Abstract
Latinos with limited English proficiency (LEP) experience multiple barriers to accessing efficacious mental health treatments. Using a stage model of behavioral therapies research, this Stage 1b investigation evaluated the Brief Behavioral Activation Treatment for Depression (BATD), an intervention which may be well-equipped to address existing treatment barriers.
A sample of 10 Latinos with LEP and depressive symptomatology participated in a 10-session,direct (i.e., literal) Spanish-language translation of BATD, with no other cultural modifications. Participants were assessed at each session for depressive symptomatology and for the proposed BATD mechanisms: activity engagement and environmental reward. One month after treatment, participants were reassessed and interviewed to elicit feedback about BATD.
Hierarchical Linear Model analyses were used to measure BATD outcomes. Results showed depressive symptomatology decreased (p<.001), while both activation (p = .04) and environmental reward (p = .02) increased over the course of BATD. Increases in activation corresponded concurrently with decreases in depression (p = .01), while environmental reward preceded decreases in depressive symptomatology (all p’s≤ .04). Follow-up analyses revealed sustained clinical gains in depression and activation, and an increase in environmental reward at follow-up.
Participant interviews conducted one month after treatment conclusion indicated that BATD is an acceptable treatment for our sample of interest. Despite the limitations inherent to a study restricted to sample of ten, preliminary outcomes of this Stage I research suggest that members of this otherwise underserved group showed improvements in depressive symptomatology and are willing to participate in and adhere to BATD. The study’s positive outcomes suggest that a Stage II randomized clinical trial is a logical next step.
Keywords: Spanish-speaking Latinos, depression, behavioral activation, treatment development
The lifetime prevalence of Major Depressive Disorder (MDD) is 16.6% and its effects impair members of all racial and ethnic groups (Feliciano & Arean, 2007; Kessler, Chiu, Demler& Walters, 2005). Among the general Latino population, MDD rates range from 3–18%(Mendelson, Rehkopf & Kubzansky, 2008; Kessler et al., 2003; Vega et al., 1998). However, among Latinos with LEP, who constitute approximately half of the U.S. Latino population (U.S. Census Bureau, 2011), MDD rates are reportedly as high as 25% (Folsom et al., 2007; Muñoz, Ying, Pérez-Stable & Miranda, 1993).
Although MDD is highly treatable, well-established barriers preclude Latinos with LEP from accessing quality mental health care (Blanco et al., 2007; U.S. Department of Health and Human Services [DHSS, 2001]). For example, less than 5% of Latino immigrants afflicted with psychological disorders seek mental health services from specialized practitioners (Vega et al., 2007) due to a combination of linguistic and economic barriers, cultural-stigma, and the lack of empirically-supported psychosocial interventions (DHHS, 2001; Pincay & Guarnaccia, 2007; Vega et al., 2007). Moreover, this group reportedly drops out of treatment at a higher rate than non-Latino White-Americans (Organista & Muñoz, 1996; Miranda et al., 2003).
Despite the aforementioned barriers to access, Latinos with LEP tend to express positive attitudes towards psychosocial treatments for depression (Karasz & Watkins, 2006; Cooper et al., 2003). Some have proposed that it may be due to the nature of these interventions, which activate the reportedly valued-belief among Latinos of doing one’s part in one’s recovery (“poner de su parte”) (Caplan et al., 2013; Interian et al., 2010; Pincay & Guarnaccia, 2007), a concept highly consistent with the framework of behavioral approaches (Organista, 2000). In fact, these treatments have been regarded as worthy treatments for Latinos with mental health needs by allowing clients to take control over everyday situations, in contrast to the lack of control they may experience as a result of socioeconomic marginalization in the United States, including poverty and racism (Comas-Diaz, 1981).
Behavioral Activation (BA) presents a particularly promising form of behavior therapy for Latinos with LEP. According to BA, depression results when constructive (i.e., non-depressive) behaviors are not positively reinforced. The depressive state is then maintained by reinforcement of negative behaviors, such as avoidance and receiving sympathy from others (Lewinsohn, 1974). Through BA, and specifically “poner de su parte,” participants engage in activities important and enjoyable to them (Hopko, Lejuez, Ruggiero & Eifert, 2003). Concurrently, participants are required to monitor their mood while they engage in these activities. This increases their awareness of the effect that positive and negative behaviors have over their mood (Hopko et al., 2003; Lejuez et al., 2011). Latinos with LEP may be more willing to participate in this behavioral framework, in contrast to therapies that focus on internal factors, such as cognitions and biology, because it may reduce the stigma associated with receiving treatment (Santiago-Rivera et al., 2008).
A number of studies and resultant meta-analyses demonstrate BA’s efficacy (Mazzuccheli, Kane & Rees, 2009; Cuijpers, van Straten & Warmerdam, 2007; Ekers, Richards & Gilbody, 2008). A recent open-label trial (N = 10) evaluating a culturally-modified Spanish BA version showed significant decreases in depression post-treatment. Despite promising results, this study was limited by low retention rates (3 of 10 completed treatment) and the absence of male participants. The trial also did not examine the BA proposed mechanisms of change, lacked follow-up data, and did not evaluate the need for cultural modifications (Kanter et al., 2010).
Building on the promising outcomes of the trial conducted by Kanter and colleagues (2010), we evaluated the Brief Behavioral Activation Treatment for Depression, a 10-session weekly version of BA, which may reduce current treatment disparities for Latinos (BATD; Lejuez et al., 2001; Lejuez et al., 2011). Studies show that minority samples similarly-situated to Latinos with LEP (e.g., Fortuna, Alegria & Gao, 2010; Alegria et al., 2002) are more likely to complete BATD than alternative treatments, such as supportive counseling or treatment as usual (e.g., Magidson et al., 2011). Furthermore, BATD’s idiographic approach focuses on individuals’ unique personal values. The process of value identification and subsequent activity selection is entirely client-directed and focused, and therefore individually tailored (Collado, MacPherson, Risco & Lejuez, accepted for publication). With the help of a therapist, the client identifies important life areas (e.g., relationships), values within those life areas (e.g., be an involved parent), and activities in which the client can engage that are congruent with those values (e.g., attend the child’s extracurricular activities). Each value is incorporated into the treatment to the extent the client deems it important. Thus, the therapist does not make any assumptions about the individual’s values. This feature of BATD may prove particularly useful when treating U.S.-based Latinos given the group’s heterogeneity, whose members represent more than 20 countries, each embedded within different sociocultural contexts and histories. BATD’s idiographic nature prevents placing clients into predetermined and oftentimes erroneous categories based on assumptions of cultural heritage alone and promotes a treatment plan that is highly relevant to the participant’s needs. At the individual level, this may help foster treatment response and retention; from a more global perspective, this indicates that BATD may be an efficacious treatment for heterogeneous populations. Lastly, BATD can be tailored to accommodate the needs of clients with low-literacy by providing them with modified treatment materials (Lejuez et al., 2011). Given its inherent characteristics, BATD may effectively decrease depression and reduce attrition by offering a treatment platform equipped to address the various challenges associated with obtaining care among this group.
Using the Stage Model of Behavioral Therapies research framework (see Rounsaville, Caroll & Onken, 2001; Carroll & Nuro, 2002), the current study investigated BATD as a treatment for depression among Latinos with LEP through a Spanish translation of the intervention. The direct translation permitted individual tailoring without making any other specific, a priori cultural modifications (Collado et al., accepted for publication). The primary goal of this Stage I research was to evaluate BATD, an idiographic intervention, employing the rationale that BATD provides a flexible and easily-tailored treatment framework able to address the individual and psychological needs of depressed Latinos. Consistent with Stage I treatment development, the current investigation included a small number of participants (N = 10) as part of an open-label trial (Carroll & Nuro 2002; Rounsaville, Caroll & Onken, 2001). As a second goal, the study examined the acceptability of a direct (i.e., verbatim)Spanish language translation of the intervention. The latter goal ensured that any future cultural modifications to BATD targeting depressed Latinos with LEP would be guided by prior evidence to support such changes. We hypothesized that, over time, participants would experience reductions in depressive symptoms and both increases in level of activation and contact with environmental reward. We also expected to find correspondence between both increases in levels of activation and environmental reward with decreases in levels of depression. Finally, we hypothesized that patients would sustain clinical gains one month after treatment.
Method
Participants
Participants (N = 10) were recruited through flyers and referrals provided by two different community centers serving Latinos. Participants were excluded from the study if they did not meet the following inclusion criteria: 1) be a minimum of 18 years old, 2) be of Latino descent, 3) have a self-reported LEP, 4) have a cut-off score of 10 or higher in the BDI-II, indicating mild depressive symptomatology (please see Measures), 5) have completed the 4th grade or higher either in their country of origin or in the US, 6) not have current substance abuse or dependence , 7) not meet diagnostic criteria for a current psychotic disorder, 8) not meet diagnostic criteria for bipolar disorder, and 9) if taking antidepressants, demonstrate stability as indicated by three or more consecutive months of use. Participants who did not meet all study criteria were provided with community referrals. The eligibility criterion of a BDI-II score of 10 or above was selected as opposed to MDD diagnosis to include individuals with a broader range of depressive symptoms1. Previous depression treatment studies with underserved groups have also used this cut-off (e.g., Daughters et al., 2012; MacPherson et al., 2010).
Procedures
Preliminary eligibility was determined over the telephone. From 42 callers who responded to our advertisement efforts, 29 were screened and 13 could not be recontacted after they left a message expressing interest in the study. Of those screened, 5 were ineligible based on study criteria (current psychotic symptoms [n = 2], language ineligibility [n = 1], low BDI-II score [n = 2]), and 8 were unable to be reached after various attempts. Of the remaining 24 eligible participants, 19 were scheduled for a baseline appointment and the other 5 participants indicated that they were not interested in participating after study procedures were reviewed. Ten participants showed up to their initial meeting. Efforts to reschedule the 9 no-show potential participants included calling them several times as well as sending them a letter to call our Center.
Permission to conduct the current research was obtained from the [Academic Institution Omitted] Institutional Review Board (IRB) along with a federal Certificate of Confidentiality (COC) from the National Institute of Mental Health as a precaution to protect any reports of illegal immigration status from forced disclosure. At the initial meeting, a research assistant (RA) reviewed study procedures, obtained verbal informed consent, and discussed the COC.
Immediately prior to each BATD one-hour session, participants completed study assessments. There were a total of 10 assessment points and participants earned $10 each time. Due to limited literacy, three participants requested that the questions be read to them at every session. Potential covariates included demographic information, mean scores of bi-weekly assessments of therapeutic alliance (Bedregal, Paris, Añez, Shahar, & Davidson, 2006)and baseline acculturative stress (Rodriguez et al., 2002) (please see Measures).
During the one-month follow-up, participants completed the same assessments administered prior to each BATD session and the in-depth interview, for which they earned $20. An RA fully trained in standard interview methodology (Kvale, 1994)followed a predetermined script. Each of the eight participants that completed the weekly, BATD sessions also completed the follow-up assessment, as did one of the two participants that completed only four BATD sessions; the remaining participant could not be reached.
Intervention
The study utilized an untested direct Spanish translation of the current BATD manual (Lejuez et al.,2011),allowing for individual tailoring but without any other cultural modifications (Collado et al., accepted for publication). The translation was headed by the third author (FM) and conducted by four bilingual psychologists. As outlined in the manual, the first session of BATD focused on providing depression psychoeducation, reviewing the treatment’s rationale, discussing the importance of monitoring daily activities, describing session attendance policies and stressing the importance of attending every session weekly, and explaining the relationship between treatment adherence and the likelihood of treatment success. Starting in the first session and continuing until the end of treatment, the homework assignment focused on participants monitoring their daily activities until the subsequent session and reporting a numerical rating of both enjoyment and importance for each activity completed.
The second BATD session began with a brief review of the previous session’s content, including a discussion of completed activities as well as the ratings of enjoyment and importance, making use of the completed daily monitoring record forms, and assessing any difficulties associated with homework completion. The remainder of the second session was devoted to a thorough discussion of life areas (e.g., relationships) and corresponding values (e.g., be a caring husband) important for participants, with the purpose of selecting activities consistent with these values in future sessions (e.g., taking spouse on monthly dates).
During the third session, participants selected at least fifteen activities they considered rewarding (taking into consideration both expected enjoyment and importance) that were consistent with life areas they deemed important and their expressed personal values. These could have constituted activities already a part of the participants’ schedule or new activities. Participants proceeded to rank the activities in terms of difficulty such that they completed easier activities toward the beginning of treatment and progressed towards more challenging activities. Starting in the fourth session, participants worked toward engaging in three to five activities on their list that reflected their values.
Specific to session 5,participants were introduced to “contracts”, which provided the opportunity to request assistance from friends and family in order to accomplish selected activities because the activity is challenging for participants or because company may potentially increase the “enjoyment” and “importance” of the activity. Of note, discussing contracts with individuals from a supportive network does not require that participants disclose they are seeking depression treatment or sign any document; rather, participants may simply ask these individuals to join them in completing the specific activity.
No new material was introduced beyond this point. Sessions 6 through 10 consisted of continued engagement on meaningful activities and daily monitoring, as well as discussions of an individualized post-treatment plan within a behavioral activation framework of scheduling activities corresponding to participants’ values and drafting “contracts” with people in their support network. Throughout treatment, depression-consistent and depression-inconsistent patterns are identified with the assistance of the monitoring forms and ratings of enjoyment and importance.
Measures
In line with our study aims, questionnaires were selected to assess four principal domains including depressive symptomatology, activation and environmental reward, qualitative information regarding participants’ experience with BATD, and potential treatment covariates. Spanish translations of all assessments were utilized.
Beck Depression Inventory-II (BDI-II; Beck, Steer & Brown, 1996): The BDI-II is a reliable and well-validated assessment of depression severity in English and Spanish (Sanz, Perdigón & Vázquez, 2003). It was administered to determine diagnostic inclusion as well as weekly, to identify depressive mood variations throughout treatment course. The Inventory consists of 21 items, with cumulative scores ranging between 0 and 63, with higher scores representing increased depression severity. In the current trial, Cronbach’s alpha for the BDI-II ranged from .75 to .93 across all sessions.
Structured Clinical Interview for DSM-IV (SCID-IV, non-patient version; First, Spitzer, Gibbon, & Williams, 1995). To determine diagnostic eligibility and obtain a clinical picture of each participant, a trained research assistant (RA) conducted the following SCID-IV modules: 1) primary affective disorders, 2) substance use disorders, 3) primary anxiety disorders, and 4) and psychotic symptoms.
The Behavioral Activation for Depression Scale (BADS; Kanter et al., 2007):consists of 25 items to measure the extent to which individuals become more activated and less avoidant through the course of the BA intervention. Subscales comprising the BADS include Avoidance/Rumination, Social Impairment, School/Work Impairment, and Activation. Given that examining participants’ activation levels through treatment course was highly relevant to our study hypotheses, we examined weekly increases in the total BADS scale as well as in the BADS Activation subscale specifically. The internal consistency of the Spanish version of the complete BADS scale has been reported at .80 and at .81 for the BADS Activation subscale when administered to a sample comprised of students at a Spanish university (Barraca, Pérez-Álvarez, & Bleda, 2011). In the current sample, Cronbach’s alpha for the total BADS scale ranged from .80 to .94 and from .81 to .96 for the BADS Activation subscale across all BATD sessions.
The Reward Probability Index (RPI; Carvalho, et al, 2011): The RPI is a 20 item scale that was developed to assess availability of rewards in the environment. The total RPI consists of two subscales: 1) the Reward Probability Index, which includes items measuring the likelihood to which individuals are able to obtain rewards through instrumental behaviors, and 2) the Environmental Suppressors Index, consisting of items that describe the availability of aversive and unpleasant experiences in respondents’ environment. Because there is no existing Spanish translation of the RPI, the team headed by FM translated the original version of the RPI into Spanish and the first author (AC) was responsible for back-translating the items into English (please see Fouad & Bracken, 1986 for more information about this procedure). In the original validation study, internal consistency of the total RPI scale was α = .90 and between α = .82 and .90 for each individual subscale (Carvalho et al., 2011). In the current sample, the Cronbach’s alpha for the total RPI scale ranged between .83 and .89 across all weeks of treatment. Further, Cronbach’s alpha for the Reward Probability Index ranged between .84 and .95 and between .73 and .88 for the Environmental Suppressors Index across sessions.
Our rationale for administering both the BADS and the RPI was based on the purported differences between the constructs they assess. Manos, Kanter and Busch (2010) indicated that the BADS measures frequency of activation and avoidance, whereas the RPI measures the probability of obtaining environmental rewards.
For our second study aim, an in-depth interview was conducted at a one-month follow-up to assess treatment acceptability, feasibility, satisfaction, comprehensibility of BATD’s rationale, language and manual organization, perceived effectiveness, and suggestions.
Demographics Questionnaire: A standard demographics questionnaire was created that included items regarding participants’ education, income, years of residence in the United States, English language ability (neither read nor write = 0; read or write = 1; read and write = 2), depression treatment history, and immigration status, and antidepressant use among other variables (please see Table 1).
Table 1.
Demographic and Clinical Characteristics(N = 10)
| Demographic Characteristics | Clinically-Relevant Variables | ||
|---|---|---|---|
| Age, mean, (SD) | 41.45 (14.99) | BDI-II score, mean, (SD) | 27.60 (10.84) |
| Gender, n female | 7 | BADS score, mean, (SD) | 75.75 (24.45) |
| Marital Status, n | BADS Activation score, | 20.29 (15.21) | |
| Single (never married) | 3 | mean, (SD) | |
| Married | 3 | RPI score, mean, (SD) | 47.63 (6.32) |
| Divorced | 1 | Environmental Suppressors | 20.00 (2.39) |
| Other | 3 | score, mean, (SD) | |
| Years living in the United States, mean (SD) |
17.82 (13.42) | Reward Probability Index score, mean, (SD) |
27.62 (7.89) |
| Education, grade, mean (SD) | 7.00 (3.99) | ||
| Total Annual Income, n | |||
| <$14,999 | 7 | ||
| $15,000 - $29,000 | 2 | ||
| $30,000 - $44,999 | 1 | ||
| Employment, n | |||
| Half-time | 3 | ||
| Full-time | 2 | ||
| Retired | 1 | ||
| Unemployed | 4 | ||
| Family in the United States, yes, n | 7 | ||
| Ever received depression treatment, yes, n |
4 | ||
| Depression, n | |||
| Current MDD | 6 | ||
| Past MDD | 6 | ||
| Current Double Depression | 2 | ||
| Past Dysthymia | 3 | ||
| Current Generalized Anxiety | 5 | ||
| Disorder, n | |||
| Current Posttraumatic Stress | 2 | ||
| Disorder, n | |||
| Past Alcohol Abuse, n | 1 | ||
Note. BDI-II = Beck Depression Inventory; BADS = Behavioral Activation for Depression Scale; RPI = Reward Probability Index composite score.
Multidimensional Acculturative Stress Inventory (MASI; Rodriguez et al., 2002):Originally created to measure acculturative stress from living in the United States for individuals of Mexican origin, the scale is comprised of four subscales including English Competency Pressures (7 items), Pressure to Acculturate (7 items), Pressure Against Acculturation (4 items), and Spanish Competency Pressures (7 items). Given the non-applicability of the last subscale for the current sample, we only used the first three. Higher scores indicate greater stress. The Spanish version of the questionnaire has achieved Cronbach alpha values ranging from .74 to .91. Our current sample demonstrated an internal consistency of the three subscales at α =.89.
The Therapeutic Alliance with Clinician Questionnaire (TAC; Neale & Rosenheck, 1995) assesses the strength of the therapeutic relationship using a 9-item Likert scale format. The Spanish version of the questionnaire (Bedregal, Paris, Jr., Añez, Shahar & Davidson, 2006) was evaluated with a sample predominantly comprised of depressed individuals and achieved high internal consistency (α = .96). In our sample, internal consistency ranged from α’s = .87 to .94.
Therapist Competence, Adherence, and Fidelity
An advanced graduate student (AC) with native Spanish fluency who had two years prior experiencing delivering other BATD-based interventions, served as the study therapist. As part of her training for the current trial, she completed three, two-hour workshops conducted by the BATD developer and completed two hours of weekly supervision prior and throughout study course with two doctoral level psychologists, including the treatment developer (CWL) and the fifth author (LM). The primary goals of supervision included ensuring BATD treatment fidelity and standardization and discussing participant progress and challenges encountered at each session. Treatment Fidelity Strategies for Monitoring and Improving Provider Training procedures outlined by the NIH Behavior Change Consortium (Bellg et al., 2004) were followed.
In line with our IRB requirements to protect this vulnerable group of individuals, we asked permission of each participant to record (or have a supervisor observe) sessions. Unfortunately seven participants refused this request. Therefore our review of tapes included 20% of randomly selected sessions from the three available clients using a rating form containing topics prescribed (BATD-consistent) and proscribed (BATD-inconsistent) for each session. Although a very limited sample, the ratings indicated perfect adherence. For the other patients, the therapist self-reported adherence and non-adherence using the same rating form. The therapist and the treatment developer reviewed these ratings in weekly supervision to ensure that all BA components were included in each session while therapeutic elements not part of the treatment were not. Notably, the BATD manual was used at all times to ensure standardization of treatment and consistency of delivery.
To ensure study integrity, a Spanish-speaking RA administered the outcome assessments; neither the therapist nor the RA discussed aspects related to participants’ assessment or treatment.
Statistical Analyses
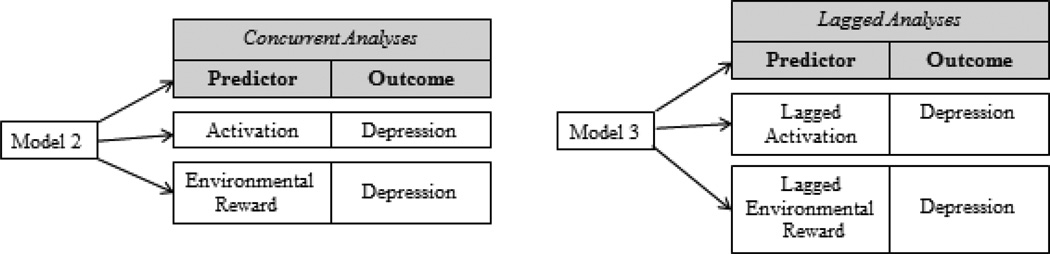
We conducted repeated measures analyses utilizing Hierarchical Linear Modeling (HLM; Raudenbush & Bryk, 2002). Although the discussion of sufficient sample size for using this data analytic approach is still an active area of research and debate (e.g., Hedeker & Mermelstein, 2000), we opted to use HLM in the current sample (N = 10) as it provides a means to use all of the available participants, even when there are missing data. HLM also allows a more comprehensive understanding of potential changes in depressive symptomatology over time as well as the proposed treatment mechanisms over the course of BATD treatment. HLM as an approach to the analysis of repeated measures has been recommended because of: 1) its ability to include multiple measurement points while accommodating missing data, 2) examining individual change over time in outcomes, and 3) including the average change and the individual variation around this average change (Raudenbush & Bryk, 2002; Singer & Willett, 2003). Further, HLM allows for examination of the rate of change for each individual; each participant serves as his or her own referent, which is especially important in a small sample. Guidelines offered by the Institute of Medicine (2001) suggest using our selected analytic approach in order to obtain reliable and valid results and maximize information from small trials. We used Restricted Maximum Likelihood (REML) estimates and random effects, which are both preferred when estimating effects in small samples (Bickel, 2007). In addition to the approach’s benefits, HLM allowed us to control for baseline scores of each measure when investigating change in those measures over time as well as to include all available participant data. We specified HLM Level-1 intercepts and slopes as random given expected within-person variability in baseline scores and change in symptoms throughout treatment. The individual growth parameters (intercept, slope) at HLM Level-1 are parameters that become the dependent variables explained by between-subject (person-specific changes) factors at HLM Level- 2. All independent variables, other than time, were centered. We tested three different models. The first model examined the linear effects of time for each construct of interest (i.e., depressive symptoms, activation, and environmental reward). To test the correspondence between the hypothesized increases in activation and contact with environmental reward, and decreases in depression we tested an additional two models (See Figure 2) Model 2 examined the concurrence between depressive symptomatology and BATD proposed mechanism of change (e.g., BDI-II score at session 3 and BADS score at session 3) if construct scores did show variability over time, baseline scores of these constructs were specified as covariates of depressive symptomatology over treatment course (HLM Level 2). Model 3 examined whether BATD proposed mechanisms of change predicted depression levels by lagging activation and reward derived by the environment (e.g., BADS score at session 5 and BDI–II at session 6). To analyze maintenance of clinical gains, we conducted paired t-tests between post-treatment and follow-up to analyze maintenance of clinical gains (See Table 3). The effect size for each dependent measure was calculated using Cohen’s d with the untreated sample mean at baseline relative with the treated sample mean at Session 10 and the pooled sample standard deviation as the denominator. All available data were used in our analyses. For our second study goal, broad themes were derived at the outset to categorize participant responses using Hill’s guidelines (Hill, Thompson & Williams, 1997).Statements applying to all participants were labeled “general,” those applying to half or more participants were labeled “typical” and statements consistent between two but less than half participants, were labeled “variants.”
Table 3.
Paired T-tests Analyses Evaluating Changes in Depressive Symptomatology, Activation, and Contact with Environmental Reward between the Last BATD session and the 1-Month Follow-up (n=8)
| Clinical Variables |
Last Session Mean (SD) |
1-Month Follow-up Mean (SD) |
P |
|---|---|---|---|
| BDI-II | 13.71 (7.34) | 11.14 (5.70) | .253 |
| BADS | 89.00 (21.40) | 80.00 (28.05) | .219 |
| BADS-Activation | 27.00 (11.72) | 29.62 (6.82) | .457 |
| RPI | 55.50 (9.20) | 59.75 (10.11) | .034 |
Note. Means and standard deviations presented for participants. BDI-II = Beck Depression Inventory; BADS = Behavioral Activation for Depression Scale; RPI = Reward Probability Index composite score.
Results
Demographic and Clinical Characteristics
Baseline demographic and clinical characteristics of the sample are summarized in Table 1. The sample consisted of seven females and three males born in Guatemala, El Salvador, Honduras, Mexico, Nicaragua, and Peru. Participants reported residing in the US for a mean of 17.82 years (SD = 13.42) and the sample’s mean age was 41.45 years (SD = 14.99). Seven participants reported earning a yearly income of less than $15,000. Participants’ mean education level was 7th grade (SD = 3.99).BDI-II scores ranged from 10 to 46, with 8 individuals falling between the “moderate” and “extreme” depressive symptoms categorization. Baseline mean scores of clinically-relevant variables are also presented in Table 1.
Treatment Attendance and Adherence
Averaging across participants, 7.8 sessions were completed over a mean of 10.7 weeks, which resulted in 88% of completed sessions; two participants completed 4 sessions and the remaining eight completed all sessions. The eight participants who completed treatment did so between 10 weeks and 13 weeks. Techniques for promoting initial presentation to treatment and continued retention (Interian, Allen, Gara, & Escobar, 2008)were used throughout the study. Mean percentage rate of homework completion was 86.54 % (completion within each participant ranged from 41.7% to 100%).
Model 1: Linear Effects of Time
Examination of individual trajectories in depression overtime indicated a linear slope was the appropriate and parsimonious effect of time to model. Treatment covariates, including demographic information, baseline levels of acculturative stress, and mean scores of bi-weekly assessments of therapeutic alliance were not significant when entered into HLM models (all p’s >.17) and thus, were not included in our final models.
Model 1 results showed a significant linear decrease over time on depressive symptomatology (β = −1.64,SE = 0.21, p < .001). Further, total BADS (β = 1.91, SE = .0.79, p = .04) and BADS’ Activation subscale (β = 0.86, SE = 0.35, p = .04) showed a significant linear increase over the course of BATD. In addition, total environmental reward measured by total RPI score showed a significant linear increase over time (β = 0.45, SE = .16, p = .02). However, there were no significant linear changes over time for RPI Environmental Suppressors (β = −0.14, SE = 0.18, p = .46), or RPI Reward Probability (β = 0.32, SE = 0.17, p = .10). Baseline scores of these two subscales were specified as covariates of depressive symptomatology over treatment course (HLM Level 2) as indicated in Table 2. These covariates were not significant although the baseline score of RPI Environmental Suppressors approached significance (p = .06).
Table 2.
HLM Analyses
| Fixed Effects Models | Β | SE | T | P |
|---|---|---|---|---|
| Model 1- Linear Effects of Time | ||||
| BDI-II | ||||
| Intercept | 25.751 | 3.381 | 7.616 | <0.001 |
| Time | −1.639 | 0.212 | −7.723 | <0.001 |
| BADS | ||||
| Intercept | 80.122 | 8.700 | 9.210 | <0.001 |
| Time | 1.913 | 0.794 | 2.408 | 0.039 |
| BADS- Activation | ||||
| Intercept | 21.003 | 3.754 | 5.594 | <0.001 |
| Time | 0.857 | 0.346 | 2.475 | 0.035 |
| RPI | ||||
| Intercept | 52.662 | 3.224 | 16.337 | <0.001 |
| Time | 0.452 | 0.159 | 2.843 | 0.019 |
| RPI-Reward Probability | ||||
| Intercept | 30.148 | 2.629 | 11.466 | <0.001 |
| Time | 0.320 | 0.172 | 1.864 | 0.095 |
| RPI-Environmental Suppressors | ||||
| Intercept | 22.504 | 1.419 | 15.861 | <0.001 |
| Time | −0.139 | 0.179 | −0.775 | 0.458 |
|
Model 2- Concurrent Association between Depression with Activation and Environmental Reward | ||||
| Intercept | 24.006 | 2.947 | 8.145 | <0.001 |
| Time | −1.240 | 0.282 | −4.391 | 0.002 |
| BADS | −0.143 | 0.041 | −3.472 | 0.007 |
| Intercept | 23.401 | 3.120 | 7.500 | <0.001 |
| Time | −1.279 | 0.208 | −6.154 | <0.001 |
| BADS- Activation | −0.208 | 0.094 | −2.211 | 0.054 |
| Intercept | 25.573 | 3.357 | 7.617 | <0.001 |
| Time | −1.371 | 0.290 | −4.728 | <0.001 |
| RPI | −0.217 | 0.146 | −1.482 | 0.173 |
| Intercept | −0.992 | 0.337 | 0.943 | <0.001 |
| Time | −1.676 | 0.244 | −6.884 | <0.001 |
| Baseline RPI- Reward Probability (Level 2) |
0.036 | 0.033 | 1.064 | 0.322 |
| Intercept | 1.386 | 1.540 | 0.900 | 0.398 |
| Time | −1.687 | 0.191 | −8.830 | <0.001 |
| Baseline RPI- Environmental Suppressors (Level 2) |
−0.182 | 0.081 | −2.256 | 0.059 |
| Model 3- Activation and Environmental Reward Preceding Depression | ||||
| Intercept | 5.007 | 3.226 | 1.552 | 0.155 |
| Time | −1.058 | 0.266 | −3.979 | 0.003 |
| Lagged BADS | −0.080 | 0.044 | −1.810 | 0.104 |
| Intercept | 3.690 | 3.144 | 1.173 | 0.271 |
| Time | −1.010 | 0.235 | −4.302 | 0.002 |
| Lagged BADS-Activation | −0.183 | 0.105 | −1.774 | 0.115 |
| Intercept | 4.326 | 2.965 | 1.459 | 0.179 |
| Time | −1.130 | 0.281 | −4.027 | 0.003 |
| Lagged RPI | −0.260 | 0.105 | −2.471 | 0.036 |
Note. BDI-II= Beck Depression Inventory; BADS = Behavioral Activation for Depression Scale; RPI = Reward Probability Index composite score
Models 2 and 3: Association between Depression with Activation and with Environmental Reward
Model 2 analyses, which tested the concurrent association between depression and BATD’s proposed mechanisms, showed concurrence of depressive symptoms with BADS total activation(β = −0.14, SE = 0.04, p = .01) and the BADS’ Activation subscale (β = −0.208, SE = 0.094, p= .05), such that higher levels of activation corresponded to lower levels of depression. This concurrent relationship was not observed for RPI total contact with environmental reward (β = 0.22, SE = 0.15, p = .17).
Model 3, which tested whether the proposed mechanisms of BATD preceded depressive symptomatology, indicated that higher total contact with reward in the environment preceded reductions in depressive symptomatology (β= −0.26, SE= 0.11, p=.04). In turn, neither construct of Activation preceded reductions in depression over time (p’s> .12).
Maintenance of Clinical Gains
Given the absence of a control group for comparison, it was important to determine whether gains after treatment conclusion were sustained. Paired t-tests demonstrated overall maintenance of clinical gains for both Activation measures and an increase in contact with environmental reward between post-treatment and the one-month follow-up (t = −2.63, df = 7, p = .03). See Table 3 for a summary of these results.
Effect Sizes
Effect sizes for all clinically-relevant variables pre- and post-treatment ranged from medium to large. More specifically, changes in depressive symptomatology (d = 1.45) and total reward derived from the environment (d = − 1.00) exhibited large effects. Changes in RPI Reward Probability (d = −0.65), RPI Environmental Suppressors (d = − 0.75), total BADS Activation (d = − 0.70) and Activation subscale (d = −0.50) represented medium effects.
In-Depth Interview Data
Finally, the in-depth interviews conducted to examine the need for targeted cultural modifications to BATD, suggested that the intervention met the needs of our sample given favorable feedback offered by participants who completed the interview (n = 9). Among general statements (i.e., statements applying to all participants) participants indicated that homework completion was an uncomplicated task, that their efforts to fight depression were positively received from people in their support network, that they were “much improved” after treatment, and that BATD treatment components and forms were easy to understand. In addition, all participants reported valuing the relationship with the BATD therapist and the RA. Although no “general” or “typical” (i.e., statements applying to half or more participants) suggestions to modify the treatment were offered, “variant” suggestions (i.e., statements consistent between two but less than half of participants) included delivering BATD in a group setting, extending the treatment beyond 10 sessions, and decreasing the number of questionnaires administered at each session. Participants did not suggest specific changes to BATD’s content. See Table 4 for a summary of participants’ responses.
Table 4.
In-Depth Interview Results (n = 9)
| Type of Comment | |||
|---|---|---|---|
| Theme | General (n = 100%) | Typical (n ≥ 50%) | Variant (20% ≥ n < 50%) |
| Feasibility |
|
|
|
| Acceptability |
|
|
|
| Satisfaction |
|
|
|
| Comprehension |
|
||
| Perceived Effectiveness |
|
|
|
| Suggestions |
|
||
Discussion
The current Stage I trial evaluated the outcomes of BATD among 10 Latinos with LEP who had elevated depressive symptomatology. The treatment’s sole modification included a direct translation into Spanish. In lieu of a uniform and global, cultural modification, and in line with its basic theoretical framework, BATD was individually-tailored based on each participant’s unique values, both culturally and otherwise. Results indicated that depressive symptomatology decreased and both activation levels and environmental rewards increased over the course of treatment. Moreover, depression and activation systematically co-occurred over time: while depression decreased, activation increased. Lagged findings demonstrated that increases in contact with environmental reward preceded decreases in depressive symptomatology at a subsequent session. In addition, our findings suggested that clinical gains obtained during BATD were sustained, with a significant increase in total environmental reward between the last session of treatment and the one-month follow-up. Finally, in-depth interview responses indicated satisfaction with the flexible nature of the treatment and did not suggest need for modifications to the treatment (cultural or more general).
Several findings are worthy of discussion. First, the concurrent association between depression and activation may suggest that these constructs are closely related; a lack of activation may be a feature of depression and vice versa. The prospective relationship observed between environmental reward and depression, on the other hand, may indicate that environmental reward may have an effect on depression. Second, findings demonstrated that BATD resulted in sustained clinical gains, but environmental reward increased between end-of-treatment and the one-month follow-up. This may reflect that clients’ continued participation in activities serves to increase their perceived ability to come into contact with such reward. Although we did not measure continued engagement in rewarding activities, it is possible that clients continue to implement BATD-relevant skills even after treatment has concluded, which was unanimously supported by participant statements at the in-depth interview.
The in-depth interview component offers support, at a very preliminary stage, that a direct Spanish translation of the BATD manual was not only acceptable but also culturally-sensitive. This may be due to the intervention’s ability of allowing individual treatment tailoring, in a case-by-case basis. These interviews cannot rule out the possibility that while the tailoring approach worked well with a Latina therapist who has a strong interest in culturally-sensitive treatment delivery, an explicit, a priori BATD cultural modification may have worked as well or better with therapists who do not share these qualities (Collado et al., accepted for publication).
The present study has several limitations. First, the absence of a control group precludes the ability to draw specific conclusions about BATD’s ability to reduce depressive symptomatology and increase the proposed mechanisms of change. At this stage, it is unclear whether the changes observed are a product of BATD or an effect of maturation. Second, a small sample size raises the potential for inadequate power to detect significance, lack of generalizability, and inflated effect size estimations and significance tests. Third, the current study utilized a BDI-II score of 10 as an inclusion criterion. Although 8 of 10 participants fell within the categories of “moderate” or “extreme” depressive symptomology as indicated by this measure, future studies should use a higher cut-off score and/or a MDD diagnosis as the inclusion criterion. This would allow researchers to determine the efficacy of BATD for the treatment of clinical depression among Latinos with LEP. Fourth, only three participants agreed to the request of recording their sessions. Future work should explore efforts to ethically increase client comfort with taping/observation of sessions to provide a more stringent test of adherence and fidelity. This is especially important to guard against bias and its impact on adherence ratings that could result from only a small number of participants agreeing to be recorded. Fifth, although medium to large effect sizes were observed in clinically-relevant variables from the first to the last BATD session, future work would benefit from examination of reliable change or clinically significant changes. Sixth, the RPI and BADS instruments have not been validated in our sample of interest. For instance, RPI Environmental Suppressors could be tapping into normative experiences of immigrant Latinos; the scale includes items such as “I have few financial resources, which limits what I can do,” and “People have been mean or aggressive toward me.” If these scale items do in fact describe this group’s experiences, observing changes in the subscale over time, as was the case in our results, will be unlikely. Seventh, weekly administration of questionnaires may have been too proximal to be able to detect effects. Related to this limitation, future research should better examine temporal relationships and the directionality of depression and the proposed BATD mechanisms. Finally, it is important to note the number of initial callers that contacted the study (N = 42) and those who were enrolled in the study (N = 10). A significant proportion of callers were lost due to inability to be reached after making the initial call. Although these numbers appear to be comparable to other community-based depression trials (e.g., Arean et al., 2005; MacPherson et al., 2010) particular attention should be paid to these rates in future studies enrolling a community sample of Latinos. The study limitations afford numerous opportunities to expand upon and enhance this line of research to establish the efficacy of BATD as a treatment for depression among Latinos with LEP.
Despite these limitations, the current investigation provides a valuable contribution to a scarce depression treatment literature for Latinos with LEP, who have few treatment options and continue to face mental health care barriers and disparities. This is also one of the few investigations that elicited comprehensive feedback from participants to gain insight as to their personal treatment experience and examine the need for BATD’s cultural modification from a sample that has been historically underrepresented in this type of research. Additionally, the study demonstrated the potential value of BATD in supporting treatment adherence, with 8 of 10 treatment completers with 100% attendance among these individuals (and mean homework completion of 86.54%) exceeding rates observed in the literature (e.g., Floyd et al., 2004). ‘These treatment adherence rates are consistent with participants’ positive feedback from the in-depth interviews regarding treatment acceptability, feasibility, satisfaction, and perceived effectiveness. Finally, this is the first published study examining potential relationships between proposed BATD mechanisms and depressive symptomatology. Altogether, these results suggest the promise of BATD in terms of depression-related outcomes, acceptability, retention and adherence in this underserved, understudied group in high need of depression mental health services. The positive outcomes characterizing this study suggest that a Stage II randomized clinical trial is a logical next step.
Figure 1.
Representation of models testing the correspondence between increases in activation and contact with environmental reward, and decreases in depression. Model 2 tested the concurrent association between depression with activation and environmental reward. Model 3 tested whether increases in activation and contact with environmental reward preceded decreases in depression.
Acknowledgement
The authors would like to thank Dr. Lea Dougherty for her guidance in the data analytic plan and Juan Fogelbach for his editing advice. Further the authors would like to thank Nancy Cavazos from the Therapeutic Relief Center, Inc., and Maria Herrera from the Spanish-speaking Community of Maryland, Inc. for their assistance in participant recruitment.
Footnotes
All participants except for one had a BDI-II score of 18 or higher, indicating at least mild depression. The remaining participant had a BDI-II score of 10. Results remained significant after re-conducting all analyses without this participant.
References
- Alegría M, Canino G, Ríos R, Vera M, Calderón J, Rusch D, Ortega AN. Mental health care for Latinos: Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino Whites. Psychiatric Services. 2002;53(12):1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- Areán PA, Gum A, McCulloch CE, Bostrom A, Gallagher-Thompson D, Thompson L. Treatment of depression in low-income older adults. Psychology And Aging. 2005;20(4):601–609. doi: 10.1037/0882-7974.20.4.601. [DOI] [PubMed] [Google Scholar]
- Barraca Mairal J, Pérez-Álvarez M, Lozano Bleda H. Avoidance and activation as keys to depression: Adaptation of the Behavioral Activation for Depression Scale (BADS) in a Spanish sample. The Spanish Journal of Psychology. 2011;14(2):998–1009. doi: 10.5209/rev_sjop.2011.v14.n2.45. [DOI] [PubMed] [Google Scholar]
- Bedregal L, Paris M, Añez L, Shahar G, Davidson L. Preliminary evaluation of the validity and reliability of the Spanish version of the Therapeutic Alliance with Clinician (TAC) questionnaire. Social Indicators Research. 2006;78(1):19–32. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory. 2nd ed. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Bell RA, Franks P, Duberstein PR, Epstein RM, Feldman MD, Garcia EF, Kravitz RL. Suffering in silence reasons for not disclosing depression in primary care. The Annals of Family Medicine. 2011;9(5):439–446. doi: 10.1370/afm.1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci D, Ory M, Czajkowski S. Enhancing Treatment Fidelity in Health Behavior Change Studies: Best Practices and Recommendations From the NIH Behavior Change Consortium. Health Psychology. 2004;23(5):443–451. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- Bickel R. Multilevel analysis for applied research: it's just regression! New York: Guilford Press; 2007. [Google Scholar]
- Blanco C, Patel SR, Liu L, Jiang H, Lewis-Fernández R, Schmidt AB, Liebowitz MR, Olfson M. National trends in ethnic disparities in mental health care. Medical Care. 2007;45(11):1012–1019. doi: 10.1097/MLR.0b013e3180ca95d3. [DOI] [PubMed] [Google Scholar]
- Caplan S, Escobar J, Paris M, Alvidrez J, Dixon JK, Desai MM, Scahill LD, Whittemore R. Cultural Influences on Causal Beliefs About Depression Among Latino Immigrants. Journal of Transcultural Nursing. 2013;24(1):68–77. doi: 10.1177/1043659612453745. [DOI] [PubMed] [Google Scholar]
- Carvalho JP, Gawrysiak MJ, Hellmuth JC, McNulty JK, Magidson JF, Lejuez CW, Hopko DR. The Reward Probability Index: Design and validation of a scale measuring access to environmental reward. Behavior Therapy. 2011;42(2):249–262. doi: 10.1016/j.beth.2010.05.004. [DOI] [PubMed] [Google Scholar]
- Carroll K, Nuro K. One size cannot fit all: A stage model for psychotherapy manual development. Clinical Psychology: Science and Practice. 2002;9(4):396–406. [Google Scholar]
- Collado A, MacPherson L, Risco C, Lejuez CW accepted for publication. Cultural Adaptation and Individual Tailoring: Two Approaches to the Development of Culturally-Responsive Treatment. [Letter to the editor] Primary Care Companion to the Journal of Clinical Psychiatry. doi: 10.4088/PCC.13l01540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comas-Díaz L. Effects of cognitive and behavioral group treatment on the depressive symptomatology of Puerto Rican women. Journal of Consulting and Clinical Psychology. 1981;49(5):627–632. doi: 10.1037//0022-006x.49.5.627. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Gonzales J, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, Wang NY, Ford DE. The acceptability of treatment for depression among African-American, Hispanic, and White primary care patients. Medical Care. 2003;41:479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, Warmerdam L. Behavioral treatment of depression: A meta-analysis of activity scheduling. Clinical Psychology Review. 2007;27:318–326. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Braun AR, Sargeant MN, Reynolds EK, Hopko DR, Blanco C, Lejuez CW. Effectiveness of a brief behavioral treatment for inner-city illicit drug users with elevated depressive symptoms: The Life Enhancement Treatment for Substance Use (LETS Act!) Journal Of Clinical Psychiatry. 2008;69(1):122–129. doi: 10.4088/jcp.v69n0116. [DOI] [PubMed] [Google Scholar]
- Ekers D, Richards D, Gilbody S. A meta-analysis of randomized trials of behavioural treatment of depression. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2008;38(5):611–623. doi: 10.1017/S0033291707001614. [DOI] [PubMed] [Google Scholar]
- Feliciano L, Arean PA. Mood disorders: Depressive disorders. In: Hersen M, Turner SM, Beidel DC, editors. Adult psychopathology and diagnosis. 5th ed. Hoboken, New Jersey: John Wiley & Sons, Inc; 2007. pp. 286–316. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. Nov, [Google Scholar]
- Floyd M, Scogin F, McKendree-Smith NL, Floyd DL, Rokke PD. Cognitive Therapy for Depression: A Comparison of Individual Psychotherapy and Bibliotherapy for Depressed Older Adults. Behavior Modification. 2004;28(2):297–318. doi: 10.1177/0145445503259284. [DOI] [PubMed] [Google Scholar]
- Folsom D, Gilmer T, Barrio C, Moore D, Bucardo J, Lindamer L, Garcia P, Hawthorne W, Hough R, Patterson T, Jeste DV. A longitudinal study of the use of mental health services by persons with serious mental illness: Do Spanish-speaking Latinos differ from English-speaking Latinos and Caucasians? The American Journal of Psychiatry. 2007;164(8):1173–1180. doi: 10.1176/appi.ajp.2007.06071239. [DOI] [PubMed] [Google Scholar]
- Fortuna LR, Alegria M, Gao S. Retention in depression treatment among ethnic and racial minority groups in the United States. Depression And Anxiety. 2010;27(5):485–494. doi: 10.1002/da.20685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fouad N, Bracken B. Cross-cultural translation and validation of two US psychoeducational assessment instruments. School Psychology International. 1986;7(3):167–172. [Google Scholar]
- Hedeker D, Mermelstein RJ. Analysis of Longitudinal Substance Use Outcomes Using Ordinal Random-Effects Regression Models. Addiction. 2000;95(3):381–394. doi: 10.1080/09652140020004296. [DOI] [PubMed] [Google Scholar]
- Hill CE, Thompson BJ, Williams EN. A guide to conducting consensual qualitative research. The Counseling Psychologist. 1997;25:517–572. [Google Scholar]
- Hopko DR, Lejuez CW, Ruggiero KJ, Eifert GH. Contemporary behavioral activation treatments for depression: Procedures, principles, and progress. Clinical Psychology Review. 2003;23:699–717. doi: 10.1016/s0272-7358(03)00070-9. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Small Clinical Trials: Issues and Challenges. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- Interian A, Allen L, Gara M, Escobar J. A pilot study of culturally adapted cognitive behavior therapy for Hispanics with major depression. Cognitive and Behavioral Practice. 2008;15(1):67–75. [Google Scholar]
- Interian A, Martinez I, Rios L, Krejci J, Guarnaccia PJ. Adaptation of a motivational interviewing intervention to improve antidepressant adherence among Latinos. Cultural Diversity And Ethnic Minority Psychology. 2010;16(2):215–225. doi: 10.1037/a0016072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanter JW, Mulick PS, Busch AM, Berlin KS, Martell CR. The Behavioral Activation for Depression Scale (BADS): Psychometric properties and factor structure. Journal of Psychopathology and Behavioral Assessment. 2007;29(3):191–202. [Google Scholar]
- Kanter JW, Santiago-Rivera AL, Rusch LC, Busch AM, West P. Initial outcomes of a culturally adapted behavioral activation for Latinas diagnosed with depression at a community clinic. Behavior Modification. 2010;34(2):120–144. doi: 10.1177/0145445509359682. [DOI] [PubMed] [Google Scholar]
- Karasz A, Watkins L. Conceptual models of treatment in depressed Hispanic patients. Annals of Family Medicine. 2006;4(6):527–533. doi: 10.1370/afm.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas K, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvale S. InterViews: An introduction to qualitative research interviewing. Thousand Oaks, CA US: Sage Publications, Inc; 1994. [Google Scholar]
- Lejuez CW, Hopko DR, Acierno R, Daughters SB, Pagoto SL. Ten year revision of the brief behavioral activation treatment for depression: Revised treatment manual. Behavior Modification. 2011;35(2):111–161. doi: 10.1177/0145445510390929. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, Hopko SD. A brief behavioral activation treatment for depression: Treatment manual. Behavior Modification. 2001;25(2):255–286. doi: 10.1177/0145445501252005. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM. A behavioral approach to depression. In: Friedman RM, Katz MM, editors. The psychology of depression: Contemporary theory and research. New York: Wiley; 1974. [Google Scholar]
- Magidson JF, Gorka SM, MacPherson L, Hopko DR, Blanco C, Lejuez CW, Daughters SB. Examining the effect of the Life Enhancement Treatment for Substance Use (LETS ACT) on residential substance abuse treatment retention. Addictive Behaviors. 2011;36(6):615–623. doi: 10.1016/j.addbeh.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzucchelli T, Kane R, Rees C. Behavioral activation treatments for depression in adults: A meta-analysis and review. Clinical Psychology: Science And Practice. 2009;16(4):383–411. [Google Scholar]
- Mendelson T, Rehkopf DH, Kubzansky LD. Depression among Latinos in the United States: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2008;76(3):355–366. doi: 10.1037/0022-006X.76.3.355. [DOI] [PubMed] [Google Scholar]
- Miranda J, Chung JY, Green BL, Krupnick J, Siddique J, Revicki DA, Belin T. Treating depression in predominantly low-income young minority women: A randomized controlled trial. JAMA: Journal of the American Medical Association. 2003;290(1):57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- Muñoz R, Ying Y, Pérez-Stable E, Miranda J. The prevention of depression: Research and practice. Baltimore, MD US: Johns Hopkins University Press; 1993. [Google Scholar]
- Organista KC. Latinos. In: White JR, Freeman AS, editors. Cognitive-behavioral group therapy. Washington, DC: American Psychological Association; 2000. pp. 281–303. [Google Scholar]
- Organista KC, Muñoz RF. Cognitive behavioral therapy with Latinos. Cognitive and Behavioral Practice. 1996;3:255–270. [Google Scholar]
- Pincay IE, Guarnaccia PJ. 'It's like going through an earthquake': Anthropological perspectives on depression among Latino immigrants. Journal of Immigrant and Minority Health. 2007;9(1):17–28. doi: 10.1007/s10903-006-9011-0. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and data analysis methods. 2nd ed. Thousand Oaks, California: Sage Publications; 2002. [Google Scholar]
- Rodriguez N, Myers HF, Mira C, Flores T, Garcia-Hernandez L. Development of the Multidimensional Acculturative Stress Inventory for adults of Mexican origin. Psychological Assessment. 2002;14(4):451–461. [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology: Science and Practice. 2001;8(2):133–142. [Google Scholar]
- Santiago-Rivera A, Kanter J, Benson G, Derose T, Illes R, Reyes W. Behavioral activation as an alternative treatment approach for Latinos with depression. Psychotherapy: Theory, Research, Practice, Training. 2008;45(2):173–185. doi: 10.1037/0033-3204.45.2.173. [DOI] [PubMed] [Google Scholar]
- Sanz J, Perdigón A, Vázquez C. Adaptación española del Inventario para la Depresión de Beck-ll (BDI-II): 2. Propiedades psicométricas en población general. Cliníca y Salud. 2003;14(3):249–280. [Google Scholar]
- Singer J, Willett J. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford, England: Oxford University Press; 2003. [Google Scholar]
- U. S. Census Bureau. Shin Hyon B, Bruno Rosalind., editors. Language Use and English-Speaking Ability: 2000. 2000 Retrieved from http://www.census.gov/prod/2003pubs/c2kbr-29.pdf on June 2, 2010.
- U. S. Census Bureau. The Hispanic Population: 2010. 2010 Census Briefs. 2010 Retrieved from http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf on October 2, 2011.
- U.S. Department of Health and Human Services. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: Washington, DC: Author; 2001. [Google Scholar]
- Vega W, Karno M, Alegria M, Alvidrez J, Bernal G, Escamilla M, Escobar J, Guarnaccia P, et al. Research issues for improving treatment of U.S. Hispanics with persistent mental disorders. Psychiatric Services. 2007;58(3):385–394. doi: 10.1176/ps.2007.58.3.385. [DOI] [PubMed] [Google Scholar]
- Vega WA, Kolody B, Aguilar-Gaxiola S, Alderete E, Catalano R, Caraveo-Anduaga J. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Archives of General Psychiatry. 1998;55:771–778. doi: 10.1001/archpsyc.55.9.771. [DOI] [PubMed] [Google Scholar]
- Vega W, Rodriguez M, Ang A. Addressing stigma of depression in Latino primary care patients. General Hospital Psychiatry. 2010;32(2):182–191. doi: 10.1016/j.genhosppsych.2009.10.008. [DOI] [PubMed] [Google Scholar]