, Onder A, Tekbaş G, Baç B. A serious medicolegal problem after surgery: gossypiboma. Am J Forensic Med Pathol. 2012;33:54–57. doi: 10.1097/PAF.0b013e31821c09fe. [DOI] [PubMed] [Google Scholar]
- 4.Paramythiotis D, Michalopoulos A, Papadopoulos VN, Panagiotou D, Papaefthymiou L, Digkas E, et al. Gossypiboma presenting as mesosigmoid abscess [corrected] Tech Coloproctol. 2011;15 Suppl 1:S67–S69. doi: 10.1007/s10151-011-0735-z. [DOI] [PubMed] [Google Scholar]
- 5.Rajković Z, Altarac S, Pape D. An unusual cause of chronic lumbar back pain: retained surgical gauze discovered after 40 years. Pain Med. 2010;11:1777–1779. doi: 10.1111/j.1526-4637.2010.00969.x. [DOI] [PubMed] [Google Scholar]
- 6.Wu SD, Rios RR, Meeks JJ, Nadler RB. Rectal Hem-o-Lok clip migration after robot-assisted laparoscopic radical prostatectomy. Can J Urol. 2009;16:4939–4940. [PubMed] [Google Scholar]
- 7.Modrzejewski A, Kiciak A, Sledż M, Sygit K, Borycka-Kiciak K, Grzesiak W, et al. Migration of a foreign body into the colon and its autonomous excretion. Med Sci Monit. 2011;17:CS34–CS38. doi: 10.12659/MSM.881438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steinhagen E, Khaitov S, Steinhagen RM. Intraluminal migration of mesh following incisional hernia repair. Hernia. 2010;14:659–662. doi: 10.1007/s10029-010-0708-6. [DOI] [PubMed] [Google Scholar]


