Abstract
Objectives. We examined the impact of community mobilization (CM) on the empowerment, risk behaviors, and prevalence of HIV and sexually transmitted infection in female sex workers (FSWs) in Karnataka, India.
Methods. We conducted behavioral–biological surveys in 2008 and 2011 in 4 districts of Karnataka, India. We defined exposure to CM as low, medium (attended nongovernmental organization meeting or drop-in centre), or high (member of collective or peer group). We used regression analyses to explore whether exposure to CM was associated with the preceding outcomes. Pathway analyses explored the degree to which effects could be attributable to CM.
Results. By the final survey, FSWs with high CM exposure were more likely to have been tested for HIV (adjusted odd ratio [AOR] = 25.13; 95% confidence interval [CI] = 13.07, 48.34) and to have used a condom at last sex with occasional clients (AOR = 4.74; 95% CI = 2.17, 10.37), repeat clients (AOR = 4.29; 95% CI = 2.24, 8.20), and regular partners (AOR = 2.80; 95% CI = 1.43, 5.45) than FSWs with low CM exposure. They were also less likely to be infected with gonorrhea or chlamydia (AOR = 0.53; 95% CI = 0.31, 0.87). Pathway analyses suggested CM acted above and beyond peer education; reduction in gonorrhea or chlamydia was attributable to CM.
Conclusions. CM is a central part of HIV prevention programming among FSWs, empowering them to better negotiate condom use and access services, as well as address other concerns in their lives.
HIV prevention strategies with female sex workers (FSWs) have traditionally relied on individual behavior change, involving peer educators, condom promotion, and provision of sexual health services.1,2 Over the past decade, there has been a growing recognition that HIV epidemics are “socially and culturally produced,”3 and that psychosocial and community-level processes underlie an individual’s ability to adopt safer sexual behaviors. This has influenced approaches to HIV prevention, with more attention being paid to structural and social factors (such as violence, stigma, and poverty) that shape individual-level risk behaviors (e.g., condom use) and interventions that are targeted toward contextual factors in the HIV risk environment.4–8
Among FSW populations, community mobilization (CM) has been endorsed as one of the structural interventions that improve the risk environment, with it's effectiveness in addressing health and social issues of poor and marginalized populations largely explained through “empowerment.”9–12 Such programs have been recognized in the Joint United Nations Programme on HIV/AIDS investment framework, which includes CM as a critical enabler to core programs.13 In contrast to peer education, which usually involves peers meeting FSWs in the field, talking to them about the program, about difficulties they are facing in their lives, about the importance of condom use, and about the clinics and drop-in centers and other program activities, CM involves bringing together FSWs of various typologies who are scattered and hidden across rural areas and towns through mobilization, participation, and empowerment processes, to provide them with the space and the opportunity to act together, to fight injustices against them, and to campaign for their rights. Thus, whereas peer education can be a fairly “top down” approach, CM is designed to be an inclusive process that is initiated and sustained by the community to bring about the changes they desire (e.g., reduction in violence) through the process of empowerment. Empowerment can be defined as “the processes by which those who have been denied the ability to make choices (disempowered) acquire such an ability.”14(p437) Most empowerment approaches recognize a dynamic interplay between gaining internal skills and overcoming external barriers, often drawing upon a conceptual framework that distinguishes “power within” (for example, self-confidence or critical thinking skills that contribute to individual agency), “power to” (for example, the ability to make individual decisions that determine and demonstrate such agency), and “power with” (communal decisions, such as group solidarity or collective action, which acknowledge that positive change may often be effected by individuals working together, rather than alone).9,15,16 In the context of sex work, the principles of social solidarity and CM seek to shift the burden of safer sex negotiation from being solely that of an individual FSW to a concept that is collectively shared and owned by the SW community, by acknowledging the dynamics and inequalities between a FSW and her client and the owners, pimps, and madams of sex establishments where sex workers work.17
The Sonagachi program in Kolkata in east India provided one of the first examples of a rights-based HIV prevention program for FSWs, focusing on the mobilization and empowerment of brothel-based sex workers, as well as engagement with power structures,12,18–20 with data suggesting that HIV prevalence remained much lower in this setting compared with FSWs elsewhere in India.19 More recently, a growing body of evidence has suggested that organizing FSWs into support groups and community-based organizations can help the community to collectively challenge factors contributing to their vulnerability, such as stigma, discrimination, poverty, housing instability, violence, and harassment.21–31 However, although studies have reported strong associations between CM and collective power, uptake of sexually transmitted infection (STI) services, and consistent condom use with clients,11,17,32–35 there remains a paucity of data examining the impact of CM on biological (HIV or STI) outcomes.
India has an estimated 2.4 million people living with HIV.36 Karnataka state in south India has the fourth highest HIV prevalence in the country. HIV is predominantly transmitted heterosexually, with the prevalence of HIV previously exceeding 1% in the general population, and a prevalence of more than 30% among FSWs in some districts.37,38 Before 2003, there was little HIV prevention programming in Karnataka. The Karnataka Health Promotion Trust was established in 2003 as part of the India Avahan initiative, funded by the Bill & Melinda Gates foundation.39,40 The program aimed to slow the HIV epidemic by rapidly scaling up targeted HIV prevention programs, reaching more than 60 000 FSWs and 20 000 men who have sex with men and transgenders in 20 of the 30 districts in the state.
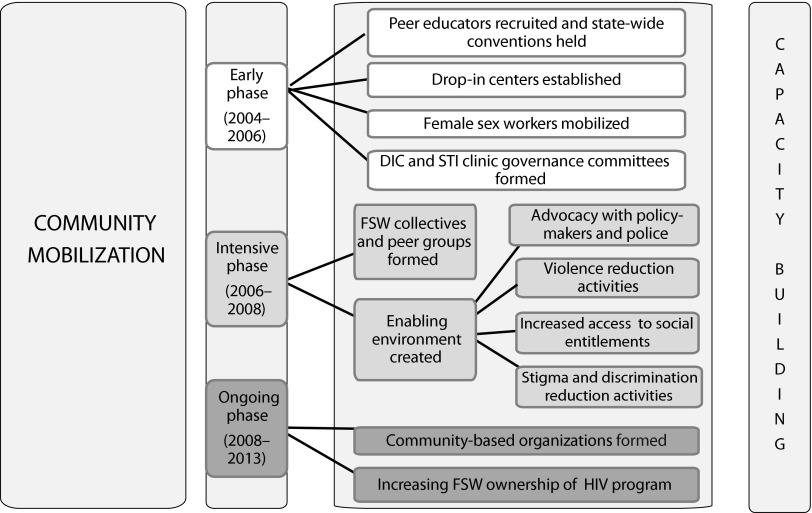
Community mobilization and the empowerment of FSWs formed a core part of HIV prevention programming in Karnataka (Figure 1).21,29–31 The process of mobilization and empowerment was gradual, with later phases of the program building on previous phases, and each activity contributing to the mobilization of SWs. For example, in the early phase of the project, peer educators were recruited from the FSW community. FSWs were brought together, and safe drop-in centers were created to respond to FSWs’ need for somewhere safe to rest, dress up, and meet friends. The program organized events and meetings for FSWs together with clinical services in these drop-in centers. These services included the provision of the “gray pack,” which was supplied every 3 to 6 months for the periodic presumptive treatment of gonorrhea and Chlamydia (containing 1 g azithromycin and 400 mg cefixime). These drop-in centers, in turn, helped attract more SWs, which resulted in the centers becoming a space where FSWs could meet each other and share their experiences, which helped create a sense of solidarity. The program then worked to support and develop critical thinking among the FSW community, providing a forum where FSWs could discuss the difficulties in their lives and reflect on how they could work together to address the challenges they faced.
FIGURE 1—
Community mobilization activities of Karnataka Health Promotion Trust: Karnataka, India, 2003–2014.
Note. DIC = drop-in center; FSW = female sex worker; STI = sexually transmitted infection.
In the intensive phases of the program (2006–2008), FSWs built on their sense of solidarity and started to undertake collective action, working with policymakers, the police, government officials, human rights lawyers, and the media to address issues of stigma, discrimination, violence, and social inequity.21,31 This, in turn, gave birth to collectivization and the formation of community-based institutions, such as peer groups or collectives. In the maintenance phase (2008–2013), FSW community-based organizations were formed to enable the process of handing over ownership of the Avahan program to FSWs and to the state government by 2013, which is now complete.41
A detailed analysis of the impact of Avahan on HIV and risk behavior has been conducted, and suggests that the combination HIV program had a significant impact on HIV prevalence in Karnataka.42 However, a key policy debate, especially given current resource constraints, has been whether it is necessary to include CM, collectivization, and empowerment components in FSW HIV prevention programming, which can be costly and time-consuming. Therefore, we examined the impact of CM on HIV and STI prevalence, HIV risk behaviors, and collective and individual power among FSWs in Karnataka, using secondary analyses of data from 2 rounds of behavioral–biological surveys conducted with FSWs in 2008 and 2011.
METHODS
We conducted 2 rounds of district-level, cross-sectional integrated behavioral–biological assessment (IBBA) surveys37,43 with FSWs in 4 districts in Karnataka (Belgaum, Bellary, Shimoga, and Bangalore), chosen purposively to reflect Karnataka’s different sociocultural regions and the size of the FSW population. Mapping and enumeration of FSWs in these districts estimated that approximately 34 250 women sell sex across the 4 districts (Bangalore: 19 662; Bellary: 4286; Shimoga: 1882; Belgaum: 8429). Intervention programs were initiated in each district between April 2004 and October 2005, with follow-up cross-sectional surveys conducted in 2008 and in 2011. A probability-based sampling method was used. We used conventional cluster sampling for FSWs who sold sex at home, or in brothels, lodges, and dabhas (road-side drinking establishments), where the population of FSWs was relatively stable. We used conventional time-location cluster sampling for street-based FSWs. We used the same sampling technique for the baseline and follow-up surveys. Sample size calculations were designed to detect a 10% to 15% increase in condom use with 90% power and α error of 5%, assuming a baseline value for consistent condom use with commercial clients of 50%.
We estimated that 385 participants (rounded to 400) were required for each cross-sectional survey round in Bellary, Belgaum, and Shimoga. In Bangalore Urban, we used a similar approach, but 800 participants (comprising 400 street-based FSWs and 400 non–street-based [home-, brothel- and phone-based] FSWs) were sampled for each round.
Behavioral Questionnaire and Laboratory Methods
We used a structured behavioral questionnaire to collect data on FSWs’ sexual behavior and intervention exposure, as previously described.26 All interviews were conducted in the local language (Kannada) by trained interviewers. To ensure confidentiality, we did not collect identifying information, and data could not be linked between rounds. Blood samples were taken to test for HIV, herpes simplex virus 2 (HSV-2), and syphilis, and urine samples were collected to test for chlamydial infection and gonorrhea, as previously described.42 In brief, HIV serological testing used a synthetic peptide enzyme immunoassay (Detect HIV 1/2 system; BioChem ImmunoSystems, Montreal, Quebec), and positive tests were confirmed using a recombinant antigen enzyme immunoassay (Genedia HIV 1/2 ELISA 3.0; Green Cross Life Science Corporation, Yongin, South Korea). Serological testing for HSV-2 used an immunoglobulin-G enzyme immunoassay (Kalon Biological Ltd., Aldershot, United Kingdom). Serological testing for syphilis used the rapid plasma reagin (RPR) method (Span Diagnostics, Sachin, India), and if positive, syphilis was confirmed by the Treponema pallidum hemagluttination assay (TPHA) test (Omega Diagnostics Ltd., Alloa, Scotland). Reactive syphilis infection was defined as being RPR positive (any titer) and TPHA positive. High-titer syphilis was defined as having an RPR titer of 1:8 or greater and being TPHA positive. Urine samples were tested by polymerase chain reaction for gonorrhea and chlamydia using the Roche Amplicor system (Roche Molecular Diagnostics, Pleasanton, CA) on samples from Shimoga, and the Gen-Probe Aptima assay (Gen-Probe Inc, San Diego, CA) on samples from Bellary, Belgaum, and Bangalore Urban.
All positive specimens and 10% of negative specimens were sent to the National AIDS Research Institute in Pune, India, for quality assurance. Because of budget constraints, chlamydia and gonorrhea were tested for in 2008 only, and HSV-2 was tested in 2011 only in Belgaum and Bellary districts.
Statistical Analyses
Data were double entered using the Census and Survey Processing System (CSPro; https://www.census.gov/population/international/software/cspro). The district IBBA data were merged to form 1 database to allow analysis across districts and rounds.
For the purposes of our analysis, and following discussions with project staff, we used the following as proxy measures to define exposure to CM activities: “high” if a woman reported being a member of a FSW peer group or FSW collective; “medium” if she had ever attended a drop-in center or a nongovernmental organization (NGO) meeting; and “low” if she had not done any of the preceding.
A range of outcomes were considered in our analysis. HIV-related outcomes that were assessed included HIV or STI service use, condom use at last sex with occasional and repeat clients and regular partners, and HIV and STI prevalence. Here, “occasional” clients were defined as “clients who have come to you only once or a few times, but you do not remember their faces or do not know them,” and “repeat” clients were defined as “clients you recognize well, who have come to you repeatedly, and you know them.” Building upon theories of the process of empowerment, we explored whether CM had affected measures of collective and individual power. Measures of collective power (power with) were explored using questions about feeling a sense of unity: “I feel a strong sense of unity with FSWs I do not know”; negotiating on behalf of other FSWs, “In the last 1 year, have you negotiated with or stood up against a powerbroker to help a fellow FSW?”; and attendance at a public event to campaign for FSW rights, “In the last 6 months, have you attended any public events, such as a rally or a gathering of sex workers, where you could be identified as a sex worker?”11 A measure of individual power (power to) was developed by looking at whether respondents had answered “no” to “In the past 1 month, was there a time when you wanted to use a condom during sexual intercourse but did not use it?” or “In the past 1 month, was there a time when you wanted to use a condom during sexual intercourse with a client but did not use it?”
All statistical analyses were performed using the survey data analysis techniques in STATA (version 12.0; StataCorp, College Station, TX). Appropriate weights were used to account for the differential recruitment of FSWs by typology within districts, differential nonresponse rates, and differential probabilities of FSW selection across districts. We used odds ratios (ORs) as the measure of association, and the Wald χ2 test as the statistical test. We used logistic regression analyses to examine associations between exposure to CM and the various outcome variables. In the multivariate models, potential sociodemographic and sex work characteristic confounders (data available as a supplement to the online version of this article at http://www.ajph.org) were added to the model using a stepwise approach. District, duration in sex work, sex work typology (place where soliciting clients or place where FSWs had sex with clients), relationship status (marital status or regular partner), and socioeconomic status (literacy or additional income to sex work) were added a priori. (When there was a choice of 2 variables, the variable that caused the greatest shift in the OR was selected.) In addition, other sociodemographic and sex work variables that caused the OR of the independent variable to change by 10% or more were also included in the final model. The adjusted Wald test was used to test for effect modification for the following sociodemographic variables: age, duration in sex work, place where soliciting clients, place where FSWs had sex with clients, charge per sex act, and regular partner.
Pathway Analyses
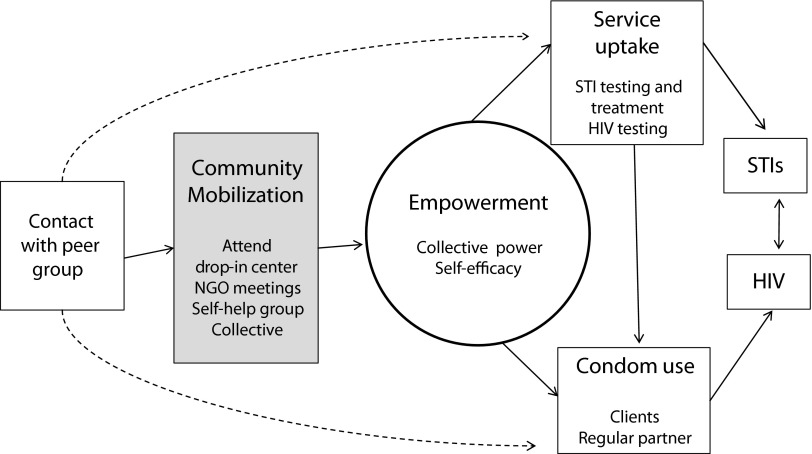
Pathway analysis was used to explore the hierarchical relationships between different protective factors for HIV infection among FSWs. To inform this analysis, we developed a conceptual framework (Figure 2) to describe the possible pathways through which CM could be having an effect on HIV risk. We used this analysis to obtain estimates of the degree to which CM might be having an impact on key HIV-related outcomes, over and above peer education activities alone.44 For this, we first used logistic regression to examine associations between peer education and the outcome variables using data from 2011. We then added CM to the adjusted multivariate model, to assess whether, by adjusting for CM, the adjusted ORs substantially shifted closer to 1.0 (which would suggest that CM was acting on the pathway between peer education and the outcome variable).44 When peer education was significantly associated with an outcome variable, we calculated the proportion difference in the adjusted ORs between peer education and the outcome variable, and peer education and the outcome variable, adjusting for CM ([OR adjusted for confounders − OR adjusted for confounders and CM]/OR adjusted for confounders).
FIGURE 2—
Conceptual hierarchical framework of protective factors for HIV and sexually transmitted infection among female sex workers: Karnataka State, India.
Note. NGO = nongovernmental organization; STI = sexually transmitted infection.
RESULTS
A total of 3909 FSWs participated in the 2 survey rounds (1975 in 2008; 1934 in 2011). Sociodemographic characteristic details are shown as data available as a supplement to the online version of this article at http://www.ajph.org. Mean age of participants was 32.5 years (range = 18–57 years). Most were illiterate (64.0%), and were either married (36.0%) or separated, divorced, deserted, or widowed (46.1%); 9.5% were devadasi. (The devadasi tradition involves a ritual in which adolescent girls are dedicated to gods and goddesses and subsequently inducted into sex work, and is the most common form of traditional sex work in northern Karnataka.45)
Most women had 1 or more children (91.2%) and an additional source of income to sex work (64.5%). Participants were a mean age of 15.6 years (range = 10–34 years) at sexual debut, and had been selling sex on average for 6.9 years (range = 0–38 years). Most women solicited clients on the street or in public places (43.0%), with the remainder soliciting clients at home (27.9%), by phone (21.6%), or in brothels (7.5%). On average, women sold sex to 2.3 clients per day (range = 1–25) and charged 330.9 rupees (US $6.06) per sex act (range = 0–3000 rupees).
Exposure to the HIV Prevention Program and Community Mobilization
By the 2008 survey, program coverage of study participants was high; 95.3% of FSWs reported meeting a peer educator, and 89.8% reported seeing a condom demonstration. In addition, CM efforts had started to take effect; 82.0% of participants reported attending an NGO meeting, and 73.5% reported that they had visited a project drop-in center. One half of participants (50.1%) were members of a collective or a peer group. When we categorized participants according to their level of exposure to CM activities, approximately 50% had high exposure (member of a collective or peer group), 40% had medium exposure (attended an NGO meeting or project drop-in center), and 10% of women had low exposure (none of the preceding actions took place; data available as a supplement to the online version of this article at http://www.ajph.org).
Between 2008 and 2011, there were relatively small changes in FSWs’ access to or use of different services (met a peer educator [2008: 95.3% vs 2011: 97.5%]; saw a condom demonstration (2008: 89.8% vs 2011: 92.8%); attended an NGO meeting [2008: 82.0% vs 2011: 87.7%]; visited a drop-in center [2008: 73.5% vs 2011: 61.0%]; was a member of a collective or peer group [2008: 50.1% vs 2011: 52.0%]. In combination, the distribution of exposure to CM activities among FSWs was relatively similar between 2008 and 2011 (low: 10.6% vs 7.7%; medium: 39.3% vs 38.9%; high: 50.1% vs 53.4%; data available as a supplement to the online version of this article at http://www.ajph.org).
Community Mobilization and Collective and Individual Power
We next examined associations between levels of exposure to CM activities and different measures of collective (power with) and individual (power to) power. At the 2011 survey, in both univariate and adjusted analyses, women who were highly exposed to CM activities were significantly more likely than women with low exposure to report all measures of collective and individual power (Table 1). Similarly, women with medium exposure to CM activities were significantly more likely than women with low exposure to report all measures of power, although the strength of the associations were not as strong as those with high exposure (Table 1).
TABLE 1—
Collective Power, Individual Efficacy, and Exposure to Community Mobilization Activities: Pooled Data From 4 Districts, Karnataka, India; Integrated Behavioral-Biological Assessment Data; 2011
| Exposure |
Wald Test Crude OR (95% CI) |
Wald Test Adjusted ORa (95% CI) |
||||||
| Characteristic | No/Low (n = 149), % | Medium (n = 764), % | High (n = 1021), % | Wald Test P | No/Low vs Medium Exposure | No/Low vs High Exposure | No/Low vs Medium Exposure | No/Low vs High Exposure |
| I feel a strong sense of unity with sex workers I do not know | 78.5 | 92.5 | 95.0 | < .001 | 3.38** (1.97, 5.81) | 5.21** (3.06, 8.88) | 3.11** (1.83, 5.29) | 3.99** (2.34, 6.80) |
| In last 6 mo attended rally or other public event where could be identified as FSW | 1.2 | 6.5 | 19.1 | < .001 | 5.63* (1.31, 24.19) | 19.00** (4.58, 79.00) | 5.17* (1.17, 22.87) | 13.90** (3.26, 59.22) |
| In last 1 y have stood up or negotiated against someone to help fellow sex workers | 2.6 | 8.0 | 20.8 | < .001 | 3.22* (1.08, 9.61) | 9.79*** (3.32, 28.86) | 3.17* (1.01, 9.96) | 7.52** (2.43, 23.25) |
| In past month had time when wanted to use a condom but did not (self-efficacy)b | 49.0 | 51.8 | 65.3 | < .001 | 1.12 (0.73, 1.71) | 1.96*** (1.27, 3.03) | 1.77*** (1.13, 2.76) | 2.45** (1.49, 4.03) |
| Home-based | 53.7 | 49.9 | 62.8 | < .001 | 0.86 (0.52, 1.43) | 1.46 (0.86, 2.47) | 1.32 (0.76, 2.31) | 1.59 (0.86, 2.91) |
| Brothel-based | 49.5 | 55.0 | 67.2 | .048 | 1.25 (0.55, 2.81) | 2.09 (0.92, 4.78) | 1.81 (0.74, 4.41) | 2.66* (1.06, 6.66) |
| Street-based | 22.4 | 57.6 | 72.2 | .001 | 4.71*** (1.53, 14.52) | 9.01** (3.24, 25.06) | 6.82*** (1.93, 24.04) | 17.26** (5.31, 56.13) |
| In past month had time when wanted to use a condom with a client but did not (self-efficacy)b | 78.9 | 86.4 | 89.1 | .002 | 1.69* (1.05, 2.72) | 2.18*** (1.33, 3.56) | 0.54* (0.36, 0.89) | 0.42*** (0.25, 0.70) |
| Home-based | 85.1 | 86.6 | 89.8 | .2 | 1.13 (0.62, 2.05) | 1.53 (0.80, 2.94) | 1.28 (0.69, 2.38) | 1.67 (0.82, 3.38) |
| Brothel-based | 77.1 | 87.4 | 89.7 | .14 | 2.06 (0.76, 5.60) | 2.57* (1.06, 6.24) | 2.01 (0.69, 5.85) | 2.42 (0.93, 6.27) |
| Street-based | 52.3 | 82.4 | 84.9 | .004 | 4.25* (1.19, 15.20) | 5.12*** (1.94, 13.54) | 04.08* (1.09, 15.31) | 4.88*** (1.84, 12.93) |
Note. CI = confidence interval; FSW = female sex worker; OR = odds ratio.
Adjusted for district, duration sex work, sex work typology, literacy, marital status, previously sold sex in Mumbai, and have repeat clients.
Self-efficacy defined as answering “no” to “In the past 1 month, was there a time when you wanted to use a condom during sexual intercourse but did not use it?” or “In the past 1 month, was there a time when you wanted to use a condom during sexual intercourse with a client but did not use it?”
*P < .05; **P < .01; ***P < .001.
For measures of individual power, the place where FSWs had sex with their clients was an effect modifier, with exposure to CM activities being most significantly associated with individual power among women who had sex with their clients on the street compared with those who had sex with their clients in brothels or at home (Table 1). Similar associations were seen in 2011 as those in 2008, for “feeling a sense of unity” and “negotiating on behalf of other FSWs,” but not for other measures of collective and individual power (data available as a supplement to the online version of this article at http://www.ajph.org).
Community Mobilization and HIV or STI Service Use and Condom Use
There were strong associations between exposures to CM activities and uptake of HIV or STI services (2011), with women with low exposure being significantly less likely to have accessed HIV or STI services or to have received a gray pack than women with medium or high exposure (Table 2). Reported condom use at last sex with casual clients, regular clients, and with regular partners (2011), each increased with the level of exposure to CM activities.
TABLE 2—
HIV/STI Service Uptake, Condom Use at Last Sex, HIV/STI Prevalence, and Exposure to Community Mobilization Activities: Pooled Data From 4 Districts, Karnataka, India; Integrated Behavioral-Biological Assessment Data 2011; and STI Data 2008
| Exposure |
Wald Test Crude OR (95% CI) |
Wald Test Adjusted ORa (95% CI) |
||||||
| Characteristic | No/Low (n = 149), % | Medium (n = 764), % | High (n = 1021), % | Wald Test P | No/Low vs Medium Exposure | No/Low vs High Exposure | No/Low vs Medium Exposure | No/Low vs High Exposure |
| Visited STI clinic past 6 mo | 29.9 | 84.2 | 90.9 | < .001 | 12.45*** (8.26, 18.79) | 23.27*** (14.92, 36.29) | 12.22*** (7.89, 18.94) | 24.53*** (15.33, 39.27) |
| Received “gray pack”b past 6 mo | 14.7 | 43.0 | 56.7 | < .001 | 4.37*** (2.70, 7.08) | 7.67*** (4.82, 12.21) | 4.17*** (2.55, 6.81) | 6.86*** (4.25, 11.10) |
| Ever taken an HIV test | 66.5 | 94.6 | 98.1 | < .001 | 8.82*** (5.52, 14.10) | 26.31*** (14.23, 48.65) | 8.15*** (4.78, 13.88) | 25.13*** (13.07, 48.34) |
| Condom use last sex act occasional clientsc (n = 1651) | 87.2 | 95.2 | 96.7 | <.001 | 2.91** (1.56, 5.11) | 4.28*** (2.22, 8.25) | 2.28* (1.11, 4.69) | 4.74*** (2.17, 10.37) |
| Condom use last sex act repeat clientsd (n = 1751) | 79.9 | 90.8 | 94.0 | < .001 | 2.47** (1.35, 4.53) | 3.95*** (2.13, 7.32) | 2.63** (1.40, 4.93) | 4.29*** (2.24, 8.20) |
| Condom use last sex act regular partner (n = 1322) | 27.6 | 29.3 | 48.0 | < .001 | 1.08 (0.66, 1.78) | 2.42** (1.46, 4.01) | 1.67 (0.87, 3.17) | 2.80** (1.43, 5.45) |
| HIV-1 infection | 9.5 | 10.9 | 10.9 | .87 | 1.17 (0.60, 2.27) | 1.18 (0.63, 2.20) | 1.26 (0.63, 2.52) | 1.07 (0.54, 2.14) |
| Reactive syphilis | 5.4 | 5.4 | 3.8 | .46 | 1.00 (0.36, 2.81) | 0.69 (0.24, 1.96) | 1.29 (0.47, 3.55) | 0.63 (0.22, 1.78) |
| High-titer syphilis | 2.4 | 2.3 | 1.2 | .34 | 0.98 (0.26, 3.69) | 0.50 (0.13, 1.98) | 1.24 (0.34, 4.55) | 0.42 (0.10, 1.72) |
| HSV-2e | 68.9 | 74.0 | 59.9 | .004 | 1.28 (0.70, 2.35) | 0.67 (0.37, 1.21) | 0.93 (0.44, 1.93) | 0.49 (0.23, 1.02) |
| Chlamydiaf | 14.0 | 6.3 | 3.9 | < .001 | 0.41*** (0.25, 0.67) | 0.25*** (0.15, 0.41) | 0.76 (0.45, 1.27) | 0.64 (0.37, 1.09) |
| Gonorrheaf | 6.6 | 3.2 | 1.2 | < .001 | 0.46 (0.21, 1.02) | 0.17*** (0.07, 0.40) | 0.95 (0.41, 2.22) | 0.39 (0.13, 1.19) |
| Chlamydia/gonorrheaf | 17.6 | 8.4 | 4.3 | < .001 | 0.43*** (0.27, 0.67) | 0.21*** (0.13, 0.34) | 0.78 (0.49, 1.25) | 0.53* (0.31, 0.87) |
Note. CI = confidence interval; HSV-2 = herpes simplex virus 2; OR = odds ratio; STI = sexually transmitted infection.
Adjusted for district, duration sex work, sex work typology, literacy, marital status, previously sold sex in Mumbai, and have repeat clients.
“Gray pack” consists of 1 g azithromycin and 400 mg cefixime for periodic presumptive treatment of gonorrhea and chlamydia.
Occasional client defined as “client who has come to you only once or a few times but you do not remember their face or do not know them.”
Repeat client defined as “client you recognize well, who has come to you repeatedly and you know them.”
HSV-2 data available for Belgaum and Bellary only (n = 803).
Chlamydia and gonorrhea data presented for 2008 as data not collected in 2011. Models adjusted for localite (born in district), additional source of income to sex work, regular partner, duration in sex work, sex work typology (where solicit clients), and district.
*P < .05; **P < .01; ***P < .001.
In univariate and adjusted analyses, women with low exposure to CM activities were significantly less likely to report condom use at last sex with occasional and regular clients compared with women with medium or high exposure. They were also significantly less likely to report condom use at last sex with their regular partner compared with women with high exposure (this association was not significant for women with medium exposure; Table 2). Similar results were also seen in 2008 (data available as a supplement to the online version of this article at http://www.ajph.org).
Community Mobilization and Prevalence of HIV and STI
At the district level, there were no clear trends between exposure to CM and prevalence of HIV or STI (data available as a supplement to the online version of this article at http://www.ajph.org). However, when we pooled the data for the 4 districts, by the 2011 survey round, there were no significant associations between different levels of CM exposure and either HIV or syphilis prevalence, but we did find a stepwise reduction in prevalence of chlamydia or gonorrhea with increasing levels of exposure to CM activities, with highly exposed women being significantly less likely than those with low exposure to be infected with chlamydia or gonorrhea (Table 2). In addition, women who were highly exposed to CM activities were less likely than those with low exposure to be HSV-2 positive (Table 2).
Pathway Analysis
Having observed strong associations between CM and various measures of collective and individual power, HIV and STI service uptake, condom use with clients and regular partners, and gonorrhoea and chlamydia prevalence, we next examined associations between peer education and the outcome variables (Table 3). In both univariate and multivariate analyses, meeting a peer educator was strongly associated with the various measures of collective and individual power, HIV or STI service uptake, and condom use at last sex with clients and regular partner, but there was no evidence of an association between meeting a peer educator and HIV or STI prevalence. For all outcome variables that were associated with meeting a peer educator, adjusting for CM caused the OR to substantially shift closer to 1.0, with a proportional reduction in the adjusted OR of between 25% and 78% (Table 3).
TABLE 3—
Peer Education and Power, Risk, and HIV/STI Prevalence, Adjusted for Sociodemographic Characteristics and Community Mobilization: Pooled Data From 4 Districts, Karnataka, India; Integrated Behavioral-Biological Assessment Data 2011 and STI Data 2008
| Met a Peer Educator, % |
Adjusted OR (95% CI) |
||||||
| Variable | No (n = 48) | Yes (n = 1886) | Wald Test P | Crude OR, (95% CI) | Sociodemographic Confoundersa | Sociodemographic Confounders and CMb | Proportional Difference in ORc (%) |
| Power | |||||||
| Feel a sense of unity with other FSWs | 60.8 | 93.5 | < .001 | 9.32*** (5.02, 17.33) | 8.14*** (4.22, 15.71) | 4.38*** (2.01, 9.56) | 46.2 |
| Negotiated on behalf of other FSWs | 0 | 21.5 | .005 | . . . | . . . | . . . | . . . |
| Attended a public event to campaign for the rights of FSWs | 0 | 13.0 | .035 | . . . | . . . | . . . | . . . |
| In past month had time when wanted to use a condom but did not (self-efficacy)d | 45.6 | 58.9 | .16 | 1.71 (0.80, 3.64) | 3.80** (1.75, 8.25) | 2.42* (1.04, 5.65) | 36.3 |
| In past month had time when wanted to use a condom with a client but did not (self-efficacy)d | 66.0 | 87.7 | < .001 | 3.69*** (1.84, 7.38) | 4.66*** (2.29, 9.46) | 3.48** (1.41, 8.60) | 25.3 |
| HIV/STI service uptake | |||||||
| Visited project STI clinic past 6 mo | 0 | 85.5 | < .001 | . . . | . . . | . . . | . . . |
| Ever taken an HIV test | 38.7 | 95.6 | < .001 | 34.68*** (16.54, 72.72) | 28.81*** (13.48, 61.57) | 6.32*** (2.67, 15.00) | 78.1 |
| Condom use last sex | |||||||
| Occasional cliente | 73.1 | 95.9 | < .001 | 8.67*** (4.05, 18.56) | 10.96*** (5.00, 24.01) | 6.78* (1.96, 23.44) | 38.1 |
| Repeat clientf | 72.4 | 92.2 | < .001 | 4.50*** (2.07, 9.78) | 5.58*** (2.49, 12.48) | 2.40 (0.80, 7.24) | 57.0 |
| Regular partner | 15.5 | 39.7 | .001 | 3.59* (1.60, 8.08) | 7.41*** (2.81, 19.56) | 5.50* (1.74, 17.35) | 25.8 |
| HIV/STI prevalence | |||||||
| HIV | 10.9 | 10.8 | .98 | 0.99 (0.41, 2.42) | 0.95 (0.33, 2.76) | 0.82 (0.24, 2.75) | |
| Active syphilis | 7.3 | 4.5 | .38 | 0.60 (0.19, 1.92) | 0.69 (0.21, 2.20) | 0.70 (0.21, 2.37) | |
| High-titer syphilis | 2.1 | 1.7 | .85 | 0.83 (0.12, 5.56) | 1.20 (0.17, 8.68) | 2.06 (0.18, 24.03) | |
| Gonorrheag | 7.2 | 2.3 | .001 | 0.30** (0.14, 0.65) | 0.56 (0.25, 1.24) | 0.68 (0.21, 2.22) | |
| Chlamydiag | 15.9 | 5.4 | < .001 | 0.30*** (0.18, 0.51) | 0.78 (0.46, 1.33) | 1.15 (0.64, 2.07) | |
| Gonorrhea/chlamydiag | 18.5 | 6.8 | < .001 | 0.32*** (0.19, 0.53) | 0.75 (0.45, 1.25) | 1.18 (0.67, 2.08) | |
Note. CI = confidence interval; CM = community mobilization; FSW = female sex worker; HSV-2 = herpes simplex virus 2; OR = odds ratio; STI = sexually transmitted infection.
Models adjusted for sociodemographic confounders: duration in sex work, sex work typology, district, marital status, localite (born in district), and repeat clients.
Models adjusted for sociodemographic confounders and community mobilization.
Proportional difference in OR calculated for outcome variables significantly associated with peer education in multivariate analyses: ([OR adjusted for confounders − OR adjusted for confounders and community moblization]/OR adjusted for confounders).
Self-efficacy defined as saying “no” to: “In the past month, was there a time when you wanted to use a condom with a client but did not use it.”
Occasional client defined as “client who has come to you only once or a few times but you do not remember their face or do not know them.”
Repeat client defined as “client you recognize well, who has come to you repeatedly and you know them.”
Data presented from 2008. Models adjusted for localite (born in district), additional source of income to sex work, regular partner, duration in sex work, sex work typology (where solicit clients), and district.
*P < .05; **P < .01; ***P < .001.
DISCUSSION
Our findings suggest that CM of FSWs is an important part of HIV prevention programming because it is strongly associated with various measures of collective (power with) and individual (power to) FSW empowerment, reductions in HIV and STI risk behaviors, and reduced prevalence of STI. In addition, pathway analyses suggest that CM is likely acting over and above the effects of peer education alone, and that the lower prevalence of gonorrhea or chlamydia among women with increased exposure to CM activities might be entirely attributable to the CM component of this program. Taken together, this study adds to a growing body of evidence suggesting that the empowerment and CM of FSWs can have important and far-reaching benefits in terms of reducing HIV risk and vulnerability.11,17–20,26,29,31,32,34,42,46,47
Our study adds to the existing literature by providing new evidence of the potential impact of CM on biological measures of HIV and STI infection. This is important because few studies have explored this previously.26,35 Although there were limitations to the measures of exposure to CM that we were able to use, the strength of this analysis was in its ability to explore the relationship between exposure to CM and biological markers of infection. These have additional value because they are not subject to the same reporting biases as self-reported risk behaviors (such as condom use and service use),48,49 or the problems associated with using self-reported STI symptoms as an indicator of actual STI infection.50,51 The anonymous cross-sectional design of the IBBA surveys did not allow us to measure incident HIV and STI infections. However, because of the periodic presumptive treatment of women by the intervention program with antibiotics (1 g azithromycin and 400 mg cefiximine) to treat gonorrhea and chlamydia infection, as well as the fact that these 2 infections are often self-limiting in nature,52,53 of the 5 STIs we measured (HIV, HSV-2, syphilis, gonorrhea, and chlamydia), gonorrhea and chlamydia probably provide the closest proxy to recent infection. The lower prevalence of gonorrhea and chlamydia among those with high exposure to CM activities corresponded with the high levels of reported condom use and HIV and STI service use among those in the high exposed group. The lack of association between exposure to CM activities and HIV is not surprising because we measured prevalent and not incident infection; therefore, women could have acquired HIV before being exposed to the HIV prevention program. However, this finding did suggest that women who had HIV continued to engage in collectivization and peer group activities, and as such, were more likely to know about the availability of antiretroviral therapy services compared with HIV-positive women with low exposure to CM activities.
A key aim of the CM activities within the India Avahan initiative has been to empower FSWs; to reduce the levels of violence, harassment, stigma, and discrimination against them; and to enable women to take more control over their lives and sexual health.11,20–22,27,29–31,35,54 We previously reported reductions in violence among this population over time.21 In this study, we found strong associations between high levels of CM and various measures of collective and individual FSW empowerment, with exposure to CM activities being most significantly associated with individual power among women who had sex with their clients on the street compared with those who had sex with their clients in brothels or at home. Street-based sex workers tend to be the most vulnerable and disempowered, and therefore, might have the largest potential for change or empowerment. We also found strong associations between high levels of CM and condom use at last sex both with clients as well as with regular partners. The impact on condom use with regular partners is important, because FSWs often find it more challenging to negotiate condom use with their regular partners than with clients, as issues of intimacy and trust become increasingly important. Although the measures of FSW empowerment were relatively crude, and empowerment and condom use might be subject to reporting biases, these results were nevertheless very encouraging and illustrate the breadth of potential effects of CM.
Study Limitations
There are several challenges to conducting a study of this type, which have limited the analysis. FSW empowerment and CM is a complex and integrated process, the effects of which might be felt at an individual, group, or district level, and the process of trying to quantify FSWs’ level of empowerment and engagement was challenging, especially because the behavioral–biological surveys we used were mainly designed to capture changes in risk behaviors and HIV and STI prevalence over time, rather than to evaluate the specific roles of CM and empowerment. As such, they did not contain detailed questions about exposure to the various components of CM, and therefore, we had to use information about women’s exposure to different components of the program as proxy measures to ascertain levels of CM exposure. Similarly, FSW empowerment is a complex construct, and our analysis would have been strengthened if there had been specific questions to measure collective and individual power, economic empowerment, and access to structural components of the program, such as the legal empowerment and social entitlements workshops. Instead, we used established theories about the process of empowerment to construct proxy measures of “power with” and “power to” other actions.
These limitations might have influenced our findings in several ways. The relatively crude nature of our measures of exposure could have resulted in us classifying women as being exposed to CM or empowered, who were not, or vice versa. Similarly, because our measure of CM exposure was at the individual level, even women who were not directly exposed to CM activities might have benefited indirectly from other women’s engagement with CM; for example, they could have still benefited from CM activities such as the violence intervention, even if they were not directly involved in CM. Our approach to constructing the measures of CM and empowerment was done in consultation with project partners, and decided upon a priori before we conducted our analysis. If anything, however, we suspect that the preceding factors and the potential associated misclassification would have led to a dilution of association.
The other important limitation in our analysis was the cross-sectional nature of the data used and the lack of a true control group. Although we had 2 rounds of data from FSWs, the data were not longitudinal. We could not compare outcomes from the same FSWs over time, but instead had to analyze each round of cross-sectional data separately. In such cases, it was not possible to ascertain the direction of associations or to make causal inferences from the results. The lack of a control population was the result of the nature of the Avahan program, which prioritized the rapid scale-up of HIV prevention programming in all districts in response to an escalating HIV epidemic. This meant that there were no IBBA control districts to act as comparison groups,42 and instead, we had to create a control comparison group by selecting FSWs from within the same IBBA districts who reported low exposure to a variety of CM. Sixty-nine percent of women who were categorized as low exposure had met with a peer educator who were trained in promoting and relaying CM messages together with condom promotion and health-seeking behaviors. Thus, the results presented in this study might have underestimated the association between exposure to CM activities and the various outcome measures. Alternatively, women who choose to participate in FSW collectives and FSW peer groups might be different in some way that also affects their risk profiles, compared to those who are not members, and this could overestimate the associations seen in this study.
Conclusions
The data from this study suggest that CM of FSWs may be associated with increased empowerment, increased uptake of HIV or STI services, increased condom use with clients and regular partners, and reduced chlamydia or gonorrhea prevalence among FSWs. These findings suggest that even in times of constrained budgets and limited resources, CM should not be seen as a luxury “add-on” to the traditional biomedical HIV prevention model. Rather, our findings suggest that CM has formed an important and integral part of the success of the Avahan HIV prevention program. The holistic approach taken addresses key concerns of FSWs and may contribute to the sustainability of the program once ownership is handed over to the Indian government and the FSW community.41
Acknowledgments
Support for this study was provided by the Bill & Melinda Gates Foundation and by the UK Department for International Development–funded STRIVE structural drivers HIV research consortium.
We would like to thank Judith Glynn, MD, PhD, for useful discussions on pathway analyses and James Moore from the Bill & Melinda Gates Foundation for helpful contributions during the study design. We also thank the female sex worker populations throughout Karnataka with whom we work, and the staff members of the program implementing nongovernmental organizations for their tireless work in enhancing HIV prevention programming.
Note. The views expressed herein are those of the authors and do not necessarily reflect the official policy or position of the Bill & Melinda Gates Foundation or the UK Department for International Development.
Human Participant Protection
This study was approved by the Institutional Ethical Review Board of St. John’s Medical College, Bangalore, India, and the Health Research Ethics Board of the University of Manitoba, Winnipeg. Participation in the IBBAs was by witnessed, verbal, informed consent. Statutory approval for the conduct of the IBBAs and their protocols was obtained from the Government of India’s Health Ministry Screening Committee.
References
- 1.Foss AM, Hossain M, Vickerman PT, Watts CH. A systematic review of published evidence on intervention impact on condom use in sub-Saharan Africa and Asia. Sex Transm Infect. 2007;83(7):510–516. doi: 10.1136/sti.2007.027144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shahmanesh M, Patel V, Mabey D, Cowan F. Effectiveness of interventions for the prevention of HIV and other sexually transmitted infections in female sex workers in resource poor setting: a systematic review. Trop Med Int Health. 2008;13(5):659–679. doi: 10.1111/j.1365-3156.2008.02040.x. [DOI] [PubMed] [Google Scholar]
- 3.Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 4.Auerbach JD, Parkhurst JO, Caceres CF. Addressing social drivers of HIV/AIDS for the long-term response: conceptual and methodological considerations. Glob Public Health. 2011;6(suppl 3):S293–S309. doi: 10.1080/17441692.2011.594451. [DOI] [PubMed] [Google Scholar]
- 5.Blankenship KM, Bray SJ, Merson MH. Structural interventions in public health. AIDS. 2000;14(suppl 1):S11–S21. doi: 10.1097/00002030-200006001-00003. [DOI] [PubMed] [Google Scholar]
- 6.Evans C, Jana S, Lambert H. What makes a structural intervention? Reducing vulnerability to HIV in community settings, with particular reference to sex work. Glob Public Health. 2010;5(5):449–461. doi: 10.1080/17441690902942472. [DOI] [PubMed] [Google Scholar]
- 7.Parkhurst JO. HIV prevention, structural change and social values: the need for an explicit normative approach. J Int AIDS Soc. 2012;15(suppl 1):1–10. doi: 10.7448/IAS.15.3.17367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strathdee SA, Wechsberg WM, Kerrigan DL, Patterson TL. HIV prevention among women in low- and middle-income countries: intervening upon contexts of heightened HIV risk. Annu Rev Public Health. 2013;34:301–316. doi: 10.1146/annurev-publhealth-031912-114411. [DOI] [PubMed] [Google Scholar]
- 9.Blanchard AK, Mohan HL, Shahmanesh M et al. Community mobilization, empowerment and HIV prevention among female sex workers in south India. BMC Public Health. 2013;13:234. doi: 10.1186/1471-2458-13-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cornish F. Empowerment to participate: a case study of participation by Indian sex workers in HIV prevention. J Community Appl Soc Psychol. 2006;16(4):301–315. [Google Scholar]
- 11.Blankenship KM, West BS, Kershaw TS, Biradavolu MR. Power, community mobilization, and condom use practices among female sex workers in Andhra Pradesh, India. AIDS. 2008;22(suppl 5):S109–S116. doi: 10.1097/01.aids.0000343769.92949.dd. [DOI] [PubMed] [Google Scholar]
- 12.Swendeman D, Basu I, Das S, Jana S, Rotheram-Borus MJ. Empowering sex workers in India to reduce vulnerability to HIV and sexually transmitted diseases. Soc Sci Med. 2009;69(8):1157–1166. doi: 10.1016/j.socscimed.2009.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwartländer B, Stover J, Hallett T et al. Towards an improved investment approach for an effective response to HIV/AIDS. Lancet. 2011;377(9782):2031–2041. doi: 10.1016/S0140-6736(11)60702-2. [DOI] [PubMed] [Google Scholar]
- 14.Kabeer N. Resources, agency, achievements: reflections on the measurement of women’s empowerment. Dev Change. 1999;30(3):435–464. [Google Scholar]
- 15.Kim JC, Watts CH, Hargreaves JR et al. Understanding the impact of a microfinance-based intervention on women’s empowerment and the reduction of intimate partner violence in South Africa. Am J Public Health. 2007;97(10):1794–1802. doi: 10.2105/AJPH.2006.095521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mosedale S. Assessing women’s empowerment: towards a conceptual framework. J Int Dev. 2005;17(2):243–257. [Google Scholar]
- 17.Kerrigan D, Moreno L, Rosario S et al. Environmental-structural interventions to reduce HIV/STI risk among female sex workers in the Dominican Republic. Am J Public Health. 2006;96(1):120–125. doi: 10.2105/AJPH.2004.042200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cornish F, Ghosh R. The necessary contradictions of “community-led” health promotion: a case study of HIV prevention in an Indian red light district. Soc Sci Med. 2007;64(2):496–507. doi: 10.1016/j.socscimed.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Ghose T, Swendeman D, George S, Chowdhury D. Mobilizing collective identity to reduce HIV risk among sex workers in Sonagachi, India: the boundaries, consciousness, negotiation framework. Soc Sci Med. 2008;67(2):311–320. doi: 10.1016/j.socscimed.2008.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jana S, Basu I, Rotheram-Borus MJ, Newman PA. The Sonagachi Project: a sustainable community intervention program. AIDS Educ Prev. 2004;16(5):405–414. doi: 10.1521/aeap.16.5.405.48734. [DOI] [PubMed] [Google Scholar]
- 21.Beattie TSH, Bhattacharjee P, Ramesh BM et al. Violence against female sex workers in Karnataka state, south India: impact on health, and reductions in violence following an intervention program. BMC Public Health. 2010;10:476. doi: 10.1186/1471-2458-10-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Biradavolu MR, Burris S, George A, Jena A, Blankenship KM. Can sex workers regulate police? Learning from an HIV prevention project for sex workers in southern India. Soc Sci Med. 2009;68(8):1541–1547. doi: 10.1016/j.socscimed.2009.01.040. [DOI] [PubMed] [Google Scholar]
- 23.Erausquin JT, Reed E, Blankenship KM. Police-related experiences and HIV risk among female sex workers in Andhra Pradesh, India. J Infect Dis. 2011;204(suppl 5):S1223–S1228. doi: 10.1093/infdis/jir539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reed E, Gupta J, Biradavolu M, Devireddy V, Blankenship KM. The context of economic insecurity and its relation to violence and risk factors for HIV among female sex workers in Andhra Pradesh, India. Public Health Rep. 2010;125(suppl 4):81–89. doi: 10.1177/00333549101250S412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reed E, Gupta J, Biradavolu M, Devireddy V, Blankenship KM. The role of housing in determining HIV risk among female sex workers in Andhra Pradesh, India: considering women’s life contexts. Soc Sci Med. 2011;72(5):710–716. doi: 10.1016/j.socscimed.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 26.Reza-Paul S, Beattie T, Syed HU et al. Declines in risk behaviour and sexually transmitted infection prevalence following a community-led HIV preventive intervention among female sex workers in Mysore, India. AIDS. 2008;22(suppl 5):S91–S100. doi: 10.1097/01.aids.0000343767.08197.18. [DOI] [PubMed] [Google Scholar]
- 27.Reza-Paul S, Lorway R, O’Brien N et al. Sex worker-led structural interventions in India: a case study on addressing violence in HIV prevention through the Ashodaya Samithi collective in Mysore. Indian J Med Res. 2012;135:98–106. doi: 10.4103/0971-5916.93431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swain SN, Saggurti N, Battala M, Verma RK, Jain AK. Experience of violence and adverse reproductive health outcomes, HIV risks among mobile female sex workers in India. BMC Public Health. 2011;11:357. doi: 10.1186/1471-2458-11-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blankenship KM, Biradavolu MR, Jena A, George A. Challenging the stigmatization of female sex workers through a community-led structural intervention: learning from a case study of a female sex worker intervention in Andhra Pradesh, India. AIDS Care. 2010;22(suppl 2):1629–1636. doi: 10.1080/09540121.2010.516342. [DOI] [PubMed] [Google Scholar]
- 30.Cornish F. Challenging the stigma of sex work in India: material context and symbolic change. J Community Appl Soc Psychol. 2006;16(6):462–471. [Google Scholar]
- 31.Gurnani V, Beattie TS, Bhattacharjee P et al. An integrated structural intervention to reduce vulnerability to HIV and sexually transmitted infections among female sex workers in Karnataka state, south India. BMC Public Health. 2011;11:755. doi: 10.1186/1471-2458-11-755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Erausquin JT, Biradavolu M, Reed E, Burroway R, Blankenship K. Trends in condom use among female sex workers in Andhra Pradesh, India: the impact of a community mobilisation intervention. J Epidemiol Community Health. 2012;66(suppl 2):ii49–ii54. doi: 10.1136/jech-2011-200511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parimi P, Mishra R, Tucker S, Saggurti N. Mobilising community collectivisation among female sex workers to promote STI service utilisation from the government healthcare system in Andhra Pradesh, India. J Epidemiol Community Health. 2012;66(suppl 2):ii62–ii68. doi: 10.1136/jech-2011-200832. [DOI] [PubMed] [Google Scholar]
- 34.Halli SS, Ramesh BM, O’Neil J, Moses S, Blanchard JF. The role of collectives in STI and HIV/AIDS prevention among female sex workers in Karnataka, India. AIDS Care. 2006;18(7):739–749. doi: 10.1080/09540120500466937. [DOI] [PubMed] [Google Scholar]
- 35.Lippman SA, Chinaglia M, Donini AA, Diaz J, Reingold A, Kerrigan DL. Findings from Encontros: a multilevel STI/HIV intervention to increase condom use, reduce STI, and change the social environment among sex workers in Brazil. Sex Transm Dis. 2012;39(3):209–216. doi: 10.1097/OLQ.0b013e31823b1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.UNAIDS. UNAIDS report on the global AIDS epidemic. 2010. Available at: http://www.unaids.org/globalreport/documents/20101123_GlobalReport_full_en.pdf. Accessed December 9, 2011.
- 37.Indian Council of Medical Research and Family Health International. National Interim Summary Report, Integrated Behavioural and Biological Assessment (IBBA), Round 1 (2005-2007) 2007. Available at: http://www.nari-icmr.res.in/pdf/IBBA/IBBA-NISR.pdf. Accessed April 23, 2014.
- 38.Population Foundation of India KSAPS. HIV/AIDS in Karnataka: Situation and Response. Bangalore, India: Karnataka State AIDS Prevention Society; 2004. Available at: http://www.prb.org/pdf04/HIVinKarnataka.pdf. Accessed December 9, 2011. [Google Scholar]
- 39.New Delhi: The Bill & Melinda Gates Foundation; 2008. Avahan–the India AIDS initiative: The business of HIV prevention at scale. Available at: http://www.gatesfoundation.org/avahan/Documents/Avahan_HIVPrevention.pdf. Accessed April 1, 2010. [Google Scholar]
- 40.Chandrasekaran P, Dallabetta G, Loo V et al. Evaluation design for large-scale HIV prevention programmes: the case of Avahan, the India AIDS initiative. AIDS. 2008;22(suppl 5):S1–S15. doi: 10.1097/01.aids.0000343760.70078.89. [DOI] [PubMed] [Google Scholar]
- 41.Bennett S, Singh S, Ozawa S, Tran N, Kang JS. Sustainability of donor programs: evaluating and informing the transition of a large HIV prevention program in India to local ownership. Glob Health Action. 2011;4:7360. doi: 10.3402/gha.v4i0.7360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ramesh BM, Beattie TS, Shajy I et al. Changes in risk behaviours and prevalence of sexually transmitted infections following HIV preventive interventions among female sex workers in five districts in Karnataka state, south India. Sex Transm Infect. 2010;86(suppl 1):i17–i24. doi: 10.1136/sti.2009.038513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ramesh BM, Moses S, Washington R et al. Determinants of HIV prevalence among female sex workers in four south Indian states: analysis of cross-sectional surveys in twenty-three districts. AIDS. 2008;22(suppl 5):S35–S44. doi: 10.1097/01.aids.0000343762.54831.5c. [DOI] [PubMed] [Google Scholar]
- 44.Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. 1997;26(1):224–227. doi: 10.1093/ije/26.1.224. [DOI] [PubMed] [Google Scholar]
- 45.Blanchard JF, O’Neil J, Ramesh BM, Bhattacharjee P, Orchard T, Moses S. Understanding the social and cultural contexts of female sex workers in Karnataka, India: implications for prevention of HIV infection. J Infect Dis. 2005;191(suppl 1):S139–S146. doi: 10.1086/425273. [DOI] [PubMed] [Google Scholar]
- 46.Campbell C, Cornish F. How can community health programmes build enabling environments for transformative communication? Experiences from India and South Africa. AIDS Behav. 2012;16(4):847–857. doi: 10.1007/s10461-011-9966-2. [DOI] [PubMed] [Google Scholar]
- 47.Kerrigan D, Telles P, Torres H, Overs C, Castle C. Community development and HIV/STI-related vulnerability among female sex workers in Rio de Janeiro, Brazil. Health Educ Res. 2008;23(1):137–145. doi: 10.1093/her/cym011. [DOI] [PubMed] [Google Scholar]
- 48.Hanck SE, Blankenship KM, Irwin KS, West BS, Kershaw T. Assessment of self-reported sexual behavior and condom use among female sex workers in India using a polling box approach: a preliminary report. Sex Transm Dis. 2008;35(5):489–494. doi: 10.1097/OLQ.0b013e3181653433. [DOI] [PubMed] [Google Scholar]
- 49.Lowndes CM, Jayachandran AA, Pradeep BS . High Levels of HIV-Related Risky Behaviour Reported Through Polling Booth Surveys in Comparison to Face-to-Face Interviews in a General Population Survey in Mysore District, Karnataka State, Southern India. Amsterdam, The Netherlands: The International Society for Sexually Transmitted Diseases Research; 2007. [Google Scholar]
- 50.Patel V, Pednekar S, Weiss H et al. Why do women complain of vaginal discharge? A population survey of infectious and pyschosocial risk factors in a South Asian community. Int J Epidemiol. 2005;34(4):853–862. doi: 10.1093/ije/dyi072. [DOI] [PubMed] [Google Scholar]
- 51.Patel V, Weiss HA, Kirkwood BR et al. Common genital complaints in women: the contribution of psychosocial and infectious factors in a population-based cohort study in Goa, India. Int J Epidemiol. 2006;35(6):1478–1485. doi: 10.1093/ije/dyl219. [DOI] [PubMed] [Google Scholar]
- 52.Gottlieb SL, Martin DH, Xu F, Byrne G, Brunham R. Summary: the natural history and immunobiology of Chlamydia trachomatis genital infection and implications for Chlamydia control. J Infect Dis. 2010;201(suppl 2):S190–S204. doi: 10.1086/652401. [DOI] [PubMed] [Google Scholar]
- 53.Hook E, Handsfield H. Gonococcal infections in the adult. In: Holmes K, Mardh P, Sparling P, editors. Sexually Transmitted Diseases. 3rd ed. New York, NY: McGraw-Hill; 1999. pp. 451–466. [Google Scholar]
- 54.Campbell C, Cornish F. Towards a “fourth generation” of approaches to HIV/AIDS management: creating contexts for effective community mobilisation. AIDS Care. 2010;22(suppl 2):1569–1579. doi: 10.1080/09540121.2010.525812. [DOI] [PubMed] [Google Scholar]