Abstract
Objective. The aim of the study was to compare the informational needs of patients with ANCA-associated vasculitis (AAV).
Methods. We developed a Vasculitis Informational Needs Questionnaire that was distributed to members of Vasculitis UK (VUK) by mail and registrants of the Vasculitis Clinical Research Consortium (VCRC) online registry with self-reported AAV. Patients were asked to use a 5-point scale (1 = not important, 5 = extremely important) to rank aspects of information in the following domains: disease, investigations, medication, disease management and psychosocial care. The source and preferred method of educational delivery were recorded.
Results. There were 314 VUK and 273 VCRC respondents. Respondents rated information on diagnosis, prognosis, investigations, treatment and side effects as extremely important. Information on patient support groups and psychosocial care was less important. There was no difference in the ratings of needs based on group, sex, age, disease duration, disease or method of questionnaire delivery. The most-preferred methods of providing information for both groups were by a doctor (with or without written material) or web based; educational courses and compact disc/digital video disc (CD/DVD) were the least-preferred methods.
Conclusion. This study demonstrates that people with AAV seek specific information concerning their disease, treatment regimes and side effects and the results of investigations. Individuals preferred to receive this information from a doctor. Patients with AAV should be treated in a similar manner to patients with other chronic illnesses in which patient education is a fundamental part of care.
Keywords: ANCA-associated vasculitis, granulomatosis with polyangiitis, eosinophilic granulomatosis with polyangiitis, microscopic polyangiitis, vasculitis, informational needs questionnaire
Introduction
Rare diseases such as ANCA-associated vasculitis (AAV) pose many challenges to both health care professionals and patients, with both groups commonly knowing little about individual rare conditions [1]. A disease is considered by the European Commission to be rare if it has a population prevalence of <5 in 10 000 [2]. There are approximately 7000 diseases classified as rare. Approximately 80% of rare diseases are genetic and present in childhood. However, a number of rare rheumatic conditions develop later in life, such as some vasculitides, scleroderma and myositis. Many of these conditions are chronic and it is well established that patient education is a key component in the management of many chronic diseases and a cornerstone of good quality care [3–5]. Provision of high-quality information can empower patients to become active partners in the management of their conditions [6–8], reduce anxiety and improve satisfaction with care [9, 10].
Patient education programmes have been developed in other long-term rheumatic conditions such as SLE and RA [11]. Development of an education resource for patients with SLE was found to have a positive effect on the patient’s level of knowledge [12]. In RA, patient education is well established and several questionnaires have been developed to assess patient knowledge [13, 14]. People who understand their illness and participate in developing their treatment plans have improved outcomes of care [15]. Thus educational programmes in common diseases such as RA and SLE can influence patient outcome and self-efficacy.
For patients with a rare disease, there are many fewer educational resources. Patients with chronic disease often need to follow complex treatment regimens. A survey carried out by Rare Disease UK of approximately 600 patients and families looking at the experience of living with a rare condition, with representation of 100 different rare conditions, found significant shortcomings in respondents’ education about their disease [16]. Fifty-two per cent of respondents felt they had not received sufficient information about their condition and 37% reported having no one to contact regarding questions about their illness.
AAV is typical of several rare rheumatic conditions and thus offers a good template to explore the educational and informational needs of patients with an acquired rare disease. There are three types of AAV: granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA) and eosinophilic granulomatosis with polyangiitis (EGPA). AAV has a prevalence of 2/10 000 [17]. Advances in therapy have transformed the survival rates of these diseases from having a poor prognosis to now routinely being a chronic relapsing condition.
In a recent review of the long-term outcome of the European Vasculitis Study Group (EUVAS) trials of new-onset AAV, the 1-year survival was 88%, 2 years was 85% and 5 years was 78% [18]. The major causes of death were active uncontrolled vasculitis in the early stage of disease, infection secondary to therapy [19] and cardiovascular disease during the chronic follow-up phase [20]. Even if patients survive the first year, they have a lifelong risk of relapse. Relapse occurs in up to 46% of patients treated with CYC, with relapses typically occurring in the first year after stopping therapy; 50% of patients with renal involvement relapse by 5 years [19]. Patients must often manage substantial burdens related to chronic illness and treatment-related side effects [21].
We have previously shown in an exploratory qualitative study using a combination of focus groups and one-on-one interviews that patients with AAV have significant informational requirements, necessitating information tailored to their specific needs and appropriate to their stage of illness [22]. Patients also reported difficulty in assimilating information when acutely ill.
Patients join support groups to gain peer support, participate in research and for access to novel therapies [23]. This is particularly true for rare diseases. Vasculitis UK (VUK), which is the main UK patient support group for patients with vasculitis, and patient members of the USA-based Vasculitis Clinical Research Consortium (VCRC) provide an excellent opportunity to explore the informational needs of patients with a rare condition. To provide tailored information for AAV, clinicians need to understand the patient’s information requirements and priorities.
The aim of the present study was to explore the informational needs of people with AAV as an example of a rare condition: e.g. what are the informational needs of patients with AAV; how do patients with AAV prioritize their informational needs; what sources of information are preferred and are there any differences in the informational needs of patients in the UK and USA?
Methods
Study design
We conducted surveys of the membership of two patient organizations using the Vasculitis Informational Needs Questionnaire (VINQ), developed through in-depth research with patient groups [22]. We surveyed members of VUK and we surveyed patient members of the VCRC Patient Contact Registry, who are predominantly based in the USA. Ethical approval for the study was provided by the Norfolk Research Ethics Committee (ref 07/Q0603/9) and by the University of South Florida Institutional Review Board for the VCRC e-mail survey (USF IRB Pro00006828).
VUK survey
Members of VUK were surveyed using the VINQ, which was distributed with the regular quarterly newsletter. A reminder invitation was not sent.
VCRC Contact Registry
Members of the VCRC Contact Registry were surveyed in March 2012 using an e-mail invitation where they log onto the VCRC website and then complete an online survey. The e-mail shot was repeated twice to non-responders after 3 and 6 weeks.
Participants
Members of VUK and the VCRC with a self-declared diagnosis of AAV were included. Respondents declaring other types of vasculitis, such as polyarteritis nodosa, IgA vasculitis (Henoch–Schönlein), GCA, Takayasu arteritis and Behçet’s disease, were excluded.
Questionnaire design and development
Searching Medline, EMBASE and Evidence-Based Medicine (EBM), we were unable to find a tool to assess the informational needs of people with AAV. One tool had been developed to assess the educational needs of patients with arthritis in general [Educational Needs Assessment Tool (ENAT)] [24] but was found to be too simplistic and was not useful in the assessment of AAV. Many of the questions were not suitable for patients with a rare and complex multisystem disease. An SLE tool [SLE Needs Questionnaire (SLENQ)] asks very little about diagnosis and treatment [25].
The informational needs of patients with cancer have been studied using survey methodology suitable for adaption for AAV. Many cancers share some features with AAV, e.g. in being serious, complex, potentially life-threatening illnesses requiring intensive immunosuppressive therapy.
The Toronto Informational Needs Questionnaire (TINQ-BC) is a validated and reliable self-administered questionnaire designed to elicit the informational needs of women with recently diagnosed breast cancer [26–28]. It has 52 items, grouped under five domains: disease, investigations, treatment, physical and psychosocial. The items are scored using a 5-point scale (1 = not important, 5 = extremely important). The TINQ-BC was shown to have internal consistency with a Cronbach’s alpha of 0.96 [26]. The questionnaire has been adapted for use in men with prostate cancer and colon cancer and has been shown to be reliable [29, 30].
We adapted the TINQ-BC for use in AAV as the VINQ. The first stage in the development of the VINQ was the generation of relevant questions [31]. Starting with the full set of items in the TINQ-BC, we removed those that were solely related to breast cancer (such as, did I need to wear a brassiere?). We then ensured that the themes from our qualitative study—reaction to diagnosis, the need for information on disease, investigations and treatment and access to knowledgeable practitioners—were represented in the VINQ. We also included items related to the subscales developed by Thorpe in the Vasculitis Self-Management Scale—namely medication, health services, infection, diet and exercise, symptom monitoring, reporting and adjusting activities [22, 32].
The content validity of the VINQ was established by asking doctors with expertise in the care of patients with vasculitis and a vasculitis specialist nurse to review the VINQ items for subject matter, use of language and patient understanding. The reviewers had not otherwise been involved in the design of the questionnaire. No further changes were made to the questionnaire at this stage.
The questionnaire was then pilot tested in 20 patients with AAV and the following questions were asked: how much time did it take to complete; were the instructions clear and easy to follow; were there any questions that were confusing; did you object to answering any questions; was the layout clear and attractive and any other comments?
Following the pilot test, the VINQ was modified to clarify the language and remove medical jargon, but no questions were either added or removed. The VINQ language and terms were slightly modified for use internationally, but these changes did not alter the content of the questions (e.g. leaflet was replaced with pamphlet, educational attainment levels were changed from the UK system to the US system, tick was changed to check and more options for ethnic origin were added) (see the VINQ supplementary data, available at Rheumatology Online).
The final version of the questionnaire used for the study has three main sections (see supplementary data, available at Rheumatology Online). The first is demographics, including age, gender, education status, diagnosis, time to diagnosis and disease duration from diagnosis. The second is informational needs. There are 33 items covering the following domains: disease, investigations, treatment and physical and psychosocial care. Respondents were asked to rank each using a 5-point scale (1 = not important, 2 = slightly important, 3 = moderately important, 4 = very important and 5 = extremely important). The stem question is, is it important for me to know. The 33 items are grouped by domain and can be found in supplementary data, available at Rheumatology Online. The third is the preferred mode of education delivery: written, by a health care professional, Internet, compact disc (CD) or group programme.
Statistical analysis
GPA, MPA and EGPA are treated and managed in very similar manners and have similar outcomes. We therefore chose to group these diseases together as AAV. The internal consistency of the questionnaire was determined using Cronbach’s alpha. Data were analysed using the Statistical Package for the Social Sciences (SPSS version 19.0; IBM, Armonk, NY, USA). The educational needs of patients with AAV were also compared with the reported needs of patients with breast cancer using the TINQ-BC [27, 28].
Results
Validation of the VINQ
The VINQ was assessed for internal consistency using Cronbach’s alpha, scoring 0.95, which indicated a high degree of internal consistency. There was also a high degree of consistency for each of the five domains (disease subscale 0.82, investigative tests 0.84, treatment 0.92, physical 0.83, psychosocial 0.90).
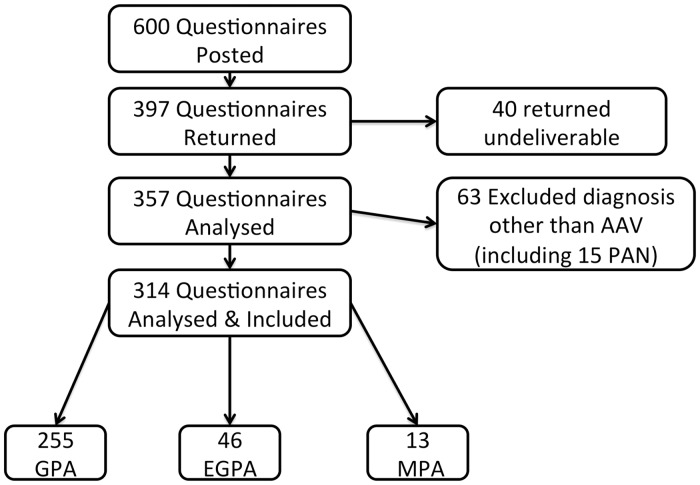
Six hundred questionnaires were posted to members of VUK. A total of 314 questionnaires were available for analysis (52% response rate). The flow chart in Fig. 1 shows the distribution of responses and the reasons for exclusion. An email message with a link to the questionnaire was distributed to 2740 registrants of the VCRC Patient Contact Registry, with two reminders sent to non-responders after 3 and 6 weeks.
Fig. 1.
Flow chart of patients from the Vasculitis UK survey
There were 387 (14.1% response rate) respondents from the VCRC, of whom 114 reported a diagnosis other than AAV and were a very heterogeneous group. The remaining 273 (10%) respondents from the VCRC with a diagnosis of AAV were included in the study.
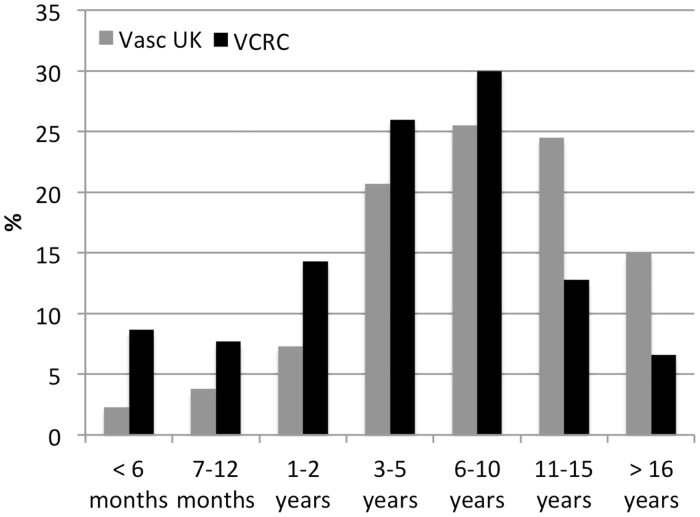
The demographic characteristics of both groups of respondents are shown in Table 1. The disease subtype distribution was representative of the whole survey population (data not shown here). VUK respondents were older than those from the VCRC, and the VCRC sample had a greater proportion of women than the VUK sample. The distribution of disease duration (self-reported date of diagnosis to date of questionnaire completion) is shown in Fig. 2 and is seen to be shorter in the VCRC group than the VUK group: 16.4% of the VCRC had a disease duration of <1 year compared with 6.1% of the VUK group. The VCRC respondents reported their origin as North American (86%) and European (12%).
Table 1.
Demographics of respondents in the Vasculitis UK and Vasculitis Clinical Research Consortium (VCRC) cohorts
| Vasculitis UK | VCRC | P-value | |
|---|---|---|---|
| Total respondents, n | 314 | 273 | |
| GPA, n (%) | 255 (81.2) | 193 (70.7) | 0.0034 |
| MPA, n (%) | 13 (4.1) | 21 (7.7) | 0.08 |
| EGPA, n (%) | 46 (14.6) | 59 (21.6) | 0.03 |
| Age, median (IQR), years | 63 (52–70) | 58 (49–64) | |
| Female, n (%) | 116 (36.9) | 184 (67.3) | <0.0001 |
| Self-reported ethnicity white, n (%) | 295 (93.9) | 265 (97.1) | 0.98 |
GPA: granulomatosis with polyangiitis; MPA: microscopic polyangiitis; EGPA: eosinophilic granulomatosis with polyangiitis; IQR: interquartile range.
Fig. 2.
Disease duration at the time of the survey for both the Vasculitis UK and Vasculitis Clinical Research Consortium (VCRC) groups
Educational attainment
In the VUK cohort, 118/314 (37.5%) were educated to school-leaving age (14–16 years depending on date of birth) without necessarily obtaining any qualifications, 121/314 (38.5%) had A levels or some further education but not to bachelor’s degree level and 53/314 (16.8%) had a bachelor’s degree or higher.
In the VCRC cohort, 32/273 (11.7%) were only educated to high school leaving or lower, 91/273 (33.3%) had received some further education but not to bachelor’s degree level and 154/273 (54.9%) were educated to bachelor’s degree level or higher.
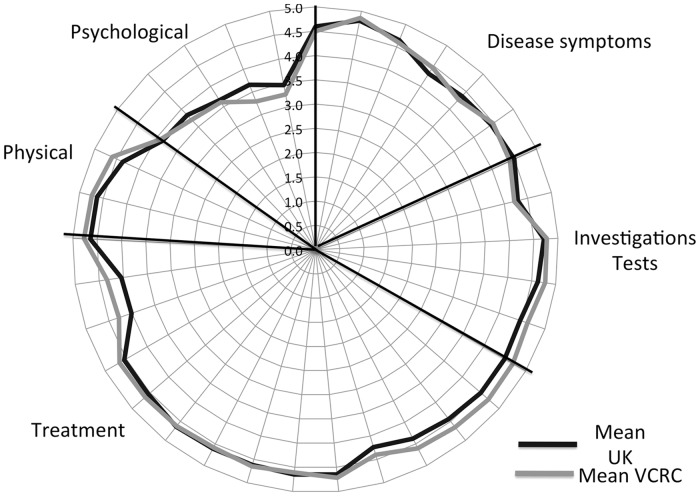
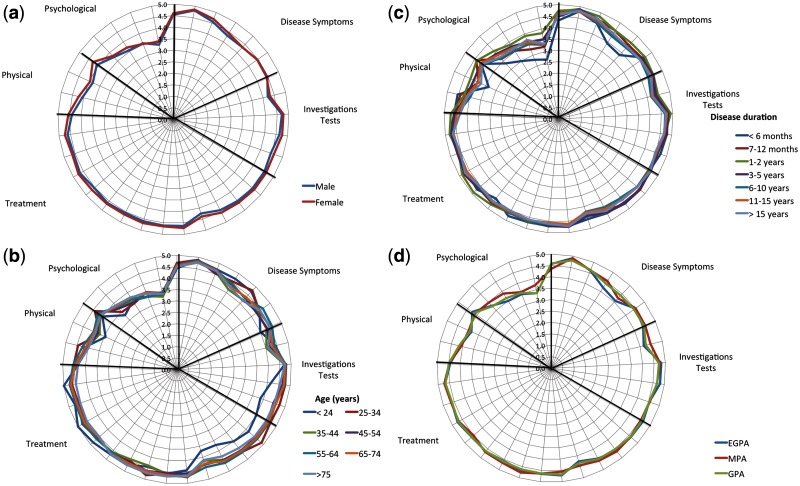
Informational needs
The informational needs of both groups of patients are high (Fig. 3), with all questions about specific needs scoring at least 3.0. The domains that were given most importance covered questions about disease diagnosis and management, with psychosocial aspects given least importance. There was no difference in the pattern of responses between the VUK and VCRC groups. There was no difference in informational needs by gender, age, disease duration or self-reported disease subtype (Fig. 4).
Fig. 3.
Informational needs of the Vasculitis Clinical Research Consortium (VCRC) and Vasculitis UK groups
Fig. 4.
Informational needs of the Vasculitis Clinical Research Consortium and Vasculitis UK groups combined
(a) Gender, (b) age at survey, (c) disease duration and survey and (d) AAV subtype.
We also compared the informational needs of patients with vasculitis with patients with cancer previously reported using the TINQ [27, 28]. Patients with vasculitis and cancer both required high levels of information, particularly the disease and treatment domains. For both groups, information about psychological aspects was much less desired (Table 2).
Table 2.
Toronto cancer informational needs and vasculitis informational needs mean scores by domain
| Subscale | TINQ, mean % | VINQ, mean % |
|---|---|---|
| Disease | 89.2 | 90.1 |
| Tests | 84.8 | 90.4 |
| Treatment | 88.9 | 92.0 |
| Physical | 80.8 | 86.0 |
| Psychological | 70.9 | 59.0 |
TINQ: Toronto Informational Needs Questionnaire; VINQ: Vasculitis Informational Needs Questionnaire.
Preferred source of information
Patients in both the VUK and VCRC groups were highly desirous that information be provided by a doctor and supported by written material. In the VUK the order of preference was doctor and written material, written material alone, doctor alone, Internet, group education, digital video disc (DVD), CD and 1–2 day course. In the VCRC group the order was Internet, doctor and written, doctor alone, written alone, education group, DVD, 1–2 day course and CD.
Discussion
This is the first study of the informational needs of patients with a rare chronic rheumatic disease and it makes a significant contribution to our knowledge about the education of patients with AAV. We adapted a cancer-specific informational needs questionnaire for use in AAV and demonstrated excellent survey reliability in two independent cohorts of patients. We showed that patients with AAV have significant informational needs that do not differ by country of origin, sex, age, disease duration or AAV subtype. We previously showed that many aspects of quality of life are impaired in AAV, with significant levels of depression and anxiety [21, 33–35]. Despite the psychological burden of disease associated with AAV, patients were relatively less interested in receiving information related to the psychological aspects of disease management, a finding that parallels the informational needs of patients with breast cancer [28]. It is possible that this reflects the questions asked in the VINQ and TINQ (see supplementary data, available at Rheumatology Online). Participants may be inhibited by the use of the word psychological; however, only one question directly asked about accessing psychological support. It is also possible that patients, by joining a group, are getting informal psychological support and therefore feel less need to know about the availability of other sources of such support; alternatively, group members may be more independent and may not need further support. Support was high on a list of desired features in a comprehensive needs assessment conducted prior to setting up a general arthritis education resource [36]. This should not be interpreted that these patients may not need psychological support.
These data support the need for patients with rare conditions to be educated in a similar manner to patients with more common chronic conditions, as both have very similar educational needs. Patients with long-term conditions such as AAV are encouraged to self-manage as much as possible. Thorpe et al. [32] recently explored some of the barriers to effective self-management and suggested that one of the barriers was lack of effective patient education, in particular, education about specific aspects of care. Successful self-management will only be achieved if patients have access to comprehensive and clear information. The provision of education and information poses particular challenges. At diagnosis, neither health care professionals nor patients may have access to much detailed information. The patient may feel isolated because friends and relatives to whom patients often turn for help are unlikely to have heard of the condition, given the lack of general awareness regarding many of these diseases. Health care professionals, unless working in the relevant subspecialty, may have limited understanding of the disease and may not be able to help patients understand and contextualize relevant information. Yet, physicians and nurses need to help patients understand information so that patients can internalize the information and contextualize what this might mean for them. Patients clearly expressed a desire for information to be provided by knowledgeable professionals, to whom access can be especially difficult. These deficits may be partly remedied by developing networks of professionals with expertise who can be called upon to provide advice. Recent guidelines have highlighted the need for patients with rare and complex conditions to be managed in networks so that all patients have equitable access to care [37, 38].
Patients with AAV consistently ranked information related to treatment as either very important or extremely important. This finding is relevant because a lack of understanding regarding medication regimens can lead to non-adherence and poor outcomes [39, 40]. A study in the USA found that patients with AAV had difficulty adhering to complex regimens and were slow to report symptoms and medication side effects [32]. An inpatient vasculitis education program in Germany showed that improvements in a patient’s knowledge of medications and side effects led to an increase in health-related quality of life [41].
There were significant differences in the educational level of the two cohorts. The UK cohort was much less likely to have been educated to degree level or above. This might reflect the median age of the VUK population of 63 years. This generation was relatively unlikely to go to university, with university intake at ∼10% of the age group. Despite educational differences, the two cohorts had similar informational needs, although delivery routes may need to be different. The VCRC cohort preference for delivery of information via the Internet likely reflects the conduct of the survey over the Internet and is consistent with other studies [42, 43].
This study has several potential weaknesses. Although the same questionnaire was used with both groups, it was administered differently to each. While the response rates differed, they were acceptable for the type of survey method [44]. It is noteworthy that we obtained quite similar results from both a written survey and an Internet-administered survey, suggesting that for this type of survey the method of administration makes little difference. There may be recall bias for the questions, which asked about information provision at diagnosis. Clearly each group of respondents is self-selected and only represent those who have joined a disease-specific patient group and access and respond to requests for participation in research studies. The VCRC group is further selected by requiring access to the Internet. The diagnosis is self-reported and we could not independently check it. There is a disproportionate overrepresentation of GPA in both groups, which is to be expected, as GPA is the most common type of ANCA vasculitis. In both groups MPA is underrepresented. Prevalence data suggest that in white Caucasian populations GPA is most common, with EGPA being least common, in a ratio of 7:3:1 [17]. In the VUK cohort this may reflect the development of the organization, which originally was established as a support group for patients with GPA.
The study has a number of strengths. We adapted and validated an established questionnaire and demonstrated it is valid for use in patients with a rare autoimmune disease. The study includes large numbers of patients and there is consistency between cohorts despite the differences in recruitment strategies and response rates, suggesting that the findings are generalizable to the AAV community as a whole and supporting the argument for needs-led provision of information.
Health care professionals should not underestimate the consequence of a diagnosis of AAV. Now that patients with AAV are routinely surviving the critical illness and disease remission is usually obtained, patient education should be recognized as an important aspect of disease management and the cornerstone of good quality care, as it is in other, more common chronic illnesses. Although the development of patient educational programmes in rare diseases poses unique challenges, the informational needs in these patients are high and need to be met.
Rheumatology key messages.
Patients with ANCA-associated vasculitis (AAV) have significant informational needs.
Patients with AAV prefer to receive educational information from a doctor.
Patients with AAV should receive education as a fundamental part of care.
Supplementary Material
Acknowledgements
The authors acknowledge Vasculitis UK (formerly Stuart Strange Trust) for conducting the mailing of the questionnaire in the UK. Thank you to the Springer Publishing Company for permission to adapt the TINQ.
Funding: Arthritis Research UK funded the development of the questionnaire through an education grant (17793). The Vasculitis Clinical Research Consortium is part of the NIH Rare Diseases Clinical Research Network (RDCRN). This work was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (U54AR057319) and the NIH Office of Rare Diseases Research (ORDR).
Disclosure statement: The authors have declared no conflicts of interest.
Supplementary data
Supplementary data are available at Rheumatology Online.
References
- 1.Schieppati A, Henter J-I, Daina E, Aperia A. Why rare diseases are an important medical and social issue. Lancet. 2008;371:2039–41. doi: 10.1016/S0140-6736(08)60872-7. [DOI] [PubMed] [Google Scholar]
- 2.Kole A, Faurisson F. The voice of 12,000 patients: experiences and expectations of rare disease patients on diagnosis and care in Europe. 2009 http://www.eurordis.org/publication/voice-12000-patients (4 March 2014, date last accessed) [Google Scholar]
- 3.Barlow JH, Turner AP, Wright CC. A randomized controlled study of the Arthritis Self-Management Programme in the UK. Health Educ Res. 2000;15:665–80. doi: 10.1093/her/15.6.665. [DOI] [PubMed] [Google Scholar]
- 4.Riemsma RP, Kirwan JR, Taal E, Rasker JJ. Patient education for adults with rheumatoid arthritis. Cochrane Database Syst Rev. 2003 doi: 10.1002/14651858.CD003688. (2):CD003688. [DOI] [PubMed] [Google Scholar]
- 5.Albano MG, Giraudet-Le Quintrec J-S, Crozet C, d’Ivernois J-F. Characteristics and development of therapeutic patient education in rheumatoid arthritis: analysis of the 2003–2008 literature. Joint Bone Spine. 2010;77:405–10. doi: 10.1016/j.jbspin.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 6.Coulter A. Partnerships with patients: the pros and cons of shared clinical decision-making. J Health Serv Res Policy. 1997;2:112–21. doi: 10.1177/135581969700200209. [DOI] [PubMed] [Google Scholar]
- 7.Opie A. Nobody’s asked for my view: user’s empowerment by multidisciplinary health teams. Qual Health Res. 1998;8:188–206. [Google Scholar]
- 8.Spalding NJ. Reducing anxiety by pre-operative education: make the future familiar. Occup Ther Int. 2003;10:278–93. doi: 10.1002/oti.191. [DOI] [PubMed] [Google Scholar]
- 9.Hesse BW, Arora NK, Burke Beckjord E, Finney Rutten LJ. Information support for cancer survivors. Cancer. 2008;112(Suppl):2529–40. doi: 10.1002/cncr.23445. [DOI] [PubMed] [Google Scholar]
- 10.Marcusen C. Information and communication needs of individuals living with advanced cancer. Semin Oncol Nurs. 2010;26:151–6. doi: 10.1016/j.soncn.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Ramos-Remus C, Salcedo-Rocha AL, Prieto-Parra RE, Galvan-Villegas F. How important is patient education? Baillieres Best Pract Res Clin Rheumatol. 2000;14:689–703. doi: 10.1053/berh.2000.0107. [DOI] [PubMed] [Google Scholar]
- 12.Young SP, Henderson E, Cheseldine DL, et al. Development and assessment of a World Wide Web site for systemic lupus erythematosus patient information. Lupus. 2002;11:478–84. doi: 10.1191/0961203302lu225oa. [DOI] [PubMed] [Google Scholar]
- 13.Hill J, Bird HA, Hopkins R, Lawton C, Wright V. The development and use of Patient Knowledge Questionnaire in rheumatoid arthritis. Br J Rheumatol. 1991;30:45–9. doi: 10.1093/rheumatology/30.1.45. [DOI] [PubMed] [Google Scholar]
- 14.Hennell SL, Brownsell C, Dawson JK. Development, validation and use of a patient knowledge questionnaire (PKQ) for patients with early rheumatoid arthritis. Rheumatology. 2004;43:467–71. doi: 10.1093/rheumatology/keh069. [DOI] [PubMed] [Google Scholar]
- 15.Ward MM, Sundaramurthy S, Lotstein D, et al. Participatory patient-physician communication and morbidity in patients with systemic lupus erythematosus. Arthritis Rheum. 2003;49:810–8. doi: 10.1002/art.11467. [DOI] [PubMed] [Google Scholar]
- 16.Limb L, Nutt S, Sen A. Experiences of Living with a Rare Disease. http://www.raredisease.org.uk/documents/RDUK-Family-Report.pdf (8 March 2013, date last accessed) [Google Scholar]
- 17.Watts RA, Mooney J, Skinner J, Scott DGI, Macgregor AJ. The contrasting epidemiology of granulomatosis with polyangiitis (Wegener’s) and microscopic polyangiitis. Rheumatology. 2012;51:926–31. doi: 10.1093/rheumatology/ker454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flossmann O, Berden A, de Groot K, et al. Long-term patient survival in ANCA-associated vasculitis. Ann Rheum Dis. 2011;70:488–94. doi: 10.1136/ard.2010.137778. [DOI] [PubMed] [Google Scholar]
- 19.Little MA, Nightingale P, Verburgh CA, et al. Early mortality in systemic vasculitis: relative contribution of adverse events and active vasculitis. Ann Rheum Dis. 2010;69:1036–43. doi: 10.1136/ard.2009.109389. [DOI] [PubMed] [Google Scholar]
- 20.Luqmani R, Suppiah R, Edwards CJ, et al. Mortality in Wegener’s granulomatosis: a bimodal pattern. Rheumatology. 2011;50:697–702. doi: 10.1093/rheumatology/keq351. [DOI] [PubMed] [Google Scholar]
- 21.Koutantji M, Harrold E, Lane SE, et al. Investigation of quality of life, mood, pain, disability, and disease status in primary systemic vasculitis. Arthritis Rheum. 2003;49:826–37. doi: 10.1002/art.11471. [DOI] [PubMed] [Google Scholar]
- 22.Mooney J, Poland F, Spalding N, Scott DGI, Watts RA. ‘In one ear and out the other—it’s a lot to take in’: a qualitative study exploring the informational needs of patients with ANCA-associated vasculitis. Musculoskeletal Care. 2013;11:51–9. doi: 10.1002/msc.1030. [DOI] [PubMed] [Google Scholar]
- 23.Aymé S, Kole A, Groft S. Empowerment of patients: lessons from the rare diseases community. Lancet. 2008;371:2048–51. doi: 10.1016/S0140-6736(08)60875-2. [DOI] [PubMed] [Google Scholar]
- 24.Hardware B, Anne Lacey E, Shewan J. Towards the development of a tool to assess educational needs in patients with arthritis. Clin Eff Nurs. 2004;8:111–7. [Google Scholar]
- 25.Moses N, Wiggers J, Nicholas C, Cockburn J. Prevalence and correlates of perceived unmet needs of people with systemic lupus erythematosus. Patient Educ Couns. 2005;57:30–8. doi: 10.1016/j.pec.2004.03.015. [DOI] [PubMed] [Google Scholar]
- 26.Galloway S, Graydon J, Harrison D, et al. Informational needs of women with a recent diagnosis of breast cancer: development and initial testing of a tool. J Adv Nurs. 1997;25:1175–83. doi: 10.1046/j.1365-2648.1997.19970251175.x. [DOI] [PubMed] [Google Scholar]
- 27.Harrison DE, Galloway S, Graydon JE, Palmer-Wickham S, Rich-van der Bij L. Information needs and preference for information of women with breast cancer over a first course of radiation therapy. Patient Educ Couns. 1999;38:217–25. doi: 10.1016/s0738-3991(99)00009-9. [DOI] [PubMed] [Google Scholar]
- 28.Graydon J, Galloway S, Palmer-Wickham S, et al. Information needs of women during early treatment for breast cancer. J Adv Nurs. 1997;26:59–64. doi: 10.1046/j.1365-2648.1997.1997026059.x. [DOI] [PubMed] [Google Scholar]
- 29.Templeton HR, Coates VE. Adaptation of an instrument to measure the informational needs of men with prostate cancer. J Adv Nurs. 2001;35:357–64. doi: 10.1046/j.1365-2648.2001.01883.x. [DOI] [PubMed] [Google Scholar]
- 30.O’Connor G, Coates V, O’Neill S. Exploring the information needs of patients with cancer of the rectum. Eur J Oncol Nurs. 2010;14:271–7. doi: 10.1016/j.ejon.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 31.Buckingham A, Saunders P. The Survey Methods Workbook: From Design to Analysis. Cambridge: Polity Press; 2004. [Google Scholar]
- 32.Thorpe CT, DeVellis RF, Blalock SJ, et al. Patient perceptions about illness self-management in ANCA-associated small vessel vasculitis. Rheumatology. 2008;47:881–6. doi: 10.1093/rheumatology/ken126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Basu N, McClean A, Harper L, et al. The characterisation and determinants of quality of life in ANCA associated vasculitis. Ann Rheum Dis. 2014;73:207–11. doi: 10.1136/annrheumdis-2012-202750. [DOI] [PubMed] [Google Scholar]
- 34.Herlyn K, Hellmich B, Seo P, Merkel PA. Patient-reported outcome assessment in vasculitis may provide important data and a unique perspective. Arthritis Care Res. 2010;62:1639–45. doi: 10.1002/acr.20276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tomasson G, Boers M, Walsh M, et al. Assessment of health-related quality of life as an outcome measure in granulomatosis with polyangiitis (Wegener’s) Arthritis Care Res. 2012;64:273–9. doi: 10.1002/acr.20649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adab P, Rankin ECC, Witney AG, et al. Use of a corporate needs assessment to define the information requirements of an arthritis resource centre in Birmingham: comparison of patients’ and professionals’ views. Rheumatology. 2004;43:1513–8. doi: 10.1093/rheumatology/keh371. [DOI] [PubMed] [Google Scholar]
- 37.Mukhtyar C, Guillevin L, Cid MC, et al. EULAR recommendations for the management of primary small and medium vessel vasculitis. Ann Rheum Dis. 2009;68:310–7. doi: 10.1136/ard.2008.088096. [DOI] [PubMed] [Google Scholar]
- 38.Ntatsaki E, Carruthers DM, Chakravarty K, et al. BSR and BHPR guideline for the management of adults with ANCA-associated vasculitis. Rheumatology. 2014 doi: 10.1093/rheumatology/ket445. doi: 10.1093/rheumatolofy/ket445. [DOI] [PubMed] [Google Scholar]
- 39.Chambers SA, Rahman A, Isenberg DA. Treatment adherence and clinical outcome in systemic lupus erythematosus. Rheumatology. 2007;46:895–8. doi: 10.1093/rheumatology/kem016. [DOI] [PubMed] [Google Scholar]
- 40.Julian LJ, Yelin E, Yazdany J, et al. Depression, medication adherence, and service utilization in systemic lupus erythematosus. Arthritis Rheum. 2009;61:240–6. doi: 10.1002/art.24236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Herlyn K, Gross WL, Reinhold-Keller E. Longitudinal effects of structured patient education programs for vasculitis patients. Z Rheumatol. 2008;67:206–10. doi: 10.1007/s00393-008-0290-9. [DOI] [PubMed] [Google Scholar]
- 42.Neville C, Fortin PR, Fitzcharles MA, et al. The needs of patients with arthritis: the patient’s perspective. Arthritis Care Res. 1999;12:85–95. doi: 10.1002/1529-0131(199904)12:2<85::aid-art3>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 43.Carpenter DM, DeVellis RF, Hogan SL, et al. Use and perceived credibility of medication information sources for patients with a rare illness: differences by gender. J Health Commun. 2011;16:629–42. doi: 10.1080/10810730.2011.551995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vehovar V, Manfreda K. Overview: on line surveys. London: Sage; 2008. pp. 177–94. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.