Background
Nearly 30% of Americans in rural areas live more than 30 miles away from an American College of Surgeons (ACS)-verified trauma center(1). This is particularly true for the state of Vermont, which has a large rural population. Trauma patients in more rural areas are typically assessed and stabilized at the smaller local hospitals and then, if necessary, transferred to a regional level I trauma center.
Initial assessment of trauma patients at the smaller facilities frequently involves CT scanning. For a variety of reasons, some of which are unnecessary, these CT scans are often repeated once the patient arrives at the level I trauma center(2). Duplicated CT scanning not only increases patient radiation and contrast exposure, but also it is a waste of healthcare dollars.
The reasons cited for repeat imaging can be broken down grossly into clinical and technical categories. Technical reasons include inability to open accompanying CD-ROM, inadequate transferred data, radiology report not included, etc. The primary clinical reason usually involves a change in patient condition. To our knowledge, the frequency and consequences of repeat imaging, including patient radiation exposure, cost to payers, and effects on clinical management, have not been studied.
Repeat CT imaging increases radiation and contrast exposure(3–6). CT scanning is also resource-intensive, and carries with it obligatory expenses including equipment charges, technical support and radiology consultation(7, 8).
We sought to determine the incidence of duplicate CT scans in trauma patients who were transferred from outside hospitals (OSH) to our rural Level I trauma center. We prospectively followed patients from their arrival in our emergency department (ED) until hospital discharge and interviewed their providers. We evaluated outcomes pertinent to the repeat imaging, including the rationale for the order, whether duplicate imaging changed patient management, effective radiation dose to the patient, and associated charges for the repeat exams.
Methods
Study design
We performed a prospective, observational study of trauma patients transferred to our level 1 trauma center (FAHC), including an interviewer-assisted survey of the physicians caring for these trauma patients. Our institutional review board approved this study with a waiver of consent. All providers were notified and encouraged to participate in the study by their clinical leaders.
Setting and Subjects
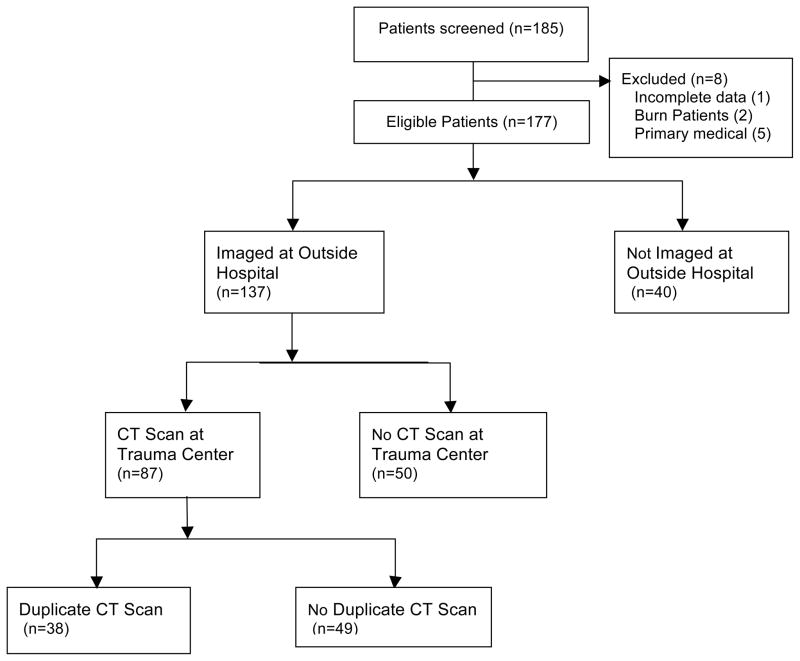
This study was conducted at a rural, academic medical center that houses the region’s only Level 1 trauma center (FAHC). We enrolled a convenience sample of subjects based on availability of the research team. CT images are usually sent as digital images on a CD or DVD from the OSH, although some OSH directly transfer images electronically via Picture Archiving and Communication System (PACS). All trauma patients, regardless of age, who were transferred from outlying hospitals for traumatic injuries during the period of September 2009 to August 2010 were eligible for the study (Figure 1). Patients were excluded from the study if they were transferred for burn care and had no other trauma. All study patients were monitored to determine if they had a second CT scan ordered during the first 24 hours at our RTC. If so, the provider who ordered the duplicate CT scan was interviewed.
Figure 1.
Study Participants.
Data collection and processing
Data was collected in the ED at the time of transfer and again at hospital discharge. Patient data was obtained from medical records and interviews of the physician managing the trauma patient using standardized questions.
After patient discharge a single researcher (HM) determined outcomes by reviewing hospital records. Data collected included: imaging studies, injury severity score (ISS), discharge disposition, total hospital days, and overall survival. “Duplicate CT Scan” was defined as a CT scan performed at our level-1 trauma center of the same body part within 24 hours of the initial scan from the outside hospital. “Additional CT Scan” was defined as a patient receiving a different CT imaging protocol or body part. For example, for a patient with a CT of the head at an OSH, CT head angiography in our ED would be considered an additional study. A patient could receive multiple duplicate and additional studies. Effective radiation dose was calculated using the exposure chart developed by the American College of Radiology and the Radiology Society of North America(7). The charge for each duplicate scan on the first 137 patients was determined by a review of the radiology billing records, and assessing the amount each patient was billed.
Results
Of the 185 trauma patients transferred to FAHC, 8 were excluded, 1 for incomplete data, 2 who had burns and 5 medical patients with no trauma. At the referring hospital, 40 did not receive a CT scan, leaving 137 who met the inclusion criteria. The median age of the patients was 44 years, with 68% male (Table 1). The most common mechanisms of injury included fall (32%), motor vehicle collision (28%), all-terrain vehicle/motorcycle collision (16%) and assault/blunt trauma (8%). Of the 137 patients who received a CT scan at the outside hospital, 87 (63%) also received CT scans at FAHC, with 38 (28%) patients receiving duplicate CT scans (Table 2).
Table 1.
Demographics of study population.
| Patients | Total (n=177) |
|---|---|
| Male (%) | 120 (68) |
| Age, median | 44.1 |
| Pediatric <18yrs (%) | 25 (14) |
| Injury severity score, median | 14 |
| Mechanism of Injury | |
| Fall | 57 (32%) |
| Motor Vehicle Collision | 49 (28%) |
| All-Terrain Vehicle/Motorcycle Collision | 28 (16%) |
| Assault/Blunt Trauma | 14 (8%) |
| Sports Injury | 10 (6%) |
| Penetrating Trauma | 9 (5%) |
| Other | 10 (6%) |
Table 2.
Frequency of diagnostic CT scans in patients transferred to regional trauma center.
| VT | NY* | Total | |
|---|---|---|---|
| CT at outside hospital | 56 | 81 | 137 |
| CT at trauma center | 41 (73%) | 47 (58%) | 87 (49%) |
| Duplicate CT scan | 17 (30%) | 21 (26%) | 38 (28%) |
| Total CTs/patient, median (IQR) | 2 (1–3) | 1 (1–3) | 2 (1–3) |
IQR, interquartile range
Includes one patient from NH
The physician interview response rate regarding the indication for duplicate CT scans was 85% (39/46 patients). The primary reasons for duplicate CT scanning cited during the interview process with the ordering physician were: inadequate transfer of data (14), decompensation of patient (10), did not agree with OSH report (4), other (5), unknown (5) (Figure 2). When we reviewed the reasons for inadequate data transfer, we found that these patients arrived at the trauma center with CD-ROM containing outside hospital imaging data. Surprisingly, of these 14 patients, in only 2 cases, the CD-ROMs could not be opened. In 12/14 cases, we found that the capacity of a single CD-ROM was insufficient to contain a full trauma scan with thin section multiplanar imaging data needed for spine reconstructions. In all of these cases, outside hospitals had sent only the rendered images but not the raw data, in order to fit the images onto CD. In contrast, images arriving from hospitals with direct digital links using PACS (picture archiving and communication systems) were adequate.
Figure 2.
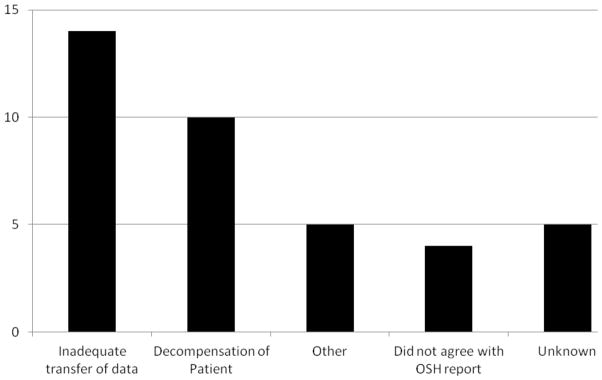
Reasons for Duplicate CT Scanning (n=32)
Physicians reported a change in patient management in 16 (42%) of the patients who received duplicate CT scans (Table 3). The median additional radiation dose was 10.2 mSv (IQR 6.6 – 15.7). The median additional charge was $409 (interquartile range [IQR] $307 – $734). Estimation of radiation dose and additional charge was only performed on the first 21 patients receiving duplicate CT scans.
Table 3.
Duplicate CT scans: impact on management, radiation exposure, and charges.
| Patients receiving duplicate CT scans (n=38) | |
|---|---|
| Change in patient management | 16 (42%) |
| Radiation dose for duplicate studies, mSv, median (IQR) | 10.2 (6.6 – 15.7)* |
| Billing charges, median (IQR) | $1,901 ($1,901 - $3,800)* |
IQR, interquartile range
Data is for first 21 patients with duplicate scans
Discussion
Frequency of CT scanning
All patients enrolled in this study had OSH CT imaging on multi-detector CT (MDCT) scanners. The percentage of patients receiving duplicate CT scans at our trauma center (28%) was less than that reported by other studies, which ranges from 40% – 91%(9–12). A prospective study from Arizona showed that transferred trauma patients who received duplicate CT scans spent more time at an OSH and had a higher ISS(11); however, reasons for these scans and the impact on patient management were not described. Our results are consistent with other reports showing that duplicate CT scanning is most heavily utilized in the assessment of central nervous system injuries in trauma patients(10). While our study is not the first to describe the frequency of duplicate CT imaging, our data supports the claim that, despite variability in the frequency of this practice, it is widespread in trauma centers across the country.
Reasons for duplicate scanning
Our study is the first to prospectively assess the reasons for duplicate imaging in transferred trauma patients. “Inadequate transfer of data” was the most commonly cited indication for requesting duplicate CT exams in our study. Surprisingly, the duplicate scans were most frequently ordered because thin section multiplanar data was not included in the transferred CT study. At the time of data collection, 50% of the OSH in this study had direct PACS to PACS transfer capabilities, which was only intermittently utilized. The alternative means of sending data was to provide a CD or DVD with the patient, which was then uploaded into our PACS system. One of the underlying factors for the inadequate transfer of data is the small storage capacity of a CD (0.7 GB). In most cases, CD storage is adequate for only one body part. Therefore, using a CD for trauma patients, who have multiple exams with inherently thin data sets, is the primary cause of “inadequate data”. A DVD’s storage capacity (5GB) may mitigate this problem, but is not the ultimate solution.
The study by Gupta et al. reported that the predominant reason for repeating a head CT was progression of symptoms (10). In our study, decompensation of the patient or progression of symptoms was given a minority of the time as the reason for duplicate CT scanning (10/38 patients, 26%), suggesting that there is variability among institutions for the rationale of duplicate scanning. Both our study and the Cook study support the conclusion that duplicate CT scanning is not commonly related to patient decompensation(13). The Cook study found that duplicate CT scans did not find new injuries, but that review of initial OSH scans by the trauma center radiologist did identify injuries that were not originally identified by the OSH(13). Prior studies assessing the impact of follow-up imaging of injured patients suggest that this practice rarely alters the patient’s care(7, 8, 14–18). Sung et al. published a retrospective paper on duplicate imaging in 2009, including all transferred patients undergoing repeat imaging whose films were reviewed by an in-house radiologist(19). The data showed 35% of all repeat scans could be avoided, and the incidence of avoidable CT scanning for trauma patients was nearly 3 times that of non-trauma patients.
Effective radiation dose
The median effective radiation dose from the initial 21 duplicate scans was 10.2 mSv (Table 3). However, at least 3 of 21 (14%) patients with duplicate scans received greater than 30 mSv of additional radiation. Smith-Bindman et al. reported that there can be a 13-fold variability in radiation from CT studies of the same body part from different institutions due to lack of standardization of imaging techniques(20). Our effective radiation doses were calculated from a standardized chart based on radiation exposure at our RTC, where we utilize dose reduction technology. We were unable to verify if the referring OSHs in our study utilize the same scanning protocols, so actual radiation doses that patients are receiving from OSHs may have been underestimated. This study’s finding that up to 37% of duplicate studies could have been avoided with adequate data transfer, supports sending CT images via a direct PACS to PACS transfer, which provides all of the necessary data for image reconstruction, as a means to decrease rates of duplicate scanning in transferred trauma patients.
Limitations
This study has several limitations. Our patient population was a convenience sample, as we were unable to continually enroll patients because our research team was not available during holidays and semester break. We cannot be certain that the patient population we studied completely reflects the incidence of these types of scans. However, we did enroll patients on nights and weekends and do not have any reason to suspect selection bias, and furthermore we have demonstrated in a prospective fashion, that duplicate scanning is present at our institution to a similar, although smaller, extent than 2 prior retrospective studies. We may be underreporting the true duplicate CT incidence because of our convenience sample. Prior to enrollment of patients for this study we ran a 3-month pilot study to refine patient enrollment and data collection (March – May 2009). This preliminary data (not included in this paper) had a similar incidence of duplicate scanning. Another limitation is that we lacked 100% participation in survey completion by physicians ordering duplicate scans. Due to the nature of the emergency department during trauma activations, our researchers in some cases were unable to interview the physician ordering the scan. It is possible that some physicians felt uncomfortable answering the questionnaire and there may be potential bias in their choice of answers that we are unable to eliminate. Because our primary outcome was a robust determination of the incidence of duplicate scans, we present the secondary outcomes in descriptive fashion without an attempt to perform inferential statistics or make overreaching generalizations.
Conclusion
Duplicate CT imaging of the same body part occurred in 28% of patients initially imaged at OSH. The most common reason (37%) for duplicated CT scanning at FAHC was inadequate transferred data from the outside hospital CT scan. Most commonly, thin section data was not always included with the transferred images. These duplicate CT scans might have been avoided if all of the CT data had been transferred to the RTC using PACS technology rather than CD-ROM. Strategies should be introduced to minimize duplicate CT scans to improve patient care, reduce radiation exposure, and decrease hospital charges for trauma patients transferred from referring hospitals to our level 1 trauma center hospital.
Footnotes
Conflict of interest statement: All of the authors declare no potential conflicts of interest.
Presentations: Preliminary results of this study were submitted in abstract format for the 6th Annual Academic Surgical Congress, Huntington Beach, CA, in February 2011.
Author Contributions
Hunter B. Moore MD, Michael O’Keefe, MS, and Kalev Freeman, MD PhD made substantial contributions to all aspects of the paper: study design, literature search, data collection, analysis and interpretation, writing and critical revision.
Scott B. Loomis MD made substantial contributions to data collection, analysis and interpretation, writing and critical revision.
Kristen K. Destigter MD, George Ebert MD, Bruce Crookes MD, Stephen M. Leffler MD made substantial contributions to study design, data analysis and interpretation, writing and critical revision.
Travis Mann-Gow BS, Lee Dorf BS, Mary H. Streeter MS made substantial contributions to data collection, analysis and interpretation.
Contributor Information
Hunter B. Moore, Email: hunter.moore@ucdenver.edu.
Scott B. Loomis, Email: scott.loomis@vtmednet.org.
Kristen K. Destigter, Email: kristen.destigter@vtmednet.org.
Travis Mann-Gow, Email: tmanngow@uvm.edu.
Lee Dorf, Email: ldorf@med.uvm.edu.
Mary H. Streeter, Email: mary.streeter@vtmednet.org.
George Ebert, Email: george.ebert@vtmednet.org.
Bruce Crookes, Email: crookes@musc.edu.
Stephen M. Leffler, Email: stephen.leffler@vtmednet.org.
Michael O’Keefe, Email: michael.okeefe@uvm.edu.
Kalev Freeman, Email: kalev.freeman@uvm.edu.
References
- 1.Hsia RY, Shen YC. Rising closures of hospital trauma centers disproportionately burden vulnerable populations. Health Aff (Millwood) 2011;30(10):1912–20. doi: 10.1377/hlthaff.2011.0510. Epub 2011/10/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998–2007. JAMA. 2010;304(13):1465–71. doi: 10.1001/jama.2010.1408. Epub 2010/10/07. [DOI] [PubMed] [Google Scholar]
- 3.Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–84. doi: 10.1056/NEJMra072149. Epub 2007/11/30. [DOI] [PubMed] [Google Scholar]
- 4.Griffey RT, Sodickson A. Cumulative radiation exposure and cancer risk estimates in emergency department patients undergoing repeat or multiple CT. AJR Am J Roentgenol. 2009;192(4):887–92. doi: 10.2214/AJR.08.1351. Epub 2009/03/24. [DOI] [PubMed] [Google Scholar]
- 5.Hall EJ, Brenner DJ. Cancer risks from diagnostic radiology. Br J Radiol. 2008;81(965):362–78. doi: 10.1259/bjr/01948454. Epub 2008/04/29. [DOI] [PubMed] [Google Scholar]
- 6.Hui CM, MacGregor JH, Tien HC, Kortbeek JB. Radiation dose from initial trauma assessment and resuscitation: review of the literature. Can J Surg. 2009;52(2):147–52. Epub 2009/04/29. [PMC free article] [PubMed] [Google Scholar]
- 7.Stein SC, Fabbri A, Servadei F. Routine serial computed tomographic scans in mild traumatic brain injury: when are they cost-effective? J Trauma. 2008;65(1):66–72. doi: 10.1097/TA.0b013e318068d75f. Epub 2008/06/27. [DOI] [PubMed] [Google Scholar]
- 8.Weinberg JA, Magnotti LJ, Croce MA, Edwards NM, Fabian TC. The utility of serial computed tomography imaging of blunt splenic injury: still worth a second look? J Trauma. 2007;62(5):1143–7. doi: 10.1097/TA.0b013e318047b7c2. discussion 7–8. Epub 2007/05/15. [DOI] [PubMed] [Google Scholar]
- 9.Chwals WJ, Robinson AV, Sivit CJ, Alaedeen D, Fitzenrider E, Cizmar L. Computed tomography before transfer to a level I pediatric trauma center risks duplication with associated increased radiation exposure. J Pediatr Surg. 2008;43(12):2268–72. doi: 10.1016/j.jpedsurg.2008.08.061. Epub 2008/12/02. [DOI] [PubMed] [Google Scholar]
- 10.Gupta R, Greer SE, Martin ED. Inefficiencies in a rural trauma system: the burden of repeat imaging in interfacility transfers. J Trauma. 2010;69(2):253–5. doi: 10.1097/TA.0b013e3181e4d579. Epub 2010/08/12. [DOI] [PubMed] [Google Scholar]
- 11.Haley T, Ghaemmaghami V, Loftus T, Gerkin RD, Sterrett R, Ferrara JJ. Trauma: the impact of repeat imaging. Am J Surg. 2009;198(6):858–62. doi: 10.1016/j.amjsurg.2009.05.030. Epub 2009/12/09. [DOI] [PubMed] [Google Scholar]
- 12.Mohan D, Barnato AE, Angus DC, Rosengart MR. Determinants of compliance with transfer guidelines for trauma patients: a retrospective analysis of CT scans acquired prior to transfer to a Level I Trauma Center. Ann Surg. 2010;251(5):946–51. doi: 10.1097/SLA.0b013e3181d76cb5. Epub 2010/04/17. [DOI] [PubMed] [Google Scholar]
- 13.Cook SH, Fielding JR, Phillips JD. Repeat abdominal computed tomography scans after pediatric blunt abdominal trauma: missed injuries, extra costs, and unnecessary radiation exposure. J Pediatr Surg. 2010;45(10):2019–24. doi: 10.1016/j.jpedsurg.2010.06.007. Epub 2010/10/06. [DOI] [PubMed] [Google Scholar]
- 14.Brown CV, Weng J, Oh D, Salim A, Kasotakis G, Demetriades D, et al. Does routine serial computed tomography of the head influence management of traumatic brain injury? A prospective evaluation. J Trauma. 2004;57(5):939–43. doi: 10.1097/01.ta.0000149492.92558.03. Epub 2004/12/08. [DOI] [PubMed] [Google Scholar]
- 15.Cuff RF, Cogbill TH, Lambert PJ. Nonoperative management of blunt liver trauma: the value of follow-up abdominal computed tomography scans. Am Surg. 2000;66(4):332–6. Epub 2000/04/25. [PubMed] [Google Scholar]
- 16.Malcolm JB, Derweesh IH, Mehrazin R, DiBlasio CJ, Vance DD, Joshi S, et al. Nonoperative management of blunt renal trauma: is routine early follow-up imaging necessary? BMC Urol. 2008;8:11. doi: 10.1186/1471-2490-8-11. Epub 2008/09/05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharma OP, Oswanski MF, Singer D. Role of repeat computerized tomography in nonoperative management of solid organ trauma. Am Surg. 2005;71(3):244–9. Epub 2005/05/05. [PubMed] [Google Scholar]
- 18.Thaemert BC, Cogbill TH, Lambert PJ. Nonoperative management of splenic injury: are follow-up computed tomographic scans of any value? J Trauma. 1997;43(5):748–51. doi: 10.1097/00005373-199711000-00003. Epub 1997/12/09. [DOI] [PubMed] [Google Scholar]
- 19.Sung JC, Sodickson A, Ledbetter S. Outside CT imaging among emergency department transfer patients. J Am Coll Radiol. 2009;6(9):626–32. doi: 10.1016/j.jacr.2009.04.010. Epub 2009/09/02. [DOI] [PubMed] [Google Scholar]
- 20.Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169(22):2078–86. doi: 10.1001/archinternmed.2009.427. Epub 2009/12/17. [DOI] [PMC free article] [PubMed] [Google Scholar]