Abstract
OBJECTIVE
Primary care visits provide an opportunity to screen adolescents for substance use and offer early intervention. Little is known, however, about what follow-up plans primary care providers (PCPs) make for adolescent patients who screen positive. The objective of this study was to determine follow-up recommendations by PCPs and assess the relationship between their diagnostic impressions of substance use severity and plans for intervention.
METHODS
Data were collected through a prospective observational study conducted at 7 primary care practices in New England. Patients aged 12 to 18 years completed an interview, which included sociodemographic characteristics and the CRAFFT substance abuse screen. PCPs received screen results, noted their diagnostic impression of participants’ substance use severity, and recorded follow-up plans. Follow-up plans other than “periodic screening” alone were defined as “active intervention.” We examined the relationship of provider impressions with follow-up recommendations by using the χ2 test.
RESULTS
For the entire sample of 2034 adolescents, PCPs recommended no plan for 369 patients, periodic screening for 1557 patients, a return visit for 98 patients, and referral to counseling for 44 patients. PCPs’ diagnostic impressions identified 97 (4.8%) patients with problem use and 19 (0.01%) patients with abuse or dependence. Recommendations for active intervention were more likely with patients’ higher severity of use. However, 1 in 5 patients thought to have problem use did not receive a recommendation for an active intervention. Parent notification was planned for only 13 patients.
CONCLUSIONS
When concerned about substance use, PCPs recommend to patients a return visit to their office more than twice as often as referral to counseling, and they seldom plan to inform parents of adolescents’ substance use. PCPs need greater opportunities for training in the delivery of medical office–based therapeutic interventions and in strategies for managing adolescent substance use in the outpatient setting.
Keywords: adolescence, substance abuse, treatment recommendations
Substance use among adolescents is a serious national problem and associated with significant morbidity and mortality. According to the National Survey on Drug Use and Health, 28% of adolescents (12–20 years of age) reported drinking alcohol and 19% reported heavy episodic drinking (also known as “binge drinking”) during the past month.1 Among adolescents aged 12 to 17 years, 9.8% are estimated to be current users of illicit drugs, with 4.9% using drugs other than marijuana.1 Nearly three quarters of students have started to drink alcohol and nearly half (47%) have tried using an illicit drug (not including alcohol or tobacco) by the senior year of high school.2
Adolescents who begin using alcohol or drugs early have an increased risk of developing an addictive disorder later in life. A study by Hingson and colleagues3 found that, compared with those who start drinking at age 21 or older, adolescents who begin drinking at age 14 or younger have a fivefold increase in risk of developing alcoholism. Early onset of substance use is also associated with greater risk of driving after drinking, alcohol-related car crashes, physical fights after drinking, and other injuries.4–6 In addition, substance-abusing adolescents are at greater risk for unprotected sexual activity, depression, suicidal ideation, and poor school performance.7,8
Primary care providers (PCPs) are well positioned to screen for substance use in their patients and to facilitate intervention before use escalates or serious harm results. Although professional guidelines have recommended an annual screening for substance use as part of routine adolescent care,9–11 actual screening practices are inconsistent.12 The CRAFFT (an acronym for key components in the questions: car, relax, alone, forget, friends, trouble) screen is one of several tools validated for adolescents.13,14 A CRAFFT total score of ≥2 is considered a positive screen and indicates a need for additional assessment and therapeutic intervention. Many adolescents who screen positive can be managed effectively in the primary care office. Adolescents who are found to have alcohol or drug dependence and those who repeatedly engage in substance-related high-risk behaviors (eg, repeated driving while intoxicated) require referral to more intensive substance abuse treatment.
Although evidence-based recommendations for the assessment and care of adolescents with substance use problems exist,15 little is known about which treatment options providers typically recommend to their patients. The primary objective of this study was to assess PCPs’ follow-up recommendations for adolescents who use substances and examine how these follow-up plans relate to their diagnostic impressions of substance use severity. A secondary objective was to determine if particular demographic characteristics were associated with an increased likelihood of active interventions after adjusting for severity of substance use.
METHODS
Sample
The study method has been previously published16 and is summarized in brief here. This was a prospective observational study conducted within a network of 5 primary care settings in New England including (1) an urban hospital-based pediatric clinic, (2) a pediatric practice in a large health maintenance organization (HMO)-type group, (3) an urban hospital-based adolescent clinic, (4) a rural family medicine practice, and (5) 3 school-based clinics in urban public high schools.
Eligible participants were patients aged 12 to 18 years presenting for a visit with a medical provider between March 1, 2003, and August 31, 2005, and their PCPs. A total of 2301 patients were eligible during this time period and 2133 (93%) agreed to participate. Ten patients were excluded because of medical or emotional instability and 7 because of language problems. Participation rates were similar across practices except for the HMO, which was slightly lower (84.3% vs 95.5%; P < .001).
Procedures
A research assistant (RA) approached eligible patients in the waiting room before their medical visit. Those who expressed interest received an explanation of the purpose and procedures of the study in a private area. Informed assent/consent was obtained. The survey instrument consisted of 8 sociodemographic questions including date of birth, gender, school grade, number of parents living at home, highest level of education completed by their parent(s), race/ethnicity, reason for visit (well, sick, follow-up, or “other” such as confidential testing), and patient status (new or established patient). The RA verbally administered the sociodemographic questions followed by the lifetime substance abuse question (Have you ever used alcohol or drugs?) and the 6-item CRAFFT screen. Responses were recorded by the RA. A subgroup of participants completed the CRAFFT screen directly on a computer (n = 222). Participants were informed that their medical provider would receive a report of their CRAFFT screening responses during their visit. Adolescent participants received $2 as compensation for their time.
PCPs were oriented to the purpose and procedures of the study during a 1-hour group meeting, and they provided written informed consent. Clinic directors were excluded from these meetings while consent was obtained to prevent any perception of coercion. Each provider received a $100 honorarium for attending the orientation meeting. During study implementation, providers were given a copy of the CRAFFT screen results before the medical visit and reviewed the screen with the patient during the visit as they felt appropriate. The providers then completed a 2-item questionnaire in which they noted their diagnostic impression with regard to substance use (no use, occasional use, problem use, abuse, or dependence) and follow-up plan (none, periodic screening, notify parents, return visit with PCP, referral for counseling, and other). Providers could recommend multiple strategies. There were no specific policies regarding substance abuse counseling or reimbursement for screening and counseling in any of the medical settings. The Children’s Hospital Boston, Committee on Clinical Investigations along with the institutional review boards at each participating site approved the study design and protocol and granted a waiver of the requirement for parental consent for adolescents <18 years of age.
Data Analysis
Ninety-nine participants were not included in final data analysis because of missing provider information, resulting in a final sample of 2034 participants. Compared with those with complete provider information, participants with incomplete provider information were more likely to be white (61% vs 48%; P < .001) and to have a positive CRAFFT screen (29% vs 14%; P < .001), but they did not differ significantly with regard to age, gender, or parent educational level.
Because providers could choose multiple follow-up plans for a patient, recommendations were collapsed into 3 mutually exclusive categories: no plan only, periodic screen only, and active intervention. Active intervention was defined as any plan beyond periodic screening including notification of parents, referral to counseling, return visit with the PCP, or noting that the patient was already in counseling for substance use.
We examined the relationship of PCPs’ impressions of their patients’ substance use severity with their follow-up recommendations using the χ2 test. To assess the association between patient demographic characteristics and provider likelihood of recommending an active intervention, we used binary logistic regression analyses to generate adjusted odds ratios (aORs) and 95% confidence intervals (CIs), controlling for potential confounders such as CRAFFT screen status.
RESULTS
The study sample (N = 2034) was 56.6% female and 48.1% non-Hispanic white. The mean age was 15.7 years. The majority of participants were established patients (91.8%) coming in for well-care visits (68.4%). Less than 7% of participants had parent(s) who had not graduated from high school. Thirty-six percent of the sample was from the hospital-based pediatric clinic, 24.2% from the hospital-based adolescent clinic, 22% from the HMO, 12.4% from the rural-based family practice, and 5.3% from the school-based health centers. Overall, 14.1% of adolescent participants screened positive on the CRAFFT screen with a score of ≥2.
Recommendation for Follow-up Plan
Table 1 presents the proportion of providers recommending each type of follow-up plan, for each diagnostic impression group and for the entire sample.
TABLE 1.
Distribution of Provider Follow-up Plans by Impression of Substance Use Severity (N = 2034)
| n (%) | No Plan (N = 369), % | Periodic Screen (N = 1557), % | Notify Parents (N = 13), % | Return Visit (N = 98), % | Counseling (N = 44), % | Already in Counseling (N = 32), % | Declined Referral (N = 8), % | |
|---|---|---|---|---|---|---|---|---|
| Diagnostic impression | ||||||||
| No use | 1544 (75.9) | 22.1 | 77.4 | 0.1 | 0.6 | 0.3 | 0.2 | 0.0 |
| Occasional use | 374 (18.4) | 7.5 | 84.8 | 1.3 | 7.2 | 3.7 | 1.9 | 0.5 |
| Problem use | 97 (4.8) | 0.0 | 43.3 | 6.2 | 54.6 | 22.7 | 13.4 | 6.2 |
| Abuse and dependence | 19 (.01) | 0.0 | 15.8 | 5.3 | 42.1 | 21.1 | 47.4 | 0.0 |
P < .001 for all categories.
Providers identified 374 (18.4%) adolescents with occasional substance use, 97 (4.8%) with problem use, and 19 (.01%) with a diagnosis of substance abuse or dependence. The most frequently recommended intervention for those with problem use was return visit with PCP (54.6%), which was recommended more than twice as often as the next most frequent option, referral to counseling (22.7%). A substantial proportion of those with abuse or dependence diagnoses were already receiving counseling (47.4%), another 21.1% were referred to counseling, and 42.1% were scheduled for return visits with the PCP. No patients with abuse or dependence declined a referral to counseling. Providers very seldom planned to notify parents about substance use. Parent notification was recommended for only 13 of the 490 patients who reported using alcohol or drugs. Nine of the 13 recommendations came from 1 site (the urban hospital-based pediatric clinic), and of these, 5 were from the same provider. Of the 13 patients for whom the provider planned to notify parents, the majority were established patients (92%), non-Hispanic white (77%), and had CRAFFT-positive screens (77%).
Table 2 presents the proportion of providers recommending no plan only, periodic screen only, or active intervention for each category of substance use severity.
TABLE 2.
Distribution of Provider Follow-up Plan Using Collapsed Mutually Exclusive Categories
| No Plan Only (N = 358), % | Periodic Screen Only (N = 1500), % | Active Intervention (N = 161), % | |
|---|---|---|---|
| Diagnostic impression | |||
| No use | 21.5 | 77.4 | 1.0 |
| Occasional use | 7.6 | 79.1 | 13.3 |
| Problem use | 0.0 | 19.6 | 80.4 |
| Abuse and dependence | 0.0 | 5.3 | 94.7 |
P < .001 for all categories.
Providers recommended an active intervention for 80.4% of those classified with problem use and 94.7% of those classified with abuse or dependence. However, providers did not recommend an active intervention for almost 1 in 5 participants (19.6%) believed to have problem use. These participants were significantly older (95% ≥16 years of age; P=.04), arriving for well-care visits (73.7%; P = .037), and tended to have CRAFFT-positive screens (68.4%; P = .066).
Associations Between Patient Characteristics and Likelihood of an Active Intervention Recommendation
We conducted analyses to determine which sociodemographic characteristics were predictive of an active intervention recommendation specifically among those in need of additional evaluation, ie, those with a CRAFFT-positive screen (Table 3). The type of visit was a significant independent predictor in this group. Participants who came in for sick, follow-up, or other visits were significantly more likely to receive an active intervention recommendation compared with those coming for a well visit. In addition, the hospital-based adolescent clinic had significantly lower odds compared with the urban hospital-based pediatric clinic. There were marginal effects for patient status and Asian race with new patients having higher odds of being recommended an active intervention compared with established patients, and Asian youth having lower odds compared with youth of other races.
TABLE 3.
Odds Ratio (With 95% CIs) of Receiving an Active Intervention Recommendation for Those Screening CRAFFT Positive (N = 287)
| aOR (95% CI) | P | |
|---|---|---|
| Age, y | ||
| <15 | Ref (≤15) | |
| ≥16 | 0.5 (0.2–1.0) | .656 |
| Gender | ||
| Male | Ref | |
| Female | 0.8 (0.4–1.6) | .592 |
| Race | ||
| White | Ref | |
| Black | 1.3 (0.5–3.6) | .574 |
| Hispanic | 1.1 (0.3–4.1) | .868 |
| Asian | 0.3 (0.1–1.1) | .073 |
| Other | 0.9 (0.3–2.5) | .777 |
| Parent education | ||
| Not high school graduate | Ref | |
| High school graduate | 1.1 (0.4–3.2) | .915 |
| College graduate | 0.7 (0.2–2.3) | .578 |
| Parents at home | ||
| 2 | Ref | |
| 1 | 1.0 (0.5–2.0) | .988 |
| None/foster | 1.0 (0.2–5.5) | .985 |
| Type of visit | ||
| Well | Ref | |
| Follow-up | 3.7 (1.5–9.3)a | .005a |
| Sick | 5.8 (2.2–15.1)a | .000a |
| Other | 5.4 (1.3–22.6)a | .020a |
| Patient status | ||
| Established patient | Ref | |
| New patient | 3.4 (0.9–12.8) | .066 |
| Medical site | ||
| Urban hospital-based pediatric clinic | Ref | |
| HMO | 1.0 (0.3–3.1) | .968 |
| Urban hospital-based adolescent clinic | 0.3 (0.1–0.8)a | .014a |
| Family medicine practice | 0.6 (0.2–1.8) | .37 |
| School-based clinic | 0.7 (0.2–3.1) | .644 |
Adjusted model controlling for age, gender, race, parent educational level, number of parents at home, reason for visit, status of patient at time of visit, and medical site. Age was collapsed into 2 variables (<16 and ≥16 years of age) because of only 1 positive CRAFFT screen in the <14-year-old category.
Significant associations.
When analyzing the entire study sample, CRAFFT screen status was, as expected, a powerful predictor of providers recommending an active intervention follow-up with those screening CRAFFT-positive having significantly greater odds of receiving this recommendation when compared with those with a negative screen (aOR: 61 [95% CI: 33.0–112.6] P < .001).
Similar to the CRAFFT-positive group, type of visit was also a significant independent predictor of an active intervention. In addition, both Asian participants and those seen at the hospital-based adolescent clinic had significantly lower odds of being recommended an active intervention compared with other race/ethnic groups or those attending other sites. Because the hospital-based adolescent clinic had the highest proportion of Asian participants (30.1% compared with <8% at any other site), additional analysis was conducted to disentangle the potential confounding between site and participant race/ethnicity. When analysis was restricted to data from just the hospital-based adolescent clinic, Asian participants at this site had a significantly lower odds of being recommended an active intervention compared with youth of other races (aOR: 0.06 [95% CI: 0.004–0.94] P = .045). When we analyzed data excluding this 1 site, Asian ethnicity was no longer a significant factor. Excluding Asian participants from the total sample, we found that the hospital-based adolescent clinic was still associated with a decreased likelihood of active intervention recommendations (aOR: 0.32 [95% CI: 0.14–0.77] P = .010).
Because the first question on the CRAFFT screen (Have you ever ridden in a car driven by someone including yourself who was ‘high’ or had been using alcohol or drugs?) might not reflect personal history of use and providers may therefore not recommend an active intervention, we analyzed the association between RAFFT (dropping the “car” item) scores and the likelihood of receiving an active intervention recommendation. One in 5 participants (21.1%, n = 430) had a RAFFT score of ≥1. Fig 1 presents the percentage of study participants receiving a recommendation for active intervention by RAFFT score.
FIGURE 1.
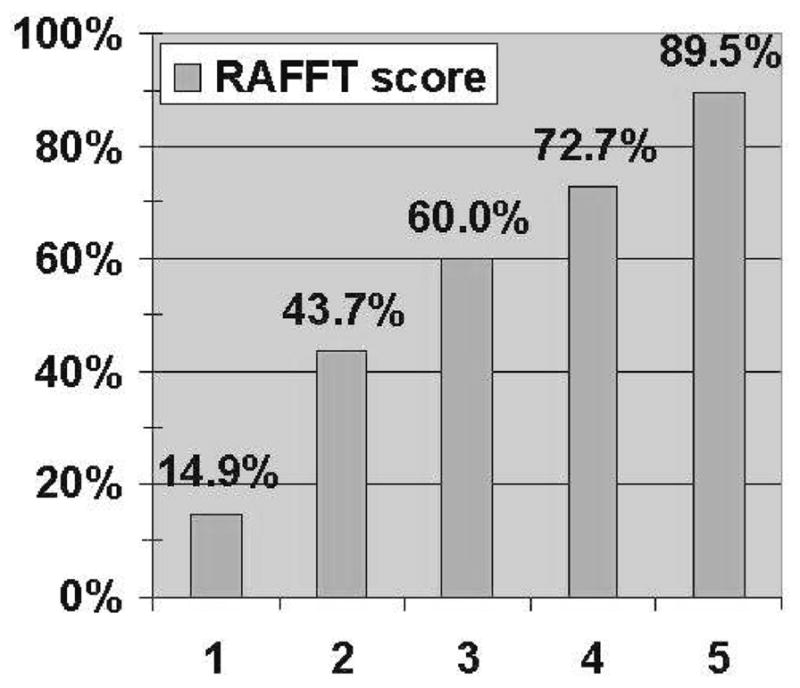
Percentage of RAFFT-positive patients with recommended active intervention.
A strong linear association (linear-by-linear χ2 = 846.56; P < .001) is noted with providers recommending a higher percentage of active intervention for those with higher scores. Among those with a RAFFT score of 1, there were similar odds of an active intervention recommendation regardless of which RAFFT item was positive.
DISCUSSION
This study is among the first to assess PCPs’ follow-up recommendations for adolescent patients with problematic substance use. We found that providers are more likely to recommend active intervention for patients they believe have a higher severity of use, with 95% of teens with abuse or dependence receiving such recommendations. However, there were still 1 in 5 patients with problem use who did not receive a recommendation for active intervention. PCPs seldom plan to notify parents of adolescents’ substance use. The frequency of return clinic visits and the lack of parental involvement may place more burden for substance use treatment on the PCP.
In previous analysis of this study data set, 1 in 7 teens were found to screen positive for substance use.16 The true prevalence may be even higher given that substance-using youth are less likely to present to physicians for routine visits, universal screening is not always implemented, and concerns regarding confidentiality may lead to underreporting. There is a dearth of research regarding provider assessment and recommendations for substance use intervention for adolescent patients. Providers may not recommend an active intervention if they have not received training in substance use screening, assessment, and referral to treatment or in how to manage a positive screen.17 Similarly, providers may be faced with a lack of substance abuse treatment resources in their communities, they may encounter insurance problems, or have difficulty finding available specialists.
Issues of adolescent confidentiality may also play a role in providers’ follow-up recommendations. Extensive research documents the importance of confidentiality in promoting adolescent’s access to health care, particularly for issues such as substance use.18,19 Most professional medical organizations support confidential care for adolescents for a broad range of services including substance use. The provision of confidential health care to teens is also influenced by federal and state law, court decisions, and insurance disclosure policies. Many adolescents who seek care may request that their parents not be notified of their substance use. Providers may be hesitant to make referrals, because it is difficult to schedule intake and counseling appointments for adolescent patients without breaking confidentiality and communicating their concern with parents. For many patients, insurance companies send explanation of benefit forms indicating the type of treatment provided, and this potentially breeches adolescents’ confidentiality when the insurance subscriber is the parent. Consequently, providers may resort to recommending return visits as the most accessible and confidential method for managing an adolescent’s substance use.
In this study, visits at the adolescent hospital-based clinic were associated with lower odds of active intervention. It is possible that because providers in this setting are adolescent-trained specialty physicians, they may have a higher comfort level in working with substance-using youth and may not view problems as being sufficiently concerning to merit treatment outside the practice. Asian ethnicity was also associated with lower odds of the provider recommending an active intervention, particularly among those screening positive on the CRAFFT. Current research examining how provider recommendations for substance use follow-up may vary by patients’ race or ethnicity is sparse, and more research is needed in this area.
Previous literature suggests that providers are better able to identify substance use during well visits rather than urgent care appointments.20 Interestingly, we found that follow-up, sick, or other visits were associated with higher odds of provider recommendations for active intervention compared with well-care visits. One possible explanation is that youth with problematic substance use may miss their health maintenance visits and instead present with acute problems that may or may not be related to their substance use. Regardless, this finding suggests that providers will miss opportunities to provide appropriate substance use interventions if substance use screening is limited to well visits.
This study has several strengths. The study had a large sample size and high participation rate. Adolescents were not required to seek parental consent, minimizing the likelihood of self-selection bias. Despite the small number of health care settings and restricted geographic area, these findings may still have a wider applicability and generalizability because of the variety of health care populations and settings that we studied. We included urban, rural, and suburban youth from diverse socioeconomic and ethnic backgrounds. In addition, study sites represented a mix of private practice, school-based, and hospital settings and also varied by specialty including general pediatrics, family practice, and adolescent/young adult medicine. Primary care providers also came from diverse training backgrounds and included family practitioners, pediatricians, physicians trained in adolescent medicine, nurse practitioners, and physician assistants. There are several potential limitations. The study relied on adolescents self-reported answers to survey questions, which were used to help providers formulate an assessment; self-report, however, has been shown to be a reliable means of measuring substance use.21 Our survey was cross-sectional, so we are unable to draw conclusions regarding any causal relationships. In this study, the CRAFFT screen was prefaced with a question meant to detect lifetime substanceuse (Have you ever used alcohol or drugs?). The CRAFFT results may not have been representative of participants’ current (past 12 months) use of drugs and alcohol. PCPs may have explored the adolescent’s current use, which could impact their diagnosis as well as follow-up plan recommendation. Finally, although there were only 13 recommendations for parental notification, there were likely a larger number of parents aware or who had been previously notified of their child’s substance use, given that 34 patients were already in counseling at the time of their visit.
CONCLUSIONS
Adolescents with problematic substance use, abuse, and dependence constitute a significant population at risk for health-related and psychosocial consequences. Providers should screen adolescents for substance use whenever there is an opportunity, including urgent care, return visits, and well care. Providers seem to prefer arranging follow-up care at their own offices for adolescents who screen positive, and they rarely notify parents. Given these findings, it is crucial that programs be developed to educate and train PCPs in effective substance abuse counseling strategies that can be implemented during an office visit. In addition, more understanding is needed of the role that parents can and should play in substance abuse treatment. Additional research should examine reasons why providers choose to use return visits over other options such as school-based drug counseling programs, outpatient substance abuse clinics, day treatment programs, and inpatient residential programs. Finally, future research should also determine if adolescents follow through with their PCP’s recommendation to return for a follow-up visit to further address substance use.
WHAT’S KNOWN ON THIS SUBJECT
PCPs are well positioned to screen their adolescent patients for substance use and facilitate intervention before serious harm results. To our knowledge; little is known about which treatment options providers typically recommend for patients who screen positive.
WHAT THIS STUDY ADDS
We found that providers prefer arranging follow-up care at their own offices for adolescent patients with problematic substance use and rarely notify parents. These findings point to a need for developing programs to train providers in effective substance abuse counseling strategies.
Acknowledgments
This study was supported by grant 45222 from the Robert Wood Johnson Foundation and grant T71 MC00009 from the Maternal and Child Health Bureau (Leadership in Adolescent Health Training). Other support was provided by grant K07 AA013280 from the National Institute on Alcohol Abuse and Alcoholism (Dr Knight), and grant 5T20MC000-11-06 (Ms Hook, Dr Knight) from the Maternal and Child Health Bureau.
We thank the physicians and staff of the New England Partnership for Substance Abuse Research for assistance with study implementation, including Kathleen Kelley, MBA; Jeanne McBride, RN, BSN, MM (quality improvement project manager, UMMHC Department of Family Medicine and Community Health; Irene Phelps, RN, BSN); Judy Shaw, RN, MPH (executive director, Vermont Child Health Improvement Program); Donald H. Taylor, III (MIT); and Colleen Sheppard, RN, BSN (Department of Pediatrics and Adolescent Medicine, Tufts-New England Medical Center). We also thank S. Jean Emans, MD, and Heather Corliss, PhD, for thoughtful reviews of the manuscript and Jonathan Mansbach, MD, Susan Gray, MD, and Catherine Gordon, MD, for invaluable input.
ABBREVIATIONS
- PCP
primary care provider
- HMO
health maintenance organization
- RA
research assistant
- aOR
adjusted odds ratio
- CI
confidence interval
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
References
- 1.Substance Use and Mental Health Services Administration. Results From the 2006 National Survey on Drug Use and Health: National Findings. Washington, DC: Department of Health and Human Services; 2007. [Google Scholar]
- 2.National Institute on Drug Abuse. Monitoring the Future: National Results on Adolescent Drug Use. Washington, DC: National Institute on Drug Abuse; 2008. [Google Scholar]
- 3.Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence: age at onset, duration, and severity. Arch Pediatr Adolesc Med. 2006;160(7):739–746. doi: 10.1001/archpedi.160.7.739. [DOI] [PubMed] [Google Scholar]
- 4.Hingson R, Heeren T, Levenson S, Jamanka A, Voas R. Age of drinking onset, driving after drinking, and involvement in alcohol related motor-vehicle crashes. Accid Anal Prev. 2002;34(1):85–92. doi: 10.1016/s0001-4575(01)00002-1. [DOI] [PubMed] [Google Scholar]
- 5.Hingson R, Heeren T, Zakocs R. Age of drinking onset and involvement in physical fights after drinking. Pediatrics. 2001;108(4):872–877. doi: 10.1542/peds.108.4.872. [DOI] [PubMed] [Google Scholar]
- 6.Hingson RW, Heeren T, Jamanka A, Howland J. Age of drinking onset and unintentional injury involvement after drinking. JAMA. 2000;284(12):1527–1533. doi: 10.1001/jama.284.12.1527. [DOI] [PubMed] [Google Scholar]
- 7.Fergusson DM, Horwood LJ, Swain-Campbell N. Cannabis use and psychosocial adjustment in adolescence and young adulthood. Addiction. 2002;97(9):1123–1135. doi: 10.1046/j.1360-0443.2002.00103.x. [DOI] [PubMed] [Google Scholar]
- 8.Patton GC, Coffey C, Carlin JB, Degenhardt L, Lynskey M, Hall W. Cannabis use and mental health in young people: cohort study. BMJ. 2002;325(7374):1195–1198. doi: 10.1136/bmj.325.7374.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Green M, editor. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. Arlington, VA: National Center for Education in Maternal and Child Health; 1994. [Google Scholar]
- 10.Kulig JW. Tobacco, alcohol, and other drugs: the role of the pediatrician in prevention, identification, and management of substance abuse. Pediatrics. 2005;115(3):816–821. doi: 10.1542/peds.2004-2841. [DOI] [PubMed] [Google Scholar]
- 11.Elster AB, Kuznets NJ, editors. AMA Guidelines for Adolescent Preventive Services (GAPS) Baltimore, MD: Williams & Wilkins; 1994. [Google Scholar]
- 12.American Academy of Pediatrics. Periodic Survey of Fellows #31: Practices and Attitudes Toward Adolescent Drug Screening. Elk Grove Village, IL: American Academy of Pediatrics, Division of Child Health Research; 1997. [Google Scholar]
- 13.Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch Pediatr Adolesc Med. 2002;156(6):607–614. doi: 10.1001/archpedi.156.6.607. [DOI] [PubMed] [Google Scholar]
- 14.Knight JR, Sherritt L, Harris SK, Gates EC, Chang G. Validity of brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE and CRAFFT. Alcohol Clin Exp Res. 2003;27(1):67–73. doi: 10.1097/01.ALC.0000046598.59317.3A. [DOI] [PubMed] [Google Scholar]
- 15.American Academy of Child and Adolescent Psychiatry. Practice Parameter for the Assessment and Treatment of Children and Adolescents With Substance Use Disorders. Washington, DC: American Academy of Child and Adolescent Psychiatry; 2004. [DOI] [PubMed] [Google Scholar]
- 16.Knight JR, Harris SK, Sherritt L, et al. Prevalence of positive substance abuse screens among adolescent primary care patients. Arch Pediatr Adolesc Med. 2007;161(11):1035–1041. doi: 10.1001/archpedi.161.11.1035. [DOI] [PubMed] [Google Scholar]
- 17.Van Hook S, Harris SK, Brooks TL, et al. The “six T’s”: barriers to screening teens for substance abuse in primary care. J Adolesc Health. 2007;40(5):456–461. doi: 10.1016/j.jadohealth.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Ford CA, Millstein SG, Halpern-Felsher BL, Irwin CE., Jr Influence of physician confidentiality assurances on adolescents’ willingness to disclose information and seek future health care. A randomized controlled trial. JAMA. 1997;278(12):1029–1034. [PubMed] [Google Scholar]
- 19.Thrall JS, McCloskey L, Ettner SL, Rothman E, Tighe JE, Emans SJ. Confidentiality and adolescents’ use of providers for health information and for pelvic examinations. Arch Pediatr Adolesc Med. 2000;154(9):885–892. doi: 10.1001/archpedi.154.9.885. [DOI] [PubMed] [Google Scholar]
- 20.Wilson CR, Sherritt L, Gates E, Knight JR. Are clinical impressions of adolescent substance use accurate? Pediatrics. 2004;114(5) doi: 10.1542/peds.2004-0098. Available at: www.pediatrics.org/cgi/content/full/114/5/e536. [DOI] [PubMed] [Google Scholar]
- 21.Winters KC, Stinchfield RD, Henly GA, Schwartz RH. Validity of adolescent self-report of alcohol and other drug involvement. Int J Addict. 1990;25(11A):1379–1395. doi: 10.3109/10826089009068469. [DOI] [PubMed] [Google Scholar]


