Abstract
Background
Cross-sectional studies show that human immunodeficiency virus (HIV) stigma is negatively correlated with social support.
Purpose
The purpose of this study is to examine the bidirectional relationship between social support and HIV stigma.
Methods
We collected quarterly data from a cohort of 422 people living with HIV in Uganda, followed for a median of 2.1 years. We used multilevel regression to model the contemporaneous and 3-month-lagged associations between social support and both enacted and internalized stigma.
Results
Lagged enacted stigma was negatively correlated with emotional and instrumental social support, and lagged instrumental social support was negatively correlated with enacted stigma. Internalized stigma and emotional social support had reciprocal lagged associations.
Conclusions
Interventions to reduce enacted stigma may strengthen social support for people living with HIV. Improved social support may in turn have a protective influence against future enacted and internalized stigma.
Keywords: HIV/AIDS, Stigma, Social support, Uganda
Introduction
Human immunodeficiency virus (HIV) stigma is a well-documented barrier to the health and well-being of people living with HIV. As described by Goffman [1], stigma is a discrediting attribute that reduces a person from a whole person to a tainted or discounted person. HIV stigma has been associated with delaying or avoidance of HIV testing [2–4], poor adherence to antiretroviral therapy (ART) [5, 6], increased risk behaviors [7], and poor engagement with care [8]. In addition, people living with HIV experience numerous mental and psychological sequelae of stigma, including stress, fear, anxiety, and depression [9–12].
Recent studies have shown that people living with HIV who report experiences of HIV stigma also report lower levels of perceived social support [12–15]. Social support refers to the provision of psychological and material resources by people within one's social network [16]. The finding that people living with HIV who are more vulnerable to stigma also have less access to social resources has profound public health consequences because social support has been associated with powerful health benefits for people living with HIV. These include less depression [10], positive health behaviors such as adherence to medication [6], improved coping and quality of life [17], and slower progression of disease to AIDS [18]. These benefits have been understood in the context of a larger body of literature examining social support and health. The mechanisms underlying the health benefits of social support have been attributed to its various functional components, which include informational, emotional (e.g., caring, empathy), and instrumental support (e.g., financial assistance or help with tasks) [16, 19, 20]. Starting with the 1979 study by Berkman and Syme [21] who showed that social isolation was a significant risk factor for mortality, research on social support and health has shown that social support fosters psychological well-being, enhances self-esteem and self-efficacy, reduces physiological arousal, and promotes functional and adaptive coping with stressors [20, 22–24]. These psychosocial benefits translate to improved health through decreased physiological stress responses, engagement in health-promoting behaviors, and avoidance of health-damaging behaviors [20, 22–24].
Conceptual Model
Based on evidence that stigma is a multidimensional construct, researchers have developed and utilized a conceptual model that separates the experience of stigma into interpersonal and intrapersonal experiences. The interpersonal experience of stigma is called enacted stigma and is defined as discriminatory behaviors directed towards people with the stigmatized condition [25]. The intrapersonal experience of stigma is called internalized stigma and is the endorsement and internalization of negative evaluations held by others [26–28]. Models of stigma describe how people internalize stigma when they perceive the negative stereotypes to be legitimate, and suffer negative cognitive, emotional and behavioral consequences, such as ambivalence about identity, low-self esteem, and low self-efficacy [26, 27, 29, 30]. While the terminology may vary, these concepts of enacted and internalized stigma are used widely in other health conditions, such as obesity [31] and mental health [32], to understand the differential effects of these two dimensions of stigma on health behaviors and outcomes.
Historically, models of stigma have predominantly focused on individuals—the stigmatized person and the stigmatizing person—and their cognitive, affective, and behavioral processes, but recent sociological and anthropological work have proposed to embed stigma in the social space [33]. These works demonstrate that stigma is a social experience in which the effects of stigma extend to the affected individual's social ties, and in which those social ties in turn shape the experience of the stigmatized individual. Qualitative studies have demonstrated that family members of people living with HIV become reluctant to disclose to others the serostatus of the affected family member for fear of discrimination and loss of social standing in their community [9, 34]. Furthermore, close social ties can often be the source of stigmatizing attitudes and actions. People living with HIV experience avoidance, ostracism, and verbal insults from their friends and family [9], and some studies theorize that the enactment of stigma is in response to the devalued status they acquire through association with the stigmatized person [34]. While HIV stigma strains existing close relationships, it can also profoundly limit the ability of people living with HIV to seek new relationships. One proposed mechanism is the lack of disclosure. Disclosure is essential for people to receive social support; yet, fear of discrimination prevents people living with HIV from disclosing their status [35, 36], and the higher their level of internalized stigma, the more likely they are to avoid disclosure and interactions with others [11, 37]. Finally, HIV stigma has been correlated with depression [10, 12], which may further limit the capacity of people living with HIV to form and maintain social relationships. These mechanisms take on particular significance in Uganda, where HIV stigma is a prominent concern among people living with HIV with profound implications for their social experience. In one study conducted in Uganda, fear of HIV serostatus disclosure was the most common concern voiced by people living with HIV and was noted by more participants than concerns about lack of food [38], which is notable in light of the high prevalence of food insecurity among people living with HIV [39, 40].
Recent findings linking social support and HIV stigma, though suggestive, have been based on cross-sectional data [12–14] or data from two time points [15], limiting our ability to illuminate the dynamic relationship between social support and HIV stigma. Furthermore, these studies have not examined how the interpersonal and intrapersonal dimensions of HIV stigma could differentially affect the social experience of people living with HIV. To address these gaps in our current understanding of HIV stigma and social support, we examined the dynamic relationship between two dimensions of social support and two dimensions of HIV stigma using longitudinal data collected from people living with HIV receiving ART at a public hospital in rural southwestern Uganda. The primary aim of our analysis was to use time-lagged models to understand how the interpersonal and intrapersonal experiences of HIV stigma shape the social support networks of people living with HIV in rural Uganda, and to understand how these relationships in turn shape their experience of HIV stigma.
Methods
Setting and Participants
We used data from an ongoing, prospective cohort of people living with HIV initiating ART in rural Uganda. Eligibility criteria included having no prior history of treatment with ART, being over 18 years of age, and living within 20 km of the Immune Suppression Syndrome (ISS) Clinic at the Mbarara Regional Referral Hospital. The ISS Clinic is located in Mbarara District, 275 km southwest of Kampala, and provides free ART for people living with HIV in southwestern Uganda, Rwanda, and the Democratic Republic of Congo [41]. Most participants live in outlying villages surrounding the town of Mbarara, spending an hour on average to travel to the clinic by paid motorbike and on foot [42]; live in multigenerational households with other relatives living close by; engage in subsistence agriculture; and frequently interact with other members of the community through religious services, agricultural work, and community gatherings. The predominant ethnic group is Ankole, and the local language is Runyankole.
Our analyses are based on data from participants who were enrolled into the cohort from 2007 through 2010. Survey questions were translated into Runyankole, back-translated into English, further modified through focus groups with key informants, and pilot-tested to ensure clarity and relevance. Trained research assistants who spoke Runyankole interviewed participants every 3 months in a private room at a research office near the ISS Clinic. Each survey took approximately 1 h to complete. Informed consent was obtained from all study participants. Ethics approval for all study procedures was obtained by the Committee on Human Research, University of California at San Francisco; the Partners Human Research Committee at Massachusetts General Hospital; and the Institutional Ethical Review Committee, Mbarara University of Science and Technology. Consistent with national guidelines, we received clearance for the study from the Uganda National Council for Science and Technology and from the Research Secretariat in the Office of the President.
Measures
The four variables of interest were emotional social support, instrumental social support, internalized stigma, and enacted stigma. We measured social support using the Social Support Scale [43], which contains six items on emotional support and four items on instrumental social support. This scale was adapted from the Duke/University of North Carolina Functional Social Support Questionnaire, which was designed to measure multiple dimensions of social support among patients in a primary care setting [44]. Higher scores reflect higher levels of social support.
We measured internalized HIV stigma using the Internalized AIDS-Related Stigma Scale, which contains six items corresponding to the guilt, shame, and worthlessness described in Goffman's conceptualization of stigma [45, 46]. The internalized stigma scale has demonstrated good internal reliability, a coherent internal structure, and good construct validity among people living with HIV in rural Uganda [47]. To measure enacted stigma, we asked participants about whether they had experienced ten different discriminatory events in the past 3 months as a result of their HIV status, such as abandonment, housing, property loss, or physical violence (see Electronic Supplementary Material). These questions were adapted from a previous publication by Nyblade et al. [48]. We created an enacted stigma index by constructing a total count of the different types of discriminatory events experienced, with higher index scores indicating greater intensity of enacted stigma. Of note, we did not have any a priori expectation that the variables would be internally consistent because these different events are diverse in both severity as well as potential drivers. Nonetheless, for the sake of comparison with our other variables of interest, we calculated the reliability of the index at baseline.
Statistical Analysis
In our regression models, we adjusted for baseline and quarterly health status using the Medical Outcome Study-HIV (MOS-HIV) Physical Health Summary (PHS) [49, 50] and CD4+ T-lymphocyte cell count. A higher PHS score reflects a better health status. Because prior studies have shown that both HIV stigma and low social support are associated with depression [10, 12], we also adjusted for depression symptom severity. We measured depression symptom severity using a version of the 15-item Hopkins Symptom Checklist for Depression [51] that was adapted to the local context with the addition of a 16th item, “feeling like I don't care about my health” [10, 52]. We restricted our calculation of the score to the 12 affective items in light of prior research suggesting that the somatic items overlap with symptoms of HIV infection and may inflate the prevalence of depression among people living with HIV [53, 54]. Participants were classified as having probable depression based on the conventional threshold score of 1.75 [55].
We adjusted for a range of other baseline (time-invariant) demographic and socioeconomic covariates with potential for influencing the relationships among stigma, social support, and health. We measured household wealth using a household asset index [56], which was entered into the models as a continuous variable, with higher values of the asset index indicating greater household wealth relative to other households in the sample. We also adjusted for baseline age, sex, educational attainment, and marital status. Time on treatment was measured in years since starting ART.
Data analysis was conducted using SAS statistical software (version 9.2, SAS Institute Inc., Cary, NC, USA). We employed multilevel modeling to address the lack of independence among residuals in the hierarchically structured data. Since our data consisted of measures that are nested within individuals, measures from the same individual may share common, unobserved characteristics that may affect the outcomes of interest. Our modeling technique allowed us to separate the composite residual into two parts: a measure-level residual unique to the particular time at which the survey was conducted, and an individual-level residual unique to a particular individual (but not to a particular time). We used multilevel models for change, in which the models are specified by simultaneously postulating a pair of subsidiary models: a level-1 submodel that describes how each individual changes over time, and a level-2 submodel that describes how these changes differ across individuals [57]. Our level-1 submodel stipulated that the trajectories of stigma and social support are linear with time.
To examine the effects of each of the two social support dimensions on each of the two stigma dimensions and, reciprocally, the effects of each of the stigma dimensions on each of the social support dimensions, we specified eight contemporaneous regression models. First, in two regression models, internalized stigma was specified as the outcome, with instrumental and emotional social support alternately included as the main predictors (while adjusting for covariates). Second, enacted stigma was specified as the outcome, with instrumental and emotional social support alternately included as the main predictors. Third, emotional social support was specified as the outcome in two regression models, with internalized and enacted stigma alternately included as the main predictors. Finally, instrumental social support was specified as the outcome, with internalized and enacted stigma alternately included as the main predictors. We also fitted lagged-covariate models, in which each of the predictors of interest were lagged by 3 months, adjusting for covariates and the lagged outcome variable. In total, we fitted 16 regression models: 8 models in which the explanatory variables of interest were measured contemporaneously with the outcomes and 8 models in which the explanatory variables were measured with a 3-month lag.
Results
Table 1 presents the baseline demographic characteristics of the 422 participants. The average age of participants at baseline was 35 years, and they were enrolled in the study for a mean of 2.3 years (median of 2.1 years). The majority of participants [298 (71 %)] were female. Approximately half were married and half were widowed or divorced. Most [357 (85 %)] had completed primary school or more. The mean internalized stigma score at baseline was 1.3 points (median, 1.0; SD, 1.5) with a range of 0–6, the mean enacted stigma score was 0.4 points (median, 0; SD, 0.8) with a range of 0–7, the mean emotional social support score was 3.8 points (median, 4; SD, 0.4), and the mean instrumental social support score was 3.6 (median, 4; SD, 0.6). The mean CD4 count at baseline was 230 cells/mL (median, 204; SD, 149). Sixteen percent of participants screened positive for probable depression at baseline.
Table 1.
Participant baseline characteristics (N =422)
| Characteristic | N (%) or mean (median) |
|---|---|
| Gender | |
| Female | 298 (71 %) |
| Male | 124 (29 %) |
| Age (years) | 35 (34) |
| Time in study (years) | 2.3 (2.1) |
| Marital status | |
| Not married | 238 (56 %) |
| Married | 184 (44 %) |
| Education | |
| None | 65 (15 %) |
| Primary or more | 357 (85 %) |
| Internalized stigma | 1.3 (1) |
| Enacted stigma | 0.4 (0) |
| Emotional social support | 3.8 (4) |
| Instrumental social support | 3.6 (4) |
| CD4 count (cells/mL) | 230 (204) |
| MOS-HIV Physical Health Summary | 46 (49) |
| Probable depression | 67 (16 %) |
Throughout the study period, the most frequently endorsed item on the internalized stigma scale was “difficult to tell other people about my HIV status,” (852 responses, 29 % of all responses), followed by “I hide my HIV status from others,” [832 (28 %)]. Similarly, the most frequently endorsed form of enacted stigma was “being gossiped about,” [768 (25 %)] followed by “being teased or insulted” [201 (7 %)].
At baseline, the Cronbach's alpha of the internalized stigma scale was 0.73. Both social support subscales showed good internal reliability at baseline (instrumental social support Cronbach's alpha=0.87, emotional social support Cronbach's alpha=0.89), as did the social support scale as a whole (Cronbach's alpha=0.91). The Cronbach's alpha for the enacted stigma index was 0.56.
Preliminary analyses supported the use of multilevel models for change and lagged models. Briefly, empirical growth plots showed substantive changes within individuals over time in enacted stigma, internalized stigma, emotional social support, and instrumental social support. Furthermore, intraclass correlation coefficients indicated large variability within individuals over time. The intraclass correlation for emotional social support was 0.53, indicating that an estimated 53 % of the total variation in social support was attributable to differences between individuals while 47 % was attributable to variability over time within individuals. Overall, over the entire study period, 198 (47 %) participants had a negative slope over time for internalized stigma (i.e., indicating that internalized stigma decreased over time) while 69 (16 %) had a slope of zero and 155 (37 %) had a positive slope. Averaged across all participants, internalized stigma decreased at a rate of 0.13 points per year. Similarly, the intraclass correlations for enacted stigma, emotional social support, and instrumental social support were 0.74, 0.83, and 0.72, respectively.
Internalized Stigma
In the contemporaneous models specifying internalized stigma as the outcome, we found no relationship between internalized stigma and either emotional or instrumental social support (Table 2). In the lagged-covariate models, we found an inverse relationship between internalized stigma and lagged emotional social support. A 1-point increase in emotional social support was associated with a 0.13-point decrease in subsequent internalized stigma (95 % CI, −0.25 to −0.005), a 10 % relative difference compared to the baseline value. There was no statistically significant association between internalized stigma and lagged instrumental social support. In all four models, higher levels of self-reported physical health and lower levels of depression were correlated with lower levels of internalized stigma.
Table 2.
The contemporaneous and lagged effects of emotional social support and instrumental social support on internalized stigma
| Effect of emotional social support on internalized stigma
|
Effect of instrumental social support on internalized stigma
|
|||
|---|---|---|---|---|
| Contemporaneous | Lagged | Contemporaneous | Lagged | |
| Variables | b (95 % confidence interval [CI]) | b (95 % CI) | b (95 % CI) | b (95 % CI) |
| Intercept | 1.02 (0.41, 1.62)** | 1.08 (0.49, 1.67)*** | 0.95 (0.46, 1.44)*** | 0.57 (0.12, 1.03)* |
| Emotional social support | −0.082 (−0.20, 0.04) | – | – | – |
| Instrumental social support | – | – | −0.070 (−0.15, 0.01) | – |
| Lagged emotional social support | – | −0.13 (−0.25, −0.005)* | – | – |
| Lagged instrumental social support | – | – | – | 0.0083 (−0.067, 0.084) |
| Lagged internalized stigma | – | 0.11 (0.077, 0.15)*** | – | 0.113 (0.078, 0.15)*** |
| Time | −0.08 (−0.12, 0) | −0.058 (−0.13, 0.014) | −0.088 (−0.17, −0.007)* | −0.063 (−0.14, 0.009) |
| Gender | ||||
| Male | Ref | Ref | Ref | Ref |
| Female | 0.11 (−0.13, 0.35) | 0.08 (−0.14, 0.30) | 0.10 (−0.14, 0.35) | 0.087 (−0.14, 0.31) |
| Age | −0.013 (−0.026, 0) | −0.012 (−0.023, 0) | −0.013 (−0.026, 0.001) | −0.012 (−0.024, 0.00) |
| Marital status | ||||
| Not married | Ref | Ref | Ref | Ref |
| Married | 0.032 (−0.13, 0.19) | 0.005 (−0.15, 0.16) | 0.030 (−0.13, 0.19) | 0.0054 (−0.15, 0.16) |
| Education | ||||
| No school | Ref | Ref | Ref | Ref |
| Primary school or more | 0.057 (−0.23, 0.35) | 0.11 (−0.16, 0.37) | 0.063 (−0.23, 0.35) | 0.10 (−0.16, 0.36) |
| Household asset wealth | 0.075 (0, 0.15) | 0.065 (−0.004, 0.13) | 0.079 (0.003, 0.15)* | 0.062 (−0.01, 0.13) |
| MOS-HIV Physical Health Summary | −0.019 (−0.02, −0.01)*** | −0.018 (−0.024, −0.012) *** | −0.019 (−0.025, −0.013)*** | −0.018 (−0.024, −0.012)*** |
| CD4 count (per 100 cells/mL) | 0.009 (−0.03, 0.45) | 0.004 (−0.033, 0.040) | 0.007 (−0.030, 0.044) | 0.005 (−0.031, 0.042) |
| Probable depression | 0.46 (0.26, 0.67) *** | 0.049 (0.28, 0.71)*** | 0.46 (0.26, 0.67)*** | 0.49 (0.28, 0.70)*** |
P <0.05;
P <0.01;
P <0.001
Enacted Stigma
In the contemporaneous models with enacted stigma as the outcome, we found that individuals with higher levels of emotional social support or instrumental social support reported lower levels of enacted stigma (Table 3). A 1-point increase in emotional social support was correlated with a 0.30-point decrease in enacted stigma (95 % CI, −0.37 to −0.24), and a 1-point increase in instrumental social support was correlated with a 0.16-point decrease in enacted stigma (95 % CI, −0.21 to −0.12). In the lagged-covariate models, we found that lagged instrumental social support was negatively correlated with subsequent enacted stigma (b =−0.07, 95 % CI −0.11, −0.03), but we found no statistically significant relationship between lagged emotional social support and subsequent enacted stigma. A 1-point increase in lagged instrumental social support was correlated with a 0.07-point decrease in subsequent enacted stigma. In all four models, higher levels of education, wealth, and physical health status were consistently associated with lower levels of enacted stigma.
Table 3.
The contemporaneous and lagged effects of emotional social support and instrumental social support on enacted stigma
| Effect of emotional social support on enacted stigma
|
Effect of instrumental social support on enacted stigma
|
|||
|---|---|---|---|---|
| Contemporaneous | Lagged | Contemporaneous | Lagged | |
| Variables | b (95 % confidence interval [CI]) | b (95 % CI) | b (95 % CI) | b (95 % CI) |
| Intercept | 1.74 (1.43, 2.05)*** | 0.72 (0.41, 1.04)*** | 1.16 (0.94, 1.39)*** | 0.79 (0.57, 1.00)*** |
| Emotional social support | −0.30 (−0.37, −0.24)*** | – | – | – |
| Instrumental social support | – | – | −0.16 (−0.21, −0.12)*** | – |
| Lagged emotional social support | – | −0.045 (−0.12, 0.03) | – | – |
| Lagged instrumental social support | – | – | – | −0.070 (−0.11, −0.03)** |
| Lagged enacted stigma | – | 0.046 (0.009, 0.083)* | – | 0.044 (0.007, 0.081)* |
| Time | 0.004 (−0.04, 0.04) | 0.006 (−0.033, 0.045) | −0.0009 (−0.049, 0.032) | 0.006 (−0.033, 0.044) |
| Gender | ||||
| Male | Ref | Ref | Ref | Ref |
| Female | 0.096 (0.003, 0.189)* | 0.099 (0.006, 0.19)* | 0.077 (−0.017, 0.17) | 0.091 (−0.002, 0.18) |
| Age | 0.001 (−0.004, 0.006) | 0.001 (−0.004, 0.006) | 0.002 (−0.004, 0.007) | 0.001 (−0.004, 0.006) |
| Marital status | ||||
| Not married | Ref | Ref | Ref | Ref |
| Married | −0.031 (−0.11, 0.043) | −0.037 (−0.11, 0.038) | −0.034 (−0.11, 0.04) | −0.038 (−0.11, 0.037) |
| Education | ||||
| No school | Ref | Ref | Ref | Ref |
| Primary school or more | −0.15 (−0.26, −0.04)** | −0.014 (−0.25, −0.03)* | −0.14 (−0.25, −0.03)* | −0.13 (−0.24, −0.02)* |
| Household asset wealth | −0.045 (−0.074, −0.016)** | −0.049 (−0.078, −0.020)*** | −0.039 (−0.068,−0.01)** | −0.046 (−0.074, −0.017)** |
| MOS-HIV Physical Health Summary | −0.009 (−0.012, −0.005)*** | −0.010 (−0.013, −0.006)*** | −0.009 (−0.012, −0.005)*** | −0.009 (−0.013, −0.006)*** |
| CD4 count (per 100 cells/mL) | 0.004 (−0.015, 0.022) | 0.006 (−0.013, 0.025) | 0.0003 (−0.019, 0.019) | 0.006 (−0.013, 0.025) |
| Probable depression | 0.075 (−0.041, 0.19) | 0.086 (−0.031, 0.020) | 0.083 (−0.033, 0.20) | 0.085 (−0.032, 0.20) |
P <0.05;
P <0.01;
P <0.001
Emotional Social Support
In the contemporaneous models with emotional social support as the outcome, we found that individuals with higher levels of internalized stigma or enacted stigma reported lower levels of emotional social support (Table 4). Each 1-point increase in the internalized stigma scale was associated with a 0.014-point decrease in the emotional social support scale (95 % CI, −0.024 to −0.003). Each one-point increase in enacted stigma was correlated with a 0.095-point decrease in emotional social support (95 % CI, −0.11 to −0.075). In the lagged-covariate models, lagged internalized stigma was negatively correlated with subsequent emotional social support (b =−0.016; 95 % CI, −0.026 to −0.005), and lagged enacted stigma was negatively correlated with subsequent emotional support (b =−0.032; 95 % CI, −0.062 to −0.01). In all four models, higher levels of wealth and physical health status were correlated with higher levels of emotional social support.
Table 4.
The contemporaneous and lagged effects internalized stigma and enacted stigma on emotional social support
| Effect of internalized stigma on emotional social support
|
Effect of enacted stigma on emotional social support
|
|||
|---|---|---|---|---|
| Contemporaneous | Lagged | Contemporaneous | Lagged | |
| Variables | b (95 % confidence interval [CI]) | b (95 % CI) | b (95 % CI) | b (95 % CI) |
| Intercept | 3.81 (3.73, 3.89)*** | 3.69 (3.52, 3.85)*** | 3.85 (3.78, 3.93)*** | 3.70 (3.44, 3.96)*** |
| Internalized stigma | −0.014 (−0.024, −0.003)* | – | – | – |
| Enacted stigma | – | – | −0.095 (−0.114, −0.075)*** | – |
| Lagged internalized stigma | – | −0.016 (−0.026, −0.005)** | – | – |
| Lagged emotional social support | – | 0.035 (−0.003, 0.074) | – | 0.019 (−0.04, 0.077) |
| Lagged enacted stigma | – | – | – | −0.032 (−0.062, −0.001)* |
| Time | −0.011 (−0.032, 0.010) | −0.013 (−0.034, 0.008) | −0.008 (−0.028, 0.012) | −0.003 (−0.051, 0.046) |
| Gender | ||||
| Male | Ref | Ref | Ref | Ref |
| Female | −0.034 (−0.079, 0.012) | −0.032 (−0.077, 0.013) | −0.025 (−0.068, 0.017) | −0.052, (−0.12, 0.020) |
| Age | −0.0002 (−0.003, 0.002) | 0.0001 (−0.002, 0.003) | 0.0001 (−0.002, 0.002) | 0.0003 (−0.003, 0.004) |
| Marital status | ||||
| Not married | Ref | Ref | Ref | Ref |
| Married | −0.004 (−0.042, 0.033) | −0.007 (−0.044, 0.031) | −0.009 (−0.044, 0.027) | −0.039 (−0.101, 0.023) |
| Education | ||||
| No school | Ref | Ref | Ref | Ref |
| Primary school or more | 0.021 (−0.033, 0.074) | 0.010 (−0.043, 0.063) | 0.002 (−0.048, 0.053) | 0.034 (−0.048, 0.116) |
| Household asset wealth | 0.025 (0.011, 0.039) *** | 0.025 (0.011, 0.039)*** | 0.020 (0.007, 0.033)** | 0.002 (0.000, 0.045)* |
| MOS-HIV Physical Health Summary | 0.002 (0.001, 0.004)** | 0.003 (0.001, 0.004)** | 0.002 (0.00, 0.004)* | 0.003 (0.0004, 0.006)* |
| CD4 (per 100 cells/mL) | −0.009 (−0.019, 0.001) | −0.009 (−0.019, 0.014) | −0.008 (−0.017, 0.002) | −0.002 (−0.018, 0.014) |
| Depression | −0.048 (−0.111, 0.016) | −0.067 (−0.13, 0.002)* | −0.047 (−0.11, 0.015) | −0.067 (−0.17, 0.03) |
P <0.05;
P <0.01;
P <0.001
Instrumental Social Support
In the contemporaneous models with instrumental social support as outcome, we found that individuals who reported higher levels of enacted stigma reported lower levels of instrumental social support, but we found no statistically significant relationship between internalized stigma and instrumental social support (Table 5). A 1-point increase in enacted stigma was associated with a 0.11-point decrease in instrumental social support (95 % CI, −0.14 to −0.08). In the lagged-covariate models, lagged enacted stigma was negatively correlated with subsequent instrumental social support (b =−0.032; 95 % CI, −0.062 to −0.001), but lagged internalized stigma did not have a statistically significant relationship with subsequent instrumental social support. In all four models, higher levels of education, wealth, and physical health status were correlated with higher levels of instrumental social support, while higher CD4 counts were associated with lower levels of instrumental social support.
Table 5.
The contemporaneous and lagged effects of internalized stigma and enacted stigma on instrumental social support
| Effect of internalized stigma on instrumental social support
|
Effect of enacted stigma on instrumental social support
|
|||
|---|---|---|---|---|
| Contemporaneous | Lagged | Contemporaneous | Lagged | |
| Variables | b (95 % confidence interval [CI]) | b (95 % CI) | b (95 % CI) | b (95 % CI) |
| Intercept | 3.53 (3.38, 3.67)*** | 3.25 (3.06, 3.43)*** | 3.58 (3.43, 3.72)*** | 3.25 (3.07, 3.44)*** |
| Internalized stigma | −0.017 (−0.034, 0.000) | – | – | – |
| Enacted stigma | – | – | −0.11 (−0.14, −0.08)*** | – |
| Lagged internalized stigma | – | −0.013 (−0.029, 0.004) | – | – |
| Lagged enacted stigma | – | – | – | −0.032 (−0.062, −0.001)* |
| Lagged instrumental social support | – | 0.083 (0.046, 0.119)*** | – | 0.084 (0.047, 0.120)*** |
| Time | −0.12 (−0.15, −0.08)*** | −0.11 (−0.15, −0.08)*** | −0.11 (−0.15, −0.07)*** | −0.11 (−0.15, −0.077)*** |
| Gender | ||||
| Male | Ref | Ref | Ref | Ref |
| Female | −0.16 (−0.25, −0.076)*** | −0.15 (−0.24, −0.07)*** | −0.15 (−0.24, −0.07)*** | −0.15 (−0.23, −0.07)*** |
| Age | 0.001 (−0.004, 0.005) | 0.0004 (−0.0004, 0.0047) | 0.001 (−0.004, 0.005) | 0.0006 (−0.004, 0.005) |
| Marital status | ||||
| Not married | Ref | Ref | Ref | Ref |
| Married | −0.028 (−0.094, 0.039) | −0.032 (−0.096, 0.033) | −0.03 (−0.096, −0.034) | −0.026 (−0.090, 0.038) |
| Education | ||||
| No school | Ref | Ref | Ref | Ref |
| Primary school or more | 0.12 (0.02, 0.22)* | 0.10 (0.008, 0.20)* | 0.10 (0.004, 0.20)* | 0.098 (0.0044, 0.19)* |
| Household asset wealth | 0.082 (0.056, 0.11)*** | 0.079 (0.053, 0.010)*** | 0.075 (0.049, 0.10)*** | 0.077 (0.052, 0.101)*** |
| MOS-HIV Physical Health Summary | 0.004 (0.001, 0.007)** | 0.004 (0.002, 0.007)** | 0.003 (0.001, 0.006)* | 0.004 (0.001, 0.007)** |
| CD4 (per 100 cells/mL) | −0.032 (−0.048, −0.015)*** | −0.030 (−0.046, −0.014)*** | −0.032 (−0.048, −0.016)*** | −0.032 (−0.048, −0.016)*** |
| Probable depression | −0.024 (−0.12, 0.074) | −0.053 (−0.15, 0.047) | −0.026 (−0.12, 0.071) | −0.040 (−0.14, 0.058) |
P <0.05;
P <0.01;
P <0.001
We further examined this apparently paradoxical relationship between instrumental social support and CD4 count. We estimated the effect of the two dimensions of stigma and two dimensions of social support on CD4 count using four multilevel modeling controlling for covariates, and found no statistically significant relationship between internalized stigma, enacted stigma, or emotional social support with CD4 count (data not shown). However, we found that individuals who reported higher levels of instrumental social support had lower CD4 counts and that a 1-point increase in instrumental social support was correlated with a 14.7 decrease in CD4 count (95 % CI, −22.6 to −6.9). We conducted exploratory subgroup analyses to further explore this finding and estimated the effects of interactions between sociodemographic variables and instrumental social support. We found that the joint interaction between gender and instrumental social support did not have a statistically significant relationship with CD4 count, but that the joint interaction of education and instrumental social support (b =−21.7; 95 % CI, −42.3 to −1.1) as well as the joint interaction of marital status and instrumental social support (b =−18.6; 95 % CI, −34.2 to −3.0) were statistically significant predictors of CD4 count. We also estimated separate multilevel models with CD4 count as the outcome and instrumental social support as the main predictor for men and women, married and unmarried participants, and participants with and without education. We found that instrumental social support was a statistically significant predictor of CD4 count for men (b =−22.0; 95 % CI, −38.4 to −5.6), women (b = −12.0; 95 % CI, −21.0 to −3.1), married participants (b = −26.0; 95 % CI, −38.2 to −13.8), and educated participants (b =−0.19; 95 % CI, −27.1 to −10.0), but not among unmarried participants or participants without a formal education.
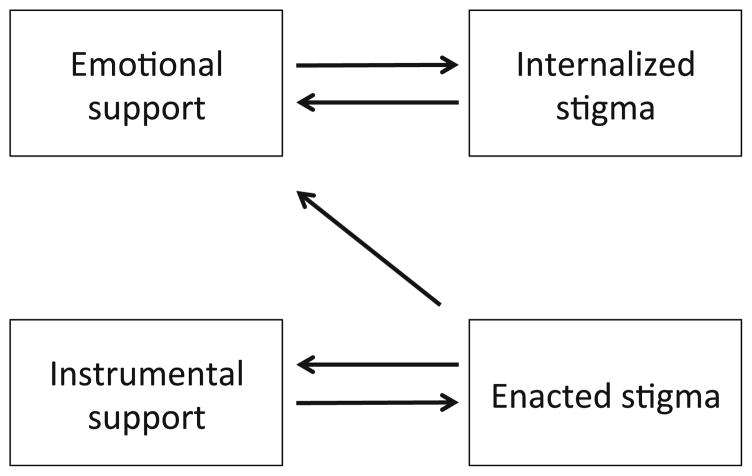
Figure 1 summarizes the lagged relationships between the two dimensions of stigma and two dimensions of social support. In summary, low levels of instrumental social support are associated with high subsequent levels of enacted stigma, which in turn are associated with lower subsequent instrumental social support. High levels of enacted stigma are associated with low subsequent levels of emotional support. Low levels of emotional social support are associated with high subsequent levels of internalized stigma, which in turn are associated with even lower subsequent levels of emotional support.
Fig. 1.
This figure represents the relationships between emotional support, instrumental support, enacted stigma, and internalized stigma. The arrows indicate statistically significant lagged, inverse associations, where the arrow points toward the construct that follows in temporal sequence
Discussion
In this longitudinal analysis of data from people living with HIV initiating ART in rural Uganda, we found evidence that enacted stigma may compromise the ability to access both emotional and instrumental support from friends and family. We also found that internalized stigma may compromise the ability to access emotional support. At the same time, we found that instrumental social support was protective against future experiences of enacted stigma but not against internalized stigma. Finally, emotional social support was protective against future internalization of stigma, but not future experiences of enacted stigma. The estimated associations were strong, large in magnitude, and robust to lagged specifications that ensured a temporal ordering between the exposures and outcomes.
One of our primary findings was that the relationship between enacted stigma and social support was bidirectional. Lagged enacted stigma had an inverse association with both emotional and instrumental social support, indicating that people living with HIV who experienced discrimination lost social support. Lagged instrumental social support had an inverse association with subsequent enacted stigma, indicating that people living with HIV who had less access to instrumental social support experienced more subsequent discrimination. These findings suggest that enacted stigma may trigger a vicious cycle, in which friends and family of people living with HIV abandon the HIV-affected person, and themselves become perpetrators of discrimination toward people living with HIV. One explanation may be that friends and family members become targets of discrimination by association. Goffman [1] describes this stigma by association, called courtesy stigma, as the process in which people who are “related through the social structure to a stigmatized individual…are all obliged to share some of the discredit of the stigmatized person” (p. 30). Goffman [1] further added that courtesy stigma “provides a reason why such relations tend either to be avoided or to be terminated” (p. 30). Bogart and colleagues [9] similarly reported that people living with HIVexperience avoidance and ostracism by family members and friends, as well as overt acts of discrimination or hurtful remarks from those who remained in contact. Yang and colleagues [34], using the example of mental illness in Hong Kong, proposed that stigma threatens the moral standing of the family and friends, and the family members' fear of social contamination and loss of face motivated them to abandon and discriminate against their ill family member.
A second primary finding of our study was that there was an inverse and bidirectional relationship between emotional social support and internalized stigma. The inverse association between emotional support and reduced subsequent internalized stigma is consistent with previously published findings from cross-sectional studies [12, 13, 15, 32]. The social cognitive behavioral model of internalized stigma holds that stigmatized people are more likely to endorse demeaning beliefs when they blame themselves (instead of broader social processes) for negative evaluations or when they do not have positive self-perceptions [26]. Having emotionally supportive family and friends may help decrease the perceived legitimacy of negative evaluations and help people living with HIV develop a more positive sense of self, leading to less internalization of stigma.
Conversely, lagged internalized stigma was inversely associated with emotional social support, indicating that people living with HIV who internalize stigma are less able to have supportive relationships with friends and family. This is consistent with reports that people with high internalized stigma are less likely to disclose their HIV status to their friends and family or to solicit support from them [12, 37]. Internalized stigma has also been associated with depression [10, 12], which could also compromise the affected persons' effectiveness in maintaining supportive relationships. Furthermore, caring for people living with HIV exerts substantive physical and psychological burdens on their caregivers, particularly in the setting of depression [58]. This could result in a negative “feedback loop” of social support [23], in which the strain of supporting a person with a serious illness results in caregivers withdrawing and severing the relationship in order to cope with the strain.
How can we understand why individuals living with HIV who report high levels of perceived instrumental social support subsequently report low levels of enacted stigma, but not internalized stigma, while those who report high levels of emotional social support subsequently report low levels of internalized stigma, but not enacted stigma? We hypothesize that having friends and family who provide tangible help with tasks and finances can protect the person from becoming targets of external, visible acts of discrimination and insults. However, such transactional relationships may not be as helpful as emotionally supportive relationships in protecting people living with HIV from endorsing negative views about themselves and losing self-esteem. While internalized stigma has been implicated in loss of self-efficacy such as that required for the disclosure of HIV serostatus to partners [27], the null association between lagged internalized stigma and instrumental social support may reflect that this loss of self-efficacy is most relevant to intimate, emotional relationships. Our results confirm the conceptual difference [11] between enacted stigma and internalized stigma by showing that internalized and enacted stigma each originate from different interpersonal processes.
These findings suggest that people living with HIV who are most affected by HIV stigma may suffer the additional burden of losing social support. The emotional and material resources provided by social support are critical for people living with HIV in resource-poor settings like Uganda, who must address day-to-day economic challenges while adhering to ART, maintaining positive health behaviors, and coping with the burden of illness and stigma. In one qualitative study of 252 individuals living with HIV in three sub-Saharan African countries, social relationships were critical for maintaining ART adherence, not only because individuals living with HIV relied on them for transport to clinic, encouragement, and regular reminders but also because of the social expectations that created obligations for people living with HIV to adhere [59].
We acknowledge several limitations of this study. First, our measures are self-reported and therefore suffer challenges generic to all analyses based on self-reported data. Second, it is difficult to disentangle the extent to which the estimated associations may simply reflect an unmeasured common factor. However, in the lagged models, we examine determinants of stigma or social support after adjusting for lagged values of the variables. Third, the perception of social support may not correlate perfectly with the actual degree of social support received. However, prior studies have demonstrated that perceived social support is more predictive of health outcomes than actual social support for people living with HIV/AIDS [60]. Fourth, our study sample consisted of individuals living with HIV who were initiating ART. Given that stigma is known to compromise the ability of people living with HIV to access and adhere to ART [6, 61], and given that access to ART has been shown to lower stigma [62–64], it is likely that overall levels of internalized stigma were lower in our sample compared to untreated individuals living with HIV. Because social support is also known to be positively associated with treatment access [59], this could have biased our estimates away from the null. Fifth, the enacted stigma index had a relatively low reliability, which was expected given the diversity of behaviors included in the index. The lack of internal consistency simply increases the amount of random noise so that regression models in which enacted stigma was specified as the dependent variable would have yielded estimates that were biased towards the null. The mean of the internalized stigma and enacted stigma scores were low, but comparable to those found in the literature [45]. Finally, the cut-off for the Hopkins Symptom Checklist used to determine probable depression is based on studies conducted in Western populations, and we acknowledge that this specific cutoff has not been validated in the Ugandan context.
Of note, we found that internalized stigma, enacted stigma, and emotional social support did not have statistically significant associations with CD4 count and that instrumental social support had an inverse association with CD4 count. This finding is paradoxical in that social support is generally thought of as being linked with better ART adherence [6] and other positive health behaviors. However, there are likely multiple pathways leading from social support to improved health, so extrapolating a direct association from the data may not be warranted. In addition, instrumental social support may not have uniformly beneficial effects on health, especially in settings where the nature of the support does not meet the recipient’s needs. For example, instrumental social support has been found to increase dependency and disability among older adults [65] or worsen glycemic control among people with diabetes mellitus [66]. Further research is indicated to clarify these associations among people living with HIV.
In summary, we found that enacted stigma may compromise the ability of people living with HIV to access support from close social ties, and that instrumental social support may be protective against future experiences of discrimination. We also found that emotional social support may be protective against future internalization of stigma. Taken together, our findings provide unique longitudinal evidence on the bidirectional relationships between stigma and social support. They also suggest the potentially powerful impacts that antistigma interventions may have on the lives of people living with HIV by interrupting the vicious feedback loop between stigma and social isolation.
Supplementary Material
Acknowledgments
We thank the Uganda AIDS Rural Treatment Outcomes study participants who made this study possible by sharing their experiences; and Anna Baylor and Nozmo Mukiibi for study coordination and support. We also thank James O'Malley for statistical advice. While these individuals are acknowledged for their assistance, no endorsement of manuscript contents or conclusions should be inferred.
Funding This study was funded by US National Institutes of Health K23MH079713, R01MH054907, and P30AI27763. The authors also acknowledge the following additional sources of salary support: the Walker Foundation, the Burke Family Foundation, T32AI007433, K23MH087228, K24MH087227, and K23MH096620.
Footnotes
Conflict of Interest The authors have no conflict of interest to disclose.
Electronic supplementary material The online version of this article (doi:10.1007/s12160-013-9576-5) contains supplementary material, which is available to authorized users.
Contributor Information
Sae Takada, Email: takada@post.harvard.edu, Harvard Medical School, Boston, MA, USA
Sheri D. Weiser, Division of HIV/AIDS and Positive Health Program, University of California at San Francisco, San Francisco, CA, USA
Elias Kumbakumba, Mbarara University of Science and Technology, Mbarara, Uganda
Conrad Muzoora, Mbarara University of Science and Technology, Mbarara, Uganda
Jeffrey N. Martin, Department of Epidemiology and Biostatistics, University of California at San Francisco, San Francisco, CA, USA
Peter W. Hunt, Division of HIV/AIDS and Positive Health Program, University of California at San Francisco, San Francisco, CA, USA
Jessica E. Haberer, Harvard Medical School, Boston, MA, USA, Center for Global Health, Massachusetts General Hospital, Boston, MA, USA
Annet Kawuma, Mbarara University of Science and Technology, Mbarara, Uganda
David R. Bangsberg, Harvard Medical School, Boston, MA, USA, Mbarara University of Science and Technology, Mbarara, Uganda, Center for Global Health, Massachusetts General Hospital, Boston, MA, USA
Alexander C. Tsai, Harvard Medical School, Boston, MA, USA, Center for Global Health, Massachusetts General Hospital, Boston, MA, USA, Chester M. Pierce MD Division of Global Psychiatry, Massachusetts General Hospital, Boston, MA, USA
References
- 1.Goffman E. Stigma; notes on the management of spoiled identity. Englewood Cliffs: Prentice-Hall; 1963. [Google Scholar]
- 2.Fortenberry JD, McFarlane M, Bleakley A, et al. Relationships of stigma and shame to gonorrhea and HIV screening. Am J Public Health. 2002;92:378–381. doi: 10.2105/ajph.92.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolfe WR, Weiser SD, Bangsberg DR, et al. Effects of HIV-related stigma among an early sample of patients receiving antiretroviral therapy in Botswana. AIDS Care. 2006;18:931–933. doi: 10.1080/09540120500333558. [DOI] [PubMed] [Google Scholar]
- 4.Pitpitan EV, Kalichman SC, Eaton LA, et al. AIDS-related stigma, HIV testing, and transmission risk among patrons of informal drinking places in Cape Town. South Africa. Ann Behav Med. 2012;43:362–371. doi: 10.1007/s12160-012-9346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rintamaki LS, Davis TC, Skripkauskas S, Bennett CL, Wolf MS. Social stigma concerns and HIV medication adherence. AIDS Pat Care STDs. 2006;20:359–368. doi: 10.1089/apc.2006.20.359. [DOI] [PubMed] [Google Scholar]
- 6.Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, Tsai AC. Impact of HIV-related stigma on HIV treatment adherence: Systematic review, meta-synthesis, and conceptual model. J Int AIDS Soc. 2013;16:18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siedner MJ, Tsai AC, Muzoora C, et al. Treatment as long-term prevention: Sustained reduction in HIV sexual transmission risk with use of antiretroviral therapy in rural Uganda. AIDS. 2013 doi: 10.1097/QAD.0000000000000136. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schuster MA, Collins R, Cunningham WE, et al. Perceived discrimination in clinical care in a nationally representative sample of HIV-infected adults receiving health care. J Gen Intern Med. 2005;20:807–813. doi: 10.1111/j.1525-1497.2005.05049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bogart LM, Cowgill BO, Kennedy D, et al. HIV-related stigma among people with HIV and their families: A qualitative analysis. AIDS Behav. 2008;12:244–254. doi: 10.1007/s10461-007-9231-x. [DOI] [PubMed] [Google Scholar]
- 10.Tsai AC, Bangsberg DR, Frongillo EA, et al. Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Soc Sci Med. 2012;74:2012–2019. doi: 10.1016/j.socscimed.2012.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steward WT, Herek GM, Ramakrishna J, et al. HIV-related stigma: Adapting a theoretical framework for use in India. Soc Sci Med. 2008;67:1225–1235. doi: 10.1016/j.socscimed.2008.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simbayi LC, Kalichman S, Strebel A, et al. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64:1823–1831. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith R, Rossetto K, Peterson BL. A meta-analysis of disclosure of one's HIV-positive status, stigma and social support. AIDS Care. 2008;20:1266–1275. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- 14.Galvan FH, Davis EM, Banks D, Bing EG. HIV stigma and social support among African Americans. AIDS Pat Care STDs. 2008;22:423–436. doi: 10.1089/apc.2007.0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mak WW, Cheung RY, Law RW, et al. Examining attribution model of self-stigma on social support and psychological well-being among people with HIV+/AIDS. Soc Sci Med. 2007;64:1549–1559. doi: 10.1016/j.socscimed.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Cohen S, McKay G. Social support, stress, and the buffering hypothesis: A theoretical analysis. In: Baum A, Singer JE, Taylor SE, editors. Handbook of Psychology and Health. Hillsdale: Erlbaum; 1984. pp. 253–267. [Google Scholar]
- 17.Friedland J, Renwick R, McColl M. Coping and social support as determinants of quality of life in HIV/AIDS. AIDS Care. 1996;8:15–32. doi: 10.1080/09540129650125966. [DOI] [PubMed] [Google Scholar]
- 18.Leserman J, Jackson ED, Petitto JM, et al. Progression to AIDS: The effects of stress, depressive symptoms, and social support. Psychosom Med. 1999;61:397–406. doi: 10.1097/00006842-199905000-00021. [DOI] [PubMed] [Google Scholar]
- 19.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 20.Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across life course. Annu Rev Sociol. 2010;36:139–157. doi: 10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berkman LF, Syme SL. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 22.Cohen S. Social relationships and health. Am Psychol. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 23.Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 24.Taylor SE, Repetti RL, Seeman T. Health psychology: What is an unhealthy environment and how does it get under the skin? Annu Rev Psychol. 1997;48:411–447. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- 25.Allport GW. The Nature of Prejudice. Reading: Addison-Wesley; 1979. [Google Scholar]
- 26.Corrigan PW, Watson AC. The paradox of self-stigma and mental illness. Clin Psychol-Sci Pr. 2002;9:35–53. [Google Scholar]
- 27.Pachankis JE. The psychological implications of concealing a stigma: A cognitive-affective-behavioral model. Psychol Bull. 2007;133:328–345. doi: 10.1037/0033-2909.133.2.328. [DOI] [PubMed] [Google Scholar]
- 28.Scheff TJ. Being mentally ill: A sociological theory. Chicago: Aldine; 1966. [Google Scholar]
- 29.Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwent BP. A modified labeling theory approach to mental disorders: An empirical assessment. Am Sociol Rev. 1989;54:400–423. [Google Scholar]
- 30.Link BG. Understanding labeling effects in the area of mental disorders: An assessment of the effects of expectations of rejection. Am Sociol Rev. 1987;52:96–112. [Google Scholar]
- 31.Carels RA, Young KM, Wott CB, et al. Internalized weight stigma and its ideological correlates among weight loss treatment seeking adults. Eat Weight Disord. 2009;14:e92–97. doi: 10.1007/BF03327805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Soc Sci Med. 2010;71:2150–2161. doi: 10.1016/j.socscimed.2010.09.030. [DOI] [PubMed] [Google Scholar]
- 33.Yang LH, Kleinman A, Link BG, et al. Culture and stigma: Adding moral experience to stigma theory. Soc Sci Med. 2007;64:1524–1535. doi: 10.1016/j.socscimed.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 34.Yang LH, Kleinman A. ‘Face’ and the embodiment of stigma in China: The cases of schizophrenia and AIDS. Soc Sci Med. 2008;67:398–408. doi: 10.1016/j.socscimed.2008.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chandra PS, Deepthivarma S, Manjula V. Disclosure of HIV infection in south India: Patterns, reasons and reactions. AIDS Care. 2003;15:207–215. doi: 10.1080/0954012031000068353. [DOI] [PubMed] [Google Scholar]
- 36.Hays RB, McKusick L, Pollack L, et al. Disclosing HIV seropositiv-ity to significant others. AIDS. 1993;7:425–431. doi: 10.1097/00002030-199303000-00019. [DOI] [PubMed] [Google Scholar]
- 37.Tsai AC, Bangsberg DR, Kegeles SM, et al. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Ann Behav Med. 2013;46:285–294. doi: 10.1007/s12160-013-9514-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mayanja BN, Ekoru K, Namugenyi H, Lubega R, Mugisha JO. Patients’ worries before starting antiretroviral therapy and their association with treatment adherence and outcomes: A prospective study in rural Uganda, 2004–2009. BMC Res Notes. 2013;6:187. doi: 10.1186/1756-0500-6-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsai AC, Bangsberg DR, Emenyonu N, et al. The social context of food insecurity among persons living with HIV/AIDS in rural Uganda. Soc Sci Med. 2011;73:1717–1724. doi: 10.1016/j.socscimed.2011.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weiser SD, Tuller DM, Frongillo EA, et al. Food insecurity as a barrier to sustained antiretroviral therapy adherence in Uganda. PLoS One. 2010;5:e10340. doi: 10.1371/journal.pone.0010340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Geng EH, Bwana MB, Kabakyenga J, et al. Diminishing availability of publicly funded slots for antiretroviral initiation among HIV-infected ART-eligible patients in Uganda. PLoS One. 2010;5:e14098. doi: 10.1371/journal.pone.0014098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Siedner MJ, Lankowski A, Tsai AC, et al. GPS-measured distance to clinic, but not self-reported transportation factors, are associated with missed HIV clinic visits in rural Uganda. AIDS. 2013;27:1503–1508. doi: 10.1097/QAD.0b013e32835fd873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Antelman G, Smith Fawzi MC, Kaaya S, et al. Predictors of HIV-1 serostatus disclosure: A prospective study among HIV-infected pregnant women in Dar es Salaam, Tanzania. AIDS. 2001;15:1865–1874. doi: 10.1097/00002030-200109280-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH. The Duke-UNC functional social support questionnaire. Measurement of social support in family medicine patients. Med Care. 1988;26:709–723. doi: 10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- 45.Kalichman SC, Simbayi LC, Cloete A, et al. Measuring AIDS stigmas in people living with HIV/AIDS: The internalized AIDS-related stigma scale. AIDS Care. 2009;21:87–93. doi: 10.1080/09540120802032627. [DOI] [PubMed] [Google Scholar]
- 46.Kalichman SC, Simbayi LC, Jooste S, et al. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav. 2005;9:135–143. doi: 10.1007/s10461-005-3895-x. [DOI] [PubMed] [Google Scholar]
- 47.Tsai AC, Weiser SD, Steward WT, et al. Evidence for the reliability and validity of the internalized AIDS-related stigma scale in rural Uganda. AIDS Behav. 2013;17:427–433. doi: 10.1007/s10461-012-0281-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nyblade L, MacQuarrie K. Can we measure HIV/AIDS-related stigma and discrimination? Current knowledge about quantifying stigma in developing countries. Washington: US Agency for International Development; 2006. [Google Scholar]
- 49.Wu AW, Revicki DA, Jacobson D, Malitz FE. Evidence for reliability, validity and usefulness of the medical outcomes study HIV health survey (MOS-HIV) Qual Life Res. 1997;6:481–493. doi: 10.1023/a:1018451930750. [DOI] [PubMed] [Google Scholar]
- 50.Wu AW, Rubin HR, Mathews WC, et al. A health status questionnaire using 30 items from the Medical Outcomes Study, Preliminary validation in persons with early HIV infection. Med Care. 1991;29:786–798. doi: 10.1097/00005650-199108000-00011. [DOI] [PubMed] [Google Scholar]
- 51.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behav Sci. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 52.Bolton P, Ndogoni L. Cross-cultural assessment of trauma-related mental illness (phase II): A report of research conducted by World Vision Uganda and The Johns Hopkins University. 2001. [Google Scholar]
- 53.Kalichman SC, Sikkema KJ, Somlai A. Assessing persons with human immunodeficiency virus (HIV) infection using the Beck Depression Inventory: Disease processes and other potential confounds. J Pers Assess. 1995;64:86–100. doi: 10.1207/s15327752jpa6401_5. [DOI] [PubMed] [Google Scholar]
- 54.Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. J Nerv Ment Dis. 2000;188:662–670. doi: 10.1097/00005053-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 55.Winokur A, Winokur DF, Rickels K, Cox DS. Symptoms of emotional distress in a family planning service: stability over a four-week period. Brit J Psych. 1984;144:395–399. doi: 10.1192/bjp.144.4.395. [DOI] [PubMed] [Google Scholar]
- 56.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: An application to educational enrollments in states of India. Demography. 2001;38:115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 57.Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford: Oxford University Press; 2003. [Google Scholar]
- 58.Prachakul W, Grant JS. Informal caregivers of persons with HIV/AIDS: A review and analysis. J Assoc Nurses AIDS Care. 2003;14:55–71. doi: 10.1177/1055329003014003005. [DOI] [PubMed] [Google Scholar]
- 59.Ware NC, Idoko J, Kaaya S, et al. Explaining adherence success in sub-Saharan Africa: An ethnographic study. PLoS Med. 2009;6:e11. doi: 10.1371/journal.pmed.1000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McDowell TL, Serovich JM. The effect of perceived and actual social support on the mental health of HIV-positive persons. AIDS Care. 2007;19:1223–1229. doi: 10.1080/09540120701402830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Weiser S, Wolfe W, Bangsberg D, et al. Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. J Acquir Immune Defic Syndr. 2003;34:281–288. doi: 10.1097/00126334-200311010-00004. [DOI] [PubMed] [Google Scholar]
- 62.Wolfe WR, Weiser SD, Leiter K, et al. The impact of universal access to antiretroviral therapy on HIV stigma in Botswana. Am J Public Health. 2008;98:1865–1871. doi: 10.2105/AJPH.2007.122044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tsai AC, Bangsberg DR, Bwana M, et al. How does antiretroviral treatment attenuate the stigma of HIV? Evidence from a cohort study in rural Uganda. AIDS Behav. 2013;17:2725–2731. doi: 10.1007/s10461-013-0503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Farmer P, Leandre F, Mukherjee JS, et al. Community-based approaches to HIV treatment in resource-poor settings. Lancet. 2001;358:404–409. doi: 10.1016/s0140-6736(01)05550-7. [DOI] [PubMed] [Google Scholar]
- 65.Seeman TE, Bruce ML, McAvay GJ. Social network characteristics and onset of ADL disability: MacArthur studies of successful aging. J Gerontol B Psychol Sci Soc Sci. 1996;51:S191–200. doi: 10.1093/geronb/51b.4.s191. [DOI] [PubMed] [Google Scholar]
- 66.Kaplan RM, Hartwell SL. Differential effects of social support and social network on physiological and social outcomes in men and women with type II diabetes mellitus. J Health Psychol. 1987;6:387–398. doi: 10.1037//0278-6133.6.5.387. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.