Abstract
Objective
Personality traits predict both health behaviors and mortality risk across the life course. However, there are few investigations that have examined these effects in a single study. Thus, there are limitations in assessing if health behaviors explain why personality predicts health and longevity.
Method
Utilizing 14-year mortality data from a national sample of over 6,000 adults from the Midlife in the United States Study, we tested whether alcohol use, smoking behavior, and waist circumference mediated the personality–mortality association.
Results
After adjusting for demographic variables, higher levels of Conscientiousness predicted a 13% reduction in mortality risk over the follow-up. Structural equation models provided evidence that heavy drinking, smoking, and greater waist circumference significantly mediated the Conscientiousness–mortality association by 42%.
Conclusion
The current study provided empirical support for the health-behavior model of personality— Conscientiousness influences the behaviors persons engage in and these behaviors affect the likelihood of poor health outcomes. Findings highlight the usefulness of assessing mediation in a structural equation modeling framework when testing proportional hazards. In addition, the current findings add to the growing literature that personality traits can be used to identify those at risk for engaging in behaviors that deteriorate health and shorten the life span.
Keywords: Big Five, personality, health-behavior model, mediation, mortality
Individual differences in personality traits have emerged as important influences on disease and comorbidity over the life course, as well as longevity (Hampson & Friedman, 2008). For example, higher levels of Conscientiousness predict greater longevity (Kern & Friedman, 2008). With these associations now replicated across diverse samples, the more important question is no longer what traits predict longevity, but why do personality traits predict how long someone lives? In other words, what are the mediating pathways connecting personality to mortality risk? The current study examined this question by testing whether three health-related behaviors recorded over a 14-year period would explain why personality predicts mortality.
Most investigations of the Big Five personality traits (i.e., Neuroticism, Extraversion, Openness to experience, Agreeableness, Conscientiousness) focus on Conscientiousness, which reflects the propensity to be goal-directed, responsible, and in control of impulses, because of the consistent finding that higher levels of Conscientiousness confer a protective effect against earlier mortality. This effect has been found in diverse samples in terms of age, sex, health status, and country of origin, and has been confirmed through several meta-analyses (r = .11, range = 0.01– 0.38; Kern, & Friedman, 2008; Jokela et al., 2013).
Findings for Neuroticism (e.g., frequent experience of negative emotions and emotional instability) are mixed. Some find a positive association with mortality risk (Christensen et al., 2002; Denollet, Sys, & Brutsaert, 1995; Mroczek, Spiro, & Turiano, 2009; Ploubidis & Grundy, 2009; Shipley, Weiss, Der, Taylor, & Deary, 2007; Terracciano, Löckenhoff, Zonderman, Ferrucci, & Costa, 2008; Wilson, Mendes de Leon, Bienas, Evans, & Bennett, 2004), others find a negative association (Korten et al., 1999; Weiss & Costa, 2005), and some report no association (Almada et al., 1991; Friedman et al., 1995; Iwasa et al., 2008; Maier & Smith, 1999).
Meta-analyses have confirmed one particular aspect of Agreeableness (the tendency to be hostile and aggressive or not) predicts increased mortality risk (Miller, Smith, Turner, Guijarro, & Hallet, 1996), but studies employing a more comprehensive measure of Agreeableness, for the most part, have not found an association (Weiss & Costa, 2005). Few studies have found a positive association between longevity and Extraversion (inclination to be outgoing, expressive, and sociable; Ploubidis & Grundy, 2009; Wilson et al., 2004). Last, earlier investigations focusing on Openness to experience (the tendency to be imaginative and creative) have found that it is generally unrelated to health and longevity (Christensen et al., 2002; Maier & Smith, 1999; Mccann, 2005; Weiss & Costa, 2005; Wilson et al., 2004), but more recent investigations have suggested a protective effect of Openness and related facets (Iwasa et al., 2008; Taylor et al., 2009; Turiano, Spiro, & Mroczek, 2012).
With ample evidence accumulating, it is important to identify the mechanisms through which personality traits are linked to mortality. The health-behavior model (HBM) of personality is the leading behavioral theory that suggests levels of certain personality traits are associated with either engagement or abstinence of certain health behaviors that ultimately impact health over the life course (Friedman, 2000; Smith, 2006). Support for this hypothesis is found in observations that lower levels of Conscientiousness and higher levels of Neuroticism have each been linked to negative behaviors, such as smoking tobacco, excessive alcohol use, illicit drug use, and unhealthy eating habits (Bogg & Roberts, 2004; Hopwood et al., 2007; Kashdan, Vetter, & Collins, 2005; Malouff, Thorsteinsson, & Schutte, 2006; Mroczek et al., 2009; Munafò, Zetteler, & Clark, 2007; Terracciano, Löckenhoff, Crum, Bien-venu, & Costa, 2008). These unhealthy behaviors are also among the leading behavioral causes of mortality (United States Department of Health & Human Services, 2013; Mokdad, Marks, Stroup, & Gerberding, 2004). One would expect these behaviors to explain a significant portion of variance in the personality–mortality association, however, there has been little explicit investigating of these pathways, let alone support for a strong mediating role in the handful of studies that have examined such links.
One of the main obstacles to testing mechanisms is methodological in nature because well-established tests of mediation, (e.g., causal steps approach, Sobel test) are appropriate for either continuous or categorical outcomes. However, when an outcome such as mortality includes both discrete (e.g., dead or alive) and continuous (e.g., survival time) information, these types of modeling approaches are not as straightforward. Thus, in reviewing prior studies, it is difficult to determine whether including health-related behaviors in models does in fact explain why certain traits are predictive of mortality risk (see Appendix in the online supplemental materials for review of prior studies). Some previous studies did not explicitly examine potential behavioral mediation of the personality–mortality association because that was not the aim of that particular study, even though relevant behaviors were included in it. Other investigations have set out to examine particular behavioral mediators, but without providing both unadjusted and health-behavior-adjusted models, it becomes difficult to determine if adjusting for health behaviors does reduce the personality– mortality association (Korten et al., 1999; Weiss & Costa, 2005; Jonassaint et al., 2007). Likewise, studies that do compare multiple models but include both health behaviors and other factors related to health behaviors (e.g., education, self-rated health) but also influencing outcomes through other pathways (e.g., access to health care, environmental constraints) limits the ability to partial out the unique effects of just health behaviors (Martin, Friedman, & Schwartz, 2007; Kern, Friedman, Martin, Reynolds, & Luong, 2009). The studies that have examined health behaviors in a separate model have found generally low reductions of the personality effects on mortality (e.g., 0% to 26% reductions; see Appendix in the online supplemental materials). Adjusting for health behaviors explains on average 12% (0% to 21% range) of the variance in the Conscientiousness–mortality association and 13% (0% to 26% range) of the variance in the Neuroticism– mortality association, with some evidence that smoking (Mroczek et al., 2009) and physical activity (Shipley et al., 2007) may be the stronger pathways accounting for the personality–mortality association.
A second major limitation with earlier work is that, although a reduction in personality–mortality association after adjusting for health behaviors suggests mediation, no statistical tests of mediation were conducted. Taylor et al., (2009) formally tested mediation through structural equation modeling with a discrete outcome (e.g., dead/alive), but found no evidence to support the role of smoking and body-mass index (BMI) as pathways between Openness and Conscientiousness with mortality risk. However, analysis of a discrete outcome along with continuous information (e.g., length of life) may provide greater power to examine the potential mediating role of health behaviors in these associations. Recently developed methods have extended the use of proportional hazards in structural equation modeling frameworks (Asparouhov, Masyn, & Muthén, 2006; Muthén & Masyn, 2005). Ploubidis and Grundy (2009) were among the first to apply this modeling technique in a large UK sample by calculating the predictive effects for each personality trait on each of the mediators (e.g., alcohol use, smoking, psychological distress, and somatic health) and the effect of each mediator on mortality risk, which ultimately allowed them to estimate statistical significance tests for each indirect effect. The authors found that higher Neuroticism was associated with increased risk of dying largely through psychological distress and somatic health, but to a lesser extent by smoking. Higher Extra-version was associated with an increased risk of dying, which was partially explained by higher prevalence of smoking.
This earlier study laid the methodological groundwork for our own work, documenting a significant indirect effect through smoking, which explained approximately 11% of why lower levels of Conscientiousness predicted an increased mortality risk in a sample of older men from the Normative Aging Study (Turiano, Hill, Roberts, Spiro, & Mroczek, 2012). However, to date, this methodology has not been utilized in a large U.S. sample with multiple behaviors being tested as possible mediators of the personality– mortality association.
Study Aims
The overall objective of the current study was to further our understanding of the personality–mortality link by assessing if health behaviors statistically mediated this association. Our first goal was to extend findings of an earlier investigation (Chapman, Fiscella, Kawachi, & Duberstein, 2010) of the personality– mortality in the National Survey of Midlife in the United States (MIDUS). This previous study found that higher levels of Neuroticism predicted increased odds of dying over the first 10 years of the MIDUS study: 179 confirmed deaths reported by the National Death Index (NDI) search as of 2004, whereas Agreeableness was associated with an increased risk of dying when Conscientiousness levels were low. The current study extends the mortality follow-up to a 14-year period (580 confirmed deaths through the 2009 NDI mortality update) as well as survival-time information so that both death status (e.g., dead or alive) and survival time (e.g., how long someone lived) could be jointly estimated in a proportional hazards modeling framework.
Our second goal was to test whether age and sex emerged as potential moderating factors of the personality–mortality association. Although findings are by no means consistent, emerging evidence does suggest that associations between personality traits and mortality may differ between men and women and in some cases may be in opposite directions (Friedman, Kern, & Reynolds, 2010; Korten et al., 1999; Taylor et al., 2009; Ploubidis & Grundy, 2009). For example, higher levels of Neuroticism may predict an increased mortality risk in women, but a decreased risk for men. We also tested trait by trait interactions because of a previous Conscientiousness × Agreeableness interaction predicting mortality in the MIDUS study (Chapman, Fiscella, Kawachi, & Duberstein, 2010) and mounting evidence that a Conscientiousness × Neuroticism interaction is an important predictor of both mortality (Friedman et al., 2010) and other important health outcomes (Turiano, Mroczek, Moynihan, & Chapman, 2013).
Our third goal was to formally test if health behaviors did mediate the personality–mortality association by testing proportional hazards in a structural equation modeling framework. We examined whether alcohol and tobacco use, and waist circumference (a proxy for both diet and exercise behavior) were mediators because these are among the leading behavioral contributors to mortality (Mokdad et al., 2004). This modeling technique allows us to simultaneously test multiple mediating pathways which is essential to ensure confounded mediation is avoided (Babyak, 2009) because there are likely multiple behavioral pathways that explain the personality-health association (Hampson & Friedman, 2008). Overall, the large national sample and updated mortality information will allow greater generalizability of study findings and the long follow-up duration will permit a more extensive test of how the Big Five personality traits are related to longevity.
Method
Sample
The MIDUS is an interdisciplinary longitudinal study examining midlife development (for review, see Brim, Ryff, & Kessler, 2004). Over 7,000 participants were recruited in 1994–1996 (N = 7,108) from a nationally representative random-digit-dialing sample of noninstitutionalized adults between the ages 25–75. Once potential participants consented to the study, they completed an approximate 30-min telephone survey and were mailed additional questionnaires. These self-completed questionnaires took approximately 2 hr to complete and were sent back to the study team when completed. If surveys were not returned, participants were contacted and sent new questionnaires. The current sample drew from the 6,325 participants who completed both the phone and the self-administered questionnaires at MIDUS 1 in 1995–1996. To be included in the current analysis, participants needed to complete the following measures: demographics such as age, sex, race, marital status, and education; the Big Five personality questionnaire; and questions regarding alcohol, smoking, and body indices. Comparing those with full versus incomplete MIDUS 1 data, participants completing only the telephone questionnaire (N = 783), were significantly younger (t = 10.19, p < .001), had higher average levels of alcohol use (t = 6.13, p < .001), and were slightly more likely to be male (χ2 = 17.03, p < .001).
Covariates
All models were adjusted for age, sex, race, marital status, and education since these variables have known associations with mortality risk. Education was coded based on the highest level obtained as of 1995–1996. A 12-point scale was constructed ranging from 1, no schooling or some grade school, to 12, professional degrees such as PhD or MD. A dummy code was constructed for both race and marital status. Caucasians were contrasted against all other races, and those married were contrasted against those who were unmarried. Descriptive information on the demographic variables can be found in Table 1.
Table 1.
Descriptive Statistics
| Variables | Deceased (n = 580) |
Alive (n = 5,745) |
Total sample (N = 6,325) |
|
|---|---|---|---|---|
| Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | Range | |
| Age | 59.90 (11.02) | 45.03 (12.40) | 46.38 (13.00) | 20–75 |
| Education | 6.04 (2.52) | 6.85 (2.48) | 6.77 (5.76) | 1–12 |
| Sex | ||||
| Female | 46% | 52% | 52% | 0–1 |
| Male | 54% | 48% | 48% | 0–1 |
| Race | ||||
| Caucasian | 91% | 91% | 91% | 0–1 |
| Other | 9% | 9% | 9% | 0–1 |
| Marital status | ||||
| Married | 58% | 66% | 66% | 0–1 |
| Unmarried | 42% | 34% | 34% | 0–1 |
| Conscientiousness | 3.37 (0.45) | 3.43 (0.44) | 3.42 (0.44) | 1–4 |
| Neuroticism | 2.17 (0.66) | 2.25 (0.66) | 2.24 (0.66) | 1–4 |
| Extraversion | 3.17 (0.58) | 3.20 (0.56) | 3.20 (0.56) | 1–4 |
| Agreeableness | 3.53 (0.47) | 3.49 (0.49) | 3.50 (0.49) | 1–4 |
| Openness | 2.98 (0.55) | 3.02 (0.52) | 3.02 (0.53) | 1–4 |
| Smoking status | ||||
| Never | 27% | 44% | 43% | 1–3 |
| Former | 34% | 25% | 25% | 1–3 |
| Current | 39% | 31% | 32% | 1–3 |
| Years smoked | 23.33 (18.86) | 9.63 (12.82) | 10.87 (14.04) | 0–61 |
| Alcohol use | 3.56 (4.75) | 3.23 (3.60) | 3.26 (3.72) | 0–30 |
| Med (IQR) | 2 (1–4) | 2 (1–4) | 2 (1–4) | |
| Waist circumference | 37.36 (5.95) | 35.20 (5.07) | 35.40 (5.76) | 14–66 |
Personality
The key predictor variables were assessed via the self-administered adjectival measures of the Big Five examined at MIDUS 1 (Prenda & Lachman, 2001). Respondents were asked how much each of 25 adjectives described themselves on a scale ranging from 1 (not at all) to 4 (a lot). The adjectives were as follows: moody, worrying, nervous, calm (Neuroticism); outgoing, friendly, lively, active, talkative (Extraversion); creative, imaginative, intelligent, curious, broad-minded, sophisticated, adventurous (Openness); organized, responsible, hardworking, careless (Conscientiousness); helpful, warm, caring, softhearted, sympathetic (Agreeableness). A mean was calculated from the adjectives for each trait, after reversing the appropriate items.
The MIDUS Big Five scale was developed from a combination of existing personality-trait lists and inventories (for review, see Lachman & Weaver, 1997). The scales have good construct validity (Mroczek & Kolarz, 1998) and all five traits significantly correlated with the NEO trait scales (Prenda & Lachman, 2001). Cronbach alphas for the personality traits were as follows: Agreeableness = .80; Conscientiousness = .58; Extraversion = .76; Neuroticism = .74; Openness = .77.
Alcohol Use
Participants answered questions about their alcohol use through the phone questionnaire portion of MIDUS 1. Participants were asked the following question: “During the year you drank most, about how many drinks would you usually have on the days that you drank?” Because there were a handful of participants who reported extremely high alcohol intake, we Winsorized the top 1% of responses and set them equal to 30 drinks. In addition, based on prior findings of a “j”-shaped relationship with alcohol use and mortality risk (Di Castelnuovo et al., 2006), we created three groups between which to distinguish: (a) nondrinkers (11%), (b) average drinkers (41%; drinking 1–2 alcoholic beverages per drinking occasion), and (c) heavier drinkers (48%; averaging 3 or more alcoholic drinks per drinking occasion). Dummy codes were created to contrast average drinkers (referent) from nondrinkers and heavy drinkers.
Smoking
Participants answered a series of questions about whether they had ever had a cigarette, ever smoked regularly (at least a few cigarettes every day), if they were currently smoking, or if they had quit smoking. We were able to create three groups from this series of questions: (a) those who never smoked during their lives; (b) those who had smoked but were currently not smoking as of 1995–1996; and (c) those who were currently smoking cigarettes in 1995–1996.
Waist Circumference
Waist circumference was utilized as a proxy variable for both eating and exercise habits because it is a strong predictor of mortality risk (Bigaard et al., 2005; Jacobs et al., 2010). Participants were asked to measure the circumference of their waists in inches using a tape measure mailed to them along with the MIDUS self-administered questionnaire.
Vital Status
Mortality data on participants was obtained through an NDI search through January, 2010. Survival time for decedents was the interval from the date of MIDUS 1 completion (1995–1996) to the date of their death (censor date January 15, 2010). Since only month and year of death were provided by NDI, every deceased participant was given the 15th day of the month as his or her day of death. Participants who were still alive (censored observations) had survival times that equaled the length of the follow-up (censored January 15, 2010). The mean survival time for decedents was 8.01 years (SD = 3.90, range = .20–14 years).
Data Analysis
A series of proportional hazards models (i.e., Cox models) was conducted to examine the association between the Big Five personality traits and mortality risk using Mplus Version 6.0 software (Muthén & Muthén, 1998–2010). Proportional hazards modeling is the most appropriate method when examining mortality as an outcome because it takes into account continuous survival times, varying ages at entry into the study, and occurrence of a discrete outcome event (Cox, 1972). Cox models yield estimates (hazard ratios; HRs) of how much a standard deviation increase in a predictor increases or decreases the chances of dying over the specified follow-up period. All predictors were converted into standard deviation units for ease of interpretation.
Estimating mediation in proportional hazards modeling through an SEM framework is an ideal approach because it allows for an assessment of both the direct and indirect effects on continuous survival time (Asparouhov et al., 2006). With a maximum likelihood robust (MLR) estimator and Monte Carlo integration, the program calculates indirect effects comparable to the Sobel method. Specifically, a product-of-coefficients approach computes the ratio of the path from the predictor to the mediator and the path from the mediator to the outcome to its standard error. We consider it important that this technique provides standard errors, confidence intervals, and significance tests. With respect to the latter, the significance test of the indirect effect permits the statistical interpretation of mediation.
Model 1 tested the baseline-unadjusted model that includes all of the Big Five personality traits. Two-way interactions among personality traits, sex, and age were tested as potential moderators of the personality–mortality association. All interactions were screened in the baseline model and if any were significant, they would be included in subsequent models. Model 2 included demographic variables considered confounds which included age, sex, race, education, and marital status. The final fully adjusted path model included each of the mediators in a single model. It is essential to include all four mediators in the same model for two main reasons: (a) the significance of the total indirect effect (sum of all specific indirect effects) determines whether the full set of variables together explain the personality–mortality association and (b) it allows an experimenter to determine whether specific indirect effects are a significant net of the effect of other mediators; in other words, it takes into account the correlation between multiple indirect effects (Preacher & Hayes, 2008).
Results
Descriptive data for the full sample, for those deceased, and for those alive are presented in Table 1. Over the 14-year follow-up, 580 participants died (approximately 9% of the sample). Testing mean differences among those who survived versus those who died over follow-up showed that the deceased were significantly older (t = 29.28, p < .001), more likely to be male (χ2 = 9.82, p < .001), less educated (t = 7.88, p < .001), and less likely to be married (χ2 = 19.16, p < .001). In terms of personality traits, those who died during the follow-up period were significantly lower in Conscientiousness (t = 3.04, p < .01) and lower on Neuroticism (t = 2.79, p < .01).
Correlations between each of the mediator variables revealed modest, but significant, positive associations. Specifically, alcohol use was positively related to both smoking (r = .20), and waist circumference (r = .11). Smoking was positively associated with waist circumference (r = .10). Those who died during the follow-up period reported higher average alcohol consumption in the past (t = 2.16, p < .05), had greater waist circumference (t = 8.46, p < .001), and were more likely to be former (χ2 = 14.35, p < .01) or current (χ2 = 44.40, p < .01) smokers, compared with those who never smoked.
The results for both the baseline and demographic adjusted models are reported in Table 2. According to Model 1, which included all the Big Five personality factors, higher levels of Conscientiousness and Neuroticism were related to a decreased hazard of dying, whereas higher Agreeableness was associated with an increased hazard of dying. There was a trend for higher levels of Extraversion to protect against mortality risk. Openness was not a significant predictor of mortality hazard.
Table 2.
Baseline Proportional Hazards Models Predicting Mortality
| Predictors | Model 1 |
Model 2 |
|---|---|---|
| Hazard ratio [95% CI] | Hazard ratio [95% CI] | |
| Conscientiousness | 0.84 [0.77, 0.92]*** | 0.88 [0.80, 0.96]** |
| Neuroticism | 0.84 [0.77, 0.91]*** | 0.99 [0.91, 1.09] |
| Extraversion | 0.90 [0.81, 1.00]* | 0.90 [0.81, 1.01]* |
| Agreeableness | 1.24 [1.12, 1.38]*** | 1.11 [0.99, 1.24]* |
| Openness | 0.93 [0.85, 1.03] | 1.09 [0.99, 1.22]* |
| Age | 3.27 [2.96, 3.62]*** | |
| Sex (Male) | 1.59 [1.33, 1.90]*** | |
| Minority status (Caucasian) | 1.09 [0.80, 1.59] | |
| Marital status (unmarried) | 1.61 [1.35, 1.92]*** | |
| Education | 0.82 [0.75, 0.90]*** | |
| AIC | 100,020.49 | 8,959.16 |
Note. AIC = Akaike Information Criterion.
p < .10.
p < .01.
p < .001.
Model 2 adjusted for demographic variables (age, sex, race, education, and marital status). Increasing age, being male, being unmarried, and having fewer years of education were all significantly associated with an increased hazard of dying over the 14-year follow-up. After adjusting for these demographic confounders, the Conscientiousness effect remained significant, albeit reduced in magnitude by about 19%. Specifically, every standard deviation increase in Conscientiousness was associated with a 13% decreased hazard of dying over the 14-year follow-up. The strength of the effects for Neuroticism and Agreeableness were substantially reduced (100% and 63% respectively) and rendered nonsignificant after adjusting for the demographic confounds. Sensitivity analyses indicated that age was the specific factor that accounted for the relationships of Neuroticism and Agreeableness with mortality risk. The Extraversion effect did not change (remained a trend). None of the two-way interactions among traits with age or sex approached statistical significance.
Test of Mediation
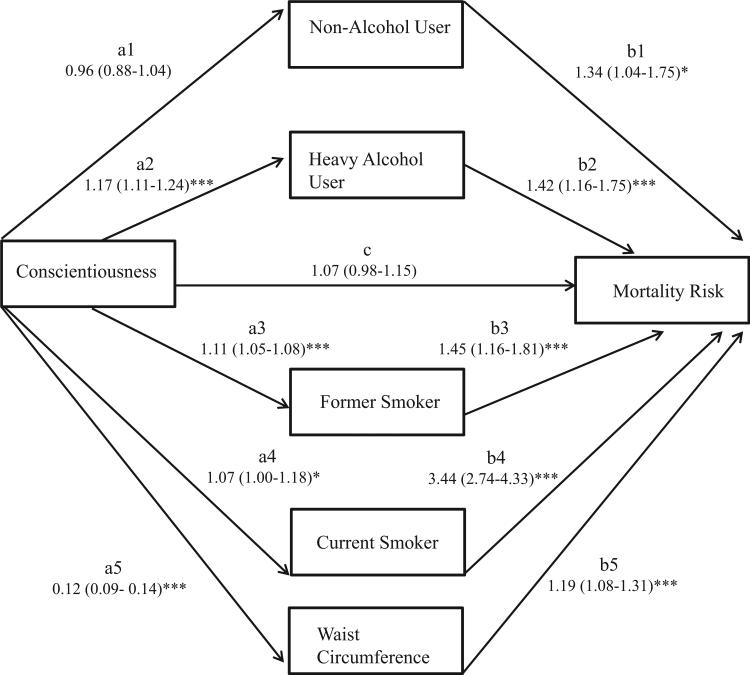
Since Conscientiousness was the only personality trait that predicted mortality after adjusting for demographic factors, all other traits were dropped from the mediation analysis. Figure 1 displays the fully adjusted path model that tests the indirect effects between Conscientiousness and mortality through each of the mediators. Although not shown on the path diagram, the model adjusts for age, sex, race, education, and marital status; for ease of interpreting the direction of effects, Conscientiousness scores were reverse-coded so higher scores reflected those scoring lower in Conscientiousness. The total effect of Conscientiousness on mortality (sum of paths [a1*b1], [a2*b2], [a3*b3], [a4*b4], [a5*b5], [c]) was significant. The full indirect effect (sum of paths [a1*b1], [a2*b2], [a3*b3], [a4*b4], [a5*b5]) was also significant, suggesting that Conscientiousness predicted mortality risk through the set of mediators tested. Examination of the indirect effects for each specific mediator revealed that Conscientiousness predicted mortality risk through previous alcohol use (sum of paths [a1*b1], [a2*b2]), smoking status1 (sum of paths [a3*b3], [a4*b4]), and waist circumference2 (path [a5*b5]. Lower levels of Conscientiousness predicted heavier average alcohol use in the past, greater odds of being a former or current smoker, and a greater waist circumference—which led to an increased hazard of dying over the 14-year follow-up. Examination of the total indirect effect revealed that this set of health behaviors significantly mediated the Conscientiousness–mortality effect, explaining 42% of this association according to the mediated proportion (Ditlevsen, Christensen, Lynch, Damsgaard, & Keiding, 2005; Kaufman, MacLehose, Kaufman, & Greenland, 2005; MacKinnon & Fairchild, 2009).
Figure 1.
Fully adjusted path model adjusting for age, sex, race, education, and marital status. Specific path estimates with 95% CI limits are as follows: total effect (HR = 0.25, CI [0.13, 0.36]***); full indirect effect (HR = 0.18, CI [0.09, 0.27]***); alcohol-use indirect effect (HR = 0.04, CI [0.01, 0.09]*); smoking indirect effect = (HR = 0.12, CI [0.04, 0.20]**); waist-circumference indirect effect (HR = 0.02, CI [0.01, 0.03]***); *p < .05. ** p < .01. *** p < .001. HR = hazard ratio.
Discussion
The current study extended earlier work examining the associations between each of the Big Five personality traits and mortality risk in a national U.S. sample of adults aged 25–74. We did not replicate earlier findings in the MIDUS of a positive association between Neuroticism and mortality risk, nor a positive association between Agreeableness and mortality risk in the context of low Conscientiousness (Chapman et al., 2010). However, examining a longer follow-up period and time to mortality occurrence, we found that higher levels of Conscientiousness predicted a decreased hazard of dying. In addition, using a parsimonious test of mediation we found that the reason those participants who scored lower in Conscientiousness were more likely to die was partly because they had greater levels of central adiposity, engaged in higher average levels of alcohol use during their lives, and were more likely to have smoked during their lives. These results not only provide direct support of the HBM of personality for Conscientiousness, but they also highlight the efficacy of using personality traits as predictors of identifying individuals at risk of engaging in unhealthy behaviors that ultimately contribute to earlier mortality.
The general consensus from prior studies investigating the personality–mortality association was that health-related behaviors such as smoking and alcohol use only slightly attenuated (if at all) the relationship between Conscientiousness and mortality (Hagger-Johnson et al., 2012; Martin et al., 2007; Taylor et al., 2009; Terracciano, Löckenhoff, Zonderman, et al., 2008; Wilson et al., 2004). Across these prior studies, between 0 and 21% of the variance in the Conscientiousness–mortality association was accounted for by health behaviors. Counter to this prior work, our study demonstrated that health-related behaviors explain a more substantial amount of variance, roughly 42% of the Conscientiousness–mortality association. Since the mediated proportion effect was calculated exactly the same as in previous studies, we can conclude that the larger amount of variance explained by health-related behaviors is not an artifact of the methodology used in this study. Rather, the size of the mediating effect is likely to be driven by the specific sample studied. We are unable to discern from our current study exactly what is unique about the MIDUS study population, but it is possible that the relationship between personality and mortality is much stronger in some samples, leaving more variance to be explained by health behaviors. Alternatively, certain samples on the whole may endorse lower levels of Conscientiousness, thus resulting in a stronger association between personality and detrimental health behaviors.
Another unique contribution of the current study was our ability to use a more parsimonious test of mediation (Asparouhov et al., 2006), allowing us to specifically identify how personality was related to each mediator and how each mediator was related to mortality. Moreover, instead of inferring whether these behaviors did in fact explain a significant amount of variance in the personality–mortality association, we were able to construct a statistical significance test for mediation via indirect-effect estimation for each behavioral mediator and the overall set of behaviors. Thus, we can conclude, statistically, that the mediated effect was large enough to be considered statistically different than zero (Kaufman et al., 2005; MacKinnon & Fairchild, 2009). Overall, our study demonstrated the usefulness of statistical advances in mediation analysis in understanding how individual differences in personality traits lead to either engagement in health-detrimental or health-protective behaviors, and how those behaviors influence how long someone lives.
Although the current study did not find any evidence for age, sex, or trait-by-trait interactions as moderators of the personality– mortality association, future work should still examine such factors as a standard model-fitting procedure. Testing and reporting such interactions is useful because it is no longer safe to assume that certain traits will be either protective or detrimental in all circumstances. We should continue to question under which conditions (i.e., trait-by-trait interactions), for whom (i.e., males vs. females), and at what times over the life course (i.e., age) are traits related to health outcomes. This specificity will bolster the idea that psychological factors such as personality are likely important processes involved in determining health and longevity.
Limitations
Even in light of the innovative statistical methods and long-term follow-up applied for the current study, there are qualifications that must be discussed. Since the majority of participants in the MIDUS sample were Caucasian and well-educated, generalizability of study findings are limited. However, this study is one of the first investigations utilizing a large U.S. sample to test the behavioral pathways connecting personality to mortality. The study could also be strengthened if we had information on the cause of death. We might expect the relationship between Conscientiousness and mortality to be stronger for some specific causes of death such as cardiovascular disease, given the role that tobacco, alcohol use, and higher levels of central adiposity play in contributing to the development of this condition (Lloyd-Jones et al., 2010).
There are also limitations with the measures of personality and health behaviors. First, there was a relatively low internal consistency of the Conscientiousness measure. This is due to the small number of items used to assess this trait. A tradeoff of the short Conscientiousness measure was to maximize coverage of the broad trait without selecting multiple items with high redundancy, which would have contributed to participant burden from the large number and scope of questionnaires participants completed. Despite the moderate level of internal consistency, the Midlife Development Inventory scale of Conscientiousness has been shown to have high test–retest reliability and good construct validity (Mroczek & Kolarz, 1998) with high correlation (r = .81) with the more expansive NEO personality measure (Lachman & Weaver, 1997). Second, although we examined some of the leading behavioral contributors to early mortality (Mokdad et al., 2004; U.S. Department of Health & Human Services, 2013), there are other behaviors and physiological factors that could be examined as mediating variables. For example, specific questions about diet, exercise, and health-care utilization are just a few other behaviors that could shed light on how personality is related to health. Likewise, more detailed questions assessing both life-time and current alcohol, tobacco, and drug-use behaviors would provide a more nuanced analysis. More detailed measures of substance-abuse patterns from ecological momentary assessment techniques found in many daily diary studies could also provide more nuanced information on substance-abuse patterns not captured in retrospective questionnaires (Shiffman, 2009). Even so, as measured, health behaviors in the current study were associated with large hazard ratios—demonstrating the long-term impact prior behavior has on health and longevity.
It is also important to interpret the current study findings in light of limitations with the temporal ordering of the variables measured. An optimal mediation study design assumes that individual differences in personality traits cause certain behaviors, and that these behaviors then lead to poorer health and an increased risk of dying. However, establishing evidence for this causal ordering is difficult to demonstrate and actually may be untestable in most situations (MacKinnon, Fairchild, & Fritz, 2007). For example, in the current study, the mediating variables of alcohol use and smoking behavior were behaviors that occurred before the measurement of personality—a common problem with the majority of prior studies investigating these health-behavior pathways (Hagger-Johnson et al., 2012; Martin et al., 2007; Taylor et al., 2009; Terracciano, Löckenhoff, Zonderman, et al., 2008; Wilson et al., 2004). This common limitation is compounded in the current study because the MIDUS questionnaires did not record the actual age when alcohol consumption was at its peak. But personality is generally considered to be a relatively stable trait, lending confidence that personality assessments measured at any given point in adulthood reflect an enduring pattern of trait experience in previous phases of adulthood. However, there are known individual differences in the stability of personality traits (Roberts, Walton, & Viechtbauer, 2006). Some persons do change in personality and these changes in personality can impact behavior (Turiano et al., 2012) and health outcomes (Mroczek & Spiro, 2007). Thus, the assumption that later personality can be used as a proxy for personality earlier in life may be tenuous.
An important objective of future research is to examine life course patterns of personality and health behavior. Repeated assessments of these constructs across adulthood are essential for more carefully untangling the potential bidirectional relationships between personality and health behavior and their influences on health (Hampson, 2012). Our findings suggest that personality may shape engagement in certain forms of health-damaging behaviors. However, we also know that engagement in some detrimental health behaviors, like smoking, may also shape normative changes in personality (Welch & Poulton, 2009). Also, poor health may affect trajectories of personality development. Life-course assessment of these constructs would shed light on temporal-precedence assumptions needed to establish support for mediation and enhance our understanding of how personality and behavior influences health across the life course.
Conclusion
There have been many important investigations over the past two decades into how personality influences health. Friedman (2000) described the need to investigate health behaviors as mediators of the personality–mortality association. Our understanding of exactly how personality influences health and longevity has improved with new developments in longitudinal and mediation methodology. The current study provides evidence that engaging in detrimental health behaviors explains at least part of the reason that individuals scoring lower on Conscientiousness are more likely to die—providing credence for the HBM of personality. Although the clinical application of these findings is still in its infancy, there is growing interest in using personality assessment in medical practice to identify individuals at risk for poor health and engagement in detrimental health-related behaviors, and to target personality as a point of intervention (Chapman et al., 2011; Moffitt et al., 2011). Using personality traits as a means to uncover chains of risk from dispositions to behavior and health/illness is an exciting possibility in the move toward personalized medicine.
Supplementary Material
Acknowledgments
This research was supported by Grant T32-MH018911-23 from the United States Department of Health and Human Services, National Institutes of Health (NIH), National Institute of Mental Health and Grants T32 AG025671-02, P01 AG20166, and K08 AG031328 from the NIH National Institute on Aging.
Footnotes
Supplemental materials: http://dx.doi.org/10.1037/hea0000038.supp
Sensitivity analyses indicated that the findings were similar when either the number of years someone smoked, or the average number of cigarettes smoked in a given day during a year in life the person smoked most heavily were used instead of smoking category as mediators.
Sensitivity analyses indicated that the findings were similar when a measure of BMI was used instead of waist circumference.
Contributor Information
Nicholas A. Turiano, Department of Psychiatry, University of Rochester School of Medicine and Dentistry and Center on Aging and the Life Course, West Lafayette, Indiana
Benjamin P. Chapman, Department of Psychiatry, University of Rochester School of Medicine and Dentistry
Tara L. Gruenewald, Davis School of Gerontology, University of Southern California
Daniel K. Mroczek, Department of Psychology, Weinberg College of Arts & Sciences and Department of Medical Social Sciences, Feinberg School of Medicine, Northwestern University.
References
- Almada SJ, Zonderman AB, Shekelle RB, Dyer AR, Daviglus ML, Costa PT, Stamler J. Neuroticism and cynicisms and risk of death in middle-aged men: The Western Electric Study. Psychosomatic Medicine. 1991;53:165–175. doi: 10.1097/00006842-199103000-00006. [DOI] [PubMed] [Google Scholar]
- Asparouhov T, Masyn K, Muthén B. Proceedings of the Joint Statistical Meeting. American Statistical Association, Biometrics Section; Seattle, Washington: Aug, 2006. Continuous time survival in latent variable models. pp. 180–187. Retrieved from http://www.statmodel.com/download/SurvivalJSM3.pdf. [Google Scholar]
- Babyak MA. Understanding confounding and mediation. Evidence Based Mental Health. 2009;12:68–71. doi: 10.1136/ebmh.12.3.68. doi:10.1136/ebmh.12.3.68. [DOI] [PubMed] [Google Scholar]
- Bigaard J, Frederiksen K, Tjonneland A, Thomsen BL, Overvad K, Heitmann BL, Sorensen TI. Waist circumference and body composition in relation to all-cause mortality in middle-aged men and women. International Journal of Obesity. 2005;29:778–784. doi: 10.1038/sj.ijo.0802976. doi: 10.1038/sj.ijo.0802976. [DOI] [PubMed] [Google Scholar]
- Bogg T, Roberts BW. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychological Bulletin. 2004;130:887–919. doi: 10.1037/0033-2909.130.6.887. doi:10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- Brim OG, Ryff CD, Kessler RC. How healthy are we? A national study of well-being at midlife. Chicago University Press; Chicago, IL: 2004. [Google Scholar]
- Chapman BP, Fiscella K, Kawachi I, Duberstein PR. Personality, socioeconomic status, all-cause mortality in the United States. American Journal of Epidemiology. 2010;171:83–92. doi: 10.1093/aje/kwp323. doi:10.1093/aje/kwp323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman BP, Roberts BW, Duberstein P. Personality and longevity: Knowns, unknowns, and implications for public health and personalized medicine. Journal of Aging Research. 2011;2011:1–24. doi: 10.4061/2011/759170. Online publication. doi:10.4061/2011/759170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen AJ, Ehlers SL, Wiebe JS, Moran PJ, Raichle K, Ferneyhough K, Lawton WJ. Patient personality and mortality: A 4-year prospective examination of chronic renal insufficiency. Health Psychology. 2002;21:315–320. doi: 10.1037//0278-6133.21.4.315. doi:10.1037/0278-6133.21.4.315. [DOI] [PubMed] [Google Scholar]
- Cox DR. Regression models and life tables. Journal of the Royal Statistical Society. 1972;34:187–220. [Google Scholar]
- Denollet J, Sys SU, Brutsaert DL. Personality and mortality after myocardial infraction. Psychosomatic Medicine. 1995;57:582–591. doi: 10.1097/00006842-199511000-00011. [DOI] [PubMed] [Google Scholar]
- Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: An updated meta-analysis of 34 prospective studies. Archives of Internal Medicine. 2006;166:2437–2445. doi: 10.1001/archinte.166.22.2437. doi:10.1001/archinte.166.22.2437. [DOI] [PubMed] [Google Scholar]
- Ditlevsen S, Christensen U, Lynch J, Damsgaard MT, Keiding N. A structural equation modeling approach for estimating the proportion of exposure effect on outcome explained by an intermediate variable. Epidemiology. 2005;16:114–120. doi: 10.1097/01.ede.0000147107.76079.07. doi:10.1097/01.ede.0000147107.76079.07. [DOI] [PubMed] [Google Scholar]
- Friedman HS. Long-term relations of personality and health: Dynamisms, mechanisms, tropisms. Journal of Personality. 2000;68:1089–1107. doi: 10.1111/1467-6494.00127. doi:10.1111/1467-6494.00127. [DOI] [PubMed] [Google Scholar]
- Friedman HS, Kern M, Reynolds CA. Personality and health, subjective well-being, and longevity. Journal of Personality. 2010;78:179–216. doi: 10.1111/j.1467-6494.2009.00613.x. doi:10.1111/j.1467-6494.2009.00613.x. [DOI] [PubMed] [Google Scholar]
- Friedman HS, Tucker JS, Tomlinson-Keasey C, Martin LR, Wingard DL, Criqui MH. Psychosocial and behavioral predictors of longevity: The aging and death of the “Termites”. American Psychologist. 1995;50:69–78. doi: 10.1037//0003-066x.50.2.69. doi:10.1037/0003-066X.50.2.69. [DOI] [PubMed] [Google Scholar]
- Hagger-Johnson G, Sabia S, Nabi H, Brunner E, Kivimaki M, Shipley M, Singh-Manoux A. Low conscientiousness and risk of all-cause, cardiovascular and cancer mortality over 17 years: Whitehall II cohort study. Journal of Psychosomatic Research. 2012;73:98–103. doi: 10.1016/j.jpsychores.2012.05.007. doi:10.1016/j.jpsychores.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson SE. Personality processes: Mechanisms by which personality traits “get outside the skin”. Annual Review of Psychology. 2012;63:315–339. doi: 10.1146/annurev-psych-120710-100419. doi:10.1146/annurev-psych-120710-100419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson SE, Friedman HS. Personality and health: A lifespan perspective. In: John OP, Robins R, Pervin L, editors. The handbook of personality. 3rded. Guilford Press; New York, NY: 2008. pp. 770–794. [Google Scholar]
- Hopwood CJ, Morey LC, Skodol AE, Stout RL, Yen S, Ansell EB, McGlashan TH. Five-factor model of personality traits associated with alcohol-related diagnoses in a clinical sample. Journal of Studies on Alcohol and Drugs. 2007;68:455–460. doi: 10.15288/jsad.2007.68.455. [DOI] [PubMed] [Google Scholar]
- Iwasa H, Masui Y, Gondo Y, Inagaki H, Kawaai C, Suzuki T. Personality and all-cause mortality among older adults dwelling in a Japanese community: A five-year population-based prospective cohort study. The American Journal of Geriatric Psychiatry. 2008;16:399–405. doi: 10.1097/JGP.0b013e3181662ac9. doi:10.1097/JGP.0b013e3181662ac9. [DOI] [PubMed] [Google Scholar]
- Jacobs EJ, Newton CC, Wang Y, Patel AV, McCullough ML, Campbell PT, Gapstur SM. Waist circumference and all-cause mortality in a large US cohort. Archives of Internal Medicine. 2010;170:1293–1301. doi: 10.1001/archinternmed.2010.201. doi:10.1001/archinternmed.2010.201. [DOI] [PubMed] [Google Scholar]
- Jokela M, Batty GD, Nyberg ST, Virtanen M, Nabi H, Sing-Manoux A, Kivimaki M. Personality and all-cause mortality: Individual-participant meta-analysis of 3,947 deaths in 76,150 adults. American Journal of Epidemiology. 2013;178:667–675. doi: 10.1093/aje/kwt170. doi:10.1093/aje/kwt170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonassaint CR, Boyle SH, Williams RB, Mark DB, Siegler IC, Barefoot JC. Facets of openness predict mortality in patients with cardiac disease. Psychosomatic Medicine. 2007;69:319–322. doi: 10.1097/PSY.0b013e318052e27d. doi: 10.1097/PSY.0b013e318052e27d. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Vetter CJ, Collins RL. Substance use in young adults: Associations with personality and gender. Addictive Behaviors. 2005;30:259–269. doi: 10.1016/j.addbeh.2004.05.014. doi:10.1016/j.addbeh.2004.05.014. [DOI] [PubMed] [Google Scholar]
- Kaufman JS, MacLehose RF, Kaufman S, Greenland S. The mediation proportion: To the editor. Epidemiology. 2005;16:710. doi: 10.1097/01.ede.0000171282.54664.71. doi: 10.1097/01.ede.0000171282.54664.71. [DOI] [PubMed] [Google Scholar]
- Kern ML, Friedman HS. Do conscientious individuals live longer? A quantitative review. Health Psychology. 2008;27:505–512. doi: 10.1037/0278-6133.27.5.505. doi: 10.1037/0278-6133.27.5.505. [DOI] [PubMed] [Google Scholar]
- Kern ML, Friedman HS, Martin LR, Reynolds CA, Luong G. Conscientiousness, career success, and longevity: A lifespan analysis. Annals of Behavioral Medicine. 2009;37:154–163. doi: 10.1007/s12160-009-9095-6. doi:10.1007/ s12160-009-9095-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korten AE, Jorm AF, Jiao Z, Letenneur L, Jacomb PA, Henderson AS, Christensen H, Rodgers B. Health, cognitive, and psychosocial factors as predictors of mortality in an elderly community sample. Journal of Epidemiology and Community Health. 1999;53:83–88. doi: 10.1136/jech.53.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman M, Weaver SL. The Midlife Development Inventory (MIDI) personality scales: Scale construction and scoring (Tech. Rep. No. 1) Department of Psychology, Brandeis University; Waltham, MA: 1997. [Google Scholar]
- Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Rosamond WD. Defining and setting national goals for cardiovascular health promotion and disease reduction. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. doi:10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ. Current directions in mediation analysis. Current Directions in Psychological Science. 2009;18:16–20. doi: 10.1111/j.1467-8721.2009.01598.x. doi:10.1111/j.1467-8721.2009.01598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. doi:10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maier H, Smith J. Psychological predictors of mortality in old age. The Journals of Gerontology: Series B. Psychological Sciences and Social Sciences. 1999;54:P44–P54. doi: 10.1093/geronb/54b.1.p44. doi:10.1093/geronb/54B.1.P44. [DOI] [PubMed] [Google Scholar]
- Malouff JM, Thorsteinsson EB, Schutte NS. The five-factor model of personality and smoking: A meta-analysis. Journal of Drug Education. 2006;36:47–58. doi: 10.2190/9EP8-17P8-EKG7-66AD. doi:10.2190/9EP8-17P8-EKG7-66AD. [DOI] [PubMed] [Google Scholar]
- Martin LR, Friedman HS, Schwartz JE. Personality and mortality risk across the life span: The importance of conscientiousness as a biopsychosocial attribute. Health Psychology. 2007;26:428–436. doi: 10.1037/0278-6133.26.4.428. doi: 10.1037/0278-6133.26.4.428. [DOI] [PubMed] [Google Scholar]
- Mccann SJH. Longevity, Big Five personality factors, and health behaviors: Presidents from Washington to Nixon. Journal of Psychology: Interdisciplinary and Applied. 2005;139:273–288. doi: 10.3200/JRLP.139.3.273-288. doi:10.3200/ JRLP.139.3.273-288. [DOI] [PubMed] [Google Scholar]
- Miller TQ, Smith TW, Turner CW, Guijarro ML, Hallet AJ. A meta-analytic review on research on hostility and physical health. Psychological Bulletin. 1996;119:322–348. doi: 10.1037/0033-2909.119.2.322. doi:10.1037/0033-2909.119.2.322. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, Caspi A. A gradient of childhood self-control predicts health, wealth, and public safety. PNAS: Proceedings of the National Academy of Sciences of the United States of America. 2011;108:2693–2698. doi: 10.1073/pnas.1010076108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Marks J, Stoup DF, Gerberding JL. Actual causes of death in the United States, 200. JAMA: Journal of American Medical Association. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. doi:10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Kolarz CM. The effect of age on positive and negative Affect: A developmental perspective on happiness. Journal of Personality and Social Psychology. 1998;75:1333–1349. doi: 10.1037//0022-3514.75.5.1333. doi:10.1037/0022-3514.75.5.1333. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Spiro A., III Psychological Science. 2007;Personality change influences mortality in older men.18:371–376. doi: 10.1111/j.1467-9280.2007.01907.x. doi: 10.1111/j.1467-9280.2007.01907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mroczek DK, Spiro A, Turiano N. Do health behaviors explain the effect of neuroticism on mortality? Journal of Research in Personality. 2009;43:653–659. doi: 10.1016/j.jrp.2009.03.016. doi:10.1016/j.jrp.2009.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munafò MR, Zetteler JI, Clark TG. Personality and smoking status: A meta-analysis. Nicotine & Tobacco Research. 2007;9:405–413. doi: 10.1080/14622200701188851. doi:10.1080/14622200701188851. [DOI] [PubMed] [Google Scholar]
- Muthén B, Masyn K. Discrete-time survival mixture analysis. Journal of Educational and Behavioral Statistics. 2005;30:27–58. doi: 10.3102/10769986030001027. [Google Scholar]
- Muthén LK, Muthén BO. MPlus user's guide. 6th ed. Authors; Los Angeles, CA: 1998–2010. [Google Scholar]
- Ploubidis GB, Grundy E. Personality and all-cause mortality: Evidence for indirect links. Personality and Individual Differences. 2009;47:203–208. doi:10.1016/j.paid.2009.02.022. [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. doi:10.3758/ BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Prenda KM, Lachman ME. Planning for the future: A life management strategy for increasing control and life satisfaction in adulthood. Psychology and Aging. 2001;16:206–216. doi:10.1037/0882-7974.16.2.206. [PubMed] [Google Scholar]
- Roberts BW, Walton K, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin. 2006;132:1–25. doi: 10.1037/0033-2909.132.1.1. doi:10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Ecological momentary assessment (EMA) in studies of substance use. Psychological Assessment. 2009;21:486–497. doi: 10.1037/a0017074. doi:10.1037/a0017074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shipley BA, Weiss A, Der G, Taylor MD, Deary IJ. Neuroticism, extraversion, and mortality in the UK health and lifestyle survey: A 21-year prospective cohort study. Psychosomatic Medicine. 2007;69:923–931. doi: 10.1097/PSY.0b013e31815abf83. doi:10.1097/PSY.0b013e31815abf83. [DOI] [PubMed] [Google Scholar]
- Smith TW. Personality as risk and resilience in physical health. Current Directions in Psychological Science. 2006;15:227–231. doi:10.1111/ j.1467-8721.2006.00441.x. [Google Scholar]
- Taylor MD, Whiteman MC, Fowkes GR, Lee AJ, Allerhand M, Deary IJ. Five factor model personality traits and all-cause mortality in the Edinburgh artery study cohort. Psychosomatic Medicine. 2009;71:631–641. doi: 10.1097/PSY.0b013e3181a65298. doi:10.1097/PSY.0b013e3181a65298. [DOI] [PubMed] [Google Scholar]
- Terracciano A, Löckenhoff CE, Crum RM, Bienvenu OJ, Costa PT. Five-factor model personality profiles of drug users. BMC Psychiatry. 2008;8 doi: 10.1186/1471-244X-8-22. no pagination. Online publication. doi:10.1186/1471-244X-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Löckenhoff CE, Zonderman AB, Ferrucci L, Costa PT. Personality predictors of longevity: Activity, emotional stability, and conscientiousness. Psychosomatic Medicine. 2008;70:621–627. doi: 10.1097/PSY.0b013e31817b9371. doi:10.1097/PSY.0b013e31817b9371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano NA, Hill PL, Roberts BW, Spiro A, III, Mroczek DK. Smoking mediates the association between conscientiousness and mortality. Journal of Research in Personality. 2012;46:719–724. doi: 10.1016/j.jrp.2012.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano NA, Mroczek DK, Moynihan J, Chapman BP. Big 5 personality traits and interleukin-6: Evidence for “healthy Neuroticism” in a US population sample. Brain, Behavior, and Immunity. 2013;28:83–89. doi: 10.1016/j.bbi.2012.10.020. doi:10.1016/j.bbi.2012.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano NA, Sprio A, III, Mroczek DK. Openness to experience and mortality in men: Analysis of trait and facets. Journal of Aging and Health. 2012;24:654–672. doi: 10.1177/0898264311431303. doi:10.1177/0898264311431303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services, Office of Disease Prevention and Health Promotion . Healthy people 2020. Author; Washington, DC: 2013. Retrieved from http://healthypeople.gov/2020/topicsobjectives2020/default.aspx. [Google Scholar]
- Weiss A, Costa PT., Jr. Domain and facet personality predictors of all-cause mortality among Medicare patients aged 65 to 100. Psychosomatic Medicine. 2005;67:724–733. doi: 10.1097/01.psy.0000181272.58103.18. doi:10.1097/01.psy .0000181272.58103.18. [DOI] [PubMed] [Google Scholar]
- Welch D, Poulton R. Personality influences on change in smoking behavior. Health Psychology. 2009;28:292–299. doi: 10.1037/a0013471. doi:10.1037/a0013471. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Mendes de Leon CF, Bienas JL, Evans DA, Bennett DA. Personality and mortality in old age. The Journals of Gerontology: Series B. Psychological Sciences and Social Sciences. 2004;59:P110–P116. doi: 10.1093/geronb/59.3.p110. doi:10.1093/geronb/59.3.P110. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.