Abstract
Background:
Palmoplantar lesions in lichen planus (LP) are uncommon. In such cases, diagnosis is usually missed. This study was conducted to document various clinical and histopathological features of palmoplantar LP.
Materials And Methods:
A total of 18 patients from our outpatient department with lesions of LP, either predominantly or exclusively on palms and/or soles were studied. Patients with history of drug intake in recent past and patients with classical acute widespread LP with a few lesions on palms or soles were excluded. In each patient, diagnosis was made on clinicopathological correlation. Various clinical and histopathological features were analyzed.
Results:
Average age of onset was 38 years. Male: female ratio was 1:0.6 and average disease duration was 11 months. Exclusive palm or sole involvement was seen in 4/18 patients. Itching was the most common symptom. Clinically the most common variant was hypertrophic. Histologically presence of parakeratosis, spongiosis, lack of melanophages, and lack of hypergranulosis in some cases was seen in addition to classical features of LP. In 3 out of 4 patients with exclusive palmoplantar involvement diagnosis of LP was missed clinically.
Conclusion:
Involvement of palms and soles in LP poses a diagnostic challenge due to variable presentations. Histopathology is of vital importance for correct diagnosis and treatment.
Keywords: Clinico-pathological study, lichen planus, palm, sole
Introduction
What was known?
Lichen planus is a common inflammatory papulosquamous disorder of unknown etiology
Involvement of palms and soles is rare in lichen planus
Clinical presentations and histological variations of LP on palms and soles are not studied well.
Lichen planus is a common inflammatory papulosquamous disorder affecting skin, mucous membranes, nails and hairs variably.[1] Involvement of palm and soles is thought to be uncommon in LP.[2] Palmoplantar LP has varied morphological presentations apart from classically described yellowish hyperkeratotic papules and plaques. Skin biopsy is of vital importance to make the correct diagnosis and thus correct treatment in such cases.[3] We studied 18 patients of LP on palm and/or soles over a period of 6 months. The aim of present study was to characterize various clinical presentations and histopathological variations in lesions of LP on palms and soles.
Materials and Methods
A total of 18 patients of palmoplantar LP were enrolled over a period of six months. All the patients were subjected to detailed history taking, clinical examination and skin biopsy after informed consent. In each patient the diagnosis was made on clinico-pathological correlation. Clinical variables, such as age, sex, family history of LP, duration of disease, symptoms, type of lesions, distribution of lesions over palms and soles, other sites affected, mucosal and nail involvement, previous treatments taken if any and previous clinical diagnosis. Patients with history of drug intake in recent past were excluded. Variables considered in histopathological examination included parakeratosis, hypergranulosis, saw-tooth, spongiosis, type of infiltrate, changes at dermo-epidermal junction (D-E junction), presence of colloid bodies, melanophages, eosinophils, depth of infiltrate and any other additional findings. Finding from all the patients were tabulated and analyzed to characterize various clinico-pathological features of LP on palms and soles.
Results
Clinical
Average age of disease onset was 38 years. The youngest patient was 9 year old, while the oldest was 72 year old. Males were more commonly affected than females with a male: female ratio 1:0.6.
Average duration of disease was 11 months with the shortest duration being 1 month while the longest being 8 years. Average duration of palmoplantar lesions was 5 months as in some patients palmoplantar involvement was preceded by lesions at other sites.
Family history of lichen planus was not seen in any of our patients and no other associated skin disease was seen except in one patient, who had atopic dermatitis with peripheral eosinophilia.
Itching was the most common symptom seen in 17/18 (94%) followed by pain (4/18) and fissuring (3/18) while none of our patient was asymptomatic.
In 4/18 (22%) patients LP appeared simultaneously in palmoplantar region and elsewhere, while in remaining 11/18 (61%) patient lesions elsewhere preceded the palmoplantar lesions.
Exclusive palmoplantar involvement was seen in 4/18 (22%) patients. Out of these 4 patients 2 had exclusive palmar lesions while 2 had lesions only on soles. Remaining 14 patients had lesions elsewhere along with palmoplantar region, lower extremities being the commonest site followed by upper limbs and trunk.
Mucosal involvement was seen in 5/18 (28%) patients, 4 of which had oral mucosal involvement and one had genital mucosal involvement. Erosions in oral cavity were seen in 3 patients while one patient had reticulate lesions. Buccal mucosa and lips were the sites affected in oral cavity while glans penis and prepuce was affected in genitalia. Nail involvement was seen in 2/18 (11%) patients. Yellowish discoloration of nails with subungual hyperkeratosis and nail dystrophy was seen.
Common site affected on sole was internal plantar arch while on palms thenar and hypo-thenar eminence and central palmar region were affected in that order. In 8/18 (44%) patient's lesions were symmetrical while asymmetrical lesions were seen in remaining 12 patients.
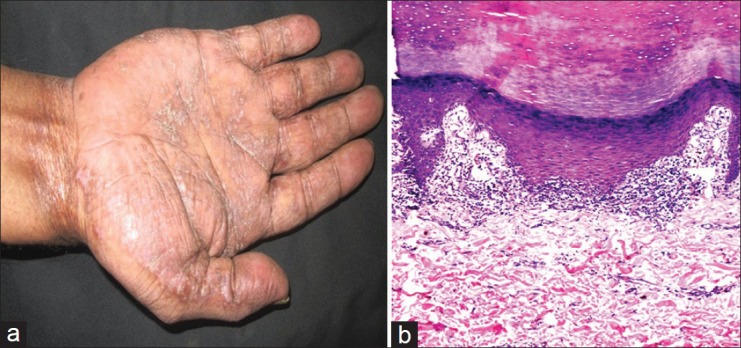
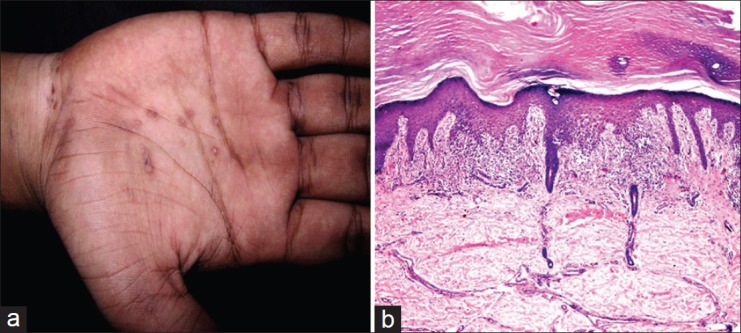
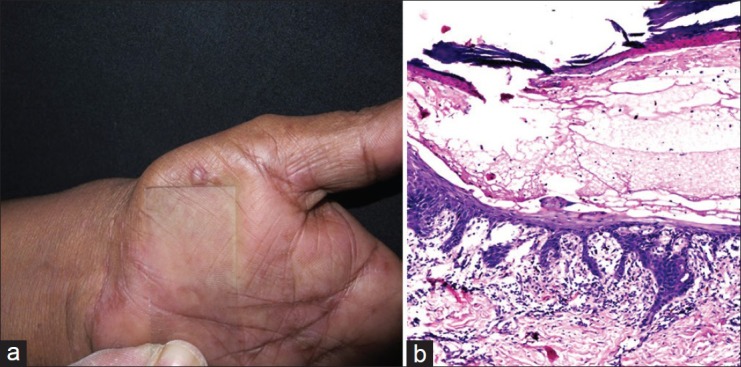
Morphologically hypertrophic variant seen in 7/18 (39%) was the most common variant [Figure 1], Diffuse scaling variant [Figure 2], psoriasiform variant with fissuring [Figure 3] and plaque with collarette scaling [Figure 4] was seen in 2/18 (11%) patients each.
Figure 1.
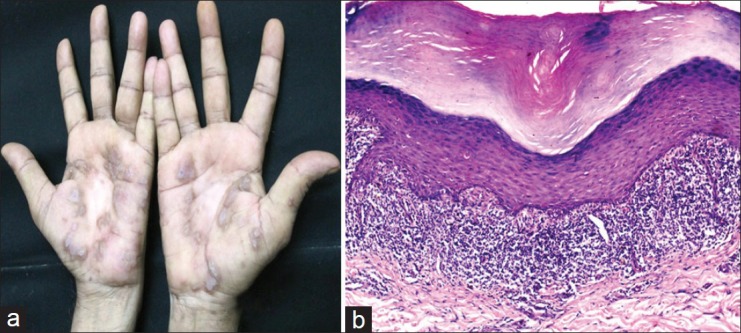
Hypertrophic variant with symmetric lesions on bilateral palms. Biopsy from lesion showing typical features of lichen planus viz, hyperkeratosis, acanthosis, wedge- shaped hypergranulosis, band like lymphocytic infiltrate and interface with saw-tooth rete-ridges (H and E, ×100)
Figure 2.
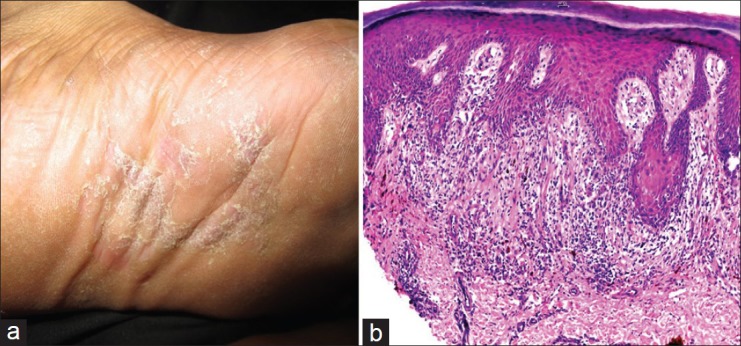
Diffuse scaly variant with lesion on sole, histologically showing irregular epidermal hyperplasia, melanophages, necrotic keratinocytes and lichenoid infiltrate with interface change. (H and E, ×100)
Figure 3.
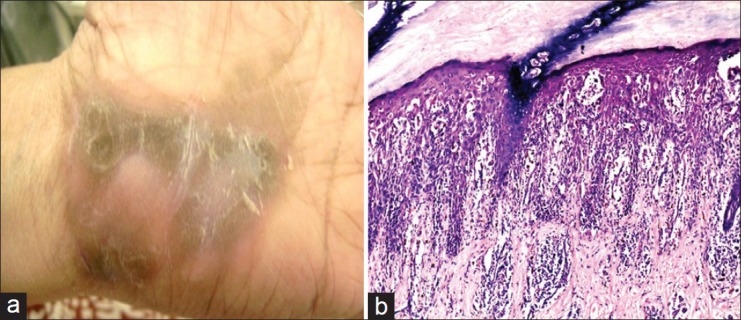
Psoriasiform variant with fissures over palm. Biopsy from lesion showing, severe spongiosis along with lichenoid lymphohistiocytic infiltrate, hypergranulosis, melanophages, irregular hyperplasia and necrotic keratinocytes. (H and E, ×100)
Figure 4.

Multiple plaques with collarette scales over sole. A large parakeratotic scale seen on biopsy corresponds to collarette scale seen clinically. Typical features of lichen planus are also seen. (H and E, ×100)
Keratotic plaque with pits was seen in one patient. Histopathologically it showed perforation of epidermis by a parakeratotic plug and this case has been published separately under the title of perforating lichen planus.[4]
Among the other variants; each seen in one patient; these includes diffuse keratoderma [Figure 5], punctate keratoses [Figure 6], vesicular [Figure 7] and macular variant.
Figure 5.
Lichen planus on palm presenting as diffuse keratoderma. Histologically there is compact hyperkeratosis with epidermal hyperplasia, hypergranulosis and band like infiltrate of lymphocytes with squamatisation. H and E, ×100)
Figure 6.
Lichen planus on palm presenting as punctuate keratoses, histologically there is compact hyperkeratosis, hypergranulosis, irregular epidermal hyperplasia and lichenoid interface (H and E, ×100)
Figure 7.
Vesicular lesion of lichen planus on palm. Biopsy from lesion showed intraepidermal vesicle along with band like lymphocytic infiltrate and interface change and saw-tooth rete-ridges. (H and E, ×100)
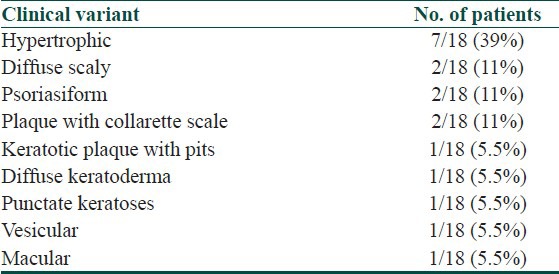
Various morphological variants seen and their percentage are shown in Table 1.
Table 1.
Various morphological variants and their percentage
Histopathological
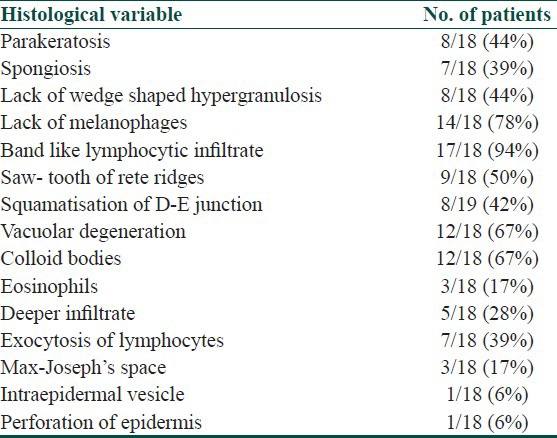
A total of 18 biopsies were obtained from palmoplantar region of 18 patients. Almost all biopsies showed characteristic features of lichen planus [Figure 1] except two cases. Perforation of epidermis by a parakeratotic plug with acrosyringeal accentuation of infiltrate was seen in one case. Also additional features like spongiosis [Figure 3], parakeratosis [Figure 4] and lack of melanophages were seen variably in some cases. One of our patient had vesicular lesions and biopsy showed intraepidermal vesicle along with classic features of lichen planus. [Figure 7] Various histological parameters and their percentage are shown below in Table 2.
Table 2.
Various histological observations with their percentage
In our study, common clinical diagnosis for patients having lesions elsewhere along with palmoplantar lesions included lichen planus, lichenoid eruption, lichen nitidus. Common clinical diagnosis for patients with exclusive palmoplantar involvement included psoriasis, eczema, keratoderma, lichen nitidus and warts. Out of 4 patients with exclusive palmoplantar involvement, a diagnosis of LP was thought clinically in only one case, while in remaining three cases it was diagnosed histopathologically.
Discussion
Palmoplantar lesions in LP were more common in males than females in our study. Similar sex bias has been observed by Sanchez-Perez et al. and Mugoni et al.[2,3]
Average age of disease onset was 38 years in our study with a range of 9-72 years, while in a study by Sanchez-Perez et al. majority of lesions appeared in between 42.5 years of age with a range of 13-71 years and in a case series of 5 cases of palmoplantar LP by Mugoni et al. average age was 65 years.[2,3]
Itching was the most common symptom seen in 90% patients. Sanchez-Perez et al. found 11% patients to be asymptomatic and pruritus as the commonest symptom in remaining.[2]
In none of our patients, there was personal or family history of lichen planus and only one had personal history of atopy. Sanchez-Perez et al. found personal and/or family history of atopy in 6 out of 36 patients.[2]
Various known morphological presentations of palmoplantar lichen planus (PPLP) include hypertrophic variant, diffuse scaly variant, punctuate keratoses, diffuse keratoderma, erosive or ulcerative lesions, pigmented macular variant, vesicular lesions, keratotic plaques with pits and umbillicated papules. In such cases it is usually mistaken clinically for other dermatoses like eczema, psoriasis, palmoplantar keratoderma, warts, secondary syphilis, lichen nitidus, arsenical keratoses, porokeratosis and so on.[2,3,5]
In a study of 87 patients of childhood lichen planus, palmoplantar lesions were observed in 2.3% of patients. Involvement of eyelid was seen in 3 patients in the same study.[6] No eyelid involvement was seen in our study.
Ucmak et al. reported four cases of PPLP in adults and found various morphologies of lesions like, keratotic papules, hard keratotic plaques, annular plaques over finger tips and diffuse erythematous plaques over bilateral palms.[7] Kim et al. reported violaceous, umbilicated and vesicle like papules in one case and violaceous petechia like macules and semi-translucent targetoid papules in other case.[8] Kim et al. reported a case in a 37-year-old male with scaly erythematous and hyperkeratotic papules mimicking secondary syphilis.[9]
Cheung-Lee MJ, reported a case with violaceous papules over palms and soles in a 60 year old female. They treated her with potent topical steroids and oral acitretin and found dramatic response to this combination therapy.[10] Rotunda et al. reported a case with multiple hyperkeratotic plaques over palms and soles diagnosed by histopathology.[11]
Kamer et al. reported a 25 year-old lady with palmoplantar LP presenting with vesicle like papules.[12] All these cases highlight variations in clinical presentations of PPLP and importance of histopathology in its diagnosis.
Malignant change can occur due to persistent chronic inflammation rarely in PPLP.[13] A case of verrucous carcinoma arising in ulcerative LP of soles has been reported.[14]
The internal plantar arch was the most commonly affected site, in our study as observed by Sanchez-Perez et al. also.[2] Amongst the sites other than palms and soles, lower extremities, especially shin was the commonest site followed by upper extremities and trunk. Mucosal and nail involvement was seen in 26% and 11% patients respectively. Mugoni et al. observed mucosal involvement in 3 out of 5 patients of palmoplantar LP.[3]
In a study by Sanchez-Perez et al. lesions began outside palmoplantar region in 72% patients as compared to 58% in our study.[2]
The palmoplantar LP showed a characteristic histopathology, very similar to that described for other sites in nearly 90% of our patients with some additional features.
Some of unusual features included, parakeratosis seen in 44%, spongiosis in 39%, lack of melanophages in 78%, lack of wedge shaped hypergranulosis in 44%, deeper infiltrate in 26%. Eosinophils were seen in 17% of patients. None of these had either history or clinical appearance of any superimposed allergic contact dermatitis or any history of atopy. Spongiosis was more pronounced in psoriasiform variant, though it was seen in other variants also. Also presence of eosinophils and spongiosis was seen in one case while other two cases showing eosinophils were not associated with spongiosis. Thus, the mere presence of focal parakeratosis, eosinophils, spongiosis and deep perivascular infiltrate does not always indicate a lichenoid drug eruption as per as LP over palms and soles is concerned.
Vesicular lesions were seen in one patient and showed intraepidermal vesicle on histopathology, which we could not explain.
Keratotic plaque with pits was seen in one case and histopathology showed perforation of epidermis by a parakeratotic plug with acrosyringeal accentuation of infiltrate.
In conclusion, LP lesions over palms and soles are not as uncommon as thought and always do not have a classical features. High index of suspicion is needed due to varied clinical presentation. Histopathology is useful for correct diagnosis in such cases.
What is new?
Involvement of palms and soles in lichen planus do not appear to be rare but under diagnosed.
LP on palms and soles has a varied clinical presentation and need a high index of suspicion.
Histopathologically, LP of palms and soles may show some unusual features like lack of melanophages, spongiosis, etc., and clinico-pathological correlation is needed in such cases.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Inamdar AC, Palit A. On lichen planus and lichenoid disorders. IADVL Textbook of Dermatology. In: Valia RG, Valia AR, editors. 3rd ed. Mumbai, India: Bhalani Publishers; 2008. [Google Scholar]
- 2.Sánchez-Pérez J, Rios Buceta L, Fraga J, García-Díez A. Lichen planus with lesions on the palms and/or soles: Prevalence and clinicopathological study of 36 patients. Br J Dermatol. 2000;142:310–4. doi: 10.1046/j.1365-2133.2000.03303.x. [DOI] [PubMed] [Google Scholar]
- 3.Mugoni MG, Montesu MA, Cottoni F. Lichen planus on palms and soles. J Eur Acad Dermatol Venereol. 1994;3:535–40. [Google Scholar]
- 4.Gutte R, Khopkar U. Perforating lichen planus. Indian J Dermatol Venereol Leprol. 2011;77:515–7. doi: 10.4103/0378-6323.82390. [DOI] [PubMed] [Google Scholar]
- 5.Khandpur S, Kathuria SD, Gupta R, Singh MK, Sharma VK. Hyperkeratotic pitted plaques on palms and soles. Indian J Dermatol Venereol Leprol. 2010;76:52–5. doi: 10.4103/0378-6323.58680. [DOI] [PubMed] [Google Scholar]
- 6.Handa S, Sahoo B. Childhood lichen planus: A study of 87 cases. Int J Dermatol. 2002;41:423–7. doi: 10.1046/j.1365-4362.2002.01522.x. [DOI] [PubMed] [Google Scholar]
- 7.Ucmak D, Azizoglu R, Harman M. Palmoplantar lichen planus- a report of four cases. Journal of Clinical and Experimental Investigations. 2011;2:80–4. [Google Scholar]
- 8.Kim MJ, Choi M, Na SY, Lee JH, Cho S. Two cases of palmoplantar lichen palnus with various clinical features. J Dermatol. 2011;37:985–9. doi: 10.1111/j.1346-8138.2010.00936.x. [DOI] [PubMed] [Google Scholar]
- 9.Kim YS, Kim MH, Kim CW, Shin DH, Choi JS, Kim KH. A case of palmoplantar lichen planus mimicking secondary syphilis. Ann Dermatol. 2009;21:429–31. doi: 10.5021/ad.2009.21.4.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheung-Lee MJ. Violaceous papules on palms and soles. J Cutan Med Surg. 2008;12:35–7. doi: 10.2310/7750.2008.07024. [DOI] [PubMed] [Google Scholar]
- 11.Rotunda AM, Craft N, Haley JC. Hyperkeratotic plaques on the palms and soles. Palmoplantar lichen planus, hyperkeratotic variant. Arch Dermatol. 2004;140:1275–80. doi: 10.1001/archderm.140.10.1275-c. [DOI] [PubMed] [Google Scholar]
- 12.Gündüz K, Inanir I, Türkdogan P, Sacar H. Palmoplantar lichen planus presenting with vesicle-like papules. J Dermatol. 2003;30:337–40. doi: 10.1111/j.1346-8138.2003.tb00397.x. [DOI] [PubMed] [Google Scholar]
- 13.Dogra D, Sharma N, Khanna N. Squamous cell carcinoma arising in lichen planus hypertrophicus. Indian J Dermatol. 1997;42:30–1. [Google Scholar]
- 14.Mayron R, Grimwood RE, Siegle RJ, Camisa C. Verrucous carcinoma arising in ulcerative lichen planus of the soles. J Dermatol Surg Oncol. 1988;14:547–51. doi: 10.1111/j.1524-4725.1988.tb01150.x. [DOI] [PubMed] [Google Scholar]


