Dear Editor,
Testicular trauma is a frequent acquired cause of infertility; being accidents, work injuries and sport activities that are the most common causes of testicular traumas.1,2 Strangely, the issue of management of serious testicular trauma and fertility preservation has not been studied extensively before, existing only sporadic reports in international literature. Besides, no guidelines exist on fertility preservation in cases of important scrotal trauma when injury may result in irreparable damage to all testicular tissue (torsion of a solitary testis, bilateral synchronous testicular torsion, and severe bilateral scrotal trauma).3 The present case report describes the presentation of a young patient who experienced a motorbike accident with an irreparable damage to all testicular tissue in which preservation of fertility through immediate postoperative sperm cryopreservation was performed.
A 31-year-old male presented to the emergency department with acute scrotum after a motorbike accident resulting in a severe blunt trauma against the motorbike's fuel tank. The patient was healthy except for a history of infertility. On physical examination, the scrotum was tender and swollen with skin hematoma. Ultrasound scan (EsaOte, Genoa, Italy) with a 7.5 MHz linear-array probe showed ruptured right testis, with interruption of normal echo-rich line of the tunica albuginea. Testis was markedly heterogeneous (Figure 1a). Color flow Doppler ultrasound of the testicle showed a small, hypoechoic, inhomogeneous and completely avascular right testis (Figure 1b). Left testis appeared inhomogeneous, markedly hypovascular, especially at the upper pole and in the middle third where the profile was deformed.
Figure 1.
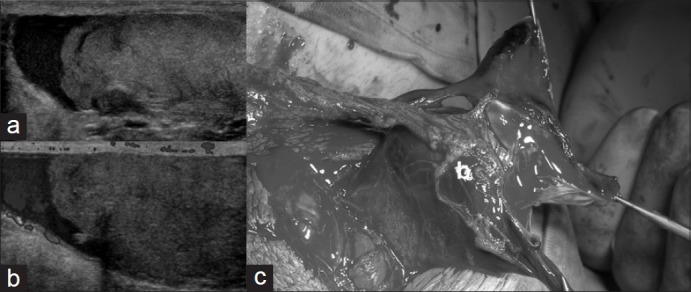
(a) Intraoperative right testis; (b) Sonographic B mode appearance; (c) Color flow Doppler ultrasound
Patient was urgently taken to the operating room for a scrotal exploration: right testis appeared completely uninhabited, parenchyma was destroyed, and right orchiectomy was performed (Figure 1c). On the left side, the testis presented a disruption of the tunica albuginea with an extrusion of more than 20% of the testicular parenchyma and the rest of testis was not bleeding and did not present a necrotic appearance. The epididymis and the mediastinum testis did not appear to be involved in the injury. After careful hemostasis, the tunica albuginea was sutured in an interrupted fashion. The patient remained stable throughout the operation (total time 47 min) and did not experience significant complications during his hospital course.
Adequate blood flow was consistently demonstrated in the left testicle postoperatively by serial Doppler evaluation. Ten days after surgery, patient underwent collection of seminal fluid revealing a sperm count of 40 million; the sperm was then cryopreserved to guarantee a future reproductive potential. The serum testosterone level was too low and for this reason, a hormone replacement therapy was set. Three months after injury, the patient reported normal erectile and ejaculatory function. Five months after the injury, spermiogram showed the onset of a cryptozoospermia and ultrasound revealed a left testicular volume decrease from 10 ml to 7 ml with an inhomogeneous, hypovascular area and the right emiscrotum completely uninhabited.
The topic of fertility preservation in patients with testicular trauma is noteworthy, but a literature review did not reveal consistent data discussing sperm or testicular tissue cryopreservation in patients suffering from scrotal trauma, existing only sporadic case report.4,5 Cryopreservation of sperm and testicular tissue has been successfully implemented in millions of patients suffering from conditions affecting their reproductive future. The majority of these cases are for young patients afflicted with cancer who underwent surgery that will jeopardize their reproductive ability.6,7 Unfortunately, despite progress in the refinement of fertility preservation techniques and the increase of educational resources, an information gap between patients and their healthcare teams persist.8 Therefore, this topic is often understated in clinical practice, especially when it is presented along with myriad other potential adverse effects.9
In rare clinical situations, injury may result in irreversible damage to all testicular tissues. Affected patients who are left permanently sterile require lifelong testosterone replacement therapy. Moreover, exogenous testosterone is known to suppress the release of gonadotropic hormones and may result in further reduction in testicular volume thus contributing to the atrophy and consequent azoospermia, which is observed in our patient. Such scenarios include torsion of a solitary testis, bilateral synchronous testicular torsion, and severe scrotal trauma, all of which are treated surgically. Fertility and testosterone production are the primary concerns of these individuals.
Traumatic rupture of the testis generally requires early scrotal exploration. Theoretically, nonviable testicular tissue that is not salvageable can be excised and an emergency testicular sperm extraction (TESE) can be performed; but an important limitation is the need for immediate access to an andrology laboratory for the freezing procedure that is not feasible in an emergency setting.
To our knowledge, only two case reports of an emergency TESE after scrotal trauma are described. In 2010, Ward et al.4 reported the case of a 24-year-old man presented with a life-threatening trauma in addition to severe genital trauma, including penile degloving, bilateral testicular avulsion, and bilateral spermatic cord laceration. In such case, a successful TESE and a testicular revascularization were performed. More recently, Gadda et al.5 described a case of successful TESE performed during an emergency scrotal exploration in a 28-year-old man with a history of right orchiopexy for cryptorchidism presenting with blunt trauma of the pelvis. Twelve hours after scrotal exploration, the extracted testicular tissue was successfully processed, and seven vials of sperms were frozen.
While this is still controversial, Woodruff et al.10 recently reported the case of a patient in which a successful cryopreservation of his sperm was performed two days after a torsion in his solitary testis. Similarly, our patient had almost total testicular loss after an important blunt scrotal trauma. Before surgery, considering his history of couple infertility, the patient expressed anxiety about future fertility: for this reason, a semen cryopreservation was planned in the early postoperative period. Unfortunately, semen analysis and cryopreservation are difficult to carry out in an emergency setting, but the procedure was successfully performed ten days after the surgery. Interestingly, three months after the surgery, the patient underwent another seminal examination and was found azoospermic. It was then postulated that within 10 days after injury, it is still possible to retrieve the sperm cells that were previously developed and passed into the seminal pathways.
Our study emphasizes that cryopreservation of semen as soon as possible after an important scrotal traumatic event should be mandatory to avoid eventual subsequent infertility, mainly with traumas affecting both testes or when only a single testis working partially.
AUTHOR CONTRIBUTIONS
GL, NP, DAG, SB and GM cared for the patient and collected clinical information. GO, BDC performed the laboratory tests. GL, NP drafted the manuscript, which was revised by CT, GM and SB. GL, NP, GDA took part in critical discussion.
COMPETING INTERESTS
All authors declare no competing interests.
REFERENCES
- 1.Shaul DB, Xie HW, Diaz JF, Mahnovski V, Hardy BE. Surgical treatment of testicular trauma: effects on fertility and testicular histology. J Pediatr Surg. 1997;32:84–7. doi: 10.1016/s0022-3468(97)90101-9. [DOI] [PubMed] [Google Scholar]
- 2.Kukadia AN, Ercole CJ, Gleich P, Hensleigh H, Pryor JL. Testicular trauma: potential impact on reproductive function. J Urol. 1996;156:1643–6. doi: 10.1016/s0022-5347(01)65472-7. [DOI] [PubMed] [Google Scholar]
- 3.Stahl PJ, Stember DS, Hsiao W, Schlegel PN. Indications and strategies for fertility preservation in men. Clin Obstet Gynecol. 2010;53:815–27. doi: 10.1097/GRF.0b013e3181f980b3. [DOI] [PubMed] [Google Scholar]
- 4.Ward MA, Burgess PL, Williams DH, Herrforth CE, Bentz ML, et al. Threatened fertility and gonadal function after a polytraumatic, lifethreatening injury. J Emerg Trauma Shock. 2010;3:199–203. doi: 10.4103/0974-2700.62110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gadda F, Spinelli MG, Cozzi G, Paffoni A, Carmignani L, et al. Emergency testicular sperm extraction after scrotal trauma in a patient with a history of contralateral orchiopexy for cryptorchidism: case report and review of the literature. Fertil Steril. 2012;97:1074–7. doi: 10.1016/j.fertnstert.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 6.Morewood T. Fertility preservation in male cancer patients. J Obstet Gynaecol. 2013;33:547. [Google Scholar]
- 7.Sheth KR, Sharma V, Helfand BT, Cashy J, Smith K, et al. Improved fertility preservation care for male patients with cancer after establishment of formalized oncofertility program. J Urol. 2012;187:979–86. doi: 10.1016/j.juro.2011.10.154. [DOI] [PubMed] [Google Scholar]
- 8.Snyder KA, Pearse W. Discussing fertility preservation options with patients with cancer. JAMA. 2011;306:202–3. doi: 10.1001/jama.2011.973. [DOI] [PubMed] [Google Scholar]
- 9.Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Oncologists’ attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol. 2002;20:1890–7. doi: 10.1200/JCO.2002.07.174. [DOI] [PubMed] [Google Scholar]
- 10.Woodruff DY, Horwitz G, Weigel J, Nangia AK. Fertility preservation following torsion and severe ischemic injury of a solitary testis. Fertil Steril. 2010;94:352.e4–5. doi: 10.1016/j.fertnstert.2009.12.057. [DOI] [PubMed] [Google Scholar]


