Abstract
Objectives. We evaluated the effect of North American public bicycle share programs (PBSPs), which typically do not offer helmets with rentals, on the occurrence of bicycle-related head injuries.
Methods. We analyzed trauma center data for bicycle-related injuries from 5 cities with PBSPs and 5 comparison cities. We used logistic regression models to compare the odds that admission for a bicycle-related injury would involve a head injury 24 months before PBSP implementation and 12 months afterward.
Results. In PBSP cities, the proportion of head injuries among bicycle-related injuries increased from 42.3% before PBSP implementation to 50.1% after (P < .01). This proportion in comparison cities remained similar before (38.2%) and after (35.9%) implementation (P = .23). Odds ratios for head injury were 1.30 (95% confidence interval = 1.13, 1.67) in PBSP cities and 0.94 (95% confidence interval = 0.79, 1.11) in control cities (adjusted for age and city) when we compared the period after implementation to the period before.
Conclusions. Results suggest that steps should be taken to make helmets available with PBSPs. Helmet availability should be incorporated into PBSP planning and funding, not considered an afterthought following implementation.
In the past decade, public bicycle share programs (PBSPs) have become increasingly common in North American cities.1 Often implemented by government agencies, either independently or through a public–private partnership, these networks of bicycles are available for shared use to individuals at some nominal cost relative to the duration of the rental. Such programs are commonly referred to as BIXI programs in Canada (Bicycle-Taxi), and programs in the United States include B-cycle, DecoBike, and CaBi (Capitol Bikeshare in Washington, DC).
Traumatic brain injuries (TBIs) account for the majority of bicycle-related deaths and one third of bicycle-related injuries.2 In 2012, an estimated 81 909 bicycle-related head injuries were treated in US emergency departments.3 Bicycle helmets have been shown to reduce the risk of head, brain, and severe brain injury by 63% to 88%.2 Observational data suggest that fatal TBI risk increases 3-fold when an injured cyclist was not wearing a helmet.4 Educational and advocacy efforts have led to the implementation of mandatory helmet legislation for bicyclists aged younger than 18 years in many American cities and states and in several Canadian cities or provinces. Although no US statewide laws currently exist for adult bicyclists, in Canada, 4 provinces (British Columbia, New Brunswick, Nova Scotia, and Prince Edward Island) have legislation requiring helmets for bicyclists of all ages.5
The popularity of PBSPs in the United States has been met with enthusiasm from the public health community because they provide cardiovascular exercise and an active lifestyle.6,7 Reduced traffic congestion and emissions are added environmental benefits.7,8 It is evident that the presence of PBSPs increases cycling activity among individuals living near available bicycles.9–11 However, PBSPs do not typically provide helmets, and in an evaluation of the barriers and facilitators to the use of a PBSP in Brisbane, Australia (where helmet use is mandatory), 61% of focus group respondents cited helmet inaccessibility or lack of desire to wear one as the main barriers to using the program.12 Accordingly, some PBSPs and cities offer courtesy helmets or free helmet giveaways,12,13 and a pilot project in the District of Columbia offers tourists loaner helmets.14 However, these efforts appear to be limited and are the exception, rather than the rule. Observational studies indicate that the majority of PBSP users do not wear helmets, and thus have significantly higher odds of riding unhelmeted than private bicycle users.9,13,15–17 Recent research in a single North American city suggests that PBSP implementation was not associated with self-reported collisions or near-misses; however, that study was underpowered and was subject to recall bias.18
With more PBSPs potentially resulting in more unhelmeted bicyclists, it is possible that cities with these programs may experience an increase in bicycling-associated head injuries compared with cities with no such programs. Our objective was to assess the effect of PBSPs on the occurrence of bicycle-related head injuries.
METHODS
In this ecological study, we examined nonequivalent comparison groups before and after introduction of PBSPs.19 We compared cities that introduced PBSP programs with cities that did not. We compared the proportion of head injuries among all patients admitted to trauma centers with bicycling-related injuries before PBSP implementation (preintervention) to the proportion after implementation (postintervention). We hypothesized that we would observe a significant increase in the proportion of bicycling-related head injuries in PBSP, but no difference between time periods in control cities.
We selected 10 cities for this study, 5 with PBSPs and 5 comparison cities (Table 1). Intervention dates for cities with PBSPs were based on the first month during which the PBSP was implemented. For cities with programs that had a small pilot PBSP that expanded over time, the intervention date was based on month and year of the expansion if it constituted a more than 75% increase in the number of stations or bicycles (Table 1). We selected comparison cities in similar geographic regions and assigned these the same intervention dates as the similar PBSP cities. We obtained data for the 24 months preceding and the 12 months following the intervention date for each city. None of the PBSP cities had free bicycle helmet distribution or helmet rental programs active during the study period.
TABLE 1—
Characteristics of Study Cities With Public Bicycle Share Programs and Controls: North America
| PBSP Information (After Implementation) |
||||||
| Cities | Intervention Datea | Preimplementation Dates | Postimplementation Dates | Population (2011),b No. | Stations, No. | Bicycles, No. |
| PBSP cities | ||||||
| Montreal, QC | May 2009 | May 1, 2007–April 30, 2009 | May 1, 2009–April 30, 2010 | 1 649 519 | 405 | 5120 |
| Washington, DC | May 2010c | May 1, 2008–April 30, 2010 | May 1, 2010–April 30, 2011 | 617 996 | 120 | 1670 |
| Minneapolis, MN | July 2011d | July 1, 2009–June 30, 2011 | July 1, 2011–June 30, 2012 | 387 753 | 70 | 1330 |
| Boston, MA | July 2012e | July 1, 2010–June 30, 2012 | July 1, 2012–June 30, 2013 | 625 087 | 600 | 1000 |
| Miami Beach, FL | March 2011 | March 1, 2009–February 28, 2011 | March 1, 2011–February 28, 2012 | 89 840 | 100 | 1000 |
| Control cities | ||||||
| Vancouver, BC | May 2009 | May 1, 2007–April 30, 2009 | May 1, 2009–April 30, 2010 | 603 502 | . . . | . . . |
| New York, NY | May 2010 | May 1, 2008–April 30, 2010 | May 1, 2010–April 30, 2011 | 8 244 910 | . . . | . . . |
| Milwaukee, WI | July 2011 | July 1, 2009–June 30, 2011 | July 1, 2011–June 30, 2012 | 597 867 | . . . | . . . |
| Seattle, WA | July 2011 | July 1, 2009–June 30, 2011 | July 1, 2011–June 30, 2012 | 620 778 | . . . | . . . |
| Los Angeles, CA | March 2011 | March 1, 2009–February 28, 2011 | March 1, 2011– February 28, 2012 | 3 819 702 | . . . | . . . |
Note. PBSP = public bicycle share program. Preimplementation period consists of the 24 months before intervention date. Postimplementation period consists of a 12-month period following intervention.
Intervention date was constructed for control cities to correspond with matched PBSP city. Some cities initially piloted PBSP programs before expanding the systems. In this case, the intervention date was based on month and year of the expansion if it constituted a > 75% increase in the number of stations or bicycles in the city.
City population based on 2011 census values.
Washington, DC, piloted the PBSP in 2008 with 10 stations and 120 bicycles and expanded to 175 stations and 1670 bicycles in May 2010. Because of the large expansion (1650% more stations and 1292% more bicycles), we chose the intervention date for this city to be the year of the expansion.
The Minneapolis PBSP started in June 2010 with 65 stations and 700 bicycles and increased in mid-2011 to 116 stations (79% increase) and 1330 bicycles (90% increase); therefore, we chose July 2011 as the implementation date for Minneapolis.
In Boston, the PBSP started in late July 2011 with 60 bicycles and 600 stations, and increased to 108 stations (80% increase) and more than 1000 bicycles (> 67% increase) through 2012. Therefore, we chose the implementation date for Boston as July 2012.
Data Sources and Variables
City-level data on trauma admissions were provided by the National Trauma Data Bank (NTDB) for US cities, by the British Columbia Trauma Registry for Vancouver, and the Quebec Trauma Registry for Montreal. The data on trauma admissions in the NTDB and the 2 Canadian systems are based on similar eligibility criteria. From each source we requested the following data elements, stratified by month and age group (< 15 years, 15–24 years, 25–49 years, ≥ 50 years, age missing): total number of bicycle-related trauma patients and total number of bicycle-related trauma patients with head injuries. Head injuries included brain injuries and skull fractures. Head injury cases were further categorized as mild or moderate to severe on the basis of the abbreviated injury score (AIS) for the head-and-neck region: AIS less than 3 was classified as mild and AIS 3 or greater was classified as moderate to severe.
Each data source provided data in aggregate form and we expanded them to anonymous individual-level data with the RESHAPE command in Stata SE version 11.2 (StataCorp LP, College Station, TX). We constructed the following variables for each individual: injury type (head or other), age (previously mentioned categories), head injury severity, city, city type (PBSP or control), and exposure. Exposure was based on whether the injury occurred before the PBSP intervention (preimplementation) or after (postimplementation). To maintain patient and hospital confidentiality, city names and dates were blinded to the authors.
Analysis
To illustrate the temporal variation in bicycling-related head injuries in PBSP and control cities, we graphed the proportion of patients with head injuries among those admitted with bicycling-related injuries over time, with time categorized into quarters. We compared the proportions between pre- and postintervention time periods for both PBSP and control cities by using χ2 analysis. In a logistic regression model evaluating the association between head injury and implementation of PBSP, we first evaluated the significance of an interaction term, which comprised city type (PBSP or comparison) and time (pre- or postimplementation). A significant interaction term would lead to stratification of analysis, and all subsequent results would be derived from 2 separate logistic models, one for each of control and PBSP cities. Otherwise, a combined logistic model would be used. Models included the variables for exposure, age, and an indicator variable for city. We felt the use of a city variable would address potential confounding at the city level, such as infrastructure, policies, and other unmeasured factors. Although a hierarchical model might have been preferred, there were insufficient observations to allow for robust estimates.
We conducted 2 sensitivity analyses. First, because head injuries were relatively common bicycling-related injuries, we conducted an additional analysis that compared adjusted odds ratios to relative risk ratios from modified Poisson regression with robust standard variance.20 Second, although PBSPs require parental approval for children, age restrictions vary across cities. We conducted a separate sensitivity analysis restricting the sample to individuals aged 15 years and older. We conducted sensitivity analyses in the same manner described for the primary analysis, including testing for interaction and using separate, stratified models when warranted.
We set statistical significance at P < .05. We conducted all analyses with Stata SE version 11.2.
RESULTS
We chose 10 cities for this study (5 with PBSPs and 5 serving as controls), of which 2 were located in Canada and 8 in the United States (Table 1). Among chosen cities, Montreal was the first to implement its PBSP, in May 2009, and Boston was last, in July 2012. Additional information about PBSPs and control cities is provided in Table 1.
Injured individuals were predominantly aged 25 to 49 years (Table 2), with a greater proportion of injuries occurring among younger (< 15 years) individuals in PBSP cities (24.3%) than control cities (16.4%). Head injuries were most often classified as moderate to severe.
TABLE 2—
Characteristics of Injuries in Public Bicycle Share Program Cities and Control Cities: North America, 2007–2012
| Preimplementation |
Postimplementation |
|||
| Characteristics | Nonhead Injuries, No. (%) | Head Injuries, No. (%) | Nonhead Injuries, No. (%) | Head Injuries, No. (%) |
| PBSP cities | ||||
| Total sample | 875 | 638 | 272 | 273 |
| Age, y | ||||
| < 15 | 246 (28.1) | 145 (22.7) | 55 (20.2) | 54 (19.8) |
| 15–24 | 115 (13.1) | 120 (18.8) | 30 (11.0) | 42 (15.4) |
| 25–49 | 274 (31.3) | 193 (30.3) | 112 (41.2) | 99 (36.3) |
| ≥ 50 | 203 (23.2) | 143 (22.4) | 63 (23.2) | 58 (21.3) |
| Unknown | 37 (4.2) | 37 (5.8) | 12 (4.4) | 20 (7.3) |
| Head injury severitya | ||||
| Mild | . . . | 169 (26.5) | . . . | 79 (29.4) |
| Moderate to severe | . . . | 324 (50.8) | . . . | 119 (44.2) |
| Unknown | . . . | 145 (22.7) | . . . | 71 (26.4) |
| Control cities | ||||
| Total sample | 1151 | 712 | 611 | 342 |
| Age, y | ||||
| < 15 | 185 (16.1) | 141 (19.8) | 80 (13.1) | 55 (16.1) |
| 15–24 | 268 (23.3) | 139 (19.5) | 158 (25.9) | 66 (19.3) |
| 25–49 | 402 (34.9) | 260 (36.5) | 229 (37.5) | 132 (38.6) |
| ≥ 50 | 251 (21.8) | 143 (20.1) | 115 (18.8) | 74 (21.6) |
| Unknown | 45 (3.9) | 29 (4.1) | 29 (4.8) | 15 (4.4) |
| Head injury severitya | ||||
| Mild | . . . | 132 (18.5) | . . . | 68 (19.9) |
| Moderate to severe | . . . | 361 (50.7) | . . . | 192 (56.1) |
| Unknown | . . . | 219 (30.8) | . . . | 82 (24.0) |
Note. PBSP = public bicycle share program. Preimplementation period consists of the 24 months before intervention date. Postimplementation period consists of a 12-month period following intervention. Intervention date was constructed for control cities to correspond with matched PBSP city. The PBSP cities were Montreal, QC; Washington, DC; Minneapolis, MN; Boston, MA; and Miami Beach, FL. The control cities were Vancouver, BC; New York, NY; Milwaukee, WI; Seattle, WA; and Los Angeles, CA. Percentages may not add to 100 because of rounding.
Injury severity groups were based on the abbreviated injury score (AIS) for the head-and-neck region: AIS < 3 was classified as mild and AIS ≥ 3 was classified as moderate to severe.
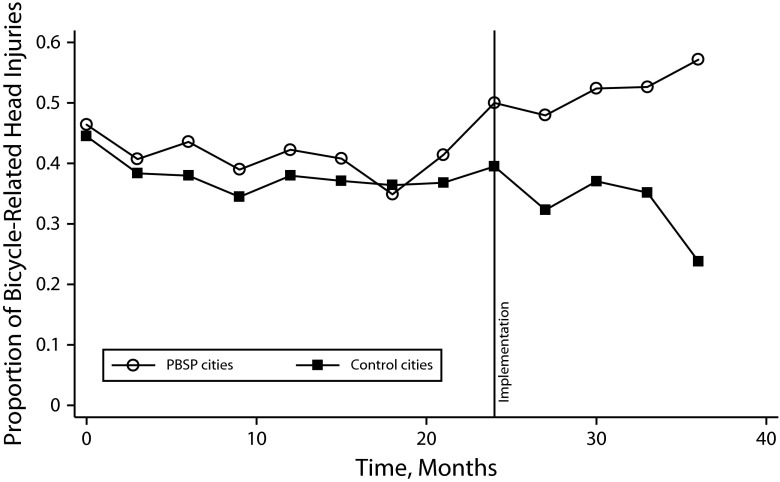
Over the 36-month study period, 2058 bicycle-related injuries were treated in trauma centers in PBSP cities and 2816 were treated in control cities. Among patients admitted to trauma centers in PBSP cities, 42.3% (n = 638) in the preimplementation period had head injuries, compared with 50.1% (n = 273) after PBSP implementation (P < .01; Figure 1). In control cities, we observed similar proportions of head injuries during these 2 periods (38.2%; n = 712 before implementation; and 35.9%; n = 342 after implementation; P = .23).
FIGURE 1—
Proportion of all bicycle-related injuries that were classified as head injuries among cities with public bike share programs and control cities, centered on intervention date (indicated by vertical line): North America.
Note. PBSP = public bicycle share program. The PBSP cities were Montreal, QC; Washington, DC; Minneapolis, MN; Boston, MA; and Miami Beach, FL. The control cities were Vancouver, BC; New York, NY; Milwaukee, WI; Seattle, WA; and Los Angeles, CA. Proportions are unadjusted.
We estimated separate logistic regression models for PBSP and control cities, because of effect modification between exposure (pre- vs postimplementation) and city type (interaction term significance, P = .02) For PBSP cities, the unadjusted odds ratio (OR) comparing the odds of bicycle-related head injury before and after PBSP implementation was 1.37 (95% confidence interval [CI] = 1.13, 1.67; Table 3). Adjusting for age and city did not substantially change the magnitude of the association or its significance (OR = 1.30; 95% CI = 1.05, 1.62). For control cities, the adjusted OR was not significant (OR = 0.94; 95% CI = 0.79, 1.11), indicating no change in the proportion of bicycle-related injuries that involved the head. These results suggest that in cities with PBSPs, holding age and city constant, the odds that bicycle-related injury was a head injury increased 30% (95% CI = 5%, 62%) following PBSP implementation. In cities without PBSPs, we did not observe a statistically significant change in the odds that bicycle-related injury was a head injury over a comparable time period (6% decrease; 95% CI = –21%, 11%). Testing for the difference in the independent, nonnested log ORs indicated significance (P = .03).
TABLE 3—
Results From Logistic Regression Analyses Showing the Association Between Public Bicycle Share Program Implementation and the Odds of a Bicycle-Related Injury Being a Head Injury: North America, 2007–2012
| PBSP Cities |
Comparison Cities |
|||
| Variable | OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) |
| Time | ||||
| Preimplementation (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Postimplementation | 1.37 (1.13, 1.67) | 1.30 (1.05, 1.62) | 0.91 (0.79, 1.06) | 0.94 (0.79, 1.11) |
| Age, y | ||||
| < 15 | . . . | 0.80 (0.62, 1.02) | . . . | 1.19 (0.94, 1.50) |
| 15–24 | . . . | 1.54 (1.16, 2.03) | . . . | 0.87 (0.70, 1.08) |
| 25–49 (Ref) | . . . | 1.00 | . . . | 1.00 |
| ≥ 50 | . . . | 1.05 (0.82, 1.35) | . . . | 0.94 (0.76, 1.17) |
| Unknown | . . . | 1.57 (1.03, 2.39) | . . . | 0.96 (0.64, 1.44) |
Note. AOR = adjusted odds ratio; CI = confidence interval; OR = odds ratio (unadjusted); PBSP = public bicycle share program. We conducted separate models for PBSP and comparison cities because of the effect modification observed between city type and time. Unadjusted ORs show results from regression with only exposure variable. The AORs were adjusted for the following covariates in multivariable regression: exposure, age, and an indicator for each city. The PBSP cities were Montreal, QC; Washington, DC; Minneapolis, MN; Boston, MA; and Miami Beach, FL. The control cities were Vancouver, BC; New York, NY; Milwaukee, WI; Seattle, WA; and Los Angeles, CA.
Results from the sensitivity analysis with modified Poisson regression were directionally consistent with logistic regression analyses (incidence rate ratio for PBSP cities = 1.14; 95% CI = 1.03, 1.27; and incidence rate ratio for comparison cities = 0.96; 95% CI = 0.87, 1.06; Table A, available as a supplement to this article at http://www.ajph.org). Analyses restricted to patients aged older than 15 years showed ORs that, although not significant, were directionally consistent with the full, all-ages model for both PBSP and comparison cities (Table B, available as a supplement to this article at http://www.ajph.org).
DISCUSSION
In this international study, implementation of a PBSP was associated with 14% greater risk of head injury among patients admitted to trauma centers for bicycle-related injuries. Although the odds of head injury among injured bicyclists increased in PBSP cities after program implementation, a similar change was not observed in comparison cities. The age restrictions for PBSP use vary across cities, and parents can provide approval in some cities. Our sensitivity analysis for patients older than 15 years showed directionally consistent effects as the full, unrestricted models. However, because children may use some PBSPs with a parent’s approval and restrictions vary across cities, the more reliable results are reported in the full models.
Public bicycle share programs do not typically provide access to helmets, resulting in many PBSP users not using these protective devices. An observational study of PBSP users in Boston, Massachusetts, and Washington, DC, found that only 19.2% of users wore helmets, compared with 51.4% of non-PBSP bicyclists.9 A similar study in New York City found that 85.3% of PBSP users were riding unhelmeted.17 Other US and Canadian studies have found that helmet use was significantly less common among PBSP users than other cyclists.13,15,16 The inclination of PBSP users to ride unhelmeted is worrisome, in light of the protective effect of bicycle helmets on head injury.2 The conclusion of our study—that PBSP implementation is associated with increased odds that a person admitted for a bicycling-related injury would have a head injury—is likely attributable to the low propensity of PBSP cyclists to use helmets. Because trauma registries often lack sufficient data on protective device use, however, we were not able to include this variable in our analyses.
Limitations
This study has several limitations. As noted previously, patient-level data were not available, so it is not possible to know whether an individual patient was using a PBSP. Our study is not population-based as it only includes patients admitted to trauma centers, and is therefore heavily influenced by more severe injuries, including TBIs. Because these injuries are a major determinant of admission (and therefore inclusion in a trauma registry), this limitation would have only biased the results to the null. Additional limitations arise as a result of limited follow-up time. Because PBSPs are a relatively new phenomenon, we were only able to consider a postimplementation period of 12 months. Evaluating follow-up for longer might lead to different results, because of a potential interaction between time and helmet use; this is an important avenue for further research. Although a segmented time series analysis or other longitudinal analysis was our initial intention, at least 48 time points are recommended for these designs.21 Finally, to preserve patient confidentiality for all trauma systems involved in this study, we were blinded to city and time. Therefore, data on city-level characteristics (e.g., population, ridership) were not available for analyses, and we were not able to adjust for seasonal autocorrelation (other than matching implementation dates in similar control and PBSP cities).
The slight jump in the proportion of head injuries in PBSP cities in the quarter before PBSP implementation might suggest some inaccuracies in the choice of intervention date for some of these cities. (These potential inaccuracies are described in the Methods section.) Alternatively, forthcoming initiatives in PBSP cities could have prompted greater awareness or improved infrastructure, which in turn led to increased bicycle ridership and associated head injuries.
Public bicycle share programs are promoted as public health interventions that increase physical activity, reduce greenhouse gases, and foster a walking- and bicycle-friendly community.6–8 Although the benefits of PBSPs may appear evident,22 if users do not wear protective bicycle helmets, they may expose themselves to increased risk of head injury. Solid data from well-designed studies support the effectiveness of bicycle helmets and legislation mandating their use,2,23–25 however, some authors continue to oppose these measures often for reasons that have no bearing on safety.26,27 Providing a helmet for PBSP riders is conceptually and logistically challenging. Carrying or purchasing a personal helmet may reduce the spontaneity of PBSP use and may simply be impractical for some.12 Strategies to increase helmet wearing include social media campaigns, free helmet giveaways, hotel-based helmet loan initiatives for tourists, and PBSP-provided courtesy helmets.12–14,28 Rental helmets are becoming increasingly popular and vending devices have been developed to allay hygiene concerns, resulting in some large cities being able to also provide helmets at PBSP dispensing stations.29
Conclusions
Although PBSPs may promote healthy and environmentally conscious lifestyles, this study suggests that, at the city level, PBSP implementation is associated with increased risk of bicycle-related head injuries. Promotion of helmet use through integrated rental programs should be a critical element of all PBSPs. This would provide users with the opportunity to reap the benefits of the PBSP while contributing to their safety.
POSTSCRIPT
It has come to the author's attention that the PBSP implementation date attributed to Washington, DC, in this article may be inaccurate. Because the analysis was blinded to city names, post hoc alteration of the date was not possible. However, individually shifting the implementation date for each city did not overly influence the results or change the overall conclusions of this study.
One additional limitation of this study was not explicitly noted in the article. This study was not able to evaluate the changes in ridership before and after PBSP implementation, so the absolute number of injuries in the cities could not be used a reliable outcome measure.
Acknowledgments
J. M. Graves received fellowship support from National Institute of Child Health and Human Development during the course of this research (PI: Rivara, T32 HD057822-01A2). This work was also supported by the Harborview Injury Prevention and Research Center, University of Washington, the National Trauma Data Bank, the Quebec Trauma Registry, and the Vancouver Trauma Registry.
The authors thank Jennifer M. Whitehill, PhD, for her critical review of and assistance with analytical approaches for this study.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Human Participant Protection
Human participant approval was not required (data were aggregated and contained no direct identifiers); however, review was requested and provided by the University of British Columbia Research Ethics Board.
References
- 1.Fishman E, Washington S, Haworth N. Bike share: a synthesis of the literature. Transp Rev. 2013;33(2):148–165. [Google Scholar]
- 2.Thompson DC, Rivara FP, Thompson R. Helmets for preventing head and facial injuries in bicyclists. Cochrane Database Syst Rev. 2000;(2):CD001855. doi: 10.1002/14651858.CD001855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Consumer Product Safety Commission. National Electronic Injury Surveillance System (NEISS) Available at: https://www.cpsc.gov/cgibin/NEISSQuery/home.aspx. Accessed August 23, 2013.
- 4.Persaud N, Coleman E, Zwolakowski D, Lauwers B, Cass D. Nonuse of bicycle helmets and risk of fatal head injury: a proportional mortality, case–control study. CMAJ. 2012;184(17):E921–E923. doi: 10.1503/cmaj.120988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bicycle Helmet Research Foundation. Helmet laws: what has been their effect? Available at: http://www.cyclehelmets.org/1096.html. Accessed August 30, 2013.
- 6.Johan de Hartog J, Boogaard H, Nijland H, Hoek G. Do the health benefits of cycling outweigh the risks? Environ Health Perspect. 2010;118(8):1109–1116. doi: 10.1289/ehp.0901747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rojas-Rueda D, de Nazelle A, Tainio M, Nieuwenhuijsen MJ. The health risks and benefits of cycling in urban environments compared with car use: health impact assessment study. BMJ. 2011;343:d4521. doi: 10.1136/bmj.d4521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maibach E, Steg L, Anable J. Promoting physical activity and reducing climate change: opportunities to replace short car trips with active transportation. Prev Med. 2009;49(4):326–327. doi: 10.1016/j.ypmed.2009.06.028. [DOI] [PubMed] [Google Scholar]
- 9.Fischer CM, Sanchez CE, Pittman M et al. Prevalence of bicycle helmet use by users of public bikeshare programs. Ann Emerg Med. 2012;60(2):228–231. doi: 10.1016/j.annemergmed.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 10.Fuller D, Gauvin L, Kestens Y et al. Impact evaluation of a public bicycle share program on cycling: a case example of BIXI in Montreal, Quebec. Am J Public Health. 2013;103(3):e85–e92. doi: 10.2105/AJPH.2012.300917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fuller D, Gauvin L, Kestens Y, Morency P, Drouin L. The potential modal shift and health benefits of implementing a public bicycle share program in Montreal, Canada. Int J Behav Nutr Phys Act. 2013;10:66. doi: 10.1186/1479-5868-10-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fishman E, Washington S, Haworth N. Barriers and facilitators to public bicycle scheme use: a qualitative approach. Transp Res Part F Traffic Psychol Behav. 2012;15(6):686–698. [Google Scholar]
- 13.Kraemer JD, Roffenbender JS, Anderko L. Helmet wearing among users of a public bicycle-sharing program in the District of Columbia and comparable riders on personal bicycles. Am J Public Health. 2012;102(8):e23–e25. doi: 10.2105/AJPH.2012.300794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.District of Columbia Department of Transportation. District Department of Transportation and Capital Bikeshare launch pilot program with Kimpton hotels to launch safe bicycling to visitors. 2011. Available at: http://adamsmorgan.wusa9.com/news/news/ddot-and-capital-bikeshare-launch-pilot-program-kimpton-hotels/61972. Accessed July 17, 2013.
- 15.Grenier T, Deckelbaum DL, Boulva K et al. A descriptive study of bicycle helmet use in Montreal, 2011. Can J Public Health. 2013;104(5):e400–e404. doi: 10.17269/cjph.104.3936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bonyun M, Camden A, Macarthur C, Howard A. Helmet use in BIXI cyclists in Toronto, Canada: an observational study. BMJ Open. 2012;2(3):pii:e001049. doi: 10.1136/bmjopen-2012-001049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basch CH, Ethan D, Rajan S, Samayoa-Kozlowsky S, Basch CE. Helmet use among users of the Citi Bike Bicycle-Sharing Program: a pilot study in New York City. J Community Health. 2014;39(3):503–507. doi: 10.1007/s10900-013-9785-7. [DOI] [PubMed] [Google Scholar]
- 18.Fuller D, Gauvin L, Morency P, Kestens Y, Drouin L. The impact of implementing a public bicycle share program on the likelihood of collisions and near misses in Montreal, Canada. Prev Med. 2013;57(6):920–924. doi: 10.1016/j.ypmed.2013.05.028. [DOI] [PubMed] [Google Scholar]
- 19.Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston, MA: Houghton Mifflin Company; 2002. [Google Scholar]
- 20.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 21.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 22.Woodcock J, Tainio M, Cheshire J, O’Brien O, Goodman A. Health effects of the London bicycle sharing system: health impact modelling study. BMJ. 2014;348:g425. doi: 10.1136/bmj.g425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thompson DC, Rivara FP, Thompson RS. Effectiveness of bicycle safety helmets in preventing head injuries. A case–control study. JAMA. 1996;276(24):1968–1973. [PubMed] [Google Scholar]
- 24.Thompson RS, Rivara FP, Thompson DC. A case–control study of the effectiveness of bicycle safety helmets. N Engl J Med. 1989;320(21):1361–1367. doi: 10.1056/NEJM198905253202101. [DOI] [PubMed] [Google Scholar]
- 25.Macpherson AK, To TM, Macarthur C, Chipman ML, Wright JG, Parkin PC. Impact of mandatory helmet legislation on bicycle-related head injuries in children: a population-based study. Pediatrics. 2002;110(5):e60. doi: 10.1542/peds.110.5.e60. [DOI] [PubMed] [Google Scholar]
- 26.Dennis J, Ramsay T, Turgeon AF, Zarychanski R. Helmet legislation and admissions to hospital for cycling related head injuries in Canadian provinces and territories: interrupted time series analysis. BMJ. 2013;346:f2674. doi: 10.1136/bmj.f2674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldacre B, Spiegelhalter D. Bicycle helmets and the law. BMJ. 2013;346:f3817. doi: 10.1136/bmj.f3817. [DOI] [PubMed] [Google Scholar]
- 28.Ethan D, Basch CE. Using social marketing as a tool to increase helmet use among bicycle-share riders in urban settings. J Mass Communicat Journalism. 2013;3:e7. [Google Scholar]
- 29.Pasquarelli A. Citi Bike to provide helmet rentals. Crain’s New York Business. 2013 Available at: http://www.crainsnewyork.com/article/20130725/TRANSPORTATION/130729922. Accessed October 1, 2013. [Google Scholar]