Abstract
Antigen presenting cells (APCs), including macrophages and dendritic cells, are early and sustained targets of Ebola virus (EBOV) infection in vivo. Because EBOV activates mitogen-activated protein kinase (MAPK) signaling upon infection of APCs, we evaluated the effect of pyridinyl imidazole inhibitors of p38 MAPK on EBOV infection of human APCs and EBOV mediated cytokine production from human DCs. The p38 MAPK inhibitors reduced viral replication in PMA-differentiated macrophage-like human THP-1 cells with an IC50 of 4.73μM (SB202190), 8.26μM (p38kinhIII) and 8.21μM (SB203580) and primary human monocyte-derived dendritic cells (MDDCs) with an IC50 of 2.67μM (SB202190). Furthermore, cytokine production from EBOV-treated MDDCs was inhibited in a dose-dependent manner. A control pyridinyl imidazole compound failed to inhibit either EBOV infection or cytokine induction. Using an established EBOV virus-like particle (VLP) entry assay, we demonstrate that inhibitor pretreatment blocked VLP entry suggesting that the inhibitors blocked infection and replication at least in part by blocking EBOV entry. Taken together, our results indicate that pyridinyl imidazole p38 MAPK inhibitors may serve as leads for the development of therapeutics to treat EBOV infection.
Keywords: Ebola virus, p38 MAPK, inhibitor, dendritic cell, THP-1, entry, antigen-presenting cell
1. Introduction
Zaire Ebola virus (EBOV) is an enveloped, negative-sense RNA virus belonging to the family Filoviridae that causes an often fatal hemorrhagic disease in humans (Khan et al., 1998). Dendritic cells (DC) and macrophages, both antigen-presenting cells (APCs), are early and sustained targets of EBOV infection (Geisbert et al., 2003). It has been hypothesized that infection of APCs and their subsequent deregulation, which is manifested in part by uncontrolled secretion of inflammatory cytokines, leads to an ineffective antiviral host response (Bray and Geisbert, 2005; Martinez et al., 2012).
APCs exposed to EBOV or virus-like particles (VLPs) expressing the EBOV glycoprotein (GP) activate MAPK signaling (Martinez et al., 2007; Wahl-Jensen et al., 2011). Microarray analysis of human macrophages exposed to EBOV demonstrated the upregulation of genes known to be activated by p38 and ERK 1/2 MAPK signaling pathways (Wahl-Jensen et al., 2011). Furthermore, similar genes were upregulated from macrophages treated with non-replicating VLPs that express the VP40 protein and GP, consistent with a previous study demonstrating EBOV VLPs induce NF-κB and MAPK signaling in human DCs (Martinez et al., 2007). Further, overexpression of GP in 293 cells modulates MAPK activity (Zampieri et al., 2007). Importantly, an siRNA screen identified canonical phosphatidylinositol-3-kinase and MAPK signaling networks, among others, as important for EBOV infection (Kolokoltsov et al., 2009). Altogether these studies suggest that MAPK signaling plays an important role in EBOV infection of APCs.
Pyridinyl imidazole inhibitors of p38 MAPK exhibit anti-inflammatory properties and have been shown, for example, to block inflammatory cytokine production in the monocytic/macrophage cell line THP-1 (Gallagher et al., 1997; Lantos et al., 1984; Lee et al., 1988; Lee et al., 1999; Lee et al., 1994). Since exposure of APCs to EBOV has been shown to activate MAPKs, we sought to evaluate how inhibition of p38 MAPK signaling would influence EBOV infection. Furthermore, because p38 MAPK signaling mediates inflammatory cytokine production, and because EBOV infection is characterized as having a deregulated immune response, including deregulated cytokine production, we also tested if p38 MAPK inhibition would inhibit EBOV-induced cytokine production (Bray and Geisbert, 2005; Hoenen et al., 2006; Kumar et al., 2003). We show that p38 MAPK chemical inhibitors SB202190, SB203580 and p38inhk III impair EBOV replication and cytokine induction. Furthermore, target cell pretreatment with SB202190 blocked EBOV GP-mediated entry by inhibiting viral particle uptake suggesting that p38 MAPK inhibitors block EBOV infection, at least in part, by blocking the entry step of the virus.
2. Methods and Materials
2.1 Preparation of p38 MAPK inhibitors
p38 MAPK pyridinyl imidazole inhibitors SB202190, p38inhK III, SB203580; control compounds SB202474 (all from EMD Millipore, Billerica, MA) and 3-Deazaneplanocin A (DZNep) (kindly provided by Dr. Victor E. Marquez, National Cancer Institute) were prepared as 150mM stock concentrations in DMSO and diluted to final concentrations of 15uM to 1uM in 0.66% DMSO (Sigma Aldrich, St. Louis, MO).
2.2 Culture and differentiation of human THP-1 cells
THP-1 cells (ATCC, Catalogue # TIB-202) were grown in RPMI-1640 media (ATCC, Manassas, VA) supplemented with 10% FBS (Life Technologies, Carlsbad, CA) and 0.05mM 2-mercaptoethanol (Life Technologies, Carlsbad, CA) at 37°C, 5% CO2. Prior to infection, cells were plated in 96-well, black, clear bottom cell culture plates (Corning Catalog #3904) at a density of 5 × 104 cells per well in 100uL volume and differentiated overnight with 200 nM phorbol 12-myristate 13-acetate (PMA, Sigma Aldrich, St. Louis, MO).
2.3 EBOV Mayinga strain expressing enhanced green-fluorescent protein
All work with Ebola virus was performed at the United States Army Medical Research Institute of Infectious Diseases (USAMRIID) at Fort Detrick, Frederick, MD, USA within biosafety level 4 containment. A recombinant EBOV engineered to express enhanced green-fluorescent protein (Ebola virus H.sapiens-rec/COD/1976/Mayinga-eGFP) was used for all experiments utilizing infectious virus. The generation and rescue of the full-length eGFP clone (derived from an Ebola virus, family Filoviridae, species Zaire ebolavirus, GenBank accession No. NC002549) was described previously (Towner et al., 2005).
2.4 Antiviral activity assays in THP-1 cells
PMA-differentiated THP-1 cells were pretreated for 1 hour with p38 MAPK inhibitors prior to infection with EBOV-eGFP at a multiplicity of infection (MOI) of 0.1. At 2–3 days post-infection (PI), total GFP fluorescence was quantified per well using a SpectraMAX M5 Spectrofluorometer (Molecular Devices) at 515 nm as a measure of EBOV infection and replication.
2.5 Isolation and differentiation of monocytes
Peripheral blood mononuclear cells (PBMCs) were isolated by density gradient centrifugation (Histopaque; Sigma Aldrich, St. Louis, MO) from anonymous, blood bank blood (New York Blood Center). CD14+ cells were isolated immunomagnetically (Miltenyi Biotec, Auburn, CA) and cultured (0.7–1×106 cells/ml) in DC media (RPMI (Life Technologies, Carlsbad, CA) containing 100units/ml of penicillin, 100g/ml streptomycin, 55μM β-mercaptoethanol) and 4% human serum AB (GemCell, Gemini Bio-Products, West Sacramento, CA)) supplemented with 500 U/ml human granulocyte-macrophage colony-stimulating factor (GM-CSF; Peprotech, Rocky Hill, NJ), 500 U/ml human interleukin-4 (IL-4; Peprotech), 1 ng/mL ciproflaxocin (Sigma Aldrich, St. Louis, MO) for 5 to 7 days at 37°C to produce immature DCs. By day 5, immature DCs expressed surface CD11c and HLA-DR, but low to no CD14 (data not shown).
2.6 MDDCs treatment and infection
Prior to infection, MDDCs were pretreated with MAPK inhibitors at final concentrations ranging from 15 μM to 1 μM in 250μL total volume per well for approximately 1 hour. Human DCs were then infected using EBOV-eGFP at an MOI of 1 or 5 for 1 hour at 37°C and 5% CO2. After infection, cells were washed 3 times with PBS and replenished with media containing inhibitors. Cells were then incubated for 2–3 days, harvested by gently scraping the wells and 50000 events (cells/sample) were analyzed for GFP fluorescence by flow cytometry as a marker of EBOV infection.
2.7 Measurement of infectious virus by plaque assay
Supernatants harvested from THP-1 cells were assayed for infectious virus titer by preparing 10-fold dilutions in minimal essential medium containing 5% certified, United States origin, heat-inactivated fetal bovine serum (HI-FBS) (Life Technologies, Carlsbad, CA) and 1X Antibiotic-Antimycotic (Life Technologies, Carlsbad, CA). 200 uL of inoculum was added in triplicate to 6-well plates of Vero E6 cells at 95–100% confluence and incubated at 37°C in 5% CO2 for 1 hour with gentle rocking every 15 minutes. Following incubation, 2mL of primary overlay was added containing equal parts of 2X Modified Eagle medium (MEM, 2X Temin’s) (Gibco) supplemented with 10% Heat inactivated FBS, 4mM (2X) Glutamax (Life Technologies, Carlsbad, CA) and 2X Antibiotic-Antimycotic preheated to 37°C and 1% SeaKem ME Agarose (Lonza) that had been preheated to liquid and allowed to cool to 50°C. The overlay was allowed to solidify at room temperature and cells were placed back at 37°C and 5% CO2 for 7 days. Following incubation, 2 ml of secondary overlay containing a final concentration of 0.5% agarose and 4% Neutral Red solution (Life Technologies, Carlsbad, CA) was added to stain viable cells and visualize virus plaques. Cells were placed back in the incubator and plaques were counted the following day.
2.8 Cytokine quantification
MDDC supernatants were assayed for the presence of cytokines using a magnetic BioPlex Human Cytokine Group I 13-Plex Cytokine Assay (Bio-Rad) according to the manufacturer’s instructions. A standard curve was prepared by rehydrating pre-mixed, lyophilized cytokine standard provided with the assay kit followed by serial dilution. Assay plates were washed using a Bio-Plex Pro Wash II Station with a magnetic plate carrier attached. Data were acquired using a Bio-Rad Bio-Plex 3D system and analyzed using Bio-Plex Manager 6.0 software and a 5-parameter logarithmic fit.
2.9 Evaluating cell viability
Cell viability was determined by assaying cell supernatants for the presence of adenylate kinase using the ToxiLight cell viability kit (Lonza, Walkersville, MD). Positive control wells containing no viable cells were prepared using the ToxiLight 100% cell lysis reagent. Luminescence was read using a SpectraMAX M5 at a 1 second integration time. Percent viability was quantified by normalizing data to untreated cells and comparing cells cultured in the presence of inhibitors for 72 hours to cells prepared using the ToxiLight 100% cell lysis kit.
3.0 VLP production and isolation
293T cells were co-transfected by using Lipofectamine 2000 (Life Technologies, Carlsbad, CA) (ratio of 1:1 DNA:plasmid) and plasmids encoding EBOV VP40 fused to β-lactamase (pcDNA BLA-VP40) or EBOV VP40 fused to green fluorescent protein (pCAGGS GFP-VP40) and either EBOV GP or vesicular stomatitis virus glycoprotein (VSV G) at a ratio of 3:2 (VP40 to envelope glycoprotein plasmid). VLPs were harvested 3 days post-transfection and the 293T cell supernatant was purified by layering over 20% sucrose in NTE buffer (100 mM NaCl, 20 mM Tris-hydrochloride pH 7.5, and 1 mM ethylenediaminetetraacetic acid [EDTA]) and pelleting at 25,000 rpm in an SW-28 rotor (approximately 80,000 g) for 2 hours at 4°C. VLPs were then gently washed without resuspension with cold NTE or PBS and re-centrifuged. VLP were finally resuspended in a total of 150 μL NTE and stored on ice at 4°C prior to use.
3.1 Entry assays
Entry assays were performed as outlined in a previous study (Martinez et al., 2010). Briefly, different VLP preparations were normalized to equivalent levels of total β-lactamase activity. VLPs were added to target cells (105 cells/well/96 well plate) and centrifuged (“spinoculated”) at 1850 rpm in a tabletop centrifuge for 45 minutes at 4°C before incubation at 37°C in 2% RPMI medium for indicated times. Target cells were then loaded for 1 hour at room temperature with a fluorescent CCF2-AM substrate (Life Technologies, Carlsbad, CA) that accumulates in the cytosol. Cells were harvested and analyzed using the violet laser of an LSR II flow cytometer. Live cells were sorted (5000 events) using side scatter and forward scatter properties, to identify live cells. Cells were then assayed for green (uncleaved CCF2-AM substrate) or blue fluorescence, which occurs upon excitation of the cytosolic CCF2-AM substrate which is cleaved by VLP delivered β-lactamase. Those cells fluorescing blue as compared with control (for example, mock control) were scored as entry positive.
3. Results
3.1 p38 MAPK inhibitors block EBOV replication in differentiated THP-1 cells
We tested whether p38 MAPK inhibitors would affect EBOV replication and EBOV-induced cytokine production in human APCs. We first tested whether inhibitor treatment would block infection of the human THP-1 cell line, a model cell line for monocytes/macrophages. Although undifferentiated monocytic-like THP-1 human cells are nonpermissive for EBOV infection, phorbol 12-myristate-13 acetate (PMA)-treatment induces their differentiation into permissive macrophage-like cells (Dube et al., 2008; Martinez et al., 2013a).
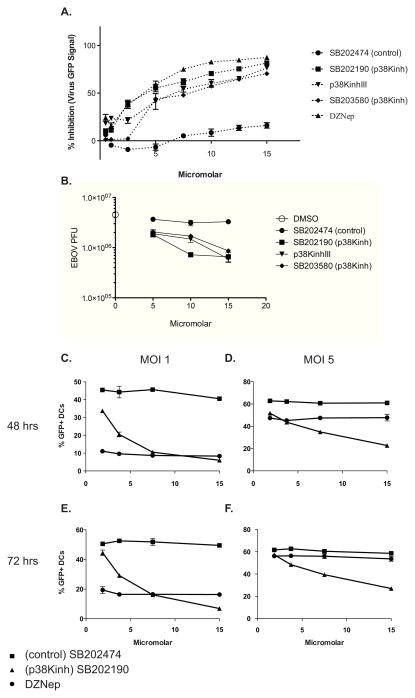
Differentiated THP-1 cells were infected at an MOI of 0.1 with recombinant EBOV expressing EBOV-eGFP (Towner et al., 2005). Pyridinyl imidazole p38MAPK inhibitors SB202190, p38inhK III, SB203580 as well as the control pyridinyl imidazole compound SB202474 that does not inhibit p38 MAPK, were added to cells approximately 1 hour prior to infection. DZNep, previously demonstrated to suppress EBOV replication in cell culture (Bray et al., 2000) served as a positive control for inhibition. 3 days post-infection cellular GFP fluorescence was assayed as a marker of viral replication. The data demonstrated inhibition by the p38 MAPK inhibitors (Figure 1A). The IC50 concentrations for each treatment, summarized in Table 1, further demonstrate significant inhibition by the p38 MAPK inhibitors but by not control compound SB202274. Cells were greater than 90% viable at all chemical concentrations tested, with the exception of SB202190, which yielded 82% viability at 15μM (data not shown). These experiments were repeated three times with similar results. Taken together, these data indicate that p38 MAPK inhibitors block EBOV replication. Cell supernatants were also measured for infectious virus by plaque assay following infection at a multiplicity of 0.1. Modest inhibition was seen in the presence of the p38 MAPK inhibitors, but not the control inhibitor, correlating with the GFP expression data (Figure 1B). The inhibition was dose-dependent with greater antiviral activity at the higher concentrations. A significant reduction in viral output, as compared to the control, was only seen with concentrations of greater than 5μM. Pretreatment with 10μM of p38 MAPK inhibitors SB202190 resulted in a slightly greater than half-log reduction in viral titer. Pretreatment using 15μM of each of the p38 MAPK inhibitors demonstrated similar suppression of replication. Since p38 MAPK inhibitor SB202190 consistently demonstrated the greatest inhibitory activity (Figure 1 and Table 1) this inhibitor was selected for use in subsequent experiments.
Figure 1. Methylsulfanylimidazole inhibitors of p38 MAPK inhibit Ebola virus replication in THP-1 cells and human MDDCs.
(A) THP-1 cells were seeded in triplicate in 96-well cell culture plates and pretreated with DZNEP, control compound SB202474, or the p38 MAPK inhibitors SB202190, p38inhK III or SB203580 at decreasing concentrations. Cells were then infected with recombinant Ebola virus expressing eGFP (EBOV-eGFP) at a MOI of 0.1 and incubated at 37°C, 5% CO2 for 3 days prior to fluorescent measurement at 515 nm. Inhibitor effect is expressed as % inhibition of infected, untreated THP-1 cells. (B) Supernatants from DMSO, control SB202474 and p38 MAPK SB202190, p38inhK III, SB203580 inhibitor-treated THP-1s three days post-infection with EBOVGFP were tested for EBOV titers by plaque assay. Plaque-forming units (PFU) are shown for supernatants. Human monocyte-derived dendritic cells (MDDCs) were pretreated with DZNEP, control compound SB202474 or p38 MAPK inhibitor SB202190 at decreasing concentrations. Cells were then infected in triplicate with EBOV-eGFP at an MOI of 1 (C and E) and 5 (D and F), the cells were washed to remove free virus and fresh media containing inhibitors was replaced. Cells were harvested at 48 (C and D) and 72 (E and F) hours and percentage of GFP+ MDDCs is shown.
Table 1.
IC50 of tested compounds in MDDCs and differentiated THP-1 cells.
| Compound | Target cell inhibition a | |
|---|---|---|
| Differentiated THP-1 | MDDCs | |
| SB202190 | 4.7μM | 2.7μM |
| SB203580 | 8.2μM | ND |
| p38KinhIII | 8.3μM | ND |
| DZNep | 3.4μM | <1μM |
| SB202474 | >15μM | >15μM |
IC50 values, as determined by inhibition of GFP expression by EBOV-GFP, were calculated for p38 MAPK inhibitors and controls using Graphpad Prism 5.0 software. ND- not determined
3.2 p38 MAPK inhibitor SB 202190 inhibits EBOV replication in human MDDCs
Next we sought to determine if p38 MAPK inhibition would similarly block EBOV infection of primary MDDCs. Human MDDCs were infected in triplicate with EBOV-eGFP at an MOI of 1 or 5 for either 48 or 72 hours in the presence of decreasing concentrations p38 MAPK inhibitors. Two relatively high MOIs were utilized to determine if the magnitude of viral input affected the result and because infectivity of DCs is lower than on Vero cells where the virus was originally titered. DZNep and control pyridinyl imidazole SB202474 were used as positive and negative controls, respectively. At each indicated time point, cells were harvested and GFP fluorescence was quantified by flow cytometry as a correlate of viral infection and replication. Figure 1(C–F) shows the percentage of infected (% GFP positive) MDDCs at MOIs of 1 and 5 at 48 and 72 PI. After 48 hours at MOI of 1, SB202190 treatment reduced the number of GFP fluorescent cells from about 50% to roughly 10% at concentrations ranging from 7.5μM to 15μM. While less profound, the percentage of fluorescent cells was also decreased at the lower concentrations assayed. This trend was reproduced at the 72-hour time point for the MOI of 1, although the overall percentage of GFP-positive cells was higher (maximum GFP-positive cells was 60% rather than 50%) for both SB202190 and control treated cultures (Figure 1C & 1E). At the higher MOI of 5, the inhibition was less prominent, particularly at lower concentrations of compound, but a dose dependent inhibition was maintained. At the 48-hour time point at MOI of 5, the 7.5μM and 15μM concentrations of SB202190 reduced the percentage of GFP-positive cells from 60% to 35% and 20%, respectively (Figure 1D). Unlike the infections performed using an MOI of 1, extending the infection to 72 hours at the higher MOI did not result in an increase in the percentage of GFP-positive cells. At an MOI of 5, DZNep also had a much weaker inhibitory effect than at an MOI of 1 (Figure 1C–F). All inhibitor concentrations tested resulted in greater than 96% viability in MDDCs (data not shown). These data demonstrate that the p38 MAPK inhibitor SB202190, but not the control compound, inhibits EBOV replication in primary human MDDCs (IC50 of 2.67μM, Table 1) as was observed in the THP-1 model.
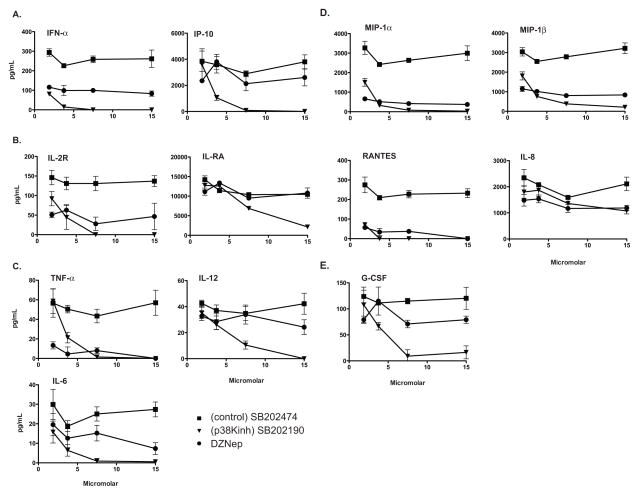
3.3 p38 MAPK inhibitor treatment of MDDCs inhibits EBOV induced cytokine production
To evaluate the effect of p38 MAPK inhibitor treatment on cytokine production, MDDCs pre-treated with DZNep, control SB202474 or p38 MAPK inhibitor SB202190 were infected with EBOV-eGFP (MOI=1), and the supernatants were analyzed for cytokine production 48 hours later. The levels of IFN-α and the IFN-induced cytokine IP-10, as well as the proinflammatory cytokines TNF-α, IL-6, IL-12, and cytokine antagonists IL-2R and IL-1RA were determined (Figure 2A–C).
Figure 2. p38 MAPK inhibitor SB 202190 inhibits cytokine production from EBOV treated MDDCs.
Supernatants from DZNEP, control SB202474 and p38 MAPK SB202190 inhibitor-treated MDDCs forty-eight hours PI with (MOI 1) EBOV-eGFP were tested for the levels of (A) interferon-alpha and IP-10, (B) IL-2R and IL-1RA as well as (C) TNF-α, IL-6 and IL-12, (D) chemokines MIP-1, MIP-1beta, IL-8 and RANTES and (E) G-CSF.
IFN-α and IP-10 production were potently suppressed by SB202190 treatment relative to control compound SB202474 (Figure 2A). The suppression by SB202190 treatment exceeded that mediated by DZNep (Figure 2A), despite the effective inhibition of virus replication by this compound (Table 1 and Figure 1). Although relatively low levels of TNFα, IL-6 and IL-12 were detected, SB202190 also reduced these cytokines in the supernatants. For these, significant suppression relative to control SB202474, was again seen at drug concentrations that did not result in effective inhibition of EBOV-eGFP replication.
Additionally, because hypersecretion of chemokines and growth factors has been associated with fatal outcome in human cases (Wauquier et al., 2010), the levels of G-CSF, MIP-1α, MIP-1β, IL-8 and RANTES were also measured (Figure 2D, E). SB202190 effectively inhibited MIP-1a, MIP-1b and RANTES production even at drug concentrations as low as 3.75μM, while significant inhibition of G-CSF was seen at 15 μM.
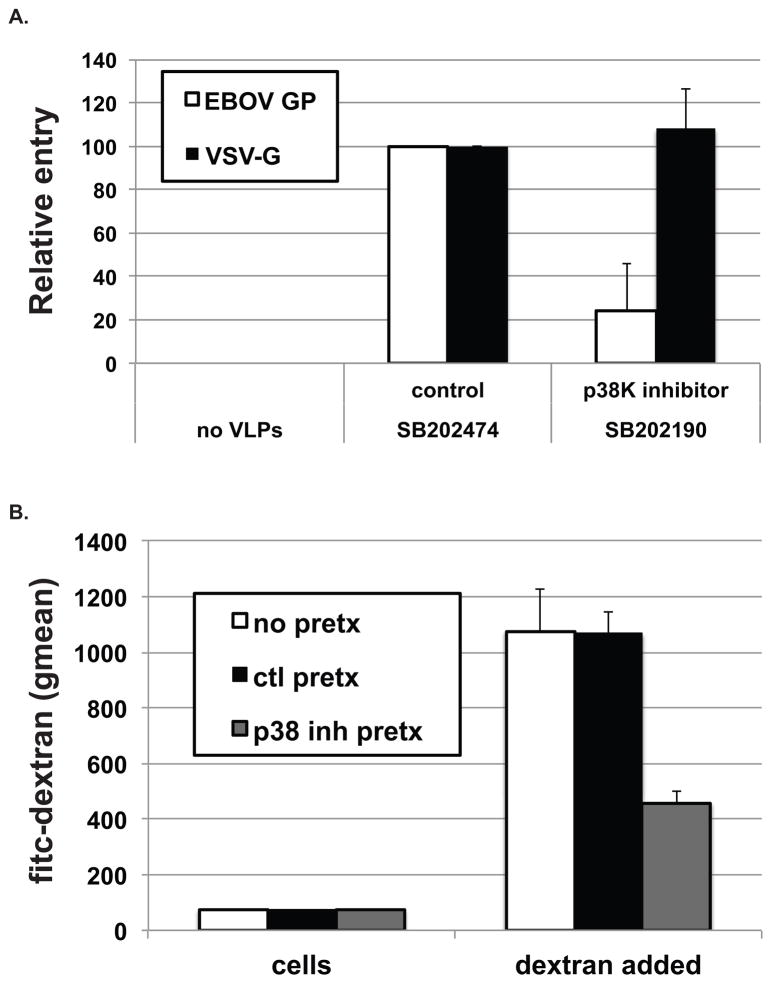
3.4 p38 MAPK inhibitor SB202190 blocks EBOV GP, but not VSV G mediated entry into human MDDCs
We next tested whether p38 MAPK inhibition could block EBOV at the level of entry by using an established virus-like particle (VLP)-based assay (Martinez et al., 2010; Martinez et al., 2013b; Simmons et al., 2003). MDDCs were pretreated for 30 minutes with 10μM of control SB202474 or p38 MAPK inhibitor SB202190. After drug treatment, MDDCs were incubated with VLPs pseudotyped with EBOV GP or VSV G and assayed for entry (Figure 3A). Shown is the relative entry normalized to the entry seen in control compound treated cells. The relative amount of EBOV GP, but not VSV G mediated entry was substantially reduced in p38 MAPK inhibitor SB202190-pretreated MDDCs. This experiment was repeated and similar results were obtained. These results suggest that the block in MDDC EBOV infection and replication may be due in part to a block of viral entry.
Figure 3. p38 MAPK Inhibitor SB 202190 inhibits EBOV GP-mediated, but not VSV G mediated entry into human DCs.
Human DCs were pretreated with 10-μM mock, control SB202474 or p38 MAPK SB202190. An entry assay was performed using virus-like particles (VLPs) that contained a chimeric VP40-β-lactamase enzyme. VLPs pseudotyped with either EBOV GP or VSV G were incubated with human DCs for 3.5 hours. Cells were then loaded with a cytoplasmic substrate that fluoresces blue upon cleavage by β-lactamase. Cells whose cytoplasm is penetrated by VLPs (entry positive) will fluoresce blue when assayed by flow cytometry. The number of cells positive for EBOV-GP (blue bar) and VSV G (black bar) mediated entry in the presence of control inhibitor was set at 100. This experiment was repeated with similar results. Shown is the average of four replicates.
3.5 p38 MAPK inhibitor SB202190, but not control, inhibits human MDDC uptake of FITC-dextran
EBOV is endocytosed into cells via macropinocytosis (Aleksandrowicz et al., 2011; Hunt et al., 2011; Mulherkar et al., 2011; Nanbo et al., 2010; Saeed et al., 2010). One possible mechanism by which the p38 MAPK inhibitors might affect EBOV entry would be through inhibition of macropinocytosis. We therefore tested whether uptake of FITC-dextran (10KDa), an indicator of macropinocytosis, is affected by 30 minute pre-treatment with 10μM of control SB202474 or p38 MAPK inhibitor SB202190. MDDCs were incubated with FITC-dextran for 30 minutes at 37°C, washed and then assayed for VLP binding and uptake (Figure 3B). Uptake by SB202190-pretreated MDDCs was significantly less efficient (approximately 60% decrease) as compared to mock and control pretreated MDDCs. Taken together, these data suggest that the p38 MAPK inhibitor-induced block in viral entry occurs in part due to a block in endocytosis.
4. Discussion
EBOV disease is associated with excessive inflammatory cytokine production, therefore, therapies that control this host response might prove beneficial. However, suppression of inflammation could also promote virus replication. Our study identifies small molecules that block the viral-induced production of potentially damaging inflammatory cytokine response while also suppressing virus replication. The development of drugs that could potently suppress replication while also decreasing inflammation could mitigate concerns that the immune suppressing activity would lead to uncontrolled virus spread. Therefore, this study suggests a unique strategy for anti-filovirus therapeutic development.
We examined the impact of the p38 MAPKs on EBOV infection in macrophages and DCs because these cells play a critical role in the pathogenesis of EBOV the disease. These cells are infected in vivo. For example, Geisbert et al. demonstrated that in infected cynomolgus macaques, DCs stain positive for EBOV antigen early after infection and throughout the course of disease, suggesting that DCs are both early and sustained targets of viral infection (Geisbert et al., 2003). In vitro, EBOV productively infects primary monocytes, macrophages and DCs and leads to their deregulation (Bosio et al., 2003; Feldmann et al., 1996; Mahanty et al., 2003; Stroher et al., 2001; Wahl-Jensen et al., 2011). That p38 MAPK signaling is important for EBOV replication in macrophages and DCs has precedence. EBOV infection induces MAPK signaling cascades in a GP-dependent manner (Martinez et al., 2007; Wahl-Jensen et al., 2011), and p38 MAPK is thought to play dual roles in DC maturation and induction of inflammatory cytokines (Ayala et al., 2000; Lee et al., 2009; Terrazas et al., 2011).
p38 MAPK signaling is activated in response to, among other things, environmental stress (Risco and Cuenda, 2012; Roux and Blenis, 2004) and plays an important role in a number of viral infections. For example, p38 MAPK activation and signaling is important for viral entry of reovirus and respiratory virus (Huang et al., 2011; Marchant et al., 2010). p38 MAPK signaling has also been implicated as playing a role in the viral transcription and translation of a number of viruses including hepatitis C virus, avian reovirus, porcine circovirus type 2, porcine reproductive and respiratory syndrome virus, rotavirus, Kaposi sarcoma-associated herpesvirus, encephalomyocarditis virus and HIV-1 (Cohen et al., 1997; George et al., 2012; Hirasawa et al., 2003; Jafri et al., 2007; Ji et al., 2009; Lee and Lee, 2012; Pan et al., 2006; Wei et al., 2009); and inhibition of p38 MAPK signaling has been shown to directly inhibit virus infection (Chang et al., 2008; Ludwig et al., 2003; Wei et al., 2009). EBOV infection induces MAPK signaling cascades in a GP-dependent manner, and p38 MAPK is thought to play dual roles in DC maturation and induction of inflammatory cytokines (Ayala et al., 2000; Lee et al., 2009; Terrazas et al., 2011). These facts motivated our analysis of p38 MAPK inhibitors on viral replication and entry. Our data identify inhibition of viral entry as one mechanism contributing to suppression of EBOV replication. This is likely due, at least in part, to suppression of macropinocytosis of virus particles, based on the FITC-dextran uptake assay. However, based on the available data, we also cannot exclude a contribution from other post-entry inhibitory mechanisms.
The p38 MAPK inhibitors tested here suppressed EBOV-induced cytokine production. That this does not simply reflect suppression of virus infection by the compounds is based upon the observation that DZNep, which more potently suppressed replication, was less effective than SB202190 in suppressing cytokine responses (Figure 2). Furthermore, p38 MAPK inhibitors are known to inhibit inflammatory responses (Han et al., 1994; Kumar et al., 2003; Lee et al., 1994). Fatal outcome in EBOV infection is associated with the presence of high levels of inflammatory cytokines (Wauquier et al., 2010). In vitro, infected macrophages produce excess levels of inflammatory cytokines that increase vascular endothelial cell junction permeability (Feldmann et al., 1996). Furthermore, induction of chemokines from infected macrophages has been been postulated to play a role in recruitment of additional targets of viral infection (Baize et al., 2002; Bray and Geisbert, 2005). Because p38 MAPK signaling is linked to inflammatory disease (reviewed in (Schieven, 2005, 2009)) and pyridinyl imidazole p38 MAPK inhibitors have been shown to exhibit anti-inflammatory activities (Gallagher et al., 1997; Lantos et al., 1984; Lee et al., 1988; Lee et al., 1999; Lee et al., 1994), we tested how p38 MAPK inhibitors might affect EBOV-induced cytokine and chemokine secretion. We show that p38 MAPK inhibitors ablated proinflammatory cytokine, chemokine and growth factor production from EBOV treated MDDCs at similar concentrations as were previously used to inhibit APC cytokine production (Mikkelsen et al., 2009; Mitchell et al., 2010; Puig-Kroger et al., 2001; Wilflingseder et al., 2004). Therefore, these findings suggest a potential therapeutic role for p38 MAPK pyridinyl imidazole inhibitors or derivatives of these compounds for the treatment of EBOV infection via multiple mechanisms: blocking or impairing EBOV infection of target APCs, as well as countering the detrimental inflammatory cytokine response generated by any escaping virus.
Highlights.
Pyridinyl imidazole inhibitors of p38 MAP kinases inhibit ebolavirus replication in macrophages and dendritic cells
Pyridinyl imidazole inhibitors of p38 MAP kinases inhibit ebolavirus induced cytokine production
Pyridinyl imidazole inhibitors of p38 MAP kinases inhibit Zaire ebolavirus entry into dendritic cells
Acknowledgments
This work was supported by NIH grants AI097568, AI109664 and AI057158 (Northeast Biodefense Center-Lipkin) to C.F.B. We thank Dr. Victor E. Marquez (National Cancer Institute) for providing DZNep.
Footnotes
Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the U.S. Army.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aleksandrowicz P, Marzi A, Biedenkopf N, Beimforde N, Becker S, Hoenen T, Feldmann H, Schnittler HJ. Ebola virus enters host cells by macropinocytosis and clathrin-mediated endocytosis. The Journal of infectious diseases. 2011;204(Suppl 3):S957–967. doi: 10.1093/infdis/jir326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayala JM, Goyal S, Liverton NJ, Claremon DA, O’Keefe SJ, Hanlon WA. Serum-induced monocyte differentiation and monocyte chemotaxis are regulated by the p38 MAP kinase signal transduction pathway. J Leukoc Biol. 2000;67:869–875. [PubMed] [Google Scholar]
- Baize S, Leroy EM, Georges AJ, Georges-Courbot MC, Capron M, Bedjabaga I, Lansoud-Soukate J, Mavoungou E. Inflammatory responses in Ebola virus-infected patients. Clinical and experimental immunology. 2002;128:163–168. doi: 10.1046/j.1365-2249.2002.01800.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosio CM, Aman MJ, Grogan C, Hogan R, Ruthel G, Negley D, Mohamadzadeh M, Bavari S, Schmaljohn A. Ebola and Marburg viruses replicate in monocyte-derived dendritic cells without inducing the production of cytokines and full maturation. The Journal of infectious diseases. 2003;188:1630–1638. doi: 10.1086/379199. [DOI] [PubMed] [Google Scholar]
- Bray M, Driscoll J, Huggins JW. Treatment of lethal Ebola virus infection in mice with a single dose of an S-adenosyl-L-homocysteine hydrolase inhibitor. Antiviral Res. 2000;45:135–147. doi: 10.1016/s0166-3542(00)00066-8. [DOI] [PubMed] [Google Scholar]
- Bray M, Geisbert TW. Ebola virus: the role of macrophages and dendritic cells in the pathogenesis of Ebola hemorrhagic fever. The international journal of biochemistry & cell biology. 2005;37:1560–1566. doi: 10.1016/j.biocel.2005.02.018. [DOI] [PubMed] [Google Scholar]
- Chang WW, Su IJ, Chang WT, Huang W, Lei HY. Suppression of p38 mitogen-activated protein kinase inhibits hepatitis B virus replication in human hepatoma cell: the antiviral role of nitric oxide. Journal of viral hepatitis. 2008;15:490–497. doi: 10.1111/j.1365-2893.2007.00968.x. [DOI] [PubMed] [Google Scholar]
- Cohen PS, Schmidtmayerova H, Dennis J, Dubrovsky L, Sherry B, Wang H, Bukrinsky M, Tracey KJ. The critical role of p38 MAP kinase in T cell HIV-1 replication. Molecular medicine (Cambridge, Mass) 1997;3:339–346. [PMC free article] [PubMed] [Google Scholar]
- Dube D, Schornberg KL, Stantchev TS, Bonaparte MI, Delos SE, Bouton AH, Broder CC, White JM. Cell adhesion promotes Ebola virus envelope glycoprotein-mediated binding and infection. J Virol. 2008;82:7238–7242. doi: 10.1128/JVI.00425-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldmann H, Bugany H, Mahner F, Klenk HD, Drenckhahn D, Schnittler HJ. Filovirus-induced endothelial leakage triggered by infected monocytes/macrophages. J Virol. 1996;70:2208–2214. doi: 10.1128/jvi.70.4.2208-2214.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher TF, Seibel GL, Kassis S, Laydon JT, Blumenthal MJ, Lee JC, Lee D, Boehm JC, Fier-Thompson SM, Abt JW, Soreson ME, Smietana JM, Hall RF, Garigipati RS, Bender PE, Erhard KF, Krog AJ, Hofmann GA, Sheldrake PL, McDonnell PC, Kumar S, Young PR, Adams JL. Regulation of stress-induced cytokine production by pyridinylimidazoles; inhibition of CSBP kinase. Bioorg Med Chem. 1997;5:49–64. doi: 10.1016/s0968-0896(96)00212-x. [DOI] [PubMed] [Google Scholar]
- Geisbert TW, Hensley LE, Larsen T, Young HA, Reed DS, Geisbert JB, Scott DP, Kagan E, Jahrling PB, Davis KJ. Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. The American journal of pathology. 2003;163:2347–2370. doi: 10.1016/S0002-9440(10)63591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George A, Panda S, Kudmulwar D, Chhatbar SP, Nayak SC, Krishnan HH. Hepatitis C virus NS5A binds to the mRNA cap-binding eukaryotic translation initiation 4F (eIF4F) complex and up-regulates host translation initiation machinery through eIF4E-binding protein 1 inactivation. The Journal of biological chemistry. 2012;287:5042–5058. doi: 10.1074/jbc.M111.308916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han J, Lee JD, Bibbs L, Ulevitch RJ. A MAP kinase targeted by endotoxin and hyperosmolarity in mammalian cells. Science. 1994;265:808–811. doi: 10.1126/science.7914033. [DOI] [PubMed] [Google Scholar]
- Hirasawa K, Kim A, Han HS, Han J, Jun HS, Yoon JW. Effect of p38 mitogen-activated protein kinase on the replication of encephalomyocarditis virus. J Virol. 2003;77:5649–5656. doi: 10.1128/JVI.77.10.5649-5656.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoenen T, Groseth A, Falzarano D, Feldmann H. Ebola virus: unravelling pathogenesis to combat a deadly disease. Trends in molecular medicine. 2006;12:206–215. doi: 10.1016/j.molmed.2006.03.006. [DOI] [PubMed] [Google Scholar]
- Huang WR, Wang YC, Chi PI, Wang L, Wang CY, Lin CH, Liu HJ. Cell entry of avian reovirus follows a caveolin-1-mediated and dynamin-2-dependent endocytic pathway that requires activation of p38 mitogen-activated protein kinase (MAPK) and Src signaling pathways as well as microtubules and small GTPase Rab5 protein. The Journal of biological chemistry. 2011;286:30780–30794. doi: 10.1074/jbc.M111.257154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt CL, Kolokoltsov AA, Davey RA, Maury W. The Tyro3 receptor kinase Axl enhances macropinocytosis of Zaire ebolavirus. J Virol. 2011;85:334–347. doi: 10.1128/JVI.01278-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jafri M, Donnelly B, McNeal M, Ward R, Tiao G. MAPK signaling contributes to rotaviral-induced cholangiocyte injury and viral replication. Surgery. 2007;142:192–201. doi: 10.1016/j.surg.2007.03.008. [DOI] [PubMed] [Google Scholar]
- Ji WT, Lee LH, Lin FL, Wang L, Liu HJ. AMP-activated protein kinase facilitates avian reovirus to induce mitogen-activated protein kinase (MAPK) p38 and MAPK kinase 3/6 signalling that is beneficial for virus replication. The Journal of general virology. 2009;90:3002–3009. doi: 10.1099/vir.0.013953-0. [DOI] [PubMed] [Google Scholar]
- Khan AS, Sanchez A, Pflieger AK. Filoviral haemorrhagic fevers. British medical bulletin. 1998;54:675–692. doi: 10.1093/oxfordjournals.bmb.a011719. [DOI] [PubMed] [Google Scholar]
- Kolokoltsov AA, Saeed MF, Freiberg AN, Holbrook MR, Davey RA. Identification of novel cellular targets for therapeutic intervention against Ebola virus infection by siRNA screening. Drug development research. 2009;70:255–265. doi: 10.1002/ddr.20303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S, Boehm J, Lee JC. p38 MAP kinases: key signalling molecules as therapeutic targets for inflammatory diseases. Nature reviews Drug discovery. 2003;2:717–726. doi: 10.1038/nrd1177. [DOI] [PubMed] [Google Scholar]
- Lantos I, Bender PE, Razgaitis KA, Sutton BM, DiMartino MJ, Griswold DE, Walz DT. Antiinflammatory activity of 5,6-diaryl-2,3-dihydroimidazo[2,1-b]thiazoles. Isomeric 4-pyridyl and 4-substituted phenyl derivatives. J Med Chem. 1984;27:72–75. doi: 10.1021/jm00367a014. [DOI] [PubMed] [Google Scholar]
- Lee JC, Griswold DE, Votta B, Hanna N. Inhibition of monocyte IL-1 production by the anti-inflammatory compound, SK&F 86002. Int J Immunopharmacol. 1988;10:835–843. doi: 10.1016/0192-0561(88)90007-0. [DOI] [PubMed] [Google Scholar]
- Lee JC, Kassis S, Kumar S, Badger A, Adams JL. p38 mitogen-activated protein kinase inhibitors--mechanisms and therapeutic potentials. Pharmacol Ther. 1999;82:389–397. doi: 10.1016/s0163-7258(99)00008-x. [DOI] [PubMed] [Google Scholar]
- Lee JC, Laydon JT, McDonnell PC, Gallagher TF, Kumar S, Green D, McNulty D, Blumenthal MJ, Heys JR, Landvatter SW, et al. A protein kinase involved in the regulation of inflammatory cytokine biosynthesis. Nature. 1994;372:739–746. doi: 10.1038/372739a0. [DOI] [PubMed] [Google Scholar]
- Lee JY, Kim H, Cha MY, Park HG, Kim YJ, Kim IY, Kim JM. Clostridium difficile toxin A promotes dendritic cell maturation and chemokine CXCL2 expression through p38, IKK, and the NF-kappaB signaling pathway. J Mol Med (Berl) 2009;87:169–180. doi: 10.1007/s00109-008-0415-2. [DOI] [PubMed] [Google Scholar]
- Lee YJ, Lee C. Stress-activated protein kinases are involved in porcine reproductive and respiratory syndrome virus infection and modulate virus-induced cytokine production. Virology. 2012;427:80–89. doi: 10.1016/j.virol.2012.02.017. [DOI] [PubMed] [Google Scholar]
- Ludwig S, Planz O, Pleschka S, Wolff T. Influenza-virus-induced signaling cascades: targets for antiviral therapy? Trends in molecular medicine. 2003;9:46–52. doi: 10.1016/s1471-4914(02)00010-2. [DOI] [PubMed] [Google Scholar]
- Mahanty S, Hutchinson K, Agarwal S, McRae M, Rollin PE, Pulendran B. Cutting edge: impairment of dendritic cells and adaptive immunity by Ebola and Lassa viruses. Journal of immunology (Baltimore, Md: 1950) 2003;170:2797–2801. doi: 10.4049/jimmunol.170.6.2797. [DOI] [PubMed] [Google Scholar]
- Marchant D, Singhera GK, Utokaparch S, Hackett TL, Boyd JH, Luo Z, Si X, Dorscheid DR, McManus BM, Hegele RG. Toll-like receptor 4-mediated activation of p38 mitogen-activated protein kinase is a determinant of respiratory virus entry and tropism. J Virol. 2010;84:11359–11373. doi: 10.1128/JVI.00804-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, Johnson J, Manicassamy B, Rong L, Olinger GG, Hensley LE, Basler CF. Zaire Ebola virus entry into human dendritic cells is insensitive to cathepsin L inhibition. Cell Microbiol. 2010;12:148–157. doi: 10.1111/j.1462-5822.2009.01385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, Johnson JC, Honko A, Yen B, Shabman RS, Hensley LE, Olinger GG, Basler CF. Ebola virus exploits a monocyte differentiation program to promote its entry. J Virol. 2013a;87:3801–3814. doi: 10.1128/JVI.02695-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, Leung LW, Basler CF. The role of antigen-presenting cells in filoviral hemorrhagic fever: gaps in current knowledge. Antiviral Res. 2012;93:416–428. doi: 10.1016/j.antiviral.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, Ndungo E, Tantral L, Miller EH, Leung LW, Chandran K, Basler CF. A mutation in the Ebola virus envelope glycoprotein restricts viral entry in a host species- and cell-type-specific manner. J Virol. 2013b;87:3324–3334. doi: 10.1128/JVI.01598-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, Valmas C, Basler CF. Ebola virus-like particle-induced activation of NF-kappaB and Erk signaling in human dendritic cells requires the glycoprotein mucin domain. Virology. 2007;364:342–354. doi: 10.1016/j.virol.2007.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikkelsen SS, Jensen SB, Chiliveru S, Melchjorsen J, Julkunen I, Gaestel M, Arthur JS, Flavell RA, Ghosh S, Paludan SR. RIG-I-mediated activation of p38 MAPK is essential for viral induction of interferon and activation of dendritic cells: dependence on TRAF2 and TAK1. The Journal of biological chemistry. 2009;284:10774–10782. doi: 10.1074/jbc.M807272200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell D, Yong M, Schroder W, Black M, Tirrell M, Olive C. Dual stimulation of MyD88-dependent Toll-like receptors induces synergistically enhanced production of inflammatory cytokines in murine bone marrow-derived dendritic cells. The Journal of infectious diseases. 2010;202:318–329. doi: 10.1086/653499. [DOI] [PubMed] [Google Scholar]
- Mulherkar N, Raaben M, de la Torre JC, Whelan SP, Chandran K. The Ebola virus glycoprotein mediates entry via a non-classical dynamin-dependent macropinocytic pathway. Virology. 2011;419:72–83. doi: 10.1016/j.virol.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanbo A, Imai M, Watanabe S, Noda T, Takahashi K, Neumann G, Halfmann P, Kawaoka Y. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS pathogens. 2010;6:e1001121. doi: 10.1371/journal.ppat.1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan H, Xie J, Ye F, Gao SJ. Modulation of Kaposi’s sarcoma-associated herpesvirus infection and replication by MEK/ERK, JNK, and p38 multiple mitogen-activated protein kinase pathways during primary infection. J Virol. 2006;80:5371–5382. doi: 10.1128/JVI.02299-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puig-Kroger A, Relloso M, Fernandez-Capetillo O, Zubiaga A, Silva A, Bernabeu C, Corbi AL. Extracellular signal-regulated protein kinase signaling pathway negatively regulates the phenotypic and functional maturation of monocyte-derived human dendritic cells. Blood. 2001;98:2175–2182. doi: 10.1182/blood.v98.7.2175. [DOI] [PubMed] [Google Scholar]
- Risco A, Cuenda A. New Insights into the p38gamma and p38delta MAPK Pathways. Journal of signal transduction. 2012;2012:520289. doi: 10.1155/2012/520289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux PP, Blenis J. ERK and p38 MAPK-activated protein kinases: a family of protein kinases with diverse biological functions. Microbiology and molecular biology reviews: MMBR. 2004;68:320–344. doi: 10.1128/MMBR.68.2.320-344.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed MF, Kolokoltsov AA, Albrecht T, Davey RA. Cellular entry of ebola virus involves uptake by a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes. PLoS pathogens. 2010;6:e1001110. doi: 10.1371/journal.ppat.1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schieven GL. The biology of p38 kinase: a central role in inflammation. Current topics in medicinal chemistry. 2005;5:921–928. doi: 10.2174/1568026054985902. [DOI] [PubMed] [Google Scholar]
- Schieven GL. The p38alpha kinase plays a central role in inflammation. Current topics in medicinal chemistry. 2009;9:1038–1048. doi: 10.2174/156802609789630974. [DOI] [PubMed] [Google Scholar]
- Simmons G, Rennekamp AJ, Chai N, Vandenberghe LH, Riley JL, Bates P. Folate receptor alpha and caveolae are not required for Ebola virus glycoprotein-mediated viral infection. J Virol. 2003;77:13433–13438. doi: 10.1128/JVI.77.24.13433-13438.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroher U, West E, Bugany H, Klenk HD, Schnittler HJ, Feldmann H. Infection and activation of monocytes by Marburg and Ebola viruses. J Virol. 2001;75:11025–11033. doi: 10.1128/JVI.75.22.11025-11033.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terrazas CA, Huitron E, Vazquez A, Juarez I, Camacho GM, Calleja EA, Rodriguez-Sosa M. MIF synergizes with Trypanosoma cruzi antigens to promote efficient dendritic cell maturation and IL-12 production via p38 MAPK. Int J Biol Sci. 2011;7:1298–1310. doi: 10.7150/ijbs.7.1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towner JS, Paragas J, Dover JE, Gupta M, Goldsmith CS, Huggins JW, Nichol ST. Generation of eGFP expressing recombinant Zaire ebolavirus for analysis of early pathogenesis events and high-throughput antiviral drug screening. Virology. 2005;332:20–27. doi: 10.1016/j.virol.2004.10.048. [DOI] [PubMed] [Google Scholar]
- Wahl-Jensen V, Kurz S, Feldmann F, Buehler LK, Kindrachuk J, DeFilippis V, da Silva Correia J, Fruh K, Kuhn JH, Burton DR, Feldmann H. Ebola virion attachment and entry into human macrophages profoundly effects early cellular gene expression. PLoS neglected tropical diseases. 2011;5:e1359. doi: 10.1371/journal.pntd.0001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wauquier N, Becquart P, Padilla C, Baize S, Leroy EM. Human fatal zaire ebola virus infection is associated with an aberrant innate immunity and with massive lymphocyte apoptosis. PLoS neglected tropical diseases. 2010;4 doi: 10.1371/journal.pntd.0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei L, Zhu Z, Wang J, Liu J. JNK and p38 mitogen-activated protein kinase pathways contribute to porcine circovirus type 2 infection. J Virol. 2009;83:6039–6047. doi: 10.1128/JVI.00135-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilflingseder D, Mullauer B, Schramek H, Banki Z, Pruenster M, Dierich MP, Stoiber H. HIV-1-induced migration of monocyte-derived dendritic cells is associated with differential activation of MAPK pathways. Journal of immunology (Baltimore, Md: 1950) 2004;173:7497–7505. doi: 10.4049/jimmunol.173.12.7497. [DOI] [PubMed] [Google Scholar]
- Zampieri CA, Fortin JF, Nolan GP, Nabel GJ. The ERK mitogen-activated protein kinase pathway contributes to Ebola virus glycoprotein-induced cytotoxicity. J Virol. 2007;81:1230–1240. doi: 10.1128/JVI.01586-06. [DOI] [PMC free article] [PubMed] [Google Scholar]