Abstract
Objective
This pilot study investigates the use of telerehabilitation to improve upper limb performance in chronic stages of stroke recovery.
Design
Intervention study with pre/post/one month follow-up tests.
Methods
Seven adults with chronic stroke participated in the study. Tests consisted of lab-based clinical and kinematic assessments. Participants completed the Upper Limb Training and Assessment (ULTrA) program at home. Training was 5 days/week, 60 min/day for 6 weeks with intermittent supervision of participants.
Results
Participants showed improvements in the training program tasks as well as clinical and kinematic assessments. Results also suggest there may be auxiliary benefits in cognitive function.
Conclusions
A home-based telerehabilitation program is a viable approach to provide rehabilitation in chronic stages of stroke.
Keywords: stroke, telerehabilitation, rehabilitation, chronic, upper limb
Introduction
Advances in technology have allowed new approaches in stroke rehabilitation. In the last decade, Internet access and use of video conferencing has expanded making it easier to conduct remote training for individuals with upper limb deficits. While earlier studies have examined the effectiveness of remote training within a building (1), or clinic to clinic communications (2), the ability to assess and train individuals in home settings is also feasible (3).
Telerehabilitation has the potential to extend rehabilitation services beyond conventional therapy and address ongoing functional needs of those with chronic upper limb deficits. Improvements continue to be possible in chronic stroke with training (4). In contrast, inactivity post stroke may lead to diminished function (5). Home-based telerehabilitation can integrate established principles of neuroscience related to training (6), with a patient-centered means of program delivery. It allows for monitoring of compliance and progress through measurement of performance even with a lack of continuous one-to-one supervision during training.
Methods
Seven participants (Table I) completed the telerehabilitation training (approximately 60 min/day, 5 days/week for 6 weeks). A comprehensive set of training modules was created to address sensorimotor deficits (3). Participants were provided with a laptop and equipment for modular tasks. Activities performed unilaterally included tactile discrimination, stereognosis, and tool use. In tactile discrimination small pin patterns (square, circle, etc) imbedded in plastic were presented to participants in a 3 sided covered box which obscured vision, but allowed tactile fingertip exploration. The participant then distinguished the pin pattern they felt from 3 computer-displayed shapes. In stereognosis, an object, for example, a wooden letter appeared on the computer screen and participants had to retrieve it from a container without vision. In tool use, children's or standard chopsticks were used to move objects such as corks. Other activities were initially performed unilaterally and then bilaterally. In reaching tasks, participants moved both vertically and horizontally to lighted targets on an “L” shaped target board instrumented with light emitting diodes (LEDs) to outline targets and proximity sensors to capture performance time. Finger tapping was done only on the horizontal aspect of the board. Object manipulation involved grasping and releasing items. While participants were presented with the same modules, difficulty level was tailored to the individual. As participants became proficient with an activity, the task was made more challenging by adding a more difficult movement, such as bilateral movements requiring greater upper limb coordination, or reducing task completion time (3). Module completion time varied as participants were allowed rests as needed. At the beginning of the program there was daily monitoring via Internet video conferencing. Participants gradually became more independent with their programs and video conferencing was reduced to once a week by the final week.
Table I. Participant demographics.
| Participant | Gender/age, years | Affected arm | Post-stroke, years |
|---|---|---|---|
| 1 | M/56 | R | 3.5 |
| 2 | M/63 | R | 11.0 |
| 3 | M/63 | R | 10.0 |
| 4 | F/53 | L | 10.0 |
| 5 | F/47 | R | 3.5 |
| 6 | M/50 | L | 7.5 |
| 7 | M/62 | R | 1.5 |
R: right; L: left.
Six of the participants also completed laboratory-based pre-, post- and one-month follow-up testing consisting of the Streamlined Wolf Motor Function Test (WMFT), a clinical assessment of upper limb function (7), kinematic assessments of unilateral reaching movements from a waist to shoulder height target using an electro-magnetic 3D motion monitor (Ascension Technology Corporation, Burlington, VT), computerized cognitive assessments using CogState software (New Haven, CT) and position sense. Using output data from the 3D motion monitor movement smoothness was calculated using a normalized jerk score (8). Cognitive tests were completed twice during the pre-test session to reduce the influence of a learning effect (9). The second cognitive test was then compared to post-intervention testing. Cognitive assessments focused on working memory (remembering appearance of a playing card), spatial memory (Groton Maze Learning Test in which errors represent either inability to follow basic rules and/or incorrect choice of the maze path) and attention (response time to card turning) (10). Proprioceptive testing of position sense consisted of a matching task (11) where one arm was passively extended 30° (reference position), held for 3 s and then returned to the original position. The participant then reproduced the reference position with the opposite arm (matching position). Absolute error was calculated by taking the absolute value of the difference between the reference and matching movements in degrees. Statistical analysis (using SPSS software, IBM, Armont, NY) consisted of the Wilcoxon signed ranks test and repeated measures analysis in the Mixed procedure, Sidak adjustments were used in post-hoc testing. Training program data were averaged over the first and last weeks for analyses and the effect size was calculated (12). All participants provided informed consent and were financially compensated for their participation.
Results
Training compliance was greater than 90% for all participants. Following training participants performed the motor tasks in the Upper Limb Training and Assessment and program more efficiently (Table II). Across tests, movement smoothness changed (F(82,2) = 4.07, p = 0.02, Fig. 1A). Post hoc testing demonstrated that movements of the more affected arm were smoother at post-testing (p = 0.02) and scores were more similar to those of the less affected hand (Fig. 1B). For 5/6 participants, there was a reduction in streamlined WMFT performance times at post testing (Fig. 2A). All participants demonstrated shorter times at the follow-up compared to the pre-test.
Table II. Mean group percent change in movement time and effect size (Cohen's d) for movement tasks for both the more affected (MA) and less affected (LA) limb.
| Reaching movement | Change in movement time | Effect size | ||
|---|---|---|---|---|
|
|
|
|||
| MA Mean, % | LA Mean, % | MA d | LA d | |
| Unilateral vertical reaching | −14.27 | −7.32 | 0.61 | 0.49 |
| Unilateral horizontal reaching | −11.54 | 1.84 | 0.55 | 0.06 |
| Unilateral finger tapping | −10.25 | 9.07 | 0.48 | 0.13 |
| Bilateral finger tapping | −26.87 | −24.16 | 0.83 | 0.64 |
Fig. 1.
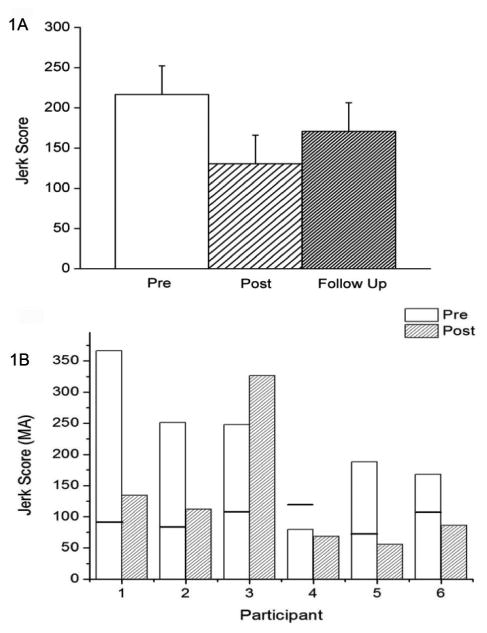
Kinematics of reaching movements. (A) Movement smoothness represented by mean (+1 standard error) normalized jerk score. (B) Bar graphs represent pre/post normalized jerk scores for the more affected (MA) hand of each participant. The line in the pre-test bar represents the normalized jerk score for the less affected hand.
Fig. 2.
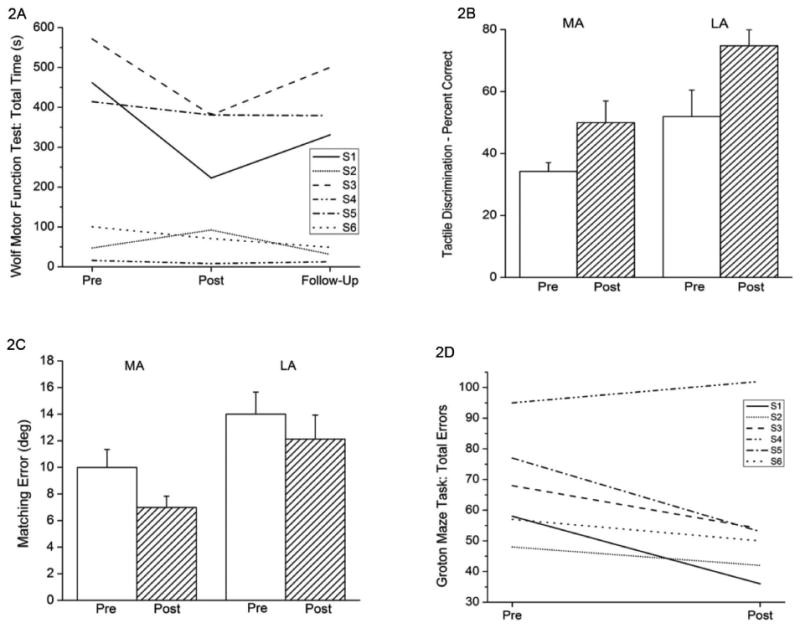
(A) Streamlined Wolf Motor Function Test scores for individual participants, (B) Mean (+ 1 standard error (SE)) tactile discrimination accuracy for the more (MA) and less (LA) affected hand, (C) Mean (+ 1 SE) elbow position matching errors, (D) Total Groton Maze Task errors for individual participants.
Improvements in sensory tasks were also noted. Tactile discrimination performance improved in the less affected hand (degrees of freedom (df) = 6, z = 2.207, p = 0.03) and trended towards improvement in the more affected hand (df = 6, z = 1.859, p = 0.06) following training (Fig. 2B). While proprioceptive matching errors decreased following training, differences between pre and post sessions were not statistically significant (Fig. 2C). Interestingly, joint matching performance was dependent upon which arm performed the matching task. When the more affected arm was used as the reference and the less affected arm performed the matching task, errors were greater (F(131.39,1) = 18.58, p < 0.01).
There was a trend toward improved cognitive performance with 5/6 participants decreasing the number of errors made in the Groton Maze Learning Test (df = 5, z = 1.68, p = 0.09, Fig. 2D). Five of the 6 participants maintained or increased their pace through the maze, suggesting they did not simply slow down to make fewer errors.
Discussion
Adults with chronic stroke demonstrated improved performance across multiple domains following home-based telerehabilitation training. Our results agree with other literature (1) and expand the scope of research by examining sensory and cognitive components. Telerehabilitation has the potential to profoundly change care practices in chronic stages of stroke. Currently, formal rehabilitation is typically discontinued within a year post stroke (13). Independent exercise program are often prematurely discontinued (14), placing the individual at risk for losing function. Home-based telerehabilitation is relatively easy to access and can provide feedback based on either one-to-one supervision or data acquired during training. Regularly monitoring a participant's home program through training data may be a positive way to utilize the Hawthorne effect in which individuals perform better when they know they are being studied. The ability to collect performance data in home-based training offers several opportunities to better understand motor learning and control following stroke which may produce better functional outcomes.
Acknowledgments
This research was supported by Blue Cross and Blue Shield Foundation of Michigan, Grant# N012096-399337. Thanks to R. Napier and C. Loji for their assistance with training and data analyses and K. Welch, MS for her assistance with statistical analyses.
References
- 1.Lange B, Flynn SM, Rizzo AA. Game-based telerehabilitation. Eur J Phys Rehabil Med. 2009;45:143–151. [PubMed] [Google Scholar]
- 2.Demaerschalk BM. Telestrokologists: treating stroke patients here, there, and everywhere with telemedicine. Semin Neurol. 2010;30:477–491. doi: 10.1055/s-0030-1268869. [DOI] [PubMed] [Google Scholar]
- 3.Brown SH, Lewis CA, McCarthy JM, Doyle ST, Hurvitz EA. The effects of Internet-based home training on upper limb function in adults with cerebral palsy. Neurorehabil Neural Repair. 2010;24:575–583. doi: 10.1177/1545968310361956. [DOI] [PubMed] [Google Scholar]
- 4.Taub E, Uswatte G, Elbert T. New treatments in neurorehabilitation founded on basic research. Nat Rev Neurosci. 2002;3:228–236. doi: 10.1038/nrn754. [DOI] [PubMed] [Google Scholar]
- 5.Paolucci S, Grasso MG, Antonucci G, Bragoni M, Troisi E, Morelli D, et al. Mobility status after inpatient stroke rehabilitation: 1-year follow-up and prognostic factors. Arch Phys Med Rehabil. 2001;82:2–8. doi: 10.1053/apmr.2001.18585. [DOI] [PubMed] [Google Scholar]
- 6.Byl NN, Pitsch EA, Abrams GM. Functional outcomes can vary by dose: learning-based sensorimotor training for patients stable poststroke. Neurorehabil Neural Repair. 2008;22:494–504. doi: 10.1177/1545968308317431. [DOI] [PubMed] [Google Scholar]
- 7.Bogard K, Wolf S, Zhang Q, Thompson P, Morris D, Nichols-Larsen D. Can the Wolf Motor Function Test Be Streamlined? Neurorehabil Neural Repair. 2009;23:422–428. doi: 10.1177/1545968308331141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Contreras-Vidal JL, Teulings HL, Stelmach GE. Elderly subjects are impaired in spatial coordination in fine motor control. Acta Psychol (Amst) 1998;100:25–35. doi: 10.1016/s0001-6918(98)00023-7. [DOI] [PubMed] [Google Scholar]
- 9.Falleti MG, Maruff P, Collie A, Darby DG. Practice effects associated with the repeated assessment of cognitive function using the CogState battery at 10-minute, one week and one month test-retest intervals. J Clin Exp Neuropsychol. 2006;28:1095–1112. doi: 10.1080/13803390500205718. [DOI] [PubMed] [Google Scholar]
- 10.Maruff P, Thomas E, Cysique L, Brew B, Collie A, Snyder P, et al. Validity of the CogState Brief Battery: Relationship to Standardized Tests and Sensitivity to Cognitive Impairment in Mild Traumatic Brain Injury, Schizophrenia, and AIDS Dementia Complex. Arch Clin Neuropsychol. 2009;24:165–178. doi: 10.1093/arclin/acp010. [DOI] [PubMed] [Google Scholar]
- 11.Goble DJ, Brown SH. Task-dependent asymmetries in the utilization of proprioceptive feedback for goal-directed movement. Exp Brain Res. 2007;180:693–704. doi: 10.1007/s00221-007-0890-7. [DOI] [PubMed] [Google Scholar]
- 12.Kotrlik JW, Williams HA. The incorporation of effect size in information technology, learning and performance research. Information Technology, Learning, and Performance Journal. 2003;21:1–7. [Google Scholar]
- 13.Langhammer B, Stanghelle JK. Bobath or motor relearning programme? A follow-up one and four years post stroke Clin Rehabil. 2003;17:731–734. doi: 10.1191/0269215503cr670oa. [DOI] [PubMed] [Google Scholar]
- 14.Dishman RK. Exercise compliance – a new view for public-health. Physician Sportsmed. 1986;14:127–145. doi: 10.1080/00913847.1986.11709075. [DOI] [PubMed] [Google Scholar]


