Sir,
Urticarial vasculitis is a disease characterized clinically by recurrent episodes of painful, persistent urticarial lesions with or without angioedema. Histologically, features of leukocytoclastic vasculitis are present. Herein we present an 11-year-old boy who developed urticarial vasculitis following 2 weeks of starting levetiracetam for seizures. Drug induced urticaria constitutes a rare etiology of urticarial vasculitis. Levetiracetam has been introduced recently and is supplanting the older antiepileptics. Its imputability has not been reported before among the drug responsible for urticarial vasculitis.
An 11-year-old boy suffering from autism spectrum disorders presented with a 10 day history of generalized pruritus and skin rash. He had been taking sodium valproate thrice a day for the last 4 years for epilepsy. Tab levetiracetam 250 mg twice a day was introduced 15 days before the appearance of symptoms. The urticarial wheals were persistent and enlarging in size. No history of fever, abdominal pain, joint pain or history of similar complains in the family was present.
Examination revealed multiple well defined dusky erythematous, annular and arciform urticarial wheals on the lower limbs [Figures 1 and 2] with no purpuric changes on diascopy. Apart from cutaneous involvement, the child was normal on systemic examination. Routine laboratory investigations including anti-nuclear antibodies and complement levels were within normal limits. Histopathology revealed features suggestive of small vessel vasculitis in the form of infiltration of vessel walls by neutrophils and eosinophils and endothelial cell swelling [Figure 3]. Levetiracetam was stopped and the patient was continued on sodium valproate. Patient was treated with a short course of oral corticosteroids (1 mg/kg) and non-sedating antihistaminics (fexofenadine), which resulted in complete resolution of the lesions in a week without any post-inflammatory hyperpigmentation following which the medicines were tapered and discontinued. Patient followed after 1 month and had no recurrence.
Figure 1.

Dusky erythematous urticarial wheals on the lower limb
Figure 2.

Annular urticarial wheals with dusky hue
Figure 3.
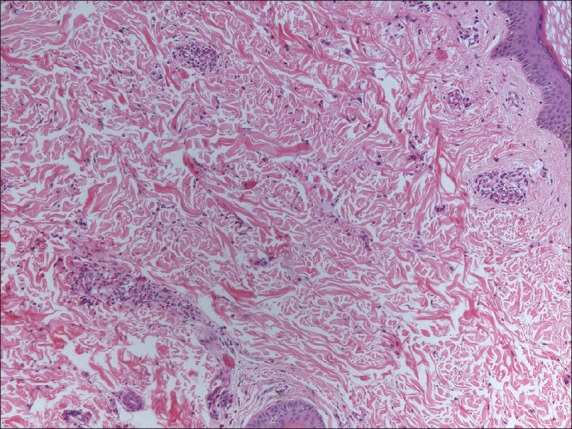
H and E stain, (×100) - Endothelial cell swelling along with neutrophilic and eosinophilic infiltration of the vessel walls
Urticarial vasculitis is a clinicopathologic entity consisting of urticarial lesions which demonstrate features of leukocytoclastic vasculitis on histology. In 1973, McDuffie recognized the hypocomplementemic form of this disease comprising low serum complement levels, arthritis, cutaneous vasculitis, in addition to other features resembling systemic lupus erythematosus.
Drugs commonly reported to induce urticarial vasculitis include cimetidine, diltiazem, potassium iodide, fluoxetine, non-steroid inflammatory drugs and glatiramer acetate.[1]
The cutaneous symptoms may include urticarial lesions persisting longer than 24 h, pronounced central clearing of lesions, purpura and residual hyperpigmentation following resolution. As the clinical characteristics of urticarial vasculitis may overlap with those of allergic urticaria, confirmation of the diagnosis requires a lesional skin biopsy.
Levetiracetam is a broad-spectrum antiepileptic that has been shown to be effective for a variety of seizures in adults and children.[2] The literature includes very few case reports exhibiting cutaneous drug reactions following levetiracetam use. Beswick et al. reported a dose-related reticular eruption with levetiracetam in a 46-year-old woman with malignant brain tumor.[3] In a study carried out in 1890 out-patients, 2.8% had developed rash with the use of antiepileptic drugs. Maculopapular cutaneous side-effects were observed in 0.6% of the patients who had used levetiracetam.[4] A case of erythema multiforme following 2 weeks of levetiracetam therapy was reported in a 27-year-old female by Yesilova et al.[5] DRESS, SJS/TEN, ecchymoses, edema and bullous pemphigoid due to the drug have also been reported.[6,7,8,9]
Levetiracetam is considered to be effective, well-tolerated and safe in patients with epilepsy and other medical conditions that are difficult to manage in view of the serious adverse effects occurring with the aromatic anticonvulsant group of drugs. Due to the probable amplified use in the future, vigilant surveillance and assessment of the safety of levetiracetam is the requisite. Our primary goal is to exemplify our recent observation of urticarial vascultis with levetiracetam, which has not been reported to date and stimulate the readers to keep in mind while evaluating a case of urticarial vasculitis in patients on anti-epileptics.
References
- 1.Cicek D, Kandi B, Oguz S, Cobanoglu B, Bulut S, Saral Y. An urticarial vasculitis case induced by glatiramer acetate. J Dermatolog Treat. 2008;19:305–7. doi: 10.1080/09546630801961067. [DOI] [PubMed] [Google Scholar]
- 2.Crepeau AZ, Treiman DM. Levetiracetam: A comprehensive review. Expert Rev Neurother. 2010;10:159–71. doi: 10.1586/ern.10.5. [DOI] [PubMed] [Google Scholar]
- 3.Beswick TC, Cohen JB. Dose-related levetiracetam-induced reticulated drug eruption. J Drugs Dermatol. 2010;9:409–10. [PubMed] [Google Scholar]
- 4.Arif H, Buchsbaum R, Weintraub D, Koyfman S, Salas-Humara C, Bazil CW, et al. Comparison and predictors of rash associated with 15 antiepileptic drugs. Neurology. 2007;68:1701–9. doi: 10.1212/01.wnl.0000261917.83337.db. [DOI] [PubMed] [Google Scholar]
- 5.Yesilova Y, Turan E, Sonmez A, Ozardali I. A case of erythema multiforme developing after levetiracetam therapy. Dermatol Online J. 2013;19:12. [PubMed] [Google Scholar]
- 6.Karadag AS, Bilgili SG, Calka O, Onder S, Kosem M, Burakgazi-Dalkilic E. A case of levetiracetam induced bullous pemphigoid. Cutan Ocul Toxicol. 2013;32:176–8. doi: 10.3109/15569527.2012.725444. [DOI] [PubMed] [Google Scholar]
- 7.Hawker K, Frohman E, Racke M. Levetiracetam for phasic spasticity in multiple sclerosis. Arch Neurol. 2003;60:1772–4. doi: 10.1001/archneur.60.12.1772. [DOI] [PubMed] [Google Scholar]
- 8.Gómez-Zorrilla S, Ferraz AV, Pedrós C, Lemus M, Peña C. Levetiracetam-induced drug reaction with eosinophilia and systemic symptoms syndrome. Ann Pharmacother. 2012;46:e20. doi: 10.1345/aph.1R084. [DOI] [PubMed] [Google Scholar]
- 9.Duong TA, Haddad C, Valeyrie-Allanore L, Sbidian E, Chosidow O, Wolkenstein P. Levetiracetam: A possible new inducer of toxic epidermal necrolysis and Stevens-Johnson syndrome in 2 cases. JAMA Dermatol. 2013;149:113–5. doi: 10.1001/2013.jamadermatol.266. [DOI] [PubMed] [Google Scholar]


