Abstract
College freshmen face a variety of academic and social challenges as they adjust to college life that can place them at risk for a number of negative outcomes, including depression and alcohol-related problems. Orientation classes that focus on teaching incoming students how to better cope with college-oriented stress may provide an opportunity to prevent the development of these adjustment problems. This article outlines a program based on behavioral activation that can be integrated into college orientation programs to provide a more comprehensive orientation experience. Data are presented from an initial pilot study in which 71 first-semester freshman at the University of Maryland participated in a 15-week, 2 hr per week orientation class (n = 37 in the behavioral activation-enhanced orientation classes and n = 34 in the control orientation as usual classes). Students’ depression and alcohol use were evaluated at the beginning, middle, and end of the course. Results indicated a Time × Group interaction such that problem drinking (but not consumption) was significantly reduced across assessments in the behavioral activation classes and largely unchanged in the standard classes. No difference was observed in depression scores; however, fairly low depression scores across the 3 time points may have limited the opportunity to observe any meaningful impact of the orientation classes on depression. The authors conclude with a discussion of the implications of their findings for preventing adjustment problems among incoming college students and future directions.
Keywords: behavioral activation, college students, alcohol problems, depression
The transition from high school to college presents many changes in the lives of freshman students. Although attending college has demonstrable benefits for the development of new social networks and skills, academic pursuits, and ultimately occupational advancement (e.g., Pascarella, & Terenzini, 1991), the critical transition into this new context also has the potential to test an individual’s experience of comfort and safety as well as ability to enjoy rewarding activities (Bernier, Larose, & Whipple, 2005). College freshmen face a variety of academic and social challenges (e.g., establishing a new social system, living away from home for the first time, academic stressors, less structure/greater independence) as they adjust to college life that can place them at risk for a number of negative outcomes, including depression and alcohol-related problems (Bernier et al., 2005; Rodgers & Tennison, 2009; Soucy & Larose, 2000).
Depression among university students is prevalent and is associated with a variety of negative sequelae. Rates of depression among university students range from 15% to 20%, with increasing incidence in the past two decades (Benton, Robertson, Tseng, Newton, & Benton, 2003; Hoban, 2007; Voelker, 2003). Depression can lead to serious impairment among university students, including an impact on academic performance and school retention (Fazio & Palm, 1998; Pritchard & Wilson, 2003). Symptoms of depression may be particularly evident as students adjust to the transition into university life (Sarason & Sarason, 1999). Specifically, individuals may be more likely to experience feelings of hopelessness and sadness during this transition period if they are having difficulty coping with the stress associated with this life adjustment effectively (Dyson & Renk, 2006; Quinn, 1997).
In addition to depression, problematic alcohol use is highly prevalent among university students. Individuals entering college show marked increases in alcohol use, compared with those who live at home or obtain jobs following graduation from high school (Johnston, O’Malley, Bachman, & Schulenberg, 2009). For example, college students engage in heavy episodic use (i.e., having five or more drinks in a row at least once in the past 2 weeks) significantly more often than other young adults (40% vs. 30%; Johnston et al., 2009). However, in high school, college-bound seniors are less likely to report heavy drinking than noncollege-bound youth. This suggests that emerging older adolescents in college “catch up to and pass” their noncollege-attending peers (Johnston et al., 2009). Alcohol is considered to be a prominent part of the college culture, present at most social functions and part of many peer interactions (Thombs, 1999). Approximately 8% of undergraduate college students meet criteria for alcohol abuse according to the Diagnostic Statistical Manual of Mental Disorders, fourth edition (DSM–IV; American Psychiatric Association, 1994), and another 11% can be classified as DSM–IV alcohol-dependent (Dawson, Grant, Stinson, & Chou, 2004). Heavy episodic drinking carries serious consequences and places college students at an increased risk for accidental injury, unplanned and unsafe sex, and a host of social and psychological problems (Wechsler, Davenport, Dowdall, Moeykens, & Castillo, 1994; Wechsler et al., 2002; Wechsler, Lee, Kuo, & Lee, 2000). Importantly, alcohol problems are evident in the early stages of college attendance, suggesting the potential utility and relevance of early intervention (Adams & Nagoshi, 1999; Reifman & Watson, 2003).
One existing resource for addressing difficulties associated with the transition to college is prolonged freshman orientation programs. Such programs have become so ubiquitous that in a recent survey conducted by the National Resource Center for The First-Year Experience and Students in Transition, 84.8% of institutions responded that they offer first-year seminars compared with 73.9% in 2000 (Tobolowsky, 2008). The content of semester-long orientation courses varies by university but typically contains information on academic policies, health and wellness, substance abuse, time management, and academic success (Rock, Coates, & Greco, 2005). These programs are based in the framework that adding extra support will increase important outcomes such as retention, student development, and access to university resources. In such domains, these programs have had some success, particularly on retention (e.g., Chapman & Reed, 1987; Potts & Schultz, 2008). In light of the potential substance use and mental health issues that are often encountered by university students, these orientation classes represent an ideal setting for prevention/early intervention efforts.
An intervention that may be a promising adjunct to standard orientation programs is behavioral activation (Jacobson et al., 1996; Lejuez, Hopko, LePage, Hopko, & McNeil, 2001). This behavioral approach, developed from early theoretical and empirical work by Ferster (1973) and Lewinsohn (Lewinsohn, 1974; Lewinsohn & Graf, 1973), targets greater contact with more valued environments through systematic efforts to increase rewarding experiences/enjoyment of daily activities, which may simultaneously reduce negative affect and improve positive affect through overt behavior change (Hopko, Lejuez, Ruggiero, & Eifert, 2003). Although behavioral activation can be provided in a more extensive protocol (Martell, Addis, & Jacobson, 2001; Martell, Dimidjian, & Herman-Dunn, 2010), application in this type of orientation setting may be best with the shorter and more activation-specific protocol referred to as the Brief Behavioral Activation Treatment for Depression (BATD; Hopko & Lejuez, 2007; Lejuez, Hopko, & Hopko, 2001). BATD has been used effectively with a variety of clinical and community populations (Daughters et al., 2008; Hopko et al., 2008; Hopko, Lejuez, LePage, Hopko, & McNeil, 2003; Jacobson et al., 1996; Lejuez et al., 2001). In addition, a growing body of literature supports the utility of behavioral activation strategies for treating depression in adolescents and young adults (Gaynor & Harris, 2008; McCarty & Weisz, 2007; Ruggiero, Morris, Hopko, & Lejuez, 2007). Although BATD has been used most often as an intervention for those with clinical levels of depressive symptoms, the approach also has potential utility in the prevention of depression (Stice, Burton, Bearman, & Rohde, 2007). Specifically, low rates of pleasant activities have been found to predict future depressive symptoms during adolescence (Clarke et al., 1992), thus working to increase contact with more valued environments may operate as a prophylactic against the development of depression.
Although most often used as a depression intervention, BATD also has clear relevance for intervening on substance use, with data showing promise in samples of community smokers (MacPherson et al., 2010) and substance users in residential treatment (Magidson et al., 2011). Providing conceptual support, behavioral economic theory and related empirical research have suggested that substance abuse is associated with diminished engagement in enjoyable substance-free activities/reinforcement (Murphy, Correia, & Barnett, 2007). For instance, large surveys of college students have demonstrated an inverse relationship between alcohol use and engagement in a range of substance-free activities (e.g., volunteer work and campus activities; Fenzel, 2005; Weitzman & Kawachi, 2000). According to behavioral economic theory, higher rates of substance abuse are most likely in contexts lacking substance-free sources of reinforcement. As such, it is thought that substance abuse will generally decrease if access to alternative reinforcers is increased (Higgins, Heil, & Plebani-Lussier, 2004). Much of this work has been applied effectively to college student drinking. For example, college students who were instructed to increase exercise and creative activities reported a reduction in drinking in comparison to the control condition in which students were not instructed to change their participation in substance-free activities (Correia, Benson, & Carey, 2005). In line with this model, BATD may prove useful as an approach for college orientation classes to decrease alcohol abuse by increasing engagement in rewarding alternatives to substance use.
Toward this end, we conducted a small-scale trial of a novel intervention incorporating BATD within a standard college orientation program with a focus on depression and alcohol use. The comparison condition received the standard college orientation program (ST), matched for overall contact time. We hypothesized participants in the BATD-enhanced college orientation program would evidence lower depression and alcohol problems across the three assessments: beginning of the semester/Week 2, midsemester/Week 7, and end of semester/Week 15.
Method
Participants and Procedures
In collaboration with the Director of Orientations at the University of Maryland, four sections of the existing semester-long college orientation program were modified and taught by Center for Addictions, Personality, and Emotion (CAPER) staff under the Director of Orientations’ supervision. Each section was randomly assigned to a treatment condition, with two sections assigned to BATD and two assigned to ST. Students enrolled into the four offered sections of the course independent of the research (registered using the university online system). The four sections were paired such that a BATD and a control class were offered at the same time. The Director of Orientations was closely involved in the design of the BATD course curriculum and ensured that the standard components of the original program remained as the core foundation of the class (see the Intervention section for description of the classes).
Students enrolled in the four-course sections were offered opportunities to participate in the assessment portion of the study. Student enrollment into the classes occurred independently of the study. Students in both the BATD and ST courses were given the option to participate in the study by voluntarily filling out questionnaire packets at three time points during the semester (beginning of the semester/Week 2, midsemester/Week 7, and end of semester/Week 15) in return for extra credit. Participation in the study was completely voluntary. To ensure that completion of questionnaires was not coercive, alternative extra credit assignments equated for time were offered. Students interested in these alternative extra credit assignments were directed to a University of Maryland affiliated online site that lists study opportunities that require the same time commitment (and thus extra credit opportunity) as the present study.
Research assistants coordinated the research participation in both the present study as well as the alternative studies offered for extra credit. Research assistants were not affiliated in any way with the courses so as to prevent the instructors or teaching assistants associated with the courses from becoming aware of which students participated in the present study (vs. alternative extra credit opportunities). Research assistants were blind to the class condition as well as the study hypotheses. At the beginning of the semester, research assistants provided information about the study and obtained written consent in the absence of the course instructor. If a student was under the age of 18, a parental permission form was required and the student signed an assent form. All study procedures were approved by the University of Maryland Institutional Review Board.
Of the 73 potential participants initially enrolled in the four sections of the semester-long college orientation program (i.e., 73 = total enrollment in the four selected sections), 71 consented to participate (97.3%), 70 participated in the first data collection (98.6%), 64 in the second data collection (90.1%), and 66 in the third data collection (93.0%). Eighty-eight percent of students had data at all three time points. Primary analyses included the 71 individuals who consented to participate in the study (34 participants in ST and 37 in BATD). The final sample was 54.3% female, with a mean age of 17.91 years (SD = 0.53). Racial distribution was as follows: 57.7% White (not of Hispanic origin), 12.7% African American, 11.3% Hispanic, 8.5% Asian or Pacific Islander, 5.6% Asian Indian, and 4.2% self-identified as “other.” The demographic characteristics of the study sample are largely consistent with the gender and racial distribution of the university undergraduate student body. The mean depression score at the first assessment (M = 5.00, SD = 6.14) fell into the normal range and is comparable to other reports using the Depression Anxiety Stress Scales (DASS-21; Lovibond & Lovibond, 1995) in college samples (Mahmoud, Hall, & Staten, 2010; Norton, 2007), with reported means of 7.70 (SD = 8.10) and 4.27 (SD = 4.32), respectively. The percent above the clinical cutoff on the Alcohol Use Diagnostic Identification Test (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993), 28.8%, is comparable to other studies of freshman college students, indicating that typically 26%–37% score above the clinical cutoff on the Alcohol Use Disorders Identification Test (AUDIT; e.g., Saitz et al., 2007).
Intervention
An extensive syllabus was used to ensure that all course instructors provided the same material over the course of the semester. The BATD-enhanced courses included all core components outlined as part of the orientation program in addition to the BATD-specific strategies. As mentioned earlier, the Director of Orientations was closely involved in ensuring that the BATD course retained all components included in the ST course and met on a biweekly basis with CAPER staff to ensure that standard components were being adequately implemented. Below are brief descriptions of the ST course and the BATD course.
ST
This class was designed to facilitate student adjustment to the University of Maryland campus and academic life. Classes were structured as discussions on a wide array of topics, including academic skills, career exploration, library resources, study abroad, campus safety, responsible decision making, academic honesty, sexuality, and diversity. In addition, students were helped to identify resources available at the University of Maryland and were encouraged to make contact with a faculty advisor to ensure academic guidance. Students in these classes were assigned weekly journal entries in which they were asked to reflect on the process of adjusting to college life. The class included time set aside each week for supportive listening about the process of adjusting to college life. Each class lasted 2 hr and met once a week.
BATD
As mentioned previously, all components of the standard orientation class were included. In addition, the BATD classes expanded on several components of the orientation course by replacing journaling and supportive discussion with BATD strategies. Week 1 began with the instructor providing the rationale focused on structuring a variety of reinforcing activities to promote a rewarding college lifestyle. The instructor also introduced activity monitoring, which involved recording of all daily activities as well as associated level of enjoyment. Completion of daily activity monitoring was assigned to occur each day of the following week (this assignment was completed for Weeks 1–3). During Week 2, the instructor led the group in a review of daily activity monitoring completed for each day of the previous week. Next, the instructor introduced the topic of goals and values. During Week 3, the students worked on identifying their values and life goals within various life domains, including school, social relationships, family, financial, hobbies/recreation, volunteer work, physical/health issues, and spirituality/personal growth. In Week 4, the goals and values identified in Week 3 were used to identify important and/or enjoyable activities in line with the valued directions. Several activities were then planned for the coming week using the behavioral checkout form, which allowed participants to track their activities and progress toward achieving weekly goals. For homework, students were instructed to record engagement in each planned activity. Sessions 5–14 focused on the behavioral checkout form starting with monitoring of planned activities from the previous week and then planning of activities for the coming week. Students were asked to regularly monitor their engagement in these activities and identify potential obstacles (as well as ways to overcome these obstacles) to goal fulfillment. Particular attention was placed on the identification of positive events affiliated with these goals. Each class lasted 2 hr and met once a week, resulting in similar attention and contact time across conditions.
Therapists
Therapists were three females and one male; two had clinical psychology doctoral degrees (one in each condition) and two were clinical psychology doctoral students (one in each condition). All completed training with the supervisor that included a 4-hr workshop for both treatments. Weekly supervision was conducted for all therapists.
Measures
Demographics
Sociodemographics, including age, gender, and race/ethnicity, were collected at the first assessment.
Depression
The Depression subscale of the 21-item version of the DASS-21 (Lovibond & Lovibond, 1995) was used to assess depressive symptoms. The seven-item Depression subscale assesses dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest or involvement, anhedonia, and inertia. Respondents indicate the extent to which they experienced each of the symptoms depicted in the items during the previous week on a 4-point Likert-type scale between 0 (Did not apply to me at all) and 3 (Applied to me very much, or most of the time). The DASS-21 was developed by selecting the highest loading items from each scale of the original 42-item version of the DASS (Lovibond & Lovibond, 1995). Lovibond and Lovibond (1995) and others (e.g., Henry & Crawford, 2005) have demonstrated that the DASS-21 is psychometrically equivalent to the original DASS. In an undergraduate sample, Lovibond and Lovibond (1995) validated the DASS against widely used measures of depression, and the DASS Depression subscale was found to be highly associated with the Beck Depression Inventory (r = 0.74; Beck & Steer, 1987) and demonstrated strong internal consistencies across subscales (α= .91 for Depression). For the present sample, internal consistency for Assessments 1, 2 and 3 was 0.82, 0.85, and 0.88, respectively.
Alcohol problems
The AUDIT (Saunders et al., 1993) was developed by the World Health Organization to identify persons whose alcohol consumption has become hazardous or harmful to their health. The AUDIT has 10 items that assesses frequency of drinking, typical quantity, frequency of heavy drinking, impaired control over drinking, increased salience of drinking, morning drinking, guilt after drinking, blackouts, alcohol-related injuries, and others concerned about. Each of the questions has a set of responses to choose from, and each response has a score ranging from 0 to 4. A total score of 8 or more has been found to indicate a strong likelihood of hazardous or harmful alcohol consumption (e.g., Babor, Higgins-Biddle, Saunders, & Monteiro, 2006; Conigrave, Hall, & Saunders, 1995; Kokotailo et al., 2004). In addition to examining percent above the clinical cutoff, the AUDIT has also been examined as two subscales (O’Hare, 2005; O’Hare & Sherrer, 1999): alcohol consumption (the first three items that assess frequency and amount of drinking) and alcohol problems (the last seven items that assess tolerance, withdrawal, and other negative consequences associated with alcohol use), with higher scores on each subscale indicative of greater alcohol consumption and greater alcohol problems, respectively. Both approaches (subscales and percent above the clinical cutoff on the total scale) were used in the present study.
Statistical Analyses
First, the two groups were compared on all demographic, depression, and alcohol problem variables to ensure equivalence of groups at the first assessment. Next, relationships between the demographic and outcome variables were examined in order to determine which variables would be included as covariates. Finally, to examine differential effects of treatment on depression and on alcohol consumption/problems, generalized estimating equations (GEEs; Liang & Zeger, 1986; Zeger & Liang, 1986) analyses were used for variables assessed at all three time points. GEE allows for inclusion of either categorical or continuous dependent variables and is advantageous when examining multiple observations that are correlated across time. Compared with traditional methods such as repeated analysis of variance and multivariate analysis of variance, GEE has several advantages, including robustness against choice of correlation matrix and ability to use all available data for analysis (i.e., GEE data analyses do not require complete data at all three time points; Liu, Dixon, Qiu, Tian, & McCorkle, 2009). GEE is a “marginal” or population-averaged model, and thus parameter estimates represent the effects averaged across clusters, with parameters and their standard errors adjusted to take into account the clustering of the data in a two-level structure (e.g., repeated observations nested in subjects) (Liang & Zeger, 1986). All analyses were conducted in PASW version 18. For analyses conducted with the AUDIT cutoff scores, the logit link function and an independent correlation matrix were specified. For all other analyses with continuous outcomes, an identity link function and an independent correlation matrix were specified. The centered linear effect of time was included. Models also included the quadratic effect of time to allow for examination of any potential acceleration or deceleration in the rate of change of depressive symptoms or alcohol problems, although we did not have a priori hypotheses to this effect. As there were four classes assigned to treatment conditions, class was included as a four-level covariate in the GEE analyses (Pocock, Assmann, Enos, & Kasten, 2002).1 Exclusion of this covariate from analyses did not alter the statistical significance of any reported effect; however, it was retained in all models in line with the original design of the study. Thus for each outcome investigated, the main effects model included the effect of class, the effect of treatment group, the effects of time (linear and quadratic), and the interaction of the group effect and the linear effect of time. Evaluation of main effects was followed by models that included interactions of treatment condition with both the linear time and the quadratic time effects in the final block. Estimates of significant Treatment Group × Linear Time interactions are reported using models after removing any nonsignificant quadratic time interactions (e.g., MacPherson et al., 2007).
Results
On the basis of independent samples t tests and chi-square analyses, the BATD and ST groups did not differ on any demographic variable or first assessment depression and alcohol consumption/problems (see Table 1). Gender, age, and race/ethnicity were each not related to depression and alcohol consumption/problems and thus were not included as covariates in the subsequent analyses (all ps > .07). Table 2 displays the group means for the outcome variables across the three time points.
Table 1.
Comparisons on Demographic, Depression, and Alcohol Problem Variables Across Treatment Condition at the First Assessment
| Characteristics | BATD (n= 37) |
ST (n= 34) |
p |
|---|---|---|---|
| Demographic variables | |||
| Age, Mean (SD) | 17.85 (0.36) | 17.97 (0.65) | .35 |
| Gender (% female) | 54.1 | 54.4 | .97 |
| Ethnicity | .61 | ||
| % White | 64.9 | 50.0 | |
| % African American | 8.1 | 17.6 | |
| % Hispanic | 8.1 | 14.7 | |
| % Asian or Pacific Islander | 10.8 | 5.9 | |
| % Asian Indian | 5.4 | 5.9 | |
| % “Other” | 2.7 | 5.9 | |
| Outcome variables | |||
| DASS-DEP, Mean (SD) | 5.51 (5.63) | 4.59 (6.87) | .54 |
| AUDIT % above clinical cutoff | 36.1 | 23.5 | .25 |
| AUDIT-C | 4.16 (2.83) | 3.65 (2.76) | .50 |
| AUDIT-P, Mean (SD) | 1.78 (1.99) | 1.50 (2.68) | .62 |
Note. BATD = Behavioral Activation Treatment for Depression; ST = standard college orientation program; DASS-DEP = Depression subscale of the 21-item version of the Depression Anxiety Stress Scales; AUDIT = Alcohol Use Disorders Identification Test; C = Consumption subscale; P = Alcohol Problems subscale.
Table 2.
Depression and AUDIT Scores for Each Condition Across the Three Time Points
| Condition | BATD (n= 37) | ST (n= 34) |
|---|---|---|
| DASS-DEP, Mean (SD) | ||
| Time 1 | 5.51 (5.63) | 4.59 (6.87) |
| Time 2 | 9.70 (7.80) | 5.87 (6.91) |
| Time 3 | 8.67 (7.88) | 6.18 (8.24) |
| AUDIT % above clinical cutoff | ||
| Time 1 | 36.1 | 23.5 |
| Time 2 | 38.2 | 36.7 |
| Time 3 | 12.1 | 27.3 |
| AUDIT-C, Mean (SD) | ||
| Time 1 | 4.16 (2.83) | 3.65 (2.76) |
| Time 2 | 4.27 (3.15) | 4.44 (3.14) |
| Time 3 | 3.57 (2.70) | 3.58 (3.21) |
| AUDIT-P, Mean (SD) | ||
| Time 1 | 1.78 (1.99) | 1.50 (2.68) |
| Time 2 | 1.76 (2.99) | 1.60 (2.61) |
| Time 3 | 0.55 (1.50) | 1.27 (2.17) |
Note. BATD = Behavioral Activation Treatment for Depression; ST = standard college orientation program; DASS-DEP = Depression subscale of the 21-item version of the Depression Anxiety Stress Scales; AUDIT = Alcohol Use Disorders Identification Test; C = consumption subscale; P = Alcohol problems subscale.
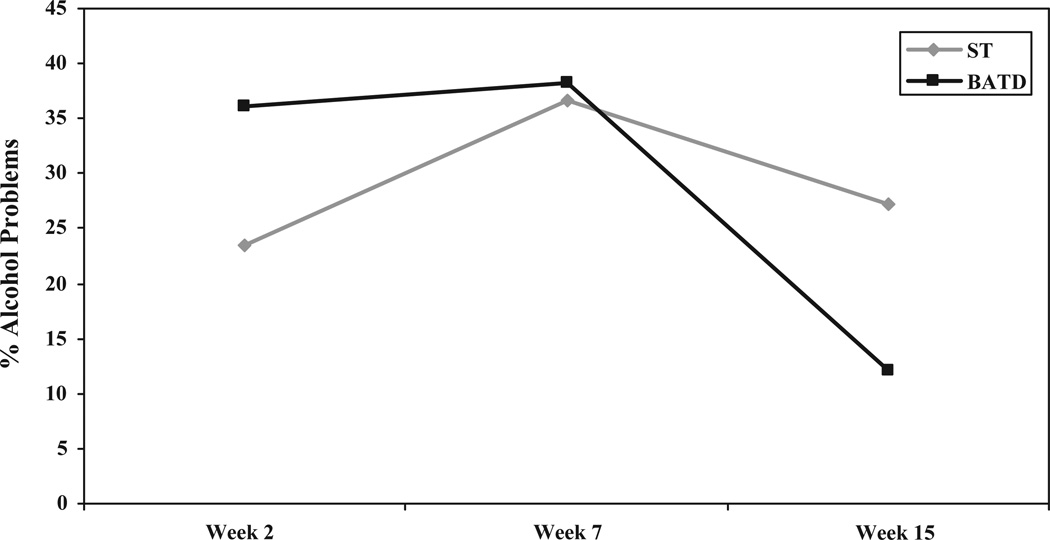
The AUDIT was examined dichotomously using the clinical cutoff as well as continuously with each of the subscales (consumption and problems). When examining the AUDIT dichotomously using the clinical cutoff, results indicated no significant main effect of orientation group (BATD vs. ST) in the AUDIT clinical cutoff (reference group = above alcohol problem cutoff) across the three time points (OR = 1.14, 95% CI [0.47, 2.79], p = .77). Nor was there an effect of class (OR = 1.11, 95% CI [0.78, 1.59], p = .56) or the main linear effect of time (OR = 1.32, 95% CI [0.96, 1.83], p = .09). However, the quadratic effect of time was significant (OR = 1.86, 95% CI [1.22, 2.83], p = .004) as was the interaction of the orientation group effect with the linear effect of time (OR = 2.20, 95% CI [1.12, 4.35], p =.02). The interaction of the orientation group effect with the quadratic effect of time was not significant (OR = 1.27, 95% CI [0.55, 2.96], p = .57). Following procedures outlined by Chinn (2000), we computed effect sizes from the model derived odds ratios for the interaction between orientation group and the linear effect of time. On the basis of these procedures, the derived effect size was d =0.44, indicating a medium effect for the change over time in the BATD versus the ST condition. As can be seen in Figure 1, the quadratic effect of time indicates that across orientation groups, there was a differential rate of change over time in the percentage of youth above the clinical cutoff. However, the significant linear effect of the Time × Orientation Group interaction indicates there was a general increase over time in the percentage of youth above the clinical cutoff in the ST. Conversely, the overall percentage of youth above the clinical cutoff for the BATD group exhibited a general decrease over time. Thus, overall, the odds of being above the clinical cutoff decreased for the BATD group, but increased slightly for the ST group.
Figure 1.
Percent above the Alcohol Use Disorders Identification Test (AUDIT) clinical cutoff across the three time points. ST = standard college orientation program; BATD = Behavioral Activation Treatment for Depression.
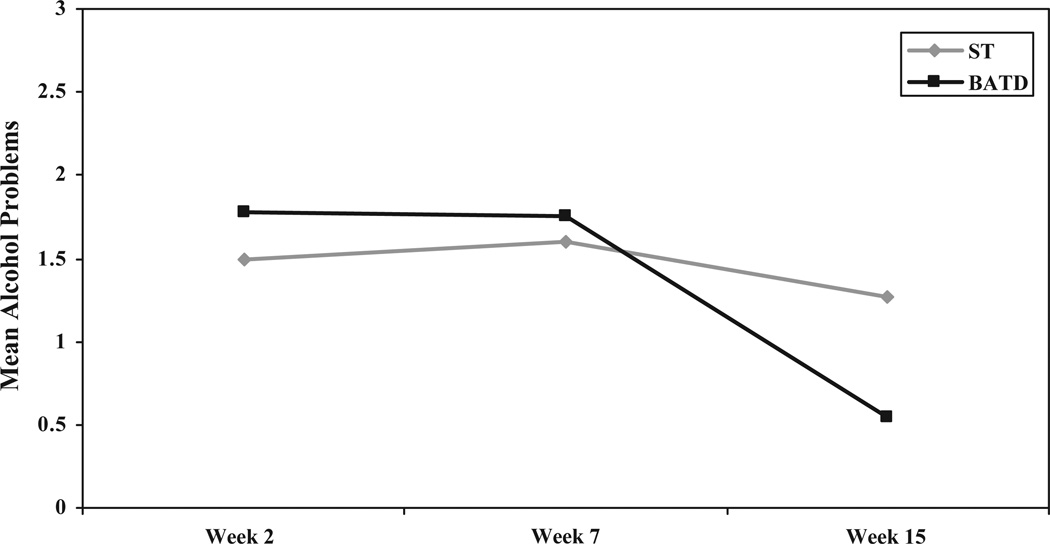
Next, we examined the two AUDIT subscales. For the Alcohol Consumption subscale, results indicated no significant main effect of class (B = −0.09, SE = 0.29, p = .76), orientation group (B = −0.05, SE = 0.70, p = .94), or for the main linear effect of time (B = −0.15, SE = 0.15, p = .30). However, there was a main quadratic effect of time (B = −0.73, SE = 0.28, p = .01), indicating that the average level of consumption as reported on the AUDIT-C was decreasing over time but that this rate of change was decelerating. Neither the interaction of the group effect with the linear time effect (B = −0.34, SE = 0.29, p = .25) nor with the quadratic time effect (B = 0.75, SE = 0.56, p = .18) was significant. The derived effect size for orientation group on alcohol consumption was d = 0.09, indicating a small effect for the BATD condition. For the Alcohol Problems subscale, the results indicated no significant main effect of class (B = −0.23, SE = 0.19, p = .23), orientation group (B = −0.15, SE = 0.51, p = .76), or the quadratic effect of time (B = −0.44, SE = 0.26, p = .09). There was a significant linear effect of time (B = −0.39, SE = 0.12, p = .002), but this should be interpreted in the context of a significant Orientation Group × Linear Effect of Time interaction (B = −0.48, SE = 0.24, p = .005). The derived effect size for the interaction was d = 0.22, indicating a small effect for the change over time in the BATD versus the ST condition. As seen in Figure 2, the ST group exhibited minimal change in alcohol problems over time, whereas similar to the clinical cutoff analyses, the mean alcohol problems for the BATD group decreased from the first through the third assessments. The interaction of the quadratic effect of time with orientation group was not significant (p = .52).
Figure 2.
Mean alcohol problems (Audit Problems subscale) across the three time points. ST = standard college orientation program; BATD = Behavioral Activation Treatment for Depression.
Regarding depressive symptom scores, mean values were higher at every assessment for the BATD group compared with ST, but results indicated no significant difference between the BATD and ST groups in depression across the three time points (B = 2.34, SE = 1.48, p = .11, d = 0.32). The main linear (B = 1.25, SE = 0.44, p = .005) and quadratic (B = −1.64, SE = .67, p = .02) effects of time were significant. The interaction of the group effect with the linear effect of time (B = 0.70, SE = 0.88, p = .43) was not significant, nor was the interaction of the group effect with the quadratic effect of time (B = −2.09, SE = 1.32, p = .12).
Discussion
College freshmen face a variety of academic and social challenges as they adjust to college life, which can place them at risk for a number of negative outcomes, including depression and alcohol-related problems. To address the difficulties associated with the transition to college, we sought to conduct a small-scale trial in the present study of a novel intervention incorporating behavioral activation strategies into an existing semester-long standard college orientation program. Two classes of the BATD-enhanced program were compared with two classes of the standard orientation program on depression symptoms and alcohol problems across three time points: beginning of the semester/Week 2, midsemester/Week 7, and end of semester/Week 15. A significant Treatment Group × Linear Effect of Time interaction was observed for alcohol problems (both with the percent above the clinical cutoff as well as the Alcohol Problems subscale). Results indicated no significant difference in depression scores as well as alcohol consumption between the two groups across the three time points.
In terms of the alcohol problems findings, a significant interaction of the orientation group effect with the linear effect of time was found, suggesting differential change for the BATD and ST groups across the three time points. The overall percentage of youth above the clinical cutoff for the BATD group generally decreased over time. Conversely, there was a noticeable increase in the percentage of youth in ST above the clinical cutoff from the first to the second assessment, with only a modest decline from the second to third assessments. Thus, the odds of being above the clinical cutoff for alcohol problems decreased between the second and third assessment for the BATD group compared with the ST group. When comparing the first and third assessments, the percentage of the BATD group above the clinical cutoff decreased by 24%, and the percentage of the ST group above the clinical cutoff increased about 4%. A similar significant pattern of results was observed when the AUDIT Alcohol Problems subscale was examined. However, there was no significant difference observed between the BATD and ST groups with the Alcohol Consumption subscale across the three time points. These results provide initial support for the utility the BATD-enhanced college orientation program to reduce problem drinking among first-semester college freshman.
On the basis of the subscale analyses, it is important to note that the BATD did not impact alcohol consumption (subscale that assessed frequency of drinking, typical quantity, and frequency of heavy drinking) but instead impacted alcohol problems (subscale that assessed impaired control over drinking, increased salience of drinking, morning drinking, guilt after drinking, blackouts, alcohol-related injuries, and others concerned about drinking). As such, these data suggest that the BATD orientation group had a reduction in the consequences associated with their drinking rather than the amount or regularity of their drinking. In line with the reinforcement theoretical framework underlying BATD as well as behavioral economic theory, higher rates of alcohol problems are most likely in contexts lacking substance-free sources of reinforcement, and thus increasing engagement in pleasurable, nonalcohol-related activities may help to decrease problematic levels of use. College students who routinely experience problems related to their use may miss or avoid opportunities to participate in the social, athletic, and cultural activities that are part of college life. It may be that this program that aims to have students identify values and goals within various life domains and specific important and/or enjoyable activities in line with the valued directions helps college freshman build a life with more options for substance-free sources of reinforcement. The focus on values in BATD may create buffers for individuals to limit problems even if their consumption rate does not change. Although reducing consumption is clearly important, limiting the negative consequences of drinking, possibly through the positive benefits of BATD, is an exciting and important possibility.
For depression, the only significant finding was a significant quadratic effect of time, as evidenced by a general increase in depression level across conditions between the first and second assessment, and then a leveling off between the second and third assessments. It is somewhat surprising that an increase was observed, and without a “no orientation program” control group, it is hard to determine whether the elevations would have been higher without either program. Somewhat surprisingly, GEE analyses indicated no significant difference between the BATD and ST groups in depression across the three time points. In fact, there was a nonsignificant but small effect indicating higher scores in BATD through the final assessment. The inability to observe any meaningful positive impact of BATD on depression may have been due to the fact that participants were not selected on the basis of elevated depression scores, and the resulting levels of depression were low across the three time points (mean scores < 10; Henry & Crawford, 2005). As a result, it is unclear what any movement—positive or negative—within the normal range of depression actually means clinically. Further research is needed to understand how these findings compare with general trends in depression symptoms for college students during the incoming year as well as whether a longer term follow-up would demonstrate differential effects for the two groups.
It is important to note some study limitations and future directions. First, even though the initial difference in the percentage of students above the cutoff on the AUDIT was not significantly different between the BATD and ST groups, the higher percentage of students with problem drinking at Time 1 might have been partly responsible for the greater decrease in the percentage of students with problem drinking between Time 1, Time 2, and Time 3 among those in the BATD condition. Second, given the study’s experimental design, manipulation checks would have been useful to make sure that participants actually experienced the changes that the BATD condition was supposed to create. Thus, a manipulation check and/or measure of participant compliance will be critical in future research (Busch, Uebelacker, Kalibatseva, & Miller, 2010). In addition, although weekly supervision was conducted with study therapists, intervention fidelity was not directly addressed in the form of taping or live observation. Although depression and alcohol consumption/problems are two important outcomes to consider when targeting the transition to college, with the exception of the AUDIT cutoff, effect sizes were modest, and there are several other outcome measures that will be beneficial to include in future work in order to obtain a more complete picture of this transition process, namely, more global measures of stress and adjustment, retention, academic success, and overall level of activity involvement. However, it is notable that several of these outcomes might require a longer follow-up period to show meaningful effects. The inclusion of longer follow-ups would also allow us to examine whether BATD outcomes persist throughout a student’s time in college. Additionally, next steps would also benefit from an examination of mechanisms, with a particular focus on specificity for the outcome of interest. That is, to better understand how increased activity engagement has its impact (e.g., through resource/value allocation and/or through affect change). It will be especially important to measure actual activities engaged in with a particular focus on the frequency, quality, and types of substance-free activities. Finally, future studies in this program of research should include rigorous methods for examining clinical significance of the outcomes observed, such as reliable change indices, to complement reporting of intervention effect sizes (cf. Lambert & Ogles, 2009).
Results indicate that the BATD-enhanced orientation program, which emphasized developing a personally meaningful lifestyle, is promising for the reduction of problem drinking for first-year university students. These results are particularly notable in that problematic alcohol use is highly prevalent among university students and linked to a number of serious negative outcomes (e.g., accidental injury, unplanned and unsafe sex, and a host of social and psychological problems; Wechsler et al., 1994, 2002, 2000). The increasingly common semester-long orientation programs are an apt means to reach college freshman and target the distress often associated with decreased environmental reward that comes with transitioning to life as a university student. The parsimony of the BATD intervention and its ability to be seamlessly integrated make it a promising adjunct to these orientation programs. Overall, this pilot study sets the stage for future work to replicate and extend these findings through more comprehensive assessments of change in behavioral activation as well as to conduct longer term follow-ups.
Acknowledgments
We gratefully acknowledge the help of Gerry B. Strumpf, Marsha N. Sargeant, Jessica M. Richards, and Frances L. Wang in conducting the study.
Footnotes
We also examined a model that included “class” as captured by three contrast coded variables. There were no significant relationships between class coded in this manner and the outcomes investigated (ps >.20).
Contributor Information
Elizabeth K. Reynolds, Center for Addictions, Personality, and Emotion Research and the Department of Psychology, University of Maryland, College Park
Laura MacPherson, Center for Addictions, Personality, and Emotion Research and the Department of Psychology, University of Maryland, College Park.
David E. Baruch, Department of Psychology, University of Wisconsin—Milwaukee
Matthew T. Tull, Department of Psychiatry and Human Behavior, University of Mississippi Medical Center
C. W. Lejuez, Center for Addictions, Personality, and Emotion Research and the Department of Psychology, University of Maryland, College Park
References
- Adams CE, Nagoshi CT. Changes over one semester in drinking game playing and alcohol use and problems in a college student sample. Substance Abuse. 1999;20:97–106. doi: 10.1080/08897079909511398. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Assocation. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro M. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary care. Geneva, Switzerland: Department of Mental Health and Substance Dependence, World Health Organization; 2006. [Google Scholar]
- Beck AT, Steer RA. Beck Depression Inventory: Manual. San Antonio, TX: The Psychiatric Corporation; 1987. [Google Scholar]
- Benton SA, Robertson JM, Tseng W, Newton FB, Benton SL. Changes in counseling center client problems across 13 years. Professional Psychology: Research and Practice. 2003;34:66–72. [Google Scholar]
- Bernier A, Larose S, Whipple N. Leaving home for college: A potentially stressful event for adolescents with preoccupied attachment patterns. Attachment & Human Development. 2005;7:171–185. doi: 10.1080/14616730500147565. [DOI] [PubMed] [Google Scholar]
- Busch AM, Uebelacker LA, Kalibatseva Z, Miller IW. Measuring homework completion in behavioral activation. Behavior Modification. 2010;34:310–329. doi: 10.1177/0145445510373384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman LC, Reed PJ. Evaluating the effectiveness of a freshman orientation course. Journal of College Student Personnel. 1987;28:178–179. [Google Scholar]
- Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Statistics in Medicine. 2000;19:3127–3131. doi: 10.1002/1097-0258(20001130)19:22<3127::aid-sim784>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Lewinsohn PM, Hops H, Andrews JA, Seeley JR, Williams JA. Cognitive-behavioral group treatment of adolescent depression: Prediction of outcome. Behavior Therapy. 1992;23:341–354. [Google Scholar]
- Conigrave KM, Hall WD, Saunders JB. The AUDIT questionnaire: Choosing a cut-off score. Addiction. 1995;90:1349–1356. doi: 10.1046/j.1360-0443.1995.901013496.x. [DOI] [PubMed] [Google Scholar]
- Correia CJ, Benson T, Carey KB. Decreased substance use following increases in alternative behaviors: A preliminary investigation. Addictive Behaviors. 2005;30:19–27. doi: 10.1016/j.addbeh.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Braun AR, Sargeant M, Reynolds ER, Hopko D, Blanco C, Lejuez CW. Effectiveness of a brief behavioral treatment for inner-city illicit drug users with elevated depressive symptoms: The Life Enhancement Treatment for Substance Use (LETS ACT!) Journal of Clinical Psychiatry. 2008;69:122–129. doi: 10.4088/jcp.v69n0116. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Another look at heavy episodic drinking and alcohol use disorders among college and noncollege youth. Journal of Studies on Alcohol. 2004;65:477–488. doi: 10.15288/jsa.2004.65.477. [DOI] [PubMed] [Google Scholar]
- Dyson R, Renk K. Freshman adaptation to university life: Depressive symptoms, stress, and coping. Journal of Clinical Psychology. 2006;62:1231–1244. doi: 10.1002/jclp.20295. [DOI] [PubMed] [Google Scholar]
- Fazio NM, Palm LJ. Attributional style, depression, and grade point averages of college students. Psychological Reports. 1998;83:159–162. doi: 10.2466/pr0.1998.83.1.159. [DOI] [PubMed] [Google Scholar]
- Fenzel LM. Multivariate analyses of predictors of heavy episodic drinking and drinking-related problems among college students. Journal of College Student Development. 2005;46:126–140. [Google Scholar]
- Ferster CB. A functional analysis of depression. American Psychologist. 1973;28:857–870. doi: 10.1037/h0035605. [DOI] [PubMed] [Google Scholar]
- Gaynor ST, Harris A. Single-participant assessment of treatment mediators: Strategy description and examples from a behavioral activation intervention for depressed adolescents. Behavior Modification. 2008;32:372–402. doi: 10.1177/0145445507309028. [DOI] [PubMed] [Google Scholar]
- Henry JD, Crawford JR. The 21-item version of the Depression Anxiety Stress Scales (DASS–21): Normative data and psychometric evaluation in a large non-clinical sample. British Journal of Clinical Psychology. 2005;44:227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Heil SH, Plebani-Lussier J. Clinical implications of reinforcement as a determinant of substance use disorders. Annual Review of Psychology. 2004;55:431–461. doi: 10.1146/annurev.psych.55.090902.142033. [DOI] [PubMed] [Google Scholar]
- Hoban M. American College Health Association National College Health Assessment spring 2006 reference group data report (abridged) Journal of American College Health. 2007;55:195–206. doi: 10.3200/JACH.55.4.195-206. [DOI] [PubMed] [Google Scholar]
- Hopko DR, Bell J, Armento MEA, Robertson SMC, Mullane C, Wolf NJ, Lejuez CW. Cognitive–behavior therapy for depressed cancer patients in a medical care setting. Behavior Therapy. 2008;39:126–136. doi: 10.1016/j.beth.2007.05.007. [DOI] [PubMed] [Google Scholar]
- Hopko DR, Lejuez CW. A cancer patient’s guide to overcoming depression and anxiety: Getting through treatment and getting back to your life. Oakland, CA: New Harbinger; 2007. [Google Scholar]
- Hopko DR, Lejuez CW, LePage J, Hopko SD, McNeil DW. A brief behavioral activation treatment for depression: A randomized trial within an inpatient psychiatric hospital. Behavior Modification. 2003;27:458–469. doi: 10.1177/0145445503255489. [DOI] [PubMed] [Google Scholar]
- Hopko DR, Lejuez CW, Ruggiero KJ, Eifert GH. Contemporary behavioral activation treatments for depression: Procedures, principles, progress. Clinical Psychology Review. 2003;23:699–717. doi: 10.1016/s0272-7358(03)00070-9. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, Prince SE. A component analysis of cognitive–behavioral treatment for depression. Journal of Consulting and Clinical Psychology. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2008. II. Bethesda, MD: National Institute on Drug Abuse; 2009. p. 306. College students and adults ages 19–50 (NIH Publication No. 09–7403) [Google Scholar]
- Kokotailo PK, Egan J, Gangnon R, Brown D, Mundt M, Fleming M. Validity of the Alcohol Use Disorders Identification Test in college students. Alcoholism: Clinical and Experimental Research. 2004;28:914–920. doi: 10.1097/01.alc.0000128239.87611.f5. [DOI] [PubMed] [Google Scholar]
- Lambert MJ, Ogles BM. Using clinical significance in psychotherapy outcome research: The need for a common procedure and validity data. Psychotherapy Research. 2009;19:493–501. doi: 10.1080/10503300902849483. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, Hopko SD. A brief behavioral activation treatment for depression: Treatment manual. Behavior Modification. 2001;25:255–286. doi: 10.1177/0145445501252005. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, LePage J, Hopko SD, McNeil DW. A brief behavioral activation treatment for depression. Cognitive and Behavioral Practice. 2001;8:164–175. [Google Scholar]
- Lewinsohn PM. A behavioral approach to depression. In: Friedman RM, Katz MM, editors. The psychology of depression: Contemporary theory and research. New York, NY: Wiley; 1974. pp. 157–185. [Google Scholar]
- Lewinsohn PM, Graf M. Pleasant activities and depression. Journal of Consulting and Clinical Psychology. 1973;41:261–268. doi: 10.1037/h0035142. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Liu S, Dixon J, Qiu G, Tian Y, McCorkle R. Using generalized estimating equations to analyze longitudinal data in nursing research. Western Journal of Nursing Research. 2009;31:948–964. doi: 10.1177/0193945909336931. [DOI] [PubMed] [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. Sydney, Australia: Psychology Foundation; 1995. [Google Scholar]
- MacPherson L, Lejuez CW, Tull MT, Matusiewicz A, Rodman S, Strong DR, Brown RB. Randomized controlled trial of behavioral activation smoking cessation treatment for smokers with elevated depressive symptoms. Journal of Consulting and Clinical Psychology. 2010;78:55–61. doi: 10.1037/a0017939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPherson L, Strong DR, Kahler CW, Abrantes AM, Ramsey S, Brown RA. Association of post smoking treatment change with future smoking and cessation efforts among adolescents with psychiatric comorbidity. Nicotine and Tobacco Research. 2007;9:1297–1307. doi: 10.1080/14622200701651734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Gorka SM, MacPherson L, Hopko DR, Blanco C, Lejuez CW, Daughters SB. Examining the effect of the Life Enhancement Treatment for Substance Use (LETS ACT) on residential substance abuse treatment retention. Addictive Behaviors. 2011;36:615–623. doi: 10.1016/j.addbeh.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmoud JSR, Hall LA, Staten R. The psychometric properties of the 21-item Depression Anxiety and Stress Scale (DASS-21) among a sample of young adults. 2010 Retrieved from http://snrs.org/publications/SOJNR articles 2/Vol10Num04Art02.pdf. [Google Scholar]
- Martell CR, Addis ME, Jacobson NS. Depression in context: Strategies for guided action. New York, NY: Norton; 2001. [Google Scholar]
- Martell CR, Dimidjian S, Herman-Dunn R. Behavioral activation for depression: A clinician’s guide. New York, NY: Guilford Press; 2010. [Google Scholar]
- McCarty CA, Weisz JR. Effects of psychotherapy for depression in children and adolescents: What we can (and can’t) learn from meta-analysis and component profiling. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46:879–886. doi: 10.1097/chi.0b013e31805467b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Correia CJ, Barnett NP. Behavioral economic approaches to reduce college student drinking. Addictive Behaviors. 2007;32:2573–2585. doi: 10.1016/j.addbeh.2007.05.015. [DOI] [PubMed] [Google Scholar]
- Norton PJ. Depression Anxiety and Stress Scales (DASS-21): Psychometric analysis across four racial groups. Anxiety, Stress & Coping. 2007;20:253–265. doi: 10.1080/10615800701309279. [DOI] [PubMed] [Google Scholar]
- O’Hare T. Comparing the AUDIT and 3 drinking indices as predictors of personal and social drinking problems in freshman first offenders. Journal of Alcohol and Drug Education. 2005;49:37–61. [Google Scholar]
- O’Hare T, Sherrer MV. Validating the Alcohol Use Disorders Identification Test with college first-offenders. Journal of Substance Abuse Treatment. 1999;17:113–119. doi: 10.1016/s0740-5472(98)00063-4. [DOI] [PubMed] [Google Scholar]
- Pascarella E, Terenzini P. How college affects students: Findings and insights from twenty years of research. San Francisco, CA: Jossey-Bass; 1991. [Google Scholar]
- Pocock SJ, Assmann SE, Enos LE, Kasten LE. Subgroup analysis, covariate adjustment and baseline comparisons in clinical trial reporting: Current practice and problems. Statistics in Medicine. 2002;21:2917–2930. doi: 10.1002/sim.1296. [DOI] [PubMed] [Google Scholar]
- Potts G, Schultz B. The freshman seminar and academic success of at-risk students. College Student Journal. 2008;42:647–658. [Google Scholar]
- Pritchard ME, Wilson G. Using emotional and social factors to predict student success. Journal of College Student Development. 2003;44:18–28. [Google Scholar]
- Quinn BP. The depression sourcebook. Los Angeles, CA: Lowell House; 1997. [Google Scholar]
- Reifman A, Watson WK. Binge drinking during the first semester of college: Continuation and desistance from high school patterns. Journal of American College Health. 2003;52:73–81. doi: 10.1080/07448480309595727. [DOI] [PubMed] [Google Scholar]
- Rock S, Coates C, Greco S. Accessing excellence at C. W. Post. Dubuque, IA: Kendal/Hunt Publishing Company; 2005. [Google Scholar]
- Rodgers LS, Tennison LR. A preliminary assessment of adjustment disorder among first-year college students. Archives of Psychiatric Nursing. 2009;23:220–230. doi: 10.1016/j.apnu.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Ruggiero KJ, Morris TL, Hopko DR, Lejuez CW. Application of behavioral activation treatment for depression to an adolescent with a history of child maltreatment. Clinical Case Studies. 2007;6:64–78. [Google Scholar]
- Saitz R, Palfai TP, Freedner N, Winter MR, MacDonald A, Lu J, DeJong W. Screening and brief intervention online for college students: The iHealth study. Alcohol and Alcoholism. 2007;42:28–36. doi: 10.1093/alcalc/agl092. [DOI] [PubMed] [Google Scholar]
- Sarason IG, Sarason BR. Abnormal psychology: The problem of maladaptive behavior. 9th ed. Upper Saddle River, NJ: Prentice Hall; 1999. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption. II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Soucy N, Larose S. Attachment and control in family and mentoring contexts as determinants of adolescent adjustment to college. Journal of Family Psychology. 2000;14:125–143. doi: 10.1037//0893-3200.14.1.125. [DOI] [PubMed] [Google Scholar]
- Stice E, Burton E, Bearman SK, Rohde P. Randomized trial of a brief depression prevention program: An elusive search for a psychosocial placebo control condition. Behavior Research and Therapy. 2007;45:863–876. doi: 10.1016/j.brat.2006.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thombs DL. An introduction to addictive behaviors. 2nd ed. New York, NY: Guilford Press; 1999. [Google Scholar]
- Tobolowsky BF. 2006 National survey of first-year seminars: Continuing innovations in the collegiate curriculum. Columbia: University of South Carolina, National Resource Center for The First-Year Experience & Students in Transition; 2008. (First-year experience monograph series No. 51) [Google Scholar]
- Voelker R. Mounting student depression taxing campus mental health services. Journal of the American Medical Association. 2003;289:2055–2056. doi: 10.1001/jama.289.16.2055. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Davenport A, Dowdall GW, Moeykens B, Castillo S. Health and behavioral consequences of binge drinking in college: A national survey of students at 140 campuses. Journal of the American Medical Association. 1994;272:1672–1677. [PubMed] [Google Scholar]
- Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study Surveys: 1933–2001. Journal of American College Health. 2002;50:203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Lee J, Kuo M, Lee H. College binge drinking in the 1990s: A continuing problem: Results of the Harvard School of Public Health 1999 College Alcohol Study. Journal of American College Health. 2000;48:199–210. doi: 10.1080/07448480009599305. [DOI] [PubMed] [Google Scholar]
- Weitzman ER, Kawachi I. Giving means receiving: The protective effect of social capital on binge drinking on college campuses. American Journal of Public Health. 2000;90:1936–1939. doi: 10.2105/ajph.90.12.1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. The analysis of discrete and continuous longitudinal data. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]