Abstract
For most dermatologists, the challenge posed by toxic epidermal necrolysis (TEN) lies not in its diagnosis, but in pulling the patient out of this life-threatening condition. However, when a patient presents with a TEN-like picture in the background of lupus erythematosus (LE), it becomes difficult to decide whether the eruption is drug induced or a manifestation of lupus itself.
Keywords: Acute cutaneous lupus erythematosus, systemic lupus erythematosus, toxic epidermal necrolysis
Introduction
What was known?
Toxic epidermal necrolysis (TEN) -like rash of lupus, a rare entity, is clinically indistinguishable from drug - induced TEN.
Toxic epidermal necrolysis (TEN) is a common, yet one of the most dreaded dermatological emergencies. TEN-like rash of lupus, which is clinically indistinguishable from drug-induced TEN, is a rare entity, with less than 50 cases reported worldwide.[1]
Unless there is a high index of suspicion, the subtle features of LE, complemented with investigative findings like hematological abnormalities, proteinuria, high positive antinuclear antibody (ANA) titer, and so on can be easily overlooked in a sick patient presenting with vesiculobullous lesions with peeling of skin, screaming for urgent management.
Case Report
We came across a 45-year-old female, who presented in emergency with a history of an insidious-onset peeling of skin, vesiculobullous lesions, and oral ulceration, which developed over the previous 10 days, without any acute primordial signs or symptoms [Figure 1]. She gave a history of fever on and off with pain in multiple joints for two years for which she had been taking diclofenac and naproxen almost on a daily basis, without developing any systemic or cutaneous adverse effect, making these two drugs unlikely culprits. She also reported a history suggestive of photosensitivity and painless oral ulcers over the previous two years. There was no history of any infection or intake of any other drug. Routine hematological and biochemical investigations revealed anemia [hemoglobin (Hb): 7 gm%] with a positivity for direct Coomb's test, hypoproteinemia (5.5 gm%), and proteinuria (3+). ANA and anti-dsDNA (dsDNA: Double-stranded deoxyribonucleic acid) were positive (ANA titer by immunoflorescence 1:1280, homogenous and peripheral; anti-dsDNA titer 1:640). The patient was put on systemic steroids, namely, prednisolone, with a dose of 1.5 mg/kg/day once daily, till clinical improvement, both cutaneous and systemic, was apparent. This was about a week later, following which the oral steroid was slowly tapered. The active vesiculobullous lesion healed completely over two weeks, revealing the previously inapparent malar and discoid rash of lupus over the face [Figure 2]. Skin biopsy from a discoid lesion over the forehead revealed epidermal atrophy, interface dermatitis, follicular plugging, and basal cell degeneration, suggesting discoid lupus erythematosus [Figure 3]. Direct immunofluorescence (DIF) showed immunoglobulin G (IgG) and complement 3 (C3) deposits at the dermo-epidermal junction.
Figure 1.

Sheet-like desquamation over back (a), chest (b), and hemorrhagic crusting over lips (c)
Figure 2.
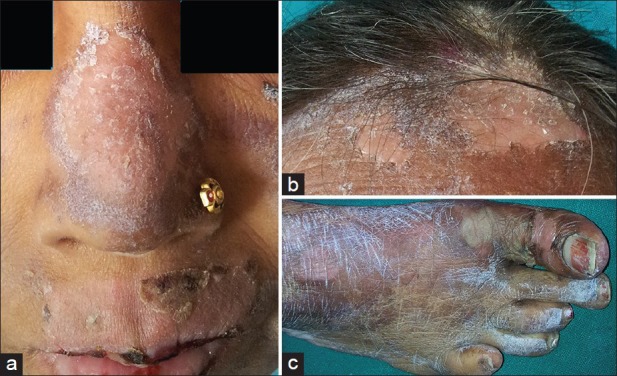
Well-defined, discoid plaques over the nose (a), forehead (b), and right foot (c)
Figure 3.
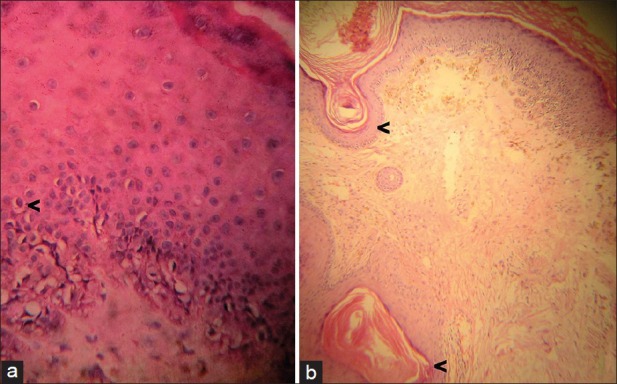
(a) Histology showing basal cell vacuolization (H and E, ×10); (b) epidermal atrophy, follicular plugging, interface dermatitis, dermal edema (H and E stain, ×10)
Discussion
Vesiculobullous lesions occurring in the setting of LE were classified by Sontheimer[2] as
TEN-like acute cutaneous LE
TEN-like subacute cutaneous LE
TEN occurring in systemic lupus erythematosus (SLE) patients not having conventional LE-specific skin lesions
Vesiculobullous changes occurring at the active border of advancing annular subacute cutaneous LE
Vesiculobullous chronic cutaneous LE.
The first three entities, which are associated with an exacerbation of activity of the underlying lupus, clinically mimic drug-induced TEN, but differ widely in terms of etiopathogenesis. It has been proposed that exaggerated keratinocyte apoptosis due to increase in Fas expression may underlie many of the major manifestations of LE, including cutaneous lesions as seen in our patient.[3,4]
Differentiating TEN-like lesions of LE from drug-induced TEN can be a challenge because TEN is known to occur with increased frequency in connective tissue disease.[5,6] Moreover, patients of SLE are often on chronic medication which further increases the risk of drug-induced TEN Histopathological findings are almost identical (full-thickness epithelial necrosis and sparse superficial lymphocytic infiltrate) Both respond well to steroids.
However, the points which favor TEN-like rash of LE over drug-induced TEN are Lack of evidence of ingestion of high-risk drugs Photodistribution of TEN-like lesions Subacute presentation over weeks Recent exacerbation of SLE History of painless oral ulcer Associated malar or discoid rash Distinctive serologic profile, including a strongly positive ANA and positive anti-dsDNA, suggestive of underlying connective tissue disease
However, these differences are largely subjective and theoretical. Lately, a unifying concept of ‘acute syndrome of apoptotic pan-epidermolysis (ASAP)’ has been proposed by Ting et al. in 2004. It encompasses all the life-threatening clinical situations of massive epidermal cleavage resulting from a hyperacute apoptotic injury, which may be drug induced or due to other causes like LE, acute graft versus host disease, pseudoporphyria, and so on.[7] More studies are required to establish this concept.
What is new?
‘Acute syndrome of apoptotic pan-epidermolysis (ASAP)’ is a unifying concept that encompasses all the life-threatening clinical situations of massive epidermal cleavage resulting from a hyperacute apoptotic injury.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Torchia D, Romanelli P, Kerdel FA. Erythema multiforme and Stevens-Johnson syndrome/toxic epidermal necrolysis associated with lupus erythematosus. J Am Acad Dermatol. 2012;67:417–21. doi: 10.1016/j.jaad.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 2.Cisneros CG, Romiti R, Santi CG, Aoki V, Valente NY, Nico MM. Toxic epidermal necrolysis-like cutaneous lupus erythematosus: A series of three patients. Acta Derm Venereol. 2010;90:175–8. doi: 10.2340/00015555-0785. [DOI] [PubMed] [Google Scholar]
- 3.Andrade F, Casciola-Rosen L, Rosen A. Apoptosis in systemic lupus erythematosus. Rheum Dis Clin North Am. 2000;26:215–27. doi: 10.1016/s0889-857x(05)70136-8. [DOI] [PubMed] [Google Scholar]
- 4.Maldelcorn R, Shear NH. Lupus-associated toxic epidermal necrolysis: A novel manifestation of lupus? J Am Acad Dermatol. 2003;48:525–9. doi: 10.1067/mjd.2003.107. [DOI] [PubMed] [Google Scholar]
- 5.Fritsch PO, Ruiz-Maldonaldo R. Stevens-Johnson syndrometoxic epidermal necrolysis. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitzpatrick's dermatology in general medicine. 5th ed. New York: McGraw-Hill; 1999. pp. 644–54. [Google Scholar]
- 6.Roujeau JC, Stern RS. Severe adverse cutaneous reactions to drugs. N Engl J Med. 1994;331:1272–85. doi: 10.1056/NEJM199411103311906. [DOI] [PubMed] [Google Scholar]
- 7.Ting W, Stone MS, Racila D, Scofield RH, Sontheimer RD. Toxic epidermal necrolysis-like acute cutaneous lupus erythematosus and the spectrum of the acute syndrome of apoptotic pan-epidermolysis (ASAP): A case report, concept review and proposal for new classification of lupus erythematosus vesiculobullous skin lesions. Lupus. 2004;13:941–50. doi: 10.1191/0961203304lu2037sa. [DOI] [PubMed] [Google Scholar]


